Abstract
Background:
A high incidence of errors occur while filling up death certificates in hospitals. The purpose of this study was to analyze the impact of an educational intervention on errors in death certification in an intensive care unit (ICU). Patients admitted to ICUs by virtue of being critically ill have a higher mortality than other hospitalized patients. This study was designed to see if any improvement could be brought about in filling death certificates.
Materials and Methods:
Educating sessions, interactive workshops, and monthly audits for the department resident doctors were conducted. One hundred and fifty death certificates were audited for major and minor errors (75 before and 75 after the educational intervention) over a period of 18 months. Fisher's exact test was applied to statistically analyze the data.
Results:
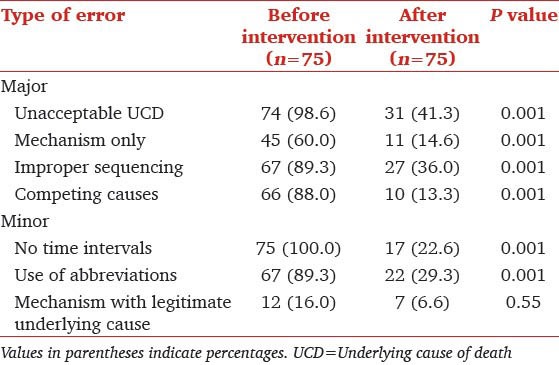
There was a significant decrease in major errors like mechanism without underlying cause of death (60.0 vs. 14.6%, P < 0.001), competing causes (88.0 vs. 13.3%, P < 0.001), and improper sequencing (89.3 vs. 36.0%, P < 0.001). There was also a significant decrease in minor errors such as use of abbreviations (89.3 vs. 29.3%, P < 0.001) and no time intervals (100.0 vs. 22.6%, P < 0.001).
Conclusion:
Authors conclude that death certification errors can be significantly reduced by educational interventional programs.
Keywords: Audit, death certification, educational intervention, errors
Introduction
The death certificate holds importance in dealing with various social and personal issues.[1] Medical Certification of Cause of Death (MCCD) under Civil Registration System, in India, has statutory backing under sections 10 (2) and 10 (3) of the Registration of Births and Deaths Act, 1969.[2] The practice of death certification has led to implementation of effective public health programs.[3] Improper filling up of the MCCD can lead to erroneous epidemiological database and misguided allocation of national resources.[4,5]
Errors in death certification are a global phenomenon. There are studies evaluating the impact of educational intervention programs on death certification errors,[6] but there are no studies in intensive care unit (ICU) in Indian settings where mortality rates are higher than in any other area of the hospital. Our study was aimed to analyze the impact of educational intervention on errors in death certification in ICU.
Materials and Methods
It as an observational study conducted in the department of Critical Care Medicine of a teaching tertiary care institute. The study had prior approval of the hospital ethics committee.
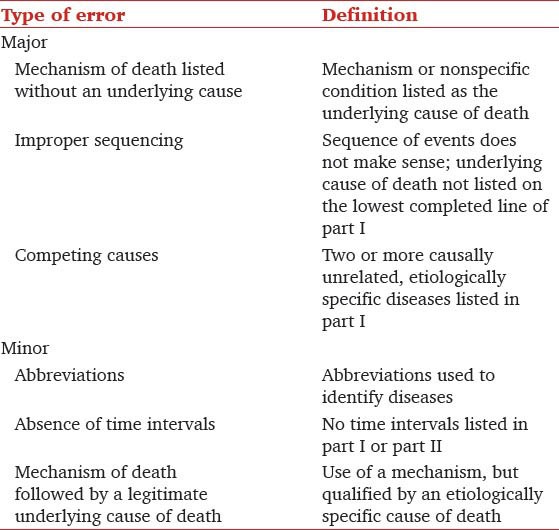
A total of 75 death certificates of the previous 9 months (from July 2009 to March 2010) were randomly obtained from the hospital's record section and were audited for the frequency of major and minor errors by a faculty and the results/errors were kept blind from the resident doctors. We followed a systematic sampling plan, that is, every second death certificate from the hospital record section was selected during the period of study. Time constraints restricted us to 75 certificates, but it would have been better if we would have analyzed the entire certificates available during that period. The errors were defined into major and minor errors as described by Myers and Farquhar[7] [Table 1]. Our institute's death certificate is based on the format given by World Health Organization (copy of death certificate attached).
Table 1.
Definition of major and minor errors in death certificates
Then an educational intervention program was planned for the 12 resident doctors undergoing their subspecialty training in Critical Care Medicine. The program consisted of a lecture taken by a faculty to re-educate the senior residents about the various aspects of a death certificate like the different parts of an MCCD, International Classification of Diseases (ICD) 10, the meaning of various terminologies, significance of writing the certificate correctly, and the types of errors encountered. Following the lecture an interactive workshop was held, wherein the resident doctors were divided into two groups consisting of six resident doctors in each group. Each group was asked to prepare death certificates on mock clinical examples. The mock examples were prepared by the faculty and consisted of brief hypothetical clinical summary of patients presenting to the ICU, his/her course in the ICU, and subsequent death. It was presented on a power point slide to both the groups simultaneously. These examples were worked up in detail by the moderating faculty before being given to the residents regarding the cause of death. A leader was appointed in each group to present the completed MCCD. The session was moderated by a faculty who clarified the queries that arose with regard to the proper filling of the certificate.
Post intervention, a monthly audit was undertaken over the next 9 months from April 2010 to December 2010. Seventy-five death certificates were audited for errors during this period. This audit included the presentation of a brief summary of all the patients who died in the ICU in the preceding month along with their death certificates. The name of the doctor filling up the MCCD was kept hidden. After analysis of the certificates and noting down the errors, the corrected death certificates were presented in the same session to reinforce the correct way of filling these certificates.
Major and minor errors [Table 2] were compared in the pre-intervention and post-intervention preparation of death certificates. Unacceptable underlying cause of death was taken as one which could not explain the sequence of events leading to death. Sample size was calculated based on the level of significance (α = 0.05) and power of test (1-β = 0.80) and critical difference in errors equal to 30%. It was taken because we wanted at least 30% improvement in the death certification after the intervention. Fisher's exact test was applied to compare major and minor errors in the pre-intervention and post-intervention certificates. Major errors included unacceptable underlying cause of death, mechanism of death, improper sequencing, and competing causes as underlying cause of death. Minor errors which were compared included no time interval, use of abbreviations, and mechanism of death with legitimate underlying cause of death. A P < 0.05 was considered as significant.
Table 2.
Frequency of errors identified during the audit of death certificates completed by residents in critical care medicine before and after an educational intervention
Results
A total of 150 death certificates (75 pre-intervention and 75 post-intervention) were studied for major and minor errors over a period of 18 months.
A significant number (98.6%) of death certificates filled up in the pre-intervention period had an unacceptable ‘underlying cause of death’ or at least one major error. ‘Improper sequencing’ (89.3%), ‘competing causes’ (88%), and ‘mechanism only’ (60%); all contributed to the major errors. Amongst minor errors, all pre intervention MCCDs had ‘no time intervals’ (100%) and the ‘use of abbreviations’ (89.3%) was high. After the educational intervention, there was a statistically significant (P < 0.05) decrease in all major errors which included unacceptable underlying cause of death (41.3%), listing mechanism of death (14.6%), improper sequencing (36%), and competing causes (13.3%). The minor errors showed a statistically significant decline in the category of ‘no time intervals’ (22.6%) and ‘use of abbreviations’ (29.3%).
Discussion
Increased education and better documentation leads to reduction in errors and improves legitimacy of death certificates.[8,9] One study showed that death certificates were completed with errors by 71.1% of the physicians before the educational intervention. Following the seminar, the proportion of death certificates with errors decreased to 9% (P < 0.0001).[10]
Errors in death certificates have been classified into major and minor.[11] The concept of the “underlying cause of death” which if not filled properly becomes a major error is often a source of confusion for certifying physicians.[12] Such errors can be more prone to occur in intensive care settings due to the complex case scenarios and multimodal presentations. It was strongly advocated in our program not to mention mechanisms of death like cardiorespiratory arrest or cardiac arrest as the cause of death since they amount to major errors.
Despite a few Indian studies in teaching and nonteaching hospitals aiming at improvement in the quality of death certification,[13,14] there has been no Indian published study from an ICU settings. A previous ICU based study in a developed country shows an incomplete and inaccurate process of death certification within the ICU.[15]
Our study design was similar to the one used by Myers and Farquhar.[7] However, apart from statistically proven reduction in major errors (as seen in previous studies also) our study also showed a significant reduction in minor errors. This was found to be statistically significant in the categories of ‘no time intervals’ and ‘use of abbreviations’.
Though it was not the primary objective of this study; an assessment about the impact of the time of death (day vs. night) on the error rate was also analyzed, but we did not find any significant relation. Errors that continued to occur even after regular educational intervention in our study were attributed to behavioral traits. Authors believe that individual interaction with the ‘defaulter’ residents and prior faculty discussion during the routine rounds as to the sequence of events in a seriously ill patient who is likely to die can reduce the error rates.
To reduce errors, it has been also recommended that death certification be completed by a physician who is familiar with the patient, even if this delays its completion.[16] However, in the Indian context this may not be possible because the family may need to travel to a distant place to perform the last rites of his relative.
The limitation of this study is that it includes death certificates from ICU only and not from other specialties. Hence, our results on errors in death certificate may not represent the total death form errors occurring in our hospital. Another limitation is that, we analyzed 75 certificates only in the pre-intervention death certificates. If we had analyzed the entire certificates, our sample size would have increased and also the strength of our study.
In conclusion, authors would like to emphasize that frequent educational courses should be carried out regarding training resident doctors for filling up the death certificates. Educational interventions not only reduce the error rates but also increase awareness regarding the consequences of a poorly filled out MCCD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Bokil PV. Death certificate. QPMPA J Med Sci. 2002;16:84–6. [Google Scholar]
- 2.New Delhi: Medical Certification of Cause of Death, presented at Vigyan Bhavan; Jan 27th – 28th, [Last accessed on 31 Jan 2011]. Status of Medical Certification of Cause of Death in India. Available From: http://gujhealth.gov.in/basicstatastics/pdf/MCCD.ppt . [Google Scholar]
- 3.Davis GG. Mind your manners. Part I: History of death certification and manner of death classification. Am J Forensic Med Pathol. 1997;18:219–23. doi: 10.1097/00000433-199709000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Madsen A, Thihalolipavan S, Maduro G, Zimmerman R, Kopaaka R, Li W, et al. An intervention to improve cause-of-death reporting in New York City hospitals, 2009-2010. Prev Chronic Dis. 2012;9:E157. doi: 10.5888/pcd9.120071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tormey WP. Accuracy of death certification. Br J Psychiatry. 2011;199:432–3. doi: 10.1192/bjp.199.5.432b. [DOI] [PubMed] [Google Scholar]
- 6.Pandya H, Bose N, Shah R, Chaudhary N, Phatak A. Educational intervention to improve death certification at a teaching hospital. Natl Med J India. 2009;22:317–9. [PubMed] [Google Scholar]
- 7.Myers KA, Farquhar DR. Improving the accuracy of death certification. CMAJ. 1998;158:1317–23. [PMC free article] [PubMed] [Google Scholar]
- 8.Selinger CP, Ellis RA, Harrington MG. A good death certificate: Improved performance by simple educational measures. Postgrad Med J. 2007;83:285–6. doi: 10.1136/pgmj.2006.054833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aung E, Rao C, Walker S. Teaching cause-of-death certification: Lessons from international experience. Postgrad Med J. 2010;86:143–52. doi: 10.1136/pgmj.2009.089821. [DOI] [PubMed] [Google Scholar]
- 10.Villar J, Pérez-Méndez L. Evaluating an educational intervention to improve the accuracy of death certification among trainees from various specialties. BMC Health Serv Res. 2007;7:183. doi: 10.1186/1472-6963-7-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weeramanthri T, Beresford B. Death certification in Western Australia-classification of major errors in certificate completion. Aust J Public Health. 1992;16:431–4. doi: 10.1111/j.1753-6405.1992.tb00092.x. [DOI] [PubMed] [Google Scholar]
- 12.Maudsley G, Williams EM. Death certification by house officers and general practitioners – practice and performance. J Public Health Med. 1993;15:192–201. [PubMed] [Google Scholar]
- 13.Garg A, Singh SV, Gupta VK. Accuracy of medical certification of the cause of death in a rural non-teaching hospital in Delhi. Natl Med J India. 2012;25:185–6. [PubMed] [Google Scholar]
- 14.Shantibala K, Akoijam BS, Usharani L, Singh HN, Laishram J, Singh TA. Death certification in a teaching hospital – a one year review. Indian J Public Health. 2009;53:31–3. [PubMed] [Google Scholar]
- 15.Tuffin R, Quinn A, Ali F, Cramp P. A review of the accuracy of death certification on the intensive care unit and the proposed reforms to the Coroner's system. J Iran Chem Soc. 2009;10:134–7. [Google Scholar]
- 16.Pritt BS, Hardin NJ, Richmond JA, Shapiro SL. Death certification errors at an academic institution. Arch Pathol Lab Med. 2005;129:1476–9. doi: 10.5858/2005-129-1476-DCEAAA. [DOI] [PubMed] [Google Scholar]


