Abstract
Congenital granular cell tumor (CGCT), or congenital epulis, is an uncommon benign soft tissue lesion that usually arises from the alveolar mucosa of neonates and may cause respiratory and feeding problems. The histogenesis and clinical history of the lesion remains obscure. Treatment involves surgical excision and recurrences are rare. The present report describes a case of congenital granular cell lesion (CGCL) in the anterior segment of maxillary alveolar ridge of a 2-month-old female. This lesion was causing feeding problem and was excised under local anesthesia, with no recurrence even after 3 years.
Keywords: Congenital epulis, congenital granular cell lesion, Newman's tumor
INTRODUCTION
Congenital granular cell lesion (CGCL) is a rare benign soft tissue tumor of the newborn. It is also synonymously known as gingival granular cell tumor (GCT) of the newborn and was first described by Newmann in 1871, hence also called as Newmann's tumor.[1] CGCL is a rare lesion of the newborn with an incidence of just 0.0006%.[2] To the best of our knowledge only 50 cases have been reported so far.[3] Though benign, this tumor may cause hindrance in breathing and suckling, depending upon the size and position of the growth. Although spontaneous regression has been documented, but the recommended treatment is surgical excision with no reports of recurrence after resection.[4]
This case report is unique as differential diagnosis has been included so as to help the clinician to arrive at a more conclusive diagnosis thereby helping him to plan the treatment accordingly. Also, more the number of case reports on this entity more is the likelihood that we will be able to build a conclusive base for the histogenesis of this uncommon and obscure lesion.
CASE REPORT
A 2-month-old female child was referred with the chief complaint of difficulty in feeding since a few days. On examination a 2 × 2 × 1 mm pedunculated growth was observed arising from the left side of maxilla in the canine region. The lesion was pink in color, similar to that of the surrounding mucosa, surface was smooth without any ulcerations and was firm in consistency. The patient was uncomfortable because of this small growth which was possibly hindering proper suction during breast feeding.[Figure 1]. Surgical excision of the growth was performed under local anesthesia. There was minimal bleeding during the procedure and the infant was comfortable with breast feeding from the very next day. The gingival mass was fixed in formalin and sent for histopathological examination.
Figure 1.

Clinical photograph showing small pedunculated gingival mass
Histopathological examination
Hematoxylin and Eosin (H and E) stained section showed keratinized stratified squamous epithelium and underlying connective tissue stroma. High power view showed delicate Collagen fibers, numerous young fibroblasts and granular cells [Figure 2]. The granular cells were large oval cells with an eosinophillic and granular cytoplasm and single basophilic nucleus; these were seen to be scattered amidst the connective tissue [Figure 3]. Clinicopathological correlations were suggestive of CGCL.
Figure 2.
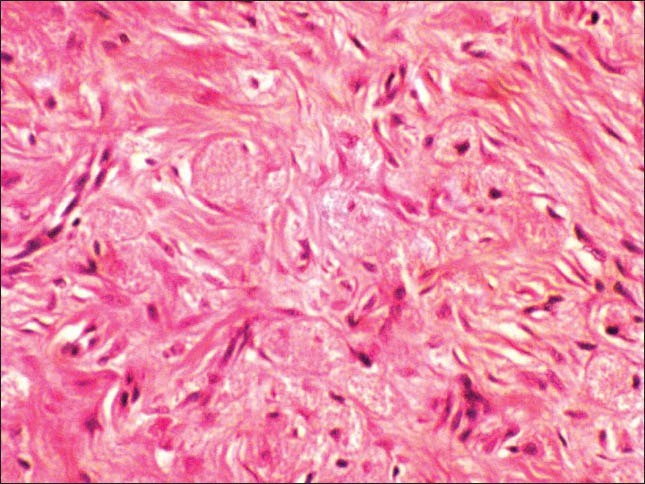
Photomicrograph showing delicate collagen fibers Abundant fibroblasts and granular cells (H&E stain, ×200)
Figure 3.
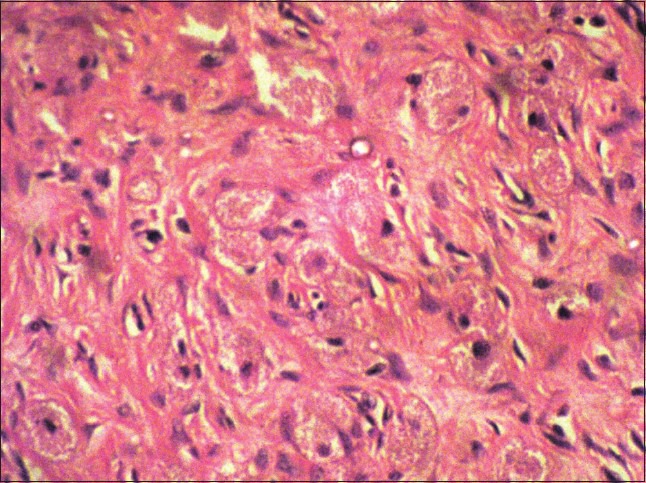
Large oval cells with granular cytoplasm and single basophilic nucleus which were scattered between collagen fibers and fibroblasts. (H&E stain, ×100)
DISCUSSION
Epulis is a Greek word literally meaning “of the gums” and is used to describe a variety of gingival overgrowths. CGCL is a rare, gingival tumor that usually arises in the incisor-canine region of the maxilla (maxilla: mandible ratio is 3:1).[5] This soft tissue tumor appears as smooth-surfaced, pedunculated growth which may be lobulated at times and arises from the gingival mucosa of maxilla or mandible.[6] It ranges in size from few millimetres to 9 cm (as reported till date), with a female preponderance of 8:1.[7]
They are usually firm in consistency, covered by a smooth or erythematous mucosa and are attached by means of a stalk to the underlying tissue. Early diagnosis can be made by prenatal ultrasonography or magnetic resonance imaging (MRI). However, MRI is considered to be superior to ultrasonography, showing its gingival origin without local extension.[8] Treatment of choice is surgical excision.
Histogenesis of this tumor is unclear and the proposed cells of origin are probably derived from one of the sources, that is, odontogenic epithelium, undifferentiated mesenchymal cells, pericytes, fibroblasts, smooth muscle cells, nerve related cells and histiocytes.[4,9] An endogenous hormonal stimulus has been proposed as the reason for its occurrence in neonates and for female predominance. But this theory was not accepted because of the lack of detectable estrogen and progesterone receptors within the lesion.[8,9]
Histologically, CGCL shows a remarkable similarity with the more common GCTs.[10] However, there are striking microscopic and epidemiological differences between the two. GCT is comparatively less vascular with an occasional component of pseudoepitheliomatous hyperplasia and contains more conspicuous nerve bundles as compare to CGCL. CGCL solely occurs on the gum pads of infants; whereas, GCT occurs in adults and may involve multiple organs.[10] Immunohistochemically, GCTs are reactive to S-100 protein and laminin, while these are absent in CGCL. GCTs also show positive staining for NGFR/p75 and inhibin-α, while CGCL does not.[11,12]
Differential diagnosis includes melanotic neuroectodermal tumor of infancy (MNTI), hemangioma, fibroma, embryonal rhabdomyosarcoma, granuloma, malignant granular cell myoblastoma, chondrogenic and osteogenic sarcoma and schwannoma.[13]
MNTI is an osteolytic pigmented neoplasm primarily affecting jaws of newborns. However, MNTI and CGCL are distinctly different as MNTI is infiltrating, contains melanin pigment and tumor mass comprises of alveolar spaces lined by cuboidal or large polygonal cells having pale cytoplasm. Hemangioma is primarily a vascular lesion with budding endothelial cells and essentially not present at birth; whereas, CGCLs manifest within the 1st month of life. Fibroma is more common in 5th, 6th and 7th decade. It consists of bundles of interlacing collagen fibers and no granular cells. Embryonal rhabdomyosarcoma is a malignant tumor of striated muscle and uncommon in the oral cavity. Granuloma is primarily a focal collection of epithelioid cells, lymphocytes and giant cells. Malignant granular cell myoblastoma is commonly seen between 30 and 60 years of age. Histologically, granular cells are in ribbons separated by septa giving an appearance of invasion or infiltration into underlying tissues. Chondrogenic and osteogenic sarcoma are malignant tumors characterized by chondroid or osteoid tissue, respectively. Schwannoma is a tumor of neural origin which shows Antoni A and B areas and Verocay bodies.
In conclusion, CGCL can be diagnosed by prenatal sonography, but prenatal findings are not specific.[14]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Newmann E. Ein fall von Kongenitalu epulis. Arch Heilkd. 1871;12:189–90. [Google Scholar]
- 2.Bosanquet D, Roblin G. CGCL: A case report and estimation of incidence. Int J Otolaryngol. 2009;31:198–9. doi: 10.1155/2009/508780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dash JK, Sahoo PK, Das SN. Congenital granular cell lesion “congenital epulis”- Report of a case. J Indian Soc Pedod Prev Dent. 2004;22:63–7. [PubMed] [Google Scholar]
- 4.Fuhr AH, Krogh PH. CGCL of the newborn: centennial review of the literature and a report of case. J Oral Surg. 1972;30:30–5. [PubMed] [Google Scholar]
- 5.Lack EE, Perez-Atayde AR, McGill TJ, Vawter GF. Gingival granular cell tumour of the newborn (congenital epulis): ultrastructural observations relating to histogenesis. Hum Pathol. 1982;13:686–9. doi: 10.1016/s0046-8177(82)80018-x. [DOI] [PubMed] [Google Scholar]
- 6.Lapid O, Shaco-Levy R, Krieger Y, Kachko L, Sagi A. Congenital epulis. Pediatrics. 2001;107:e22. doi: 10.1542/peds.107.2.e22. [DOI] [PubMed] [Google Scholar]
- 7.Kanotra S, Kanotra SP, Paul J. Congenital epulis. J Laryngol Otol. 2006;120:148–50. doi: 10.1017/S0022215105005359. [DOI] [PubMed] [Google Scholar]
- 8.Silva GC, Vieira TC, Vieira JC, Martins CR, Silva EC. Congenital granular cell tumour (congenital epulis): a lesion of multidisciplinary interest. Med Oral Patol Cir Bucal. 2007;12:E428–30. [PubMed] [Google Scholar]
- 9.Raissaki MT, Segkos M, Prokotakis EP, Haniotis V, Velegrakis GA, Gourtsoyiannis N. Congenital granular cell tumour (epulis): post natal imaging appearances. J Comp Assist Tomogr. 2005;29:520–3. doi: 10.1097/01.rct.0000167475.66503.31. [DOI] [PubMed] [Google Scholar]
- 10.Damm DD, Cibull ML, Geissler RH, Neville BW, Bowden CM, Lehmann JE. Investigations into histogenesis of congenital epulis of newborn. Oral Surg Oral Med Oral Pathol. 1993;76:205–12. doi: 10.1016/0030-4220(93)90206-j. [DOI] [PubMed] [Google Scholar]
- 11.Leocata P, Bifaretti G, Saltarelli S, Corbacelli A, Ventura L. Congenital (granular cell) epulis of the newborn: a case report with immunohistochemical study on the histogenesis. Ann Saudi Med. 1999;19:527–9. doi: 10.5144/0256-4947.1999.527. [DOI] [PubMed] [Google Scholar]
- 12.Vered M, Dobriyan A, Buchner A. Congenital granular cell epulis presents an immunohistochemical profile that distinguishes it from granular cell tumour of the adult. Virchows Arch. 2009;454:303–10. doi: 10.1007/s00428-009-0733-y. [DOI] [PubMed] [Google Scholar]
- 13.Rajendran R, Shivpathasundaram B, editors. 6th ed. Amsterdam: Elsevier Publication; Shafer's Textbook of Oral Pathology. [Google Scholar]
- 14.Tokar B, Boneval C, Mirapoglu S, Tetikkurt S, Aksöyek S, Salman T, et al. Congenital granular cell tumour of gingiva. Pediatr Surg Int. 1998;13:594–6. doi: 10.1007/s003830050412. [DOI] [PubMed] [Google Scholar]


