Abstract
Nasolabial cysts are painless, submucosal, non-odontogenic jaw cysts presenting as soft tissue swellings in the maxillary anterior mucolabial fold lateral to midline, leading to elevation of nasal ala. Present case documents bilateral nasolabial cysts in a 69-year-old Asian female patient. In the present case, extraoral swelling of maxillary lip and elevation of nasal ala was observed on right side of the face. Intraorally, soft and fluctuant bilateral cysts were observed. Straw-colored fluid was aspirated from the right cyst. Radiographically, erosion of bone in a “cupping” fashion was observed in the region of left cyst. The cysts were enucleated using intraoral approach. Histopathology of the right-sided cyst revealed a cystic cavity lined by stratified squamous cells along with a few mucosal cells. At few places, stratified squamous and pseudostratified columnar epithelia with many cilia and goblet cells were also evident. Capsule was loosely arranged with fibrous tissue and chronic inflammatory infiltrate. Left-sided cystic specimen showed two or more layered stratified squamous lining epithelium with thin capsule. Diagnosis of bilateral nasolabial/nasoalveolar cysts was confirmed.
Keywords: Non-odontogenic cyst, nasoalveolar, nasolabial
INTRODUCTION
Nasolabial cyst is a rare developmental/fissural cyst that may involve bone secondarily.[1] Intraorally, it presents as a soft-tissue swelling of the maxillary anterior mucolabial fold, lateral to midline leading to obliteration of the nasolabial fold. It is submucosal and extraosseous, spreads in the labial sulcus and expands all the soft tissues outwards.[2] Extraorally, it appears as a swelling between the upper lip and nasal aperture causing elevation of nasal ala.[3] The terms nasolabial and nasoalveolar cysts have been used synonymously, as these are similar cysts with the only difference that the former is a lesion located entirely within the soft tissues and the latter causes maxillary alveolar bone erosion.[4,5] A case report of a female patient with such bilateral cysts is presented here.
CASE REPORT
A 69-year-old female reported to the Dental college with a chief complaint of an extraoral swelling on the right side of her upper lip and elevation of the alar base [Figure 1a] since 7-8 months. History of present illness revealed that the swelling had increased in size since its initiation but was not associated with any pain, drainage through oral/nasal cavity or difficulty in breathing through nasal obstruction. Furthermore, there was no history of dacryocystitis/watery eyes but there was a swelling intraorally corresponding to this extraoral swelling which was obliterating the labial vestibule on that side.
Figure 1.
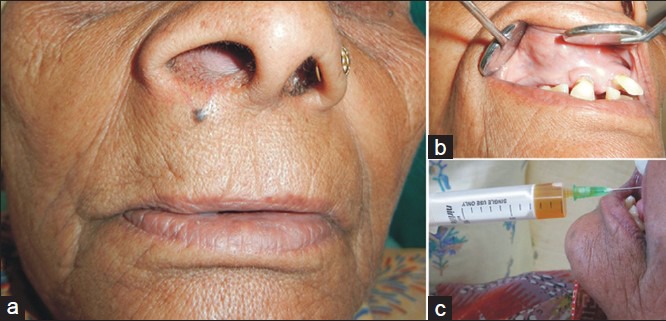
(a) Clinical picture showing extraoral swelling and elevation of alar base on the right side. (b) Clinical picture showing intraoral swelling in the labial vestibule on the right side. (c) Straw-colored fluid on aspiration from the right-sided cyst
Intraoral examination revealed bilateral smooth, soft, fluctuant masses lateral to the central incisor teeth in the maxillary labial vestibule. The right-sided mass was well-defined [Figure 1b] and measured approximately 2 × 3 cm and left-sided mass measured 1.5 × 1.5 cm when palpated bimanually. Aspiration biopsy from right-sided mass revealed straw-colored fluid [Figure 1c].
Occlusal radiograph [Figure 2a] showed a large scooped-out radiolucent area with ‘cupping’ surrounding upper left central incisor (UL1) in the middle and coronal thirds of its root, but not in the periapical area. Radiograph was noncontributory on right side. Provisional diagnosis of bilateral nasolabial cysts was made on the basis of above findings. Patient's informed consent was availed for the surgical removal of these cysts. Medical history did not present any contraindication for the surgical procedure.
Figure 2.
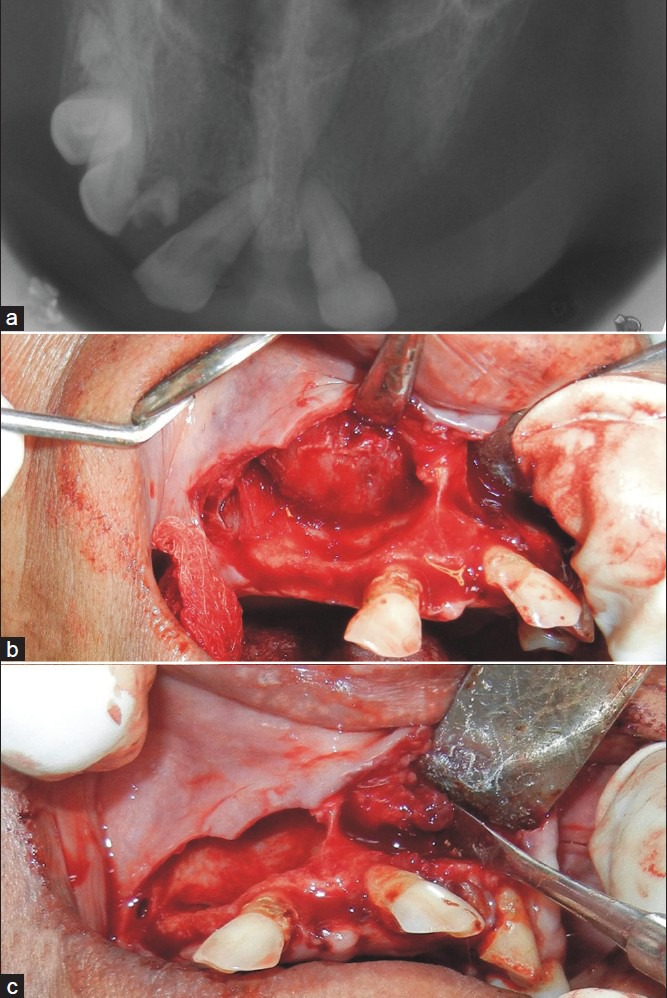
(a) Occlusal radiograph showing erosion of bone in a “cupping” fashion. (b) Enucleation of right cyst. (c) Enucleation of left cyst
The cysts were enucleated [Figure 2b and c] using intraoral approach under local anesthesia and adrenaline (1:80,000). A full-thickness incision was reflected along the crest of maxillary alveolar ridge in the canine to canine region and blunt dissection by periosteal elevator exposed two smooth, well-circumscribed cystic swellings just below the nasal floor. There had been scooping of the anterior maxilla on the left side due to expansion of the cyst. In contrast, morphology of alveolar bone on right side was not affected. In the same appointment, extractions of hopeless teeth were also done and the wound was closed with loop sutures using 3-0 non-absorbable black mersilk after debridement and irrigation with normal saline. Postoperative instructions were delivered. Tissue was sent for histopathological confirmation.
Histopathology of the right-sided cyst revealed a cystic cavity lined by variable thickness of epithelium predominantly made up of many layered stratified squamous cells along with a few mucosal cells [Figure 3]. At few places, stratified squamous and pseudostratified columnar epithelia with many cilia and goblet cells were also evident [Figure 4a and b]. Capsule showed loosely arranged fibrous tissue infiltrated with dense diffuse chronic inflammatory infiltrate. Left-sided cyst specimen showed two or more layered stratified squamous lining epithelium with thin capsule [Figure 5]. Diagnosis confirmed the presence of bilateral nasolabial cysts.
Figure 3.
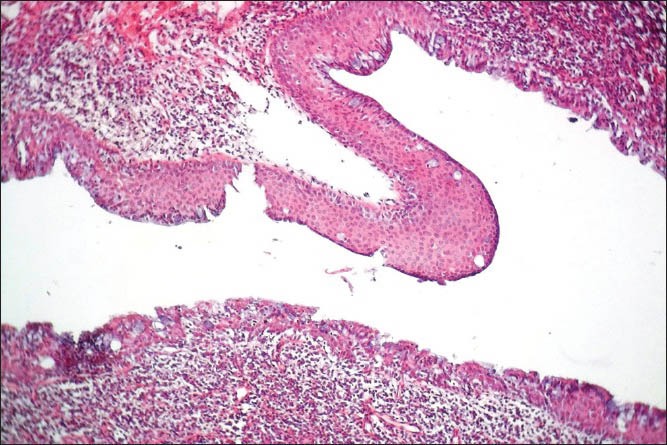
Photomicrograph of a section of right cyst showing epithelial lining predominantly made of many layered stratified squamous cells with few mucosal cells (H&E stain, ×100)
Figure 4.
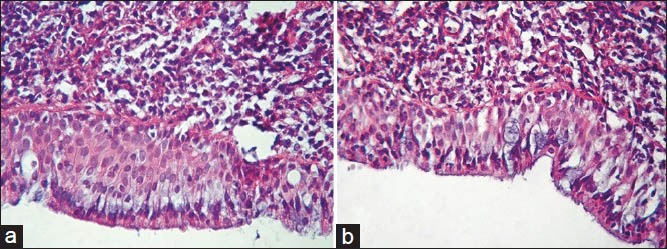
(a) Photomicrograph of right cyst: Stratified squamous epithelium with mucous cells and cilia (H&E stain, ×400). (b) Photomicrograph of right cyst: Pseudostratified ciliated columnar epithelium with goblet cells (H&E stain, ×400)
Figure 5.

Photomicrograph of left cyst showing cystic cavity lined by stratified squamous non-keratinized epithelium with thin capsule (H&E stain, ×40)
DISCUSSION
Nasolabial cyst may be asymptomatic or cause a swelling in the mucolabial fold. Patients seek medical assistance when the cyst becomes infected or cause a cosmetic defect.[1,2,4,5,6] In the present case, intraoral swellings were present in the labial vestibule on both sides, lateral to the maxillary central incisors, which is the most common symptom associated with this cyst.[1,7]
As the nasolabial cysts arise in soft tissues, in most cases there are no radiographic changes. Occasionally, pressure resorption of the underlying bone may occur, in that case, it is known as nasoalveolar cyst, where the cyst being external to the alveolar bone, produces “cupping” of the underlying cortical plate.[4] In the present report, erosion of bone in a “cupping” fashion around UL1 was observed as a sequel of pressure from the cyst.
Routine intraoral radiographs are not diagnostic for nasoalveolar cysts but assist in excluding other odontogenic or non-odontogenic cysts. Periapical inflammatory lesions can be excluded by vitality testing of the associated teeth and the absence of radiolucency in the periapical region on intraoral radiographs. Globulomaxillary and nasopalatine duct cysts can easily be mistaken as nasolabial cysts; however, both of these are intraosseous lesions.[8] In the present case, periapical radiolucency with maxillary anterior teeth was absent. On the contrary, the rarefaction was observed in the middle and coronal third of the root of UL1. Adjacent teeth were vital.
Nasolabial cyst does not cause any displacement of the teeth. However, Cohen and Hertzanu[5] have reported a case of nasolabial cyst with a high growth potential that resulted in the erosion of maxillary alveolus, invaded supporting structures in the region of incisors and caused displacement of these teeth. In the present case also, there were signs of displacement of adjacent teeth. Distolabial migration of the crowns of upper central incisors was primarily due to loss of periodontal support caused by periodontitis in addition to pressure from the cyst.
10.6% of nasolabial cysts are bilateral, this finding suggests that these cysts are developmental in origin.[9] Etiopathogenesis of this cyst involves two theories suggesting that it arises:
As a fissural cyst which develops from embryonic nasal epithelium entrapped between the merging maxillary processes and the medial and lateral nasal processes[10]
As a developmental cyst arising from the remnants of the embryonic nasolacrimal ducts, due to histological similarities to the latter.[11] Furthermore, this cyst is in the area of the naso-optic furrow and proliferation of the nasolacrimal duct has been seen at this site. Although this theory may need some revision, due to the finding of apocrine secretion along the surface of the nasolabial cyst, it seems to be the most accepted one at this stage.[12] The fact that high percentage of linings demonstrate pseudostratified columnar epithelium,[9] often with cilia or numerous goblet cells, is compatible with origin from primitive ductal or glandular structures. So, the most likely origin is from the nasolacrimal duct.[4] In case presented here, the cystic lining was predominantly stratified squamous type, although few areas showed pseudostratified ciliated columnar epithelium. Su et al.,[13] in their scanning electron microscopic examination revealed that cilia observed in the light microscope were in fact numerous short globular or irregular microvilli which probably resulted from lack of stimulation by air.
In the present case, bimanual palpation (best method of diagnosing this cyst by placing one finger in the labial sulcus and the other on the nasal floor)[9] revealed soft, fluctuant masses bilaterally. Dimension of the cyst in the soft tissues of the labial sulcus was more (2 × 3 cm) on the right side which also produced an extraoral swelling because this cyst was exclusively an extraosseous one. In contrast, the left-sided cyst measured relatively less (1.5 × 1.5 cm) in the soft tissues with no corresponding extraoral swelling because the cyst was occupying space between the vestibular sulcus and alveolar bone as was evident on surgical exploration.
The preferred method of treatment of this cyst is surgical excision by intraoral sub-labial approach, although care must be exercised to prevent perforation and collapse of the lesion.[7,9] The surgical outcome of this method is generally successful; however, complications associated with the procedure include facial swelling, gingival numbness, decreased sensation of the teeth, and wound infection. An alternative transnasal approach has been suggested that allows endoscopic marsupialization of the cystic cavity.[14] In the present case, full thickness incision was given on the crest of the ridge instead of sub-labial incision (and a mucoperiosteal flap was reflected with a periosteal elevator to expose the cysts) because the surgical procedure was inclusive of extractions of adjacent mutilated teeth.
So, in the presented case; clinical, radiographic and histological features of the lesions were suggestive of nasolabial cyst on the right side and nasoalveolar cyst (residing on the alveolar surface) on the left side, which were successfully enucleated by a modification of intraoral sublingual surgical approach. In 1-year follow-up, no evidence of complications or recurrence was observed.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.el-Din K, el-Hamd AA. Nasolabial cyst: A report of eight cases and a review of the literature. J Laryngol Otol. 1999;113:747–9. doi: 10.1017/s0022215100145098. [DOI] [PubMed] [Google Scholar]
- 2.Kuriloff DB. The nasolabial cyst-nasal hamartoma. Otolaryngol Head Neck Surg. 1987;96:268–72. doi: 10.1177/019459988709600307. [DOI] [PubMed] [Google Scholar]
- 3.Friedrich RE, Scheuer HA, Assaf AT, Zustin J. Nasolabial cyst: Case report with respect to immunohistochemical findings. In Vivo. 2012;26:453–8. [PubMed] [Google Scholar]
- 4.Neville BW, Damm DD, White DK. 2nd ed. Hamilton: BC Decker Inc; 2003. Color atlas of clinical oral pathology; p. 24. [Google Scholar]
- 5.Cohen MA, Hertanzu Y. Huge growth potential of the nasolabial cyst. Oral Surg Oral Med Oral Pathol. 1985;59:441–5. doi: 10.1016/0030-4220(85)90077-5. [DOI] [PubMed] [Google Scholar]
- 6.Roed-Petersen B. Nasolabial cysts. A presentation of five patients with a review of the literature. Br J Oral Surg. 1969;7:84–95. doi: 10.1016/s0007-117x(69)80002-8. [DOI] [PubMed] [Google Scholar]
- 7.Choi JH, Cho JH, Kang HJ, Chae SW, Lee SH, Hwang SJ, et al. Naso-labial cyst: A retrospective analysis of 18 cases. Ear Nose Throat J. 2002;81:94–6. [PubMed] [Google Scholar]
- 8.Lee J, Christmas PI. Bilateral nasolabial cysts: A case report. N Z Dent J. 2009;105:43–6. [PubMed] [Google Scholar]
- 9.Shear M, Speight PM. 4th ed. Oxford: Blackwell Munksgaard; 2007. Cysts of the Oral and Maxillofacial Regions; pp. 120–22. [Google Scholar]
- 10.Klestadt WD. Nasal cysts and the facial cleft cyst theory. Ann Otol Rhinol Laryngol. 1953;62:84–92. doi: 10.1177/000348945306200108. [DOI] [PubMed] [Google Scholar]
- 11.Van Bruggemann A. Cysts as a result of developmental problems in the nasal vestibule. Arch Oto Rhino Laryn. 1920;33:103–19. [Google Scholar]
- 12.Lopez-Rios F, Lassaletta-Atienza L, Domingo-Carrasco C, Martinez-Tello FJ. Nasolabial cyst: Report of a case with extensive apocrine change. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:404–6. doi: 10.1016/s1079-2104(97)90039-1. [DOI] [PubMed] [Google Scholar]
- 13.Su CY, Huang HT, Liu HY, Huang CC, Chien CY. Scanning electron microscopic study of the nasolabial cyst: Its clinical and embryologic implications. Laryngoscope. 2006;116:307–11. doi: 10.1097/01.mlg.0000199598.37461.8e. [DOI] [PubMed] [Google Scholar]
- 14.Su CY, Chien CY, Hwang CF. A new transnasal approach to endoscopic marsupialization of the nasolabial cyst. Laryngoscope. 1999;109:1116–8. doi: 10.1097/00005537-199907000-00020. [DOI] [PubMed] [Google Scholar]


