CASE REPORT
A 45-year-old female patient reported to the dental clinic with a complaint of swelling over the palate since 6 months. The patient had reported a couple of years back with a similar swelling at the same site which was diagnosed as minor salivary gland carcinoma 5 years back.
Intra-oral examination revealed a large lobulated mass 4.5 × 3 cm in dimension. The swelling was covered by smooth stretched oral mucosa, appearing reddish at areas. Swelling extends from the midline of the palate to the gingiva of 22-27, mediolaterally and from 11-27 anteroposteriorly. The lobulated mass was soft to firm in consistency, causing discomfort but no pain.
Radiograph revealed areas of bone erosion and destruction of the palate. Surgically, the lesion was quite vascular, was ill-circumscribed and soft to firm in consistency.
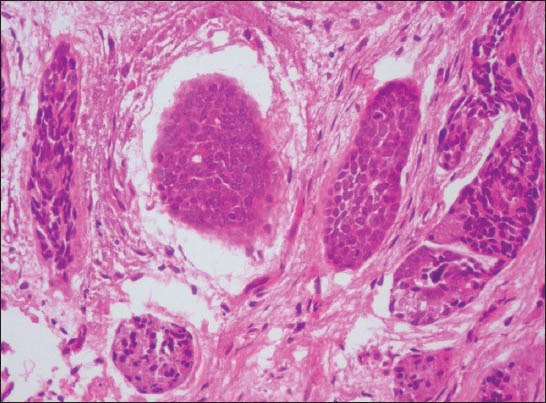
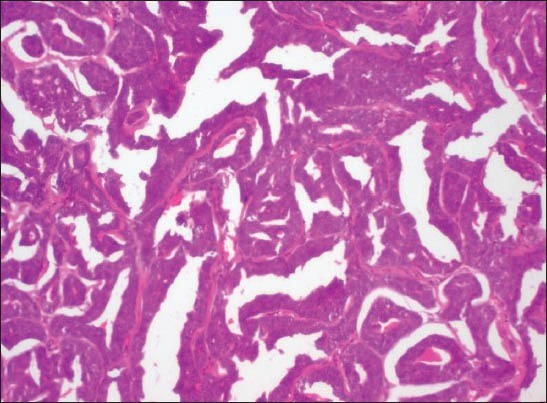
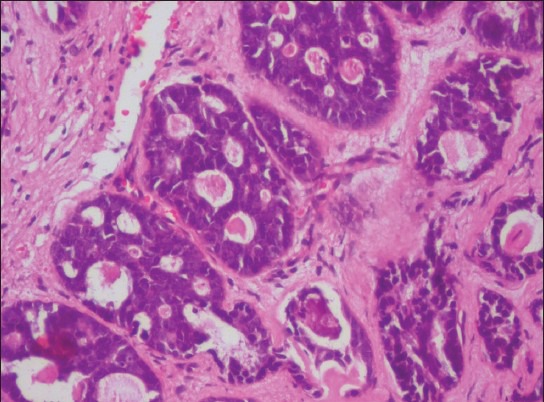
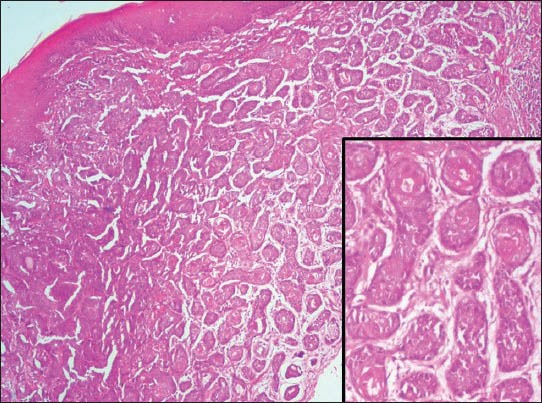
Microscopically, connective tissue stroma composing of lesional cells arranged in cords, nests, islands, cribriform pattern and in ductal structures with central eosinophilic coagulum was seen [Figure 1]. Classical areas of tumor cells arranged in epimyoepithelial islands were evident [Figure 2]. Areas of perineural and perivascular invasion were noted [Figure 3]. The neoplastic cells appeared uniform and basaloid with hyperchromatic nuclei. However other lesional areas showed solid transformation of the numerous cords, nests, islands and cribriform areas [Figure 4]. Some islands showed squamous metaplasia-like areas [Figure 5]. Areas were seen undergoing adenocarcinomatous change with basaloid tumor cells arranged in anastomosing cords with intervening thin fibrovascular connective tissue [Figure 6].
Figure 1.
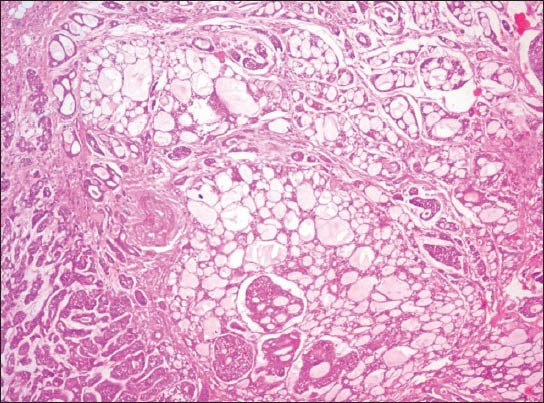
Tumor cells arranged in classical cribrifiorm pattern with ductal structures containing central eosinophilic coagulum; with one area showing compact arrangement of tumor cells (H&E stain, ×40)
Figure 2.
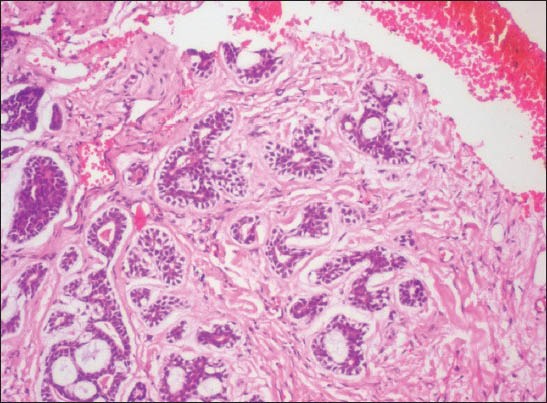
Tumor islands in cribriform, tubular, solid and epimyoepithelial pattern (H&E stain, ×40)
Figure 3.
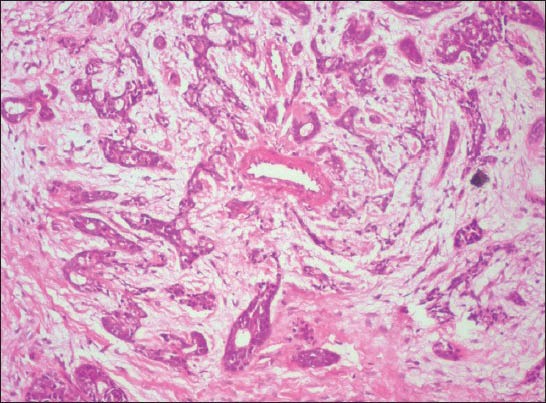
Basaloid neoplastic cells arranged in clusters, nests and cribriform pattern around blood vessel (perivascular infiltration) in loose myxoid stroma (H&E stain, ×40)
Figure 4.
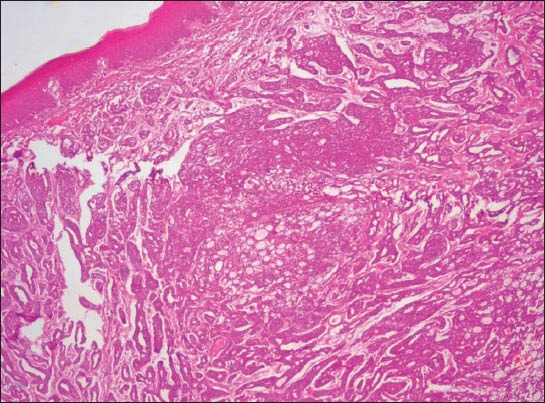
Neoplastic cells showing transformation of cords, islands and cribriform areas into solid areas and sheets within the fibrous stroma (H&E stain, ×40)
Figure 5.
Nests of cells exhibiting indistinct cytoplasmic borders and hyperchromatic nuclei. One island with cells exhibiting vesicular nucleus also seen (H&E stain, ×200)
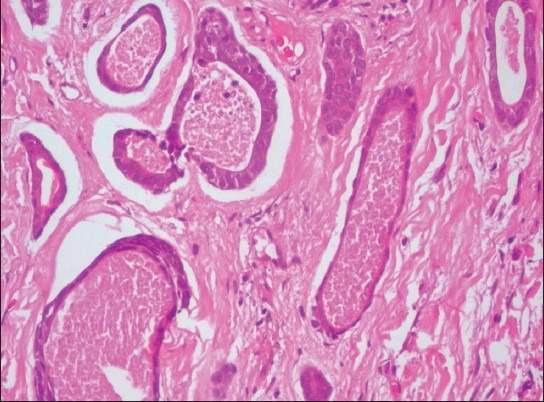
Figure 6.
Thin fibrovascular core entrapped between anastomosing cords of hyperchromatic basaloid neoplastic cells, simulating adenocarcinoma (H&E stain, ×100)
Areas of cribriform pattern [Figure 7], cords, tubules, nests and islands along with solid areas showed evidence of dedifferentiation, composed of large anaplastic cells having more amount of cytoplasm. Both hyperchromatic and vesicular nuclei with prominent nucleoli could be easily cited[Figures 8 and 9]. Typical and atypical mitotic figures were evident [Figure 10]. Some solid tumor islands also exhibited central comedo necrosis [Figure 11].
Figure 7.
Basaloid tumor cells with hyperchromatic nucleus arranged in a cribriform pattern undergoing dedifferentiation within a collagenous stroma (H&E stain, ×200)
Figure 8.
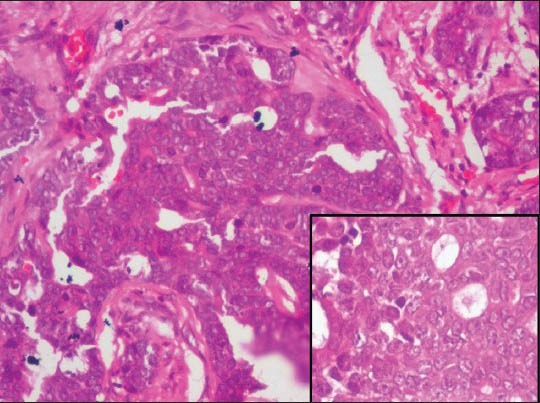
Island of tumor cells exhibiting vesicular nuclei intervened by thin fibrous septa (H&E stain ×200). Inset – high power view of tumor cells with vesiculated nuclei (H&E stain, ×400)
Figure 9.
Numerous small nests and islands of basaloid neoplastic cells arranged in loose myxoid stroma. Some solid islands show squamous metaplasia-like changes (H&E stain, ×40). Inset – Simulation of squamous eddy-like formation within tumor islands (H&E stain, ×100)
Figure 10.
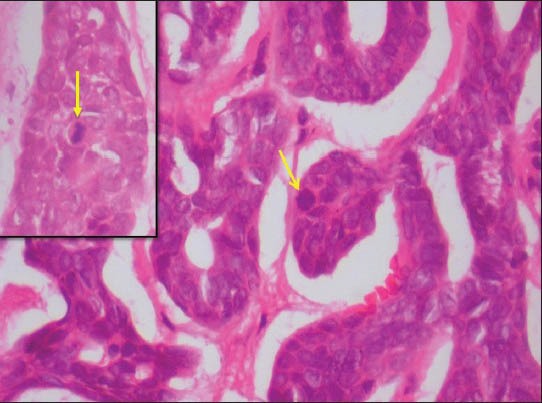
Atypical mitotic figure (arrow) seen in the tumor island (H&E stain ×400). Inset – typical mitotic figure (arrow) seen in the tumor island (H&E stain, ×400)
Figure 11.
Nests of tumor cells showing central area of comedo necrosis (H&E stain, ×200)
FINAL DIAGNOSIS
Dedifferentiated adenoid cystic carcinoma-high grade transformation
“Dedifferentiation” is defined as the abrupt transformation of a well-differentiated tumor into High grade morphology that lacks the original distinct histologic characteristics.[1] The concept of dedifferentiation was first proposed by Dahlin and Beabout in 1971.[2] Recent authors tend to preferably use the term “high grade transformation” instead of “dedifferentiation”. The conventional and high grade carcinomatous areas are clearly demarcated, although a transitional zone can be identified in some cases.
The first documentation of dedifferentiation in adenoid cystic carcinoma was done by Cheuk et al. in 1999.[1] Dedifferentiation in adenoid cystic carcinoma is associated with frequent recurrences, metastasis and rapid fatal outcome. It can occur “ab intio” or in recurrent tumors. The dedifferentiated component is usually represented by poorly differentiated adenocarcinoma, sarcomatoid carcinoma or undifferentiated carcinoma composed of anaplastic cells.[3]
In our case, classical adenoid cystic carcinoma areas comprising of ductal structures, cribriform pattern and islands of epi-myoepithelial cells were seen juxtaposed with areas of dedifferentiation exhibiting adenocarcinomatous features such as anastomosing cords of anaplastic cells, atypical mitoses, comedo necrosis and neoplastic cells with hyperchromatic and vesicular nuclei having multiple nucleoli. Hence a final diagnosis of “Dedifferentiated Adenoid cystic carcinoma” was given.
DIFFERENTIAL DIAGNOSIS
Dedifferentiated salivary gland adenocarcinomas
-
Dedifferentiated acinic cell adenocarcinoma
- The above characteristic features were not appreciated in the present case.
-
Dedifferentiated mucoepidermoid carcinoma
- Areas are characterized by multiple cystic structures with glandular formations and small nests of intermediate, mucous and few epidermoid cells
- Nuclei of the tumor cells are uniformly bland
- Such areas blend as conventional MEC areas with areas showing large anaplastic de-differentiated areas
- But in our case, dedifferentiated areas were in the form of anastomosing cords and sheets of basaloid anaplastic cells.
-
Dedifferentiated Polymorphous Low-Grade Adenocarcinoma
- Areas show variety of growth patterns – solid, cribriform, tubular and fascicular streams
- Foci of Indian file arrangement can be seen
- In our case, there was variety of growth patterns undergoing high grade transformation and lack of single file pattern. Cells showed hyperchromatic nuclei and few cells had vesicular nuclei with prominent nucleoli.
Adenocarcinomas
-
Basal cell adenocarcinoma
- Has a predominantly solid growth pattern
- Palisaded arrangement of basaloid neoplastic cells at the periphery of tumor nests seen
- Focal squamous eddy formation seen
- Two populations of cells – dark staining basaloid cells and large pale cells. Few mitoses
- In the present case areas of dedifferentiation with increased mitoses and anaplastic cells were evident.
-
Cribriform cystadenocarcinoma
- Multiple cysts separated by fibrous stroma with hemorrhage and inflammation due to rupture of cysts
- Intra-cystic papillary projections with or without delicate branching with fibrovascular cores focally is seen
- Limited areas of ductal structures or solid nests
- Our case showed predominantly solid and cribriform areas, ductal structures and areas of high grade transformation composed of anaplastic cells with basaloid morphology. Absence of intracystic papillary projections.
High grade salivary gland tumors
-
Adenocarcinoma NOS
- Several architectural patterns are appreciated like solid sheets, papillary, cystic, cribriform, cords, lobules and trabeculae
- Diverse tumor cell types including cuboidal, oval, polygonal, oncocytoid, clear cell, mucinous, sebaceous and melanoma-like cells are seen
- Tumor necrosis, perineural and vascular invasion are common
- Lacks characteristic features of other salivary gland adenocarcinomas
- Histopathologically our case showed classic areas of adenoid cystic carcinoma with cribriform, epi-myoepithelial islands and targetoid pattern. High grade areas showed anastomosing cords composed of basaloid anaplastic cells.
-
High grade Salivary duct carcinoma
- Mixture of two components: intraductal and invasive
- Roman-bridge architecture of tumor cell arranged in ductal spaces
- Central comedo necrosis in the tumor islands
- Prominent desmoplastic reaction in the invasive component
- Large pleomorphic nuclei with abundant and granular cytoplasm
- This case presented with classic areas of adenoid cystic carcinoma without any roman-bridge formation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Nagao T. “Dedifferentiation” and high-grade transformation in salivary gland carcinomas. Head Neck Pathol. 2013;7(Suppl 1):S37–47. doi: 10.1007/s12105-013-0458-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costa AF, Altemani A, Hermsen M. Current concepts on dedifferentiation/high-grade transformation in salivary gland tumors. Patholog Res Int 2011. 2011 doi: 10.4061/2011/325965. 325965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheuk W, Chan JK. Salivary gland tumors. In: Fletcher CD, editor. Diagnostic Histopathology of Tumors. 3rd ed. Vol. 1. Philadelphia: Churchill Livingstone; 2007. p. 282. [Google Scholar]
- 4.Everson JW, Nagao T. Diseases of salivary glands. In: Barnes L, editor. Surgical Pathology of Head and Neck. 3rd ed. Vol. 1. New York: Informa Healthcare USA; 2009. p. 475. [Google Scholar]


