Abstract
Objectives:
To study the effect of sleep center accreditation and Sleep Medicine board certification of physicians on patient-centered outcomes in obstructive sleep apnea (OSA).
Design:
Prospective, multicenter, comparative effectiveness study.
Setting:
Four sleep centers
Patients:
502 patients with OSA.
Interventions:
None.
Measurements and Results:
Patients at two accredited and two non-accredited centers underwent polysomnography at participating locations and completed validated questionnaires, with objective measurement of positive airway pressure (PAP) therapy adherence performed three months after therapy initiation. The proportion of patients (age 53 ± 13[SD] years; 26% women; and body mass index 33.6 ± 7.2 kg/m2) who were adherent to PAP therapy by Medicare guidelines (> 70% of nights with ≥ 4 h use over a 30-day period) was greater in accredited (79%) than non-accredited sites (64%; p = 0.004). After adjustment for confounding variables, patients who received care from accredited centers (odds ratio [OR] 2.2, 95% confidence interval [CI], 1.2-4.2; p = 0.016) and certified physicians (OR 2.3, 95% CI, 1.3-4.0; p = 0.005) were more likely to be adherent to PAP therapy than those who received care from non-accredited centers and non-certified physicians. Patient satisfaction was associated with greater education received from physician (OR 4.6; 95% CI 2.3-9.3); greater risk perception (OR 2.7; 95% CI 1.0-7.4); physician certification (OR 2.1; 95% CI 1.1-4.2); and inversely related to delays in care (OR 0.5; 95% CI 0.3-0.9; p < 0.05). Such delays were inversely related to accreditation-certification status (p < 0.0001).
Conclusions:
In patients with OSA, accreditation-certification status of sleep centers and physicians was associated with better PAP adherence, better patient education, better patient satisfaction, and greater timeliness.
Commentary:
A commentary on this article appears in this issue on page 251.
Citation:
Parthasarathy S; Subramanian S; Quan SF. A multicenter prospective comparative effectiveness study of the effect of physician certification and center accreditation on patient-centered outcomes in obstructive sleep apnea. J Clin Sleep Med 2014;10(3):243-249.
Keywords: Sleep, professional competence, obstructive sleep apnea, patient satisfaction, continuous positive airway pressure
Health care delivery in many disease conditions including obstructive sleep apnea (OSA) will be increasingly driven by quality metrics.1–3 One of the important quality metrics for OSA—adherence to positive airway pressure (PAP) therapy— remains a huge problem, with adherence of greater than four hours of daily use ranging from 46% to 83%.4,5 There is much emphasis on patient-centered care that focuses on outcomes relevant to patients such as improving patient satisfaction and enhancing the patient experience.6 We have previously shown that in a cross-sectional national survey, patients with OSA cared for by American Academy of Sleep Medicine (AASM) accredited sleep centers or Sleep Medicine board-certified physicians had lower positive airway pressure (PAP) discontinuation rates and reported greater patient satisfaction than patients cared for by non-accredited centers and non-certified physicians.7 Subsequently, Pamidi and colleagues performed a single-center retrospective chart review that demonstrated higher objective measures of PAP adherence in patients seen by a sleep specialist prior to undergoing polysomnography (PSG) than those who did not receive such sleep specialist consultation.8 Recently, a randomized controlled non-inferiority trial reported that treatment of OSA by primary care physicians was non-inferior to that of sleep specialists with regard to resolution of sleepiness, patient satisfaction, or PAP adherence.9 So far, to our knowledge, a comparative effectiveness trial, in “real-world” circumstances devoid of the artificial constraints of a randomized controlled trial, comparing the effect of both physician certification and center accreditation on clinical outcomes in patients with OSA has not been performed.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Previously, studies of the effect of physicians' board-certification status and sleep-center accreditation status on outcomes in patients with obstructive sleep apnea (OSA) have shown variable results. A prospective multi-center comparative effectiveness trial, in “real-world” circumstances devoid of the artificial constraints of a randomized controlled trial, comparing the effect of both physician certification and center accreditation on clinical outcomes in patients with OSA has so far not been performed.
Study Impact: In patients with OSA, accreditation-certification status of sleep centers and physicians was associated with better PAP adherence, better patient education, better patient satisfaction, and greater timeliness. These results suggest that health policy decisions should be directed toward care pathways involving accredited facilities and board-certified physicians.
Besides quality metrics aimed at measuring treatment adherence and resolution of symptoms, other metrics that serve as mediators are important in health promotion and chronic disease management.10 Specifically, patient education regarding their chronic disease condition can help improve risk perception and self-efficacy, and consequently serve to promote adherence to therapy and further improve health and well-being.10–13 In our previous national survey, we demonstrated that patient education and risk perception mediated the observed better PAP adherence in patients cared for by accredited centers and certified physicians, but such cross-sectional measurements may be subject to recall bias and needed to be performed in a prospective manner.7 Other important benchmarks in the management of patients with OSA such as timely delivery of care and patient satisfaction with care rendered by their physicians and centers are important patient-centric quality metrics that needed to be assessed.14
In order to address these knowledge gaps, we performed a multicenter, prospective, comparative effectiveness study involving four sleep centers (two accredited and two non-accredited) with the overall purpose of studying the effect of center accreditation and physician certification on patient-centered outcomes of OSA. We hypothesized that patients with OSA who are cared for by sleep-certified physicians or accredited centers are more likely to be adherent to PAP therapy than patients cared for by non-certified physicians and non-accredited centers. We also hypothesized that patient education regarding OSA and associated risks are provided by a greater proportion of sleep-certified physicians and accredited centers than by non-certified physicians and non-accredited centers. Lastly, we hypothesized that sleep-certified physicians and AASM-accredited centers provide more timely care and achieve greater patient satisfaction ratings than non-certified physicians and non-accredited centers.
METHODS
Participants and Centers
Consecutive patients at 4 sleep centers (2 AASM accredited and 2 non-accredited) referred with a high suspicion for OSA were approached to participate in a 3-month study that entailed a previously published and validated sleep questionnaire aimed at measuring baseline demographics and patient satisfaction.7 Exclusion criteria were: (a) age < 21 years; (b) patients with known diagnosis of OSA who were returning for a PAP titration or PAP re-titration study; (c) patients who were undergoing PSG primarily for suspicion of conditions other than OSA (such as parasomnias, narcolepsy, restless leg syndrome); and (d) cognitive impairment and inability to provide informed consent. The institutional review board approved the study and written informed consent was obtained from all participants. Of the 2 non-accredited centers, one was an urban hospital-based 4-bed academic center and the other was a suburban free-standing 4-bed non-academic center. Of the accredited centers, there was one urban hospital-based 6-bed academic laboratory and one suburban free-standing 4-bed non-academic laboratory. The centers were chosen as such to balance the effect of academic versus private affiliation, urban versus suburban location, and hospital versus free-standing facilities. All sites provided PAP support through contracted durable medical equipment companies. One of the non-accredited sites supplemented such PAP support with in-house PAP set-up by respiratory therapist.
Questionnaire Tool
Details of the questionnaire are available elsewhere.7 Briefly, patients were asked to respond “yes,” “no,” or “don't know” to the following questions: (a) whether they received adequate education from the healthcare provider about OSA in any form—verbal, audio-visual, or pamphlets; (b) whether they received adequate education about OSA from the sleep center in any form; (c) whether such education improved their understanding of OSA; (d) whether such education helped them realize the risks associated with OSA; (e) whether they received education regarding OSA from other sources; (f) whether they were satisfied with their physician's management of their OSA condition on a 5-point Likert scale that ranged from very satisfied to very dissatisfied7,15; and (g) whether they were satisfied with their sleep center's management of their OSA condition on a 5-point Likert scale. Other medical information obtained from patient self-report included demographics, nasal symptomatology, medications, insurance information, comorbid medical conditions, and Epworth Sleepiness Scale. Patients were also asked to report the time delay between the referring physician visit and PSG.
At 3 months, objective PAP adherence information was downloaded from the device and transmitted to coordinating center. Additionally, patients were queried regarding the subjective improvement in sleepiness on a Likert scale.16 Degree of improvement in subjective sleepiness was measured by a 5-point Likert scale that ranged from -1 (sleepiness is worse), 0 (no change), +1 (slightly improved), +2 (substantially improved), and +3 (completely resolved).7
Potential confounders that may affect acceptance of PAP device were also measured: PAP pressure level, device type (automatic PAP, bilevel PAP, or continuous PAP), presence and severity of nasal congestion score, age, gender, height, weight (for body mass index calculations), and highest education (did not finish high school, finished high school, college, masters, or doctorate).7 Potential confounders for timeliness in healthcare delivery such as type of health insurance (HMO, PPO, POS, Medicare, or lack of any insurance) were also requested.
Data Analysis
End-points
The primary end-point for analysis was adherence to PAP therapy as defined by Medicare criteria—specifically, the use of PAP device ≥ 4 h per night on > 70% of nights during a consecutive 30-day period anytime during the first 3 months of initial usage.17 Secondary end-points were (a) patients' perception of education they received regarding OSA, (b) patients' perception of health risks of OSA, (c) time delay in receiving PSG therapy, and (d) overall patient satisfaction of the care delivered by physician and center, measured separately.
Predictors and Confounders
In order to assess the combined “dose-effect” of sleep certification of physicians and AASM accreditation of the centers on patient outcomes, we assigned patients to 1 of 3 groups: (a) both physician and center were certified-accredited, (2) one of the two was certified-accredited, and (3) neither physician nor the center were certified-accredited. From the list of predictors and potential confounders, simple logistic regression analysis was performed to identify significant factors (independent variables) that influenced discontinuation of PAP therapy. Subsequently, we built multivariate logistic regression models with Medicare definition of PAP device adherence as the dependent variable using significant independent variables identified by univariate logistic regression analysis (p ≤ 0.10).
Multi-collinearity between independent variables was verified, and in the event of collinearity, the strongest predictor variable alone was included. Results are presented as mean and standard deviation unless otherwise specified. P values less than 0.05 were considered significant. All analysis was performed using SPSS v20.0 (IBM SPSS Inc., Armonk, NY). Unadjusted proportions were compared using Pearson χ2 test.
Power Analysis
PAP device adherence has been reported to be between 46% to 83% when defined as ≥ 4 h of daily use.4 In a previous study, we have shown a 14% difference in PAP acceptance between patients cared for by accredited and non-accredited centers.7 Based upon such information, we assumed a PAP device adherence proportion of 65% and considered a difference in PAP adherence of 14% as clinically meaningful. Therefore, a required sample size of 458 was needed to have 90% power (2-sided α) to detect a difference. Anticipating an estimated 10% attrition rate over the 3-month follow-up, we needed at least 504 participants.
RESULTS
A flow diagram outlining the recruitment is provided in Figure 1. During the recruitment period, 509 patients agreed to participate and provided informed consent. Seven of the 509 patients who gave informed consent did not have OSA and were excluded from the study (3 participants in accredited sites and 4 participants in non-accredited sites). Follow-up data were available in 487 participants with 15 participants lost to follow-up (7 in accredited and 8 in non-accredited facilities). In this real world-study, there were more certified physicians in the accredited centers (41%) than in non-accredited centers (28%; p = 0.007).
Figure 1. Flow diagram of participant recruitment and retention.
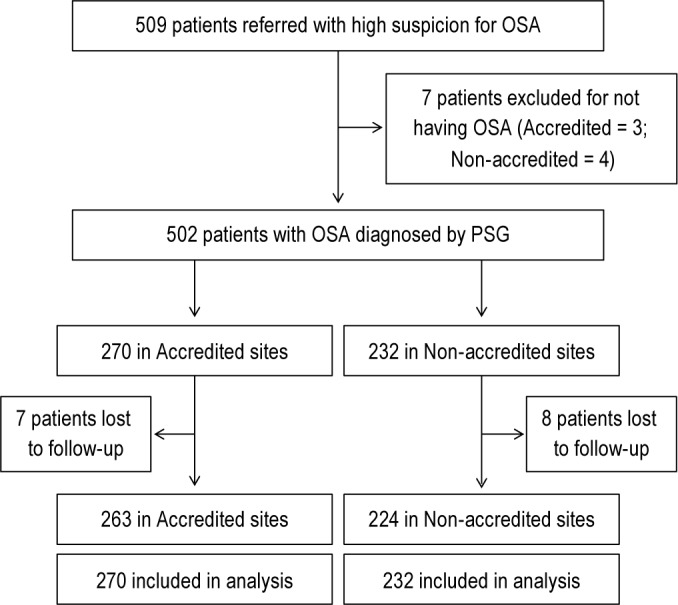
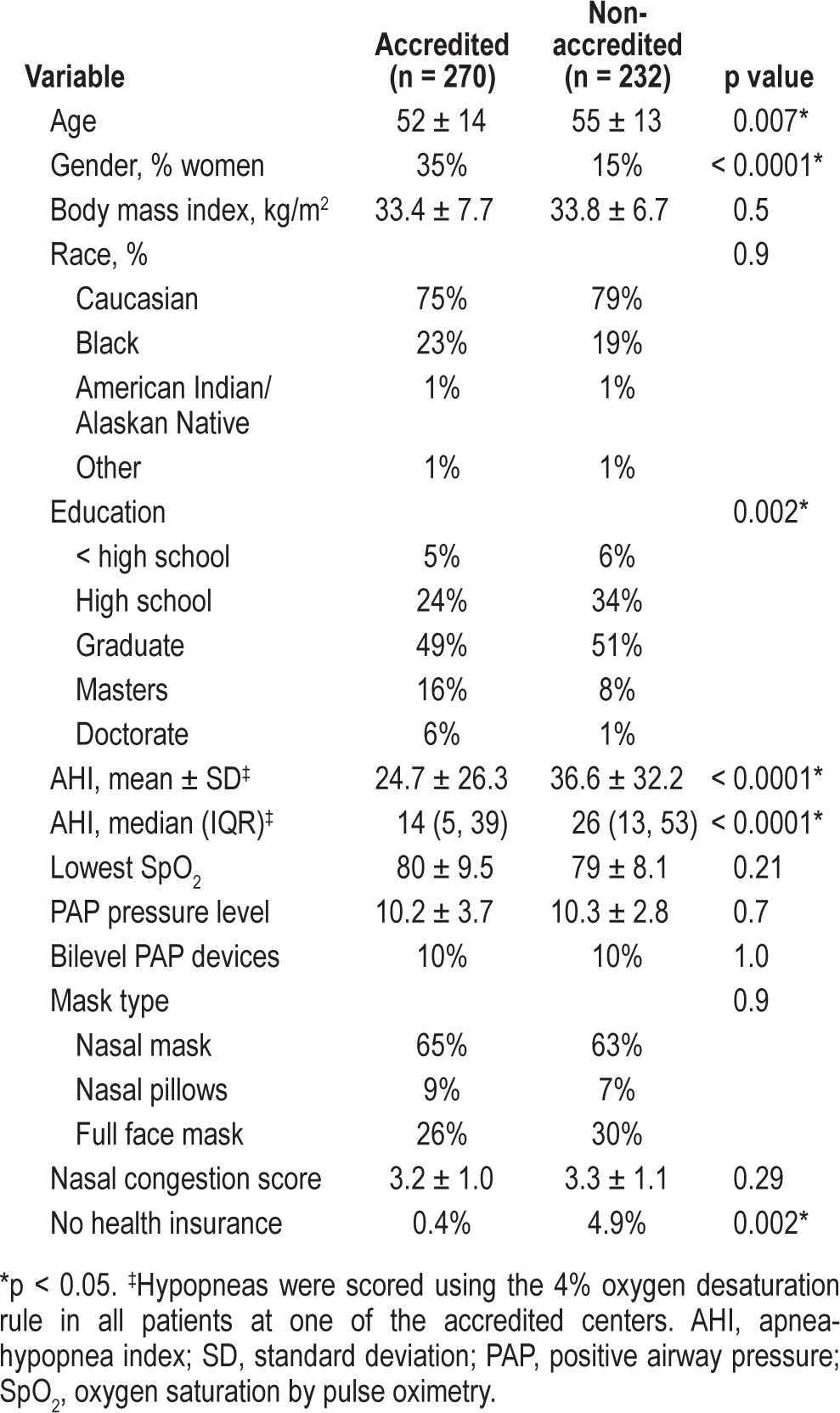
Baseline demographics of the 502 participants from the 2 accredited (n = 270) and 2 non-accredited sleep centers are shown in Table 1. Group differences in age, gender, education level, and health insurance status were observed. Differences in the apnea-hypopnea index were noted, probably attributable to one of the accredited sites having a larger proportion of patients whose PSG was scored by the 4% desaturation rule for scoring hypopneas. Notably, the lowest SpO2 was not different between the accredited and non-accredited centers (Table 1). Prescription of bilevel PAP devices was not different between accredited (10%) and non-accredited facilities (10%; p = 1.0).
Table 1.
Baseline demographics
Patient-Centered Outcomes
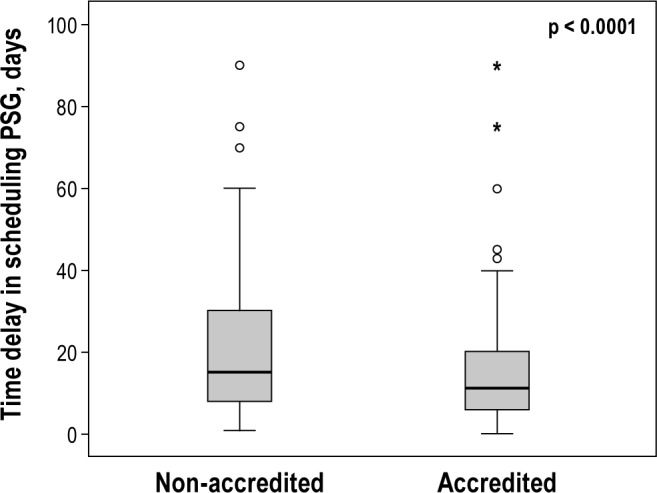
The proportion of patients adherent to PAP therapy was greater in patients cared for by accredited centers than those cared for by non-accredited centers (Table 2). Similarly, hours of PAP device use were greater in patients who received care at accredited centers than non-accredited centers (Table 2). When compared to patients at non-accredited centers, patients at accredited centers had shorter time delays for PSG (Figure 2), greater self-reported education from referring physicians and sleep center staff, better understanding about OSA, greater perception of risk of OSA, and were more likely to seek education regarding OSA from other sources (Table 2). Patient ratings of satisfaction with sleep centers were comparable between accredited and non-accredited centers. Patient ratings of satisfaction with physicians was greater for certified than non-certified physicians (unadjusted odds ratio [OR] 2.4; 95% CI 1.4-4.2). Similarly, patients rated a greater proportion of certified physicians (91%) as delivering satisfactory education regarding OSA than non-certified physicians (84%; p = 0.042). Participants reported experiencing similar improvements in sleepiness over a 3-month period in both accredited and non-accredited sites (Table 2). As expected, the Likert scores for improvement in sleepiness were directly related to daily use of PAP therapy (R2 = 0.39; p < 0.0001).
Table 2.
Patient-related outcomes
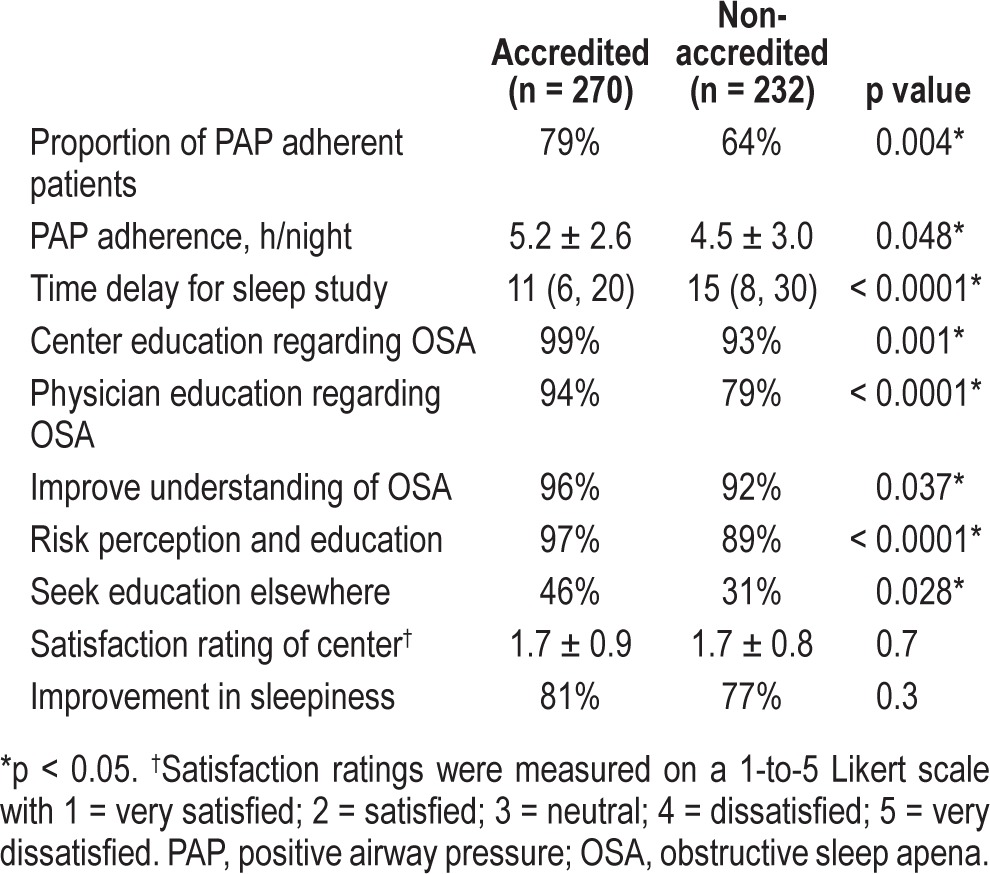
Figure 2. Time delay from referral to polysomnography (PSG) in non-accredited facilities was greater than that in accredited facilities (p < 0.0001).
Accredited and non-accredited sites were served by both sleep medicine board-certified physicians and physicians without such certification. Therefore, we categorized patients by both center accreditation and physician certification status to yield 3 groups: (a) patients cared for by an accredited center and certified physician, (b) either the center or physician was accredited or certified, or (c) neither the center nor physician was accredited or certified (Table 3). The proportion of patients who were PAP adherent was related to accreditation-certification status in a dose-dependent manner: lack of accreditation and certification (none; 59% adherent) less than either accredited center or certified physician (either; 75%), or both being accredited and certified (both; 78% p = 0.004; Table 3).
Table 3.
Proportion of patients who were adherent to PAP therapy*

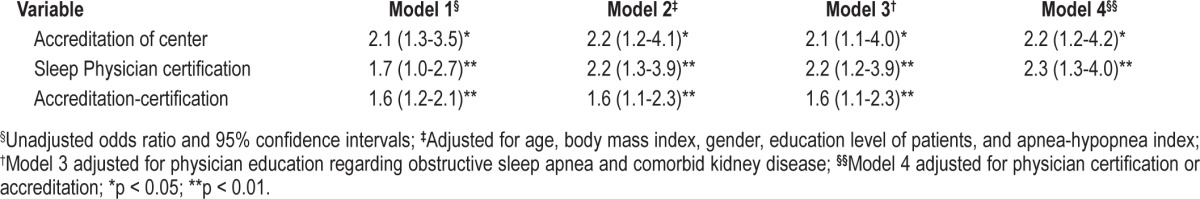
Univariate logistic regression analysis revealed the following variables that were associated with PAP adherence: accreditation of center, certification status of physician, combination of both accreditation-certification status of the provider and center, higher education level of participants, greater AHI, and greater education received from physician regarding OSA (Table 2). The presence of kidney disease was associated with lower PAP adherence (Table 4). Interestingly, health insurance status, nasal congestion scores, and medications for nasal symptoms were not associated with PAP adherence. Multivariate logistic regression models built to adjust for confounders revealed that objective PAP adherence was associated with physician certification, center accreditation status, or a combination of both in a dose-dependent manner (Table 5). Center characteristics such as academic versus non-academic, urban versus suburban, and hospital versus free-standing centers did not affect PAP adherence (all OR 0.78; 95% CI 0.38-1.61; p = 0.5).
Table 4.
Unadjusted odds ratios of determinants of PAP adherence
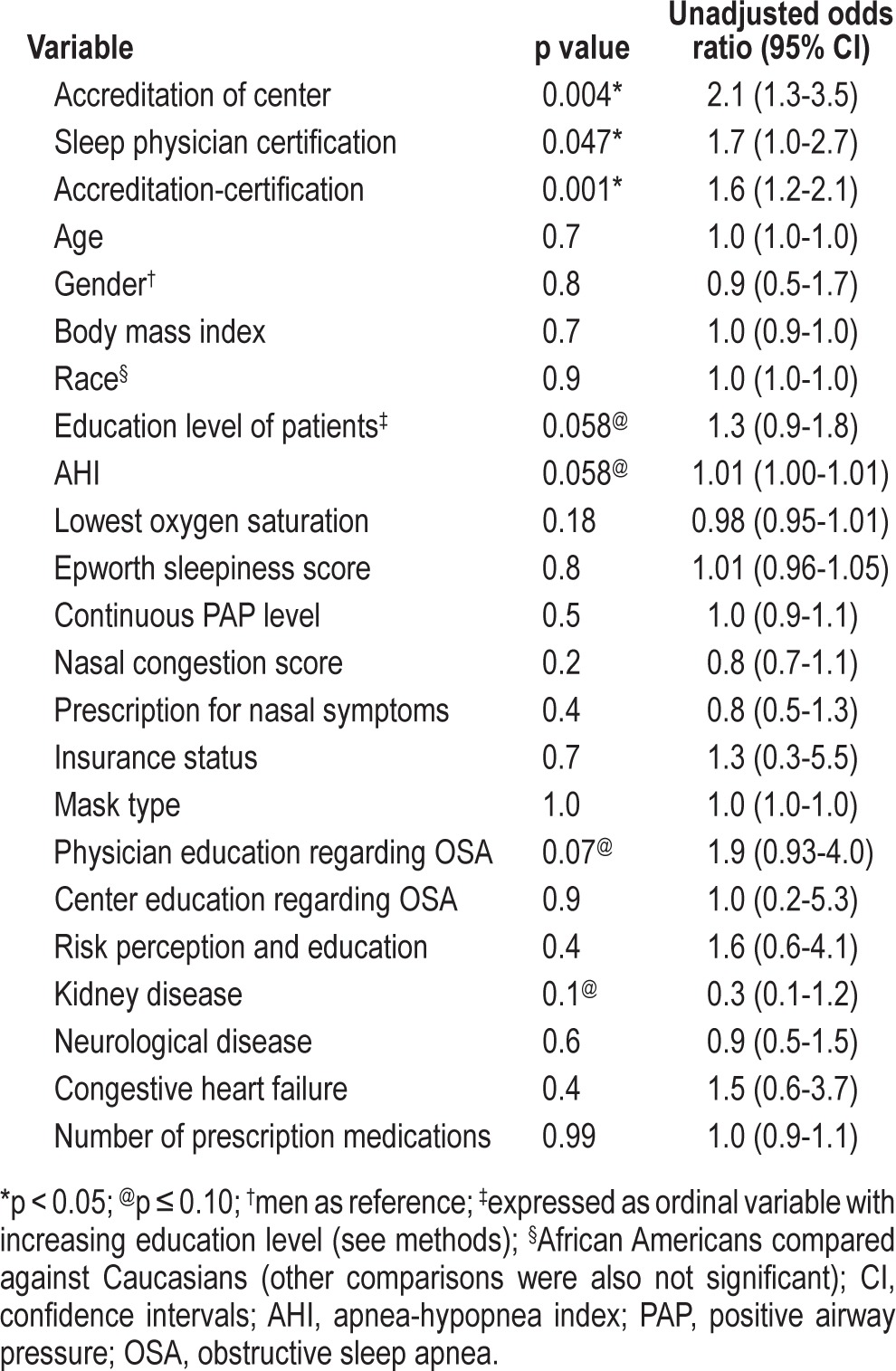
Table 5.
Adjusted odds ratios of determinants of PAP adherence
Patient Satisfaction and Timeliness of Care
Patient satisfaction was associated with greater education received from physician (OR 4.6; 95% CI 2.3-9.3; p < 0.0001), greater risk perception of OSA (OR 2.7; 95% CI 1.0-7.4; p = 0.049), and physician certification (OR 2.1; 95% CI 1.1-4.2), and inversely related to > 30-day delay for PSG (OR 0.5; 95% CI 0.3-0.9; p = 0.03). Patient satisfaction ratings of sleep centers were not different between accredited and non-accredited centers (Table 2).
Timeliness of care—time delay between the first sleep study and when the patient received the PAP device—was 24 ± 35 days (median 14 days; interquartile range 7, 30) for the entire cohort. Time delays were shorter in accredited centers than non-accredited centers (Table 2 and Figure 2). Timeliness of care was not related to insurance status (p = 0.3). The direct referrals in accredited centers (44%) were not different than those in non-accredited centers (42%; p = 0.9). Also, the proportion of split-night studies in accredited centers (18%) was not different than that in non-accredited centers (21%; p = 0.43; χ2 test). In a multiple regression model, time delay was inversely related to accreditation-certification status of center and physician (OR 0.58; 95% CI 0.45-0.75; p < 0.0001).
Internal and External Validity
Besides the internal consistency of the components of the questionnaire presented in our previous publication,7 we further checked the data for internal and external validity. In order to assess the internal validity, we correlated daily PAP use versus self-reported improvement in sleepiness. In our study, the Likert scores for improvement in sleepiness were related to daily use of PAP therapy (R2 = 0.39; p < 0.0001). The demographic characteristics of our patient population are very similar to those reported in other large series involving patients with OSA (external validity).7,18,19 Furthermore, the prescription of bilevel PAP devices was similar to that in a previous report.20
DISCUSSION
Some general observations can be made about our study. First, after adjusting for baseline differences and other confounding variables, AASM accreditation and Sleep Medicine certification status of physicians and sleep centers are associated with greater adherence to PAP therapy than non-certified physicians and non-accredited centers in real-world conditions (Table 5). Patient education regarding OSA was independently associated with better PAP adherence, increased risk perception regarding OSA, and physician certification, which together may have mediated the favorable effect of accreditation-certification on PAP adherence. While time delays were shorter in accredited than non-accredited centers, patient satisfaction with sleep centers was comparable between accredited and non-accredited facilities. However, patient satisfaction with physicians was strongly and directly associated with education received from the physician, better risk perception as it pertains to OSA, and physician certification status, and inversely related to time delays in obtaining PSG.
Efficacy, Effectiveness, and Health Policy
To our knowledge, this is the first multicenter prospective comparative effectiveness study performed in the real-world setting to show favorable effects of physician certification and center accreditation on objective PAP adherence in patients with OSA. A recent multicenter randomized controlled trial did not find a difference in PAP adherence between care rendered by sleep specialists versus primary care physicians in patients with OSA.9 In this efficacy study, controlled multiple educational interventions were delivered to sufficiently train nurses and primary care physicians who then managed patients in a well-controlled and protocolized manner that resulted in non-inferior results compared to sleep specialists.9 However, in our effectiveness study, we conducted our study in the real-world setting with typical interventions delivered by regular staff members without any special educational intervention administered to health care providers. Such differences between controlled trials and comparative effectiveness studies are important translational elements in health services research that bear much import to outcomes research and public health relevance.21 Specifically, comparative effectiveness studies such as ours need to be done first to better understand the current differences in provider training (or specialization) on patient outcomes in OSA. Subsequently, the educational intervention administered to primary care physicians and nurses found to be promising in the efficacy study by Chai-Coetzer and colleagues can be tested in the real-world setting in a comparative effectiveness trial before such data are used to influence public health policy. This is because successful efficacy studies do not necessarily translate into similar outcomes in effectiveness trials because of issues related to reach, adoption, implementation, and maintenance of such educational interventions directed at providers.22,23 Additionally, we cannot exclude the fact that differences in the US and Australian health care systems may have contributed to the observed differences.9
Accreditation of health service systems is widely considered to be a driver of quality.24 However, the effect of such accreditation on healthcare quality is stated to be uncertain and warranting more study.25 Our study is highly responsive to such a call. Physician certification in a specialty is also felt to be result in better health outcomes. For example, physician certification in cardiology has been associated with better metrics, such as reduced hospital readmission and better health-related quality of life in disease management of heart failure.26 Our current report adds to the body of literature that emphasizes the favorable effect of physician certification and training on patient-centered outcomes in OSA.7,8,27–29
Patient Education
Health promotion research in individuals with chronic disease—such as OSA—requires sufficient education to be imparted to patients to help improve self-efficacy, risk perception, and treatment adherence.12,13,30 Such educational interventions directed at patients may have played a role in previous findings of better PAP adherence in OSA patients managed by specialists.7,8 Specifically, in patients with OSA being treated by PAP therapy, Weaver and colleagues demonstrated that three major cognitive factors play a role in adherence to PAP therapy—the patient's perception of health risk associated with OSA, the patient's expectations of outcomes, and the patient's perceived ability to use the PAP device.13 All three of these factors can be favorably influenced by interventions that can deliver adequate patient education.31,32 In our previous study, patient education leading to better patient perception of risk due to OSA was associated with better PAP adherence.7 In our current study, better education delivered by certified physicians was associated with improved objective measure of PAP adherence. This is in agreement with other investigations showing the beneficial effect of intensive education on adherence to PAP therapy.33
Patient Satisfaction and Time Delays
Patient satisfaction was associated with greater education received from physician, greater risk perception of OSA, and physician certification status, and inversely related to delays in undergoing PSG. These findings are consistent with other reports that identify access to care and physician communication as important determinants of patient satisfaction.7,34 In light of this information, the sleep community and health care systems need to be mindful of their wait times (Figure 2). Contrary to our previous report, patient satisfaction ratings of sleep centers were not different between accredited and non-accredited facilities. We are unable to explain the lack of such a difference, although it is possible that patients attribute their satisfaction with health care delivery to physicians rather than systems. Alternatively, our study was probably not powered to detect such a difference in satisfaction ratings. For the same reason, we believe that we did not notice differences in resolution of symptoms. Power analysis for a sample size required to detect resolution of sleepiness may be much larger in studies of OSA that have an active control (PAP therapy) arm.35 Unlike our previous study, nasal congestion and therapy for nasal congestion was not associated with PAP adherence. The reasons for such lack of effect are unclear.
One possible limitation to this study is that lack of blinding among the centers and physicians could have resulted in a change in practice. However, accredited and non-accredited centers were equally aware that this study was being performed. If practice was favorably altered, it would have either non-differentially altered the results (both groups changing equally) or biased the results towards the null (the accredited centers changing less because their practices were already favorable, thus narrowing the difference). Thus, we do not believe that our results were altered by the lack of blinding in the study.
In conclusion, we have demonstrated under real-world conditions that AASM sleep center accreditation and Sleep Medicine board certification are important determinants of patient-centered quality metrics such as adherence to PAP therapy, patient satisfaction, patient education, and timeliness of care delivery. These results suggest that health policy decisions should be directed toward care pathways involving accredited facilities and board-certified physicians.36
DISCLOSURE STATEMENT
This study was funded by the American Sleep Medicine Foundation (ASMF). The funding institution had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Peer review of the grant application was through an independent process overseen by the ASMF. Dr. Parthasarathy received funding from HL095748 during the writing of this manuscript. He has also received research support and honorarium from Philips Respironics. Dr. Quan has received consulting fees from Saatchi and Saatchi to develop a sleep screening questionnaire. He is the Editor in Chief of Journal of Clinical Sleep Medicine. Dr. Subramanian has indicated no financial conflicts of interest.
REFERENCES
- 1.Daschle T, Domenici P, Frist W, et al. Prescription for patient-centered care and cost containment. New Engl J Med. 2013;369:471–4. doi: 10.1056/NEJMsb1306639. [DOI] [PubMed] [Google Scholar]
- 2.Strollo PJ, Jr., Badr MS, Coppola MP, et al. The future of sleep medicine. Sleep. 2011;34:1613–9. doi: 10.5665/sleep.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strollo PJ, Metersky M, Berry RB, et al. Obstructive sleep apnea: physician performance measurement set. American Medical Association and National Committee for Quality Assurance; 2008. [Google Scholar]
- 4.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Medicare & Medicaid Services. Physician Quality Reporting System. [Accessed September 10, 2013]. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/index.html.
- 6.Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA. 2012;307:1583–4. doi: 10.1001/jama.2012.500. [DOI] [PubMed] [Google Scholar]
- 7.Parthasarathy S, Haynes PL, Budhiraja R, et al. A national survey of the effect of sleep medicine specialists and American Academy of Sleep Medicine Accreditation on management of obstructive sleep apnea. J Clin Sleep Med. 2006;2:133–42. [PubMed] [Google Scholar]
- 8.Pamidi S, Knutson KL, Ghods F, et al. The impact of sleep consultation prior to a diagnostic polysomnogram on continuous positive airway pressure adherence. Chest. 2012;141:51–7. doi: 10.1378/chest.11-0709. [DOI] [PubMed] [Google Scholar]
- 9.Chai-Coetzer CL, Antic NA, Rowland LS, et al. Primary care vs specialist sleep center management of obstructive sleep apnea and daytime sleepiness and quality of life: a randomized trial. JAMA. 2013;309:997–1004. doi: 10.1001/jama.2013.1823. [DOI] [PubMed] [Google Scholar]
- 10.Schmittdiel J, Mosen DM, Glasgow RE, et al. Patient Assessment of Chronic Illness Care (PACIC) and improved patient-centered outcomes for chronic conditions. J Gen Intern Med. 2008;23:77–80. doi: 10.1007/s11606-007-0452-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aloia MS, Arnedt JT, Stepnowsky C, et al. Predicting treatment adherence in obstructive sleep apnea using principles of behavior change. J Clin Sleep Med. 2005;1:346–53. [PubMed] [Google Scholar]
- 12.Stepnowsky CJ, Palau JJ, Gifford AL, et al. A self-management approach to improving continuous positive airway pressure adherence and outcomes. Behav Sleep Med. 2007;5:131–46. doi: 10.1080/15402000701190622. [DOI] [PubMed] [Google Scholar]
- 13.Weaver TE, Maislin G, Dinges DF, et al. Self-efficacy in sleep apnea: instrument development and patient perceptions of obstructive sleep apnea risk, treatment benefit, and volition to use continuous positive airway pressure. Sleep. 2003;26:727–32. doi: 10.1093/sleep/26.6.727. [DOI] [PubMed] [Google Scholar]
- 14.NCQA. Washington, DC: 2011. National Quality Measures Clearinghouse; Health plan members' satisfaction with care: adult health plan members' ratings of their health plan. HEDIS 2012: Healthcare Effectiveness Data and Information Set. Vol. 1, narrative. http://www.qualitymeasures.ahrq.gov/content.aspx?id=34709&search=cahps+survey+version+34704.34700. [Google Scholar]
- 15.Otani K, Harris LE, Tierney WM. A paradigm shift in patient satisfaction assessment. Med Care Res Rev. 2003;60:347–65. doi: 10.1177/1077558703254865. [DOI] [PubMed] [Google Scholar]
- 16.Weaver TE. Outcome measurement in sleep medicine practice and research. Part 1: assessment of symptoms, subjective and objective daytime sleepiness, health-related quality of life and functional status. Sleep Med Rev. 2001;5:103–28. doi: 10.1053/smrv.2001.0152. [DOI] [PubMed] [Google Scholar]
- 17.Noridan Healthcare Solutions. Positive Airway Pressure (PAP) Devices FAQs. [Accessed July 6, 2011]. https://www.noridianmedicare.com/dme/news/faq/pap_devices.html%3f.
- 18.Punjabi NM, Bandeen-Roche K, Marx JJ, et al. The association between daytime sleepiness and sleep-disordered breathing in NREM and REM sleep. Sleep. 2002;25:307–14. [PubMed] [Google Scholar]
- 19.Chervin RD, Aldrich MS. The relation between multiple sleep latency test findings and the frequency of apneic events in REM and non-REM sleep. Chest. 1998;113:980–4. doi: 10.1378/chest.113.4.980. [DOI] [PubMed] [Google Scholar]
- 20.Parthasarathy S, Habib M, Quan SF. How are automatic positive airway pressure and related devices prescribed by sleep physicians? A web-based survey. J Clin Sleep Med. 2005;1:27–34. [PubMed] [Google Scholar]
- 21.Parthasarathy S. CON: thoughtful steps informed by more comparative effectiveness research is needed in home testing. J Clin Sleep Med. 2013;9:9–12. doi: 10.5664/jcsm.2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glasgow RE, Lichtenstein E, Marcus AC. Why don't we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93:1261–7. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Committee on Quality of Health Care in America, Institute of Medicine. Washington, DC: National Academies Press; 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. [Google Scholar]
- 24.Braithwaite J, Westbrook J, Pawsey M, et al. A prospective, multi-method, multi-disciplinary, multi-level, collaborative, social-organisational design for researching health sector accreditation [LP0560737] BMC Health Serv Res. 2006;6:113. doi: 10.1186/1472-6963-6-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hinchcliff R, Greenfield D, Moldovan M, et al. Narrative synthesis of health service accreditation literature. BMJ Qual Saf. 2012;21:979–91. doi: 10.1136/bmjqs-2012-000852. [DOI] [PubMed] [Google Scholar]
- 26.Philbin EF, Weil HF, Erb TA, et al. Cardiology or primary care for heart failure in the community setting: process of care and clinical outcomes. Chest. 1999;116:346–54. doi: 10.1378/chest.116.2.346. [DOI] [PubMed] [Google Scholar]
- 27.Lu B, Budhiraja R, Parthasarathy S. Sedating medications and undiagnosed obstructive sleep apnea: physician determinants and patient consequences. J Clin Sleep Med. 2005;1:367–71. [PubMed] [Google Scholar]
- 28.Scharf SM, DeMore J, Landau T, et al. Comparison of primary-care practitioners and sleep specialists in the treatment of obstructive sleep apnea. Sleep Breath. 2004;8:111–24. doi: 10.1007/s11325-004-0111-6. [DOI] [PubMed] [Google Scholar]
- 29.Collop NA, Anderson WM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2007;3:737–47. [PMC free article] [PubMed] [Google Scholar]
- 30.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 31.Richards D, Bartlett DJ, Wong K, et al. Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep. 2007;30:635–40. doi: 10.1093/sleep/30.5.635. [DOI] [PubMed] [Google Scholar]
- 32.Aloia MS, Di Dio L, Ilniczky N, et al. Improving compliance with nasal CPAP and vigilance in older adults with OAHS. Sleep Breath. 2001;5:13–21. doi: 10.1007/s11325-001-0013-9. [DOI] [PubMed] [Google Scholar]
- 33.Haynes RB. Introduction. In: Haynes RB, Taylor DW, Sackett DL, editors. Compliance in Health Care. Baltimore: Johns Hopkins University Press; 1979. [Google Scholar]
- 34.Landon BE, Zaslavsky AM, Bernard SL, et al. Comparison of performance of traditional Medicare vs Medicare managed care. JAMA. 2004;291:1744–52. doi: 10.1001/jama.291.14.1744. [DOI] [PubMed] [Google Scholar]
- 35.Parthasarathy S, Wendel C, Haynes PL, et al. A pilot study of CPAP adherence promotion by peer buddies with sleep apnea. J Clin Sleep Med. 2013;9:543–50. doi: 10.5664/jcsm.2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Noridian Healthcare Solutions. Local Coverage Determination (LCD) for Positive Airway Pressure (PAP) Devices for the Treatment of Obstructive Sleep Apnea (L171) 2012. [Accessed September 14, 2013]. https://www.noridianmedicare.com/dme/coverage/docs/lcds/current/positive_airway_pressure_pap_devices_for_the_treatment_of_obstructive_sleep_apnea.htm.


