Abstract
Objective
The purpose of this study was to examine the quality of coping skills as a predictor of change in depressive symptoms surrounding a series of naturally occurring stressors.
Method
A total of 213 undergraduate students completed study measures surrounding 3 stressors (involving 6 assessments per participant). Primary analyses focused on occasions of disappointing exam performance.
Results
Consistent with expectations, coping skill quality was predictive of more adaptive responses (i.e., less depressive symptom reactivity), with this relation being particularly strong among participants with high initial levels of depressive symptoms and on occasions when participants had a marked worsening of mood. The quality of skills used in coping with specific stressors continued to predict depressive symptom reactivity after controlling for a one-time measure of coping skill quality.
Conclusions
Our results support the importance of both stressor-specific coping skill quality and consideration of key contextual factors in understanding depressive symptom reactivity surrounding stressors.
Keywords: coping, depressive symptoms
A substantial body of research has documented that the use of some coping strategies is associated with better psychological adjustment and superior physical health (Taylor & Stanton, 2007). In a recent meta-analysis, Aldao, Nolen-Hoeksema, and Schweizer (2010) reported that, across clinical and nonclinical samples, strategies involving problem solving and cognitive reappraisal were associated with fewer depressive symptoms. While researchers have recently focused on skill development among psychotherapy clients (Strunk, DeRubeis, Chiu, & Alvarez, 2007), relatively little is known about whether (or under what conditions) these skills are normally useful to people (who are not psychotherapy clients) coping with depressive symptoms that arise in response to everyday stressors.
In this article, we examined whether variability in coping skills predicts depressive symptom reactivity (i.e., the extent of symptom worsening vs. improvement) in the wake of a series of commonplace stressors, namely, receipt of disappointing exam grades in a college class. We focused on depressive symptom reactivity over several days as we suspect the effects of coping skill use would likely occur over this relatively short interval. We further examined two potentially important contextual factors: depressive symptom severity and the degree to which stressors were associated with an affective reaction. We expected these skills would be more strongly predictive of depressive symptom reactivity among those with greater depressive symptom severity. In addition, as the use of coping skills has been proposed to be most beneficial on occasions when a notable affective shift has occurred (Beck, 1995), we expected coping skills to be more strongly related to depressive symptom reactivity on occasions involving these more marked affective reactions. Finally, we compared the predictive validity of skills assessed in the context of recurrent naturalistic stressors with a more commonly used one-time skill assessment method.
Measuring Coping Skills
Although various measures of coping skills exist, the Ways of Responding Inventory (WOR; Barber & DeRubeis, 1992) is well-suited to our purpose because it uses an open response format that is easily adapted to assess stressor-specific coping. The WOR presents participants with a series of challenging hypothetical situations (e.g., experiencing the sudden end of a relationship) and asks them to describe how they would cope with each situation. Using a manual, trained coders rate respondents’ descriptions according to the degree to which responses are consistent with adaptive coping strategies (e.g., considering evidence relevant to re-evaluation of an initial thought or generating a specific plan to cope). This rating procedure generates two summary scores: a total score and an overall quality score. The WOR Total score reflects the relative frequency of response segments deemed to be positive or negative (see Appendix for details), whereas the WOR Quality score reflects the overall quality of participants’ responses to each WOR scenario. Unlike the total score, quality scores are not constrained by the length of responses. With quality scores, raters can identify a single very positive response as reflecting more adaptive coping than two slightly positive responses. For this reason, we chose WOR quality scores as our primary coping measure.
While the WOR was developed to measure skills taught in cognitive therapy (CT; Beck, Rush, Shaw, & Emery, 1979), there is evidence to suggest that meaningful variability in these skills exists among people who have learned coping skills naturalistically. In a college student sample, Barber and DeRubeis (1992) found a moderate relationship between better coping scores on the WOR and lower depressive symptoms. In a study of smokers, those with a history of depression reported poorer coping skills on the WOR than those without a history of depression (Haaga, Thorndike, Freedman-Wheeler, Pearlman, & Wernicke, 2004). Thus, meaningful variability in coping skills has been evident even among those who have not participated in CT.
Although coping skills have been related to changes in depressive symptoms, it is unclear how well the WOR predicts coping with specific everyday stressors. Strunk and colleagues (2007) found that WOR scores were remarkably unrelated to a measure of the extent to which CT clients independently practiced using coping skills outside of therapy sessions. This finding has led us to wonder how well the WOR predicts respondents’ responses to real stressors. Compared with the WOR’s reliance on hypothetical situations, we suspected the assessment of coping following actual life events might provide a more precise estimate of coping skills as they are used. To the extent that the WOR does predict the use of coping skills in response to these stressors, the validity of the WOR would be supported. To the extent that use of coping skills in response to specific stressors is not well captured by the WOR, additional assessment strategies may be needed to capture individual differences in the use of coping skills.
Coping Skills in Context: Depressive Symptoms and Affective Reactions
Beyond examining whether coping skills are related to depressive symptom reactivity overall, we planned to examine two potentially important contextual factors: depressive symptom severity and the extent of affective reactions associated with a stressor. Aldao and colleagues (2010) found that the relation of coping strategy use and symptoms was stronger in clinical samples as compared with nonclinical samples-a finding that might be attributable to the higher symptom severity of clinical samples. With this in mind, we hypothesized that coping skills would be more consequential among those with greater depressive symptom severity.
With regard to the strength of affective reactions as a possible contextual factor, we suspected that the extent to which one uses coping skills on occasions when stressors are accompanied by affective shifts is likely to be particularly important in determining the degree of depressive symptom reactivity on those occasions. Within the CT model, therapists emphasize the use of coping skills shortly after a mood shift occurs (Beck, 1995). As affective shifts are thought to identify periods in which emotionally salient thoughts have occurred, we expect the potential benefits of using coping skills to be of greater consequence on these occasions.
Purpose
The purpose of this study was three-fold. First, we sought to examine coping skills as a predictor of depressive symptom reactivity to recurring stressors (i.e., disappointing performance on college exams). To capture the putative effects of coping skills over the time period over which we expected these skills to exert their effects, we examined change in depressive symptoms surrounding specific stressors (prior to and days after each stressor). Second, we examined two contexts in which we suspect coping skills may be of greater consequence: (a) among participants with higher initial depressive symptoms and (b) on occasions where stressors are associated with greater changes in affect. We expected that use of coping skills would be more strongly related to depressive symptom reactivity both among those with higher initial depressive symptoms and for stressors associated with larger changes in affect. Finally, we compared a general assessment of coping skills using the WOR with our measure of stressor-specific coping (inspired by the WOR) to assess how participants coped with particular stressors.
Methods
Participants
A total of 213 undergraduate students participated in this study in return for extra credit. These participants were selected for inclusion in this study on the basis of their having received at least one exam grade that was lower than their stated goal grade for an exam. This sample was largely female (81.6%; n = 173) and Caucasian (79.8%, n = 170). Minority group representation was as follows: African American (8.9%, n = 19), Hispanic (3.8%, n = 8), Asian (3.8%, n = 8), or another ethnicity (3.8%, n = 8). The average age was 20.5 years old (standard deviation [SD] = 1.7).
Measures
Patient Health Questionnaire-9 (PHQ)
The PHQ (Kroenke & Spitzer, 2002) was used to assess initial depressive symptom severity. The PHQ is a nine-item self-report questionnaire that assesses the severity of symptoms of major depressive disorder (MDD) over the past 2 weeks in accord with Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994) criteria. Because of concerns raised by our Institutional Review Board, the item assessing suicidal ideation was removed – leaving eight items. To adjust scores for this missing item, total scores were calculated by multiplying the average of the scores for the eight items administered by 9. Scores on the PHQ can range from 0 to 27, with scores of 10 or greater indicating probable diagnosis of MDD (Kroenke & Spitzer).
Modified Beck Depression Inventory (MBDI)
We modified the Beck Depression Inventory-Second Edition (BDI-II; Beck, Steer, & Brown, 1996) to assess depressive symptom reactivity in this study. Whereas the BDI-II asks respondents to report on depressive symptoms in the past 2 weeks, the MBDI asks about the past 3 days. As we did for the PHQ, we did not administer the item assessing suicidal ideation but adjusted our total scores to range from 0 to 63.
WOR
The WOR (Barber & DeRubeis, 1992) assesses cognitive and behavioral coping skills thought to be important in regulating emotional reactions (Barber, 1990). For each of six hypothetical stressful situations (e.g., a relationship ending), participants read about the situation and are presented with some initial thoughts they are asked to imagine having (e.g., “Relationships never turn out well for me”). Participants are then asked to report any further thoughts they have about the situation and what they would do at that point.
Following approximately 20 hours of training, three raters (the authors) provided ratings of participants’ WOR responses using procedures described by Barber and DeRubeis (1992; for full details, see Supplement A). The primary measure of coping skills used in this study was the WOR Quality score, which is rated on a 7-point scale ranging from 1 (likely to worsen one’s mood and situation) to 7 (likely to improve one’s mood and situation), with a score of 4 reflecting a neutral response. The intraclass correlation coefficient (ICC) of average WOR Quality ratings provided for each protocol, corrected for three raters, was .97.
WOR – Stressor-Specific Version (WOR-S)
Rather than using the WOR approach of providing hypothetical scenarios and initial thoughts, the WOR-S asks participants to report on their thoughts and behaviors following a real event. We created the WOR-S for this study to assess coping skills participants used when they received their last exam grade. Participants’ responses were coded for coping skill categories and the overall quality of the coping response using the same procedure described for the WOR. The ICC for the Quality ratings for the WOR-S, corrected for three raters, was .81.
Positive and Negative Affectivity Schedule (PANAS) and Positive and Negative Affectivity Schedule – Modified (PANAS-M)
The PANAS (Watson, Clark, & Tellegen, 1988) measures positive and negative affectivity by having respondents rate 10 positive and 10 negative emotions on a 5-point scale ranging from 1 (very slightly) to 5 (extremely) according to how they feel at the present moment. The modified version instructed respondents to rate each emotion according to how they felt immediately after receiving their exam grade. The modified version was used to assess participants’ affective responses to receiving their exam grades, and the original version was used to control for participants’ level of affect prior to each exam.
Exam grades, performance relative to goals, and outcome importance
Prior to taking each exam, participants provided their goal grade. To assess participants’ exam performance relative to their goal, difference scores between actual and goals grades were calculated for each exam with negative values reflecting disappointing exam performances. Finally, students were asked to rate the importance of doing well in the course using a 7-point scale ranging from 1 (not important at all) to 7 (very important).
Procedures
All measures were completed online over the course of three periods (A, B, and C), with each period involving two consecutive assessment points (before and after each of three exams in participants’ psychology courses). Thus, there were a total of six assessments over the course of a 10-week academic term. Times 1, 3, and 5 occurred 1 week prior to the first, second, and final exams, respectively. At each of these times, participants provided their goal grade on the upcoming exam, indicated course importance, and completed the PANAS. Times 2, 4, and 6 occurred 3 days after participants received their grade on each exam. At each of these times, participants completed the WOR-S and PANAS-M. The PHQ and WOR were completed at Time 1 only. Participants completed the MBDI at all time points.
Data Analysis
Because of missing data, the sample size varies across periods as follows: for Period A (Time 1 and 2), n = 139; for Period B (Time 3 and 4), n = 177; and for Period C (Time 5 and 6) n = 157. For analyses relying on Time 1 data not specific to the Period A stressor (e.g., initial PHQ scores), the sample size is larger (n = 213) than that available for Period A as we included all participants who reported at least one exam grade that was lower than their stated goal grade. To examine the effect of missing data, we created a variable to reflect the number of missing periods (ranging from 0 to 2). While our model allows incomplete data across periods, the model requires complete data within a given period. The number of missing periods was not significantly associated with initial depressive symptom severity (rs= .02, p = .8) or WOR score (rs = .05, p = .5).
A series of repeated measures regression analyses (without specification of random effects) were conducted using SAS Proc Mixed (Littell, Milliken, Stroup, & Wolfinger, 1996). In these analyses, the relationship between coping skills and depressive symptoms after receipt of exam grades was examined using data across periods in a single overall test. For each analysis, the dependent variable was a vector of MBDI scores from Times 2, 4, and 6 with a vector of MBDI scores from Times 1, 3, and 5 serving as a covariate. Separate repeated measures regression models were performed using the WOR-S and WOR as independent variables. Interactions of the WOR-S and WOR with the PANAS-M and PHQ were also explored. Significant effects for the independent variable indicate that the variable of interest (WOR-S, WOR, or the interactions) predicted depressive symptoms following receipt of an exam grade after covarying depressive symptoms prior to taking the exam. We examined four covariance structures (autoregressive, unstructured, compound symmetry, toeplitz) using Akaike’s information criterion (AIC) and found the unstructured covariance structure produced the best model fit.
Results
To focus on occasions where receipt of exam grades involved disappointment, we limited our analyses to include only those exams for which participants received a grade that was lower than their goal. Among the 213 participants included in our analyses, there were a total of 473 occasions on which participants obtained exam grades that fell short of their goals (86% of the 549 occasions examined). Thus, on average, we examined 2.2 disappointing exam scores (SD = .78) per participant.
At Time 1, the sample presented with an average PHQ score of 5.5 (SD = 5.3, n = 213). A total of 39 participants (18%) obtained PHQ scores of 10 or higher, indicating that had a diagnostic interview been performed, these participants likely would have met criteria for MDD. Descriptive statistics for MBDI scores are listed in Table 1. As the table shows, MBDI scores changed significantly from pre- to post-stressor for only the first of the three stressors. As the table also shows, the range in MBDI scores was considerable across all time points. Ranges of the difference scores of the MBDI assessments within each period (i.e., from pre- to post-stressor) revealed substantial variability at each period: Period A (−30.5 to 22.0), Period B (−18.1 to 27.3), and Period C (−29.4 to 38.6).
Table 1. Descriptive Statistics for the Modified Beck Depression Inventory (MBDI).
| Period A (N = 139) |
Period B (N = 177) |
Period C (N = 157) |
||||
|---|---|---|---|---|---|---|
| MBDI | Time 1 | Time 2 | Time 3 | Time 4 | Time 5 | Time 6 |
| M | 9.2 | 8.1 | 7.0 | 7.1 | 6.5 | 6.2 |
| SD | 9.4 | 9.4 | 8.7 | 9.7 | 7.7 | 10.0 |
Note. We conducted paired t tests of MBDI scores at the two assessments within each period. These two time points were before and after each of the three exams for those students who received a disappointing exam grade (n = 213). Within period, scores only differed significantly for Period A (p = .04).
Overall, participants’ coping skills at Time 1 were rated just above the neutral point of 4.0, with an average WOR Quality score of 4.4 (SD = .9, n = 212). This indicates participants’ responses were judged to be likely to somewhat improve their mood on average. WOR Quality scores were significantly associated with lower depressive symptoms on the PHQ at Time 1 (r = −.43, p < .0001, n = 212). On the WOR-S, the average Quality score was 5.0 (SD = .8, n = 139) at Time 2, 4.8 (SD = .8, n = 176) at Time 4, and 4.5 (SD = 1.0, n = 156) at Time 6–all consistent with an average tendency to use positive coping. Finally, participants on average reported that successful exam outcomes were quite important for them. On a scale ranging from 1 (not important at all) to 7 (very important), the average rated importance was 6.3 (SD = .89) at Time 1, 6.1 (SD = 1.05) at Time 3, and 6.1 (SD = 1.1) at Time 5.
While our primary research questions were assessed using quality scores from the WOR and WOR-S, we examined additional descriptive statistics related to the total score for the WOR-S as this study is the first application of this measure. The average WOR-S Total scores were 2.8 (SD=2.2) at Time 2, 2.0 (SD=2.2) at Time 4, and 1.6 (SD=2.4) at Time 6. These positive scores indicate that participants, on average, provided more positive coping responses than negative responses on the WOR-S. Separate examination of positive and negative scores suggested that the decrease in total scores was attributable to both an increase in negative coping and a decrease in positive coping across repeated administrations of the measure.
WOR-S as a Predictor of Depressive Symptom Reactivity
We first examined the WOR-S as a predictor of depressive symptom reactivity. We conducted a repeated measures regression in which WOR-S Quality score predicted MBDI after each exam controlling for MBDI before each exam. WOR-S Quality score was a significant predictor of depressive symptom reactivity (r = −.21, t = −3.2, degrees of freedom [df] = 212, p = .002), such that lower quality ratings predicted elevated depressive symptoms following receipt of exam grades.
It is possible that rather than assessing participants’ ability to cope with their exam grade, WOR-S Quality score is simply a proxy for participants’ exam performance or their performance relative to their pre-exam goals. Therefore, we included participants’ exam grades and their performance relative to their goals as covariates in a repeated regression model in which WOR-S Quality scores predicted MBDI scores after each exam controlling for MBDI scores prior to each exam. WOR-S Quality score remained a significant predictor of depressive symptom reactivity even after covarying both exam grades and exam goal discrepancy (r = −.17, t = −2.5, df = 212, p = .01).
Contextual Moderators: Initial Depressive Symptom Severity and Affective Reactions
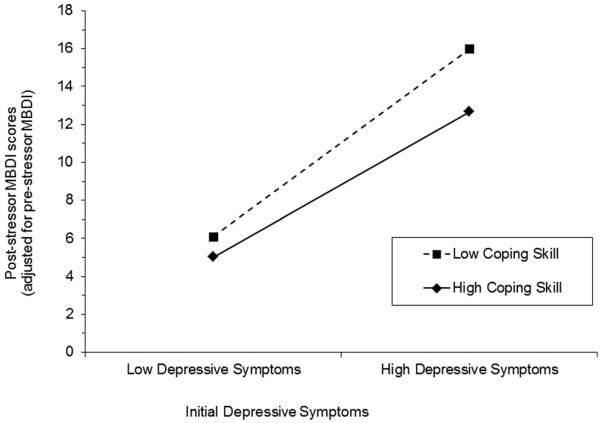
Next, we examined two contexts in which coping skills may be of greater consequence. First, we tested whether the WOR-S is a stronger predictor of depressive symptom reactivity for those who are initially more depressed. To do so, we analyzed the interaction of initial PHQ score and WOR-S Quality score in predicting depressive symptom reactivity. We found a significant interaction between PHQ score at Time 1 and WOR-S Quality score (r=−.14, t=−2.0, df=211, p = .04). Figure 1 displays this interaction using values of plus or minus one standard deviation on WOR-S Quality and the mean PHQ values among those with or without clinically elevated scores (with 10 or above being the cutpoint). As Kroenke and Spitzer (2002) have reported, individuals who score a 10 or above on the PHQ are likely to meet criteria for MDD (with 88% sensitivity and specificity). As shown in Figure 1, coping skills were more strongly related to depressive symptom reactivity among those with high depressive symptom severity as compared with those with low symptom severity.
Figure 1.
Depressive symptom severity as a moderator of stressor-specific coping skills predicting depressive symptom reactivity
Note. High and low initial depressive symptoms were assessed by the PHQ. Coping skills were assessed by the WOR-S. For initial depressive symptoms, the MBDI values plotted are the predicted values for: (1) a PHQ score of 3.3 (i.e., the mean among those with PHQ scores < 10); and (2) a PHQ score of 14.8 (i.e., the mean among those with PHQ scores ≥ 10). For coping skills, the MBDI values plotted are those predicted for a WOR-S score one standard deviation above and below the mean. Post-stressor MBDI scores (adjusted for pre-stressor MBDI) indicate depressive symptom reactivity, where higher scores indicate greater reactivity.
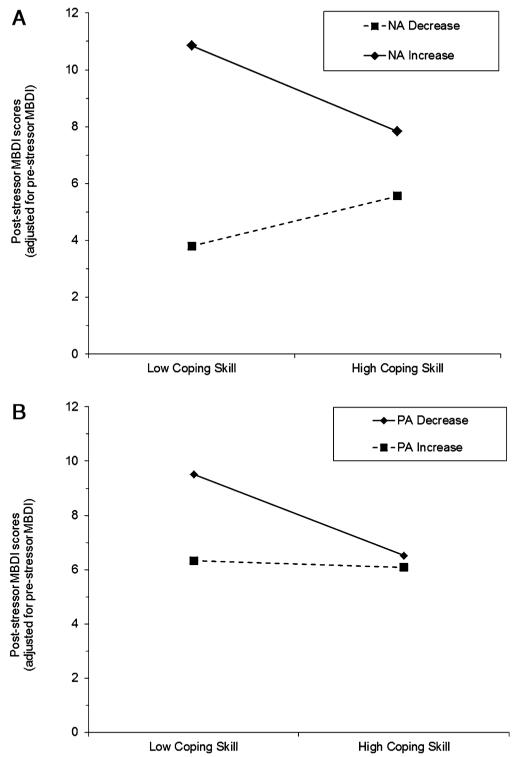
Second, we considered participants’ affective response to receiving their exam grades based on the PANAS-M as a potential moderator of the association between the WOR-S and depressive symptom reactivity. We predicted that coping skills would be more consequential when affective reactions to receiving exam grades were more marked than would be predicted on the basis of participants’ initial NA or PA scores. Two separate scores were derived from the PANAS-M, a negative affect score (NA) and a positive affect score (PA). We calculated residualized change scores of NA (NA reaction) and PA (PA reaction) by outputting the residuals of a regression model that included the respective score assessed prior to taking an exam (i.e., Times 1, 3, and 5) as a predictor of the respective score following receipt of the exam grade (i.e., Times 2, 4, and 6). NA reaction and PA reaction were moderately, negatively correlated at each time point (average r = −.34, all ps < .001).
To examine whether participants’ affective reactions to receiving their exam grades was distinct from depressive symptom reactivity, we examined the relation of PA and NA reactivity with depressive symptom reactivity. We examined these relations separately at each of the three periods and then took their average (using r-to-z transformations as needed). The average correlations of PA and NA reactivity with depressive symptom reactivity were −.16 and .35, respectively. Thus, affective reactions and depressive symptom reactivity appeared to be related, but distinct, constructs.
We examined the interaction of these residualized change scores with WOR-S in predicting depressive symptom reactivity. Both interactions were significant (WOR-S × NA reaction: r = −.32, t = −5.0, df = 211, p < .0001; WOR-S × PA reaction: r = .16, t = 2.4, df = 211, p = .02). As shown in Figure 2, WOR-S Quality score was more strongly related to depressive symptom reactivity for those who showed an increase in NA or a decrease in PA after receipt of their exam grades.
Figure 2.
A, B Changes in negative and positive affectivity as moderators of stressor-specific coping skills predicting depressive symptom reactivity.
Note. The MBDI values plotted are the predicted values for affect increase or decrease, meaning one standard deviation above or below the mean residualized change for each affect measure. Post-stressor MBDI scores (adjusted for prestressor MBDI) indicate depressive symptom reactivity, where higher scores indicate greater reactivity.
WOR as a Predictor of Depressive Symptom Reactivity
Finally, we examined whether the primary findings involving the WOR-S were consistent with those obtained when using the standard WOR completed at Time 1. Across the three time points, the average correlation of the WOR with the WOR-S was r = .11; this correlation was only significant at Time 1. Similar to the WOR-S, WOR Quality score was a significant, but slightly weaker, predictor of depressive symptom reactivity (r = −.15, t = −2.2, df = 210, p = .03).WOR Quality score remained a significant predictor of depressive symptom reactivity even after covarying exam grades and exam goal discrepancy (r = −.18, t = −2.6, df = 210, p = .009). However, unlike the WOR-S, WOR Quality score did not significantly interact with any moderator examined in predicting depressive symptom reactivity (PHQ score at Time 1: r = −.01, t = −.14, df = 208, p = .89; NA reaction: r = −.10, t = −1.5, df = 209, p = .15; PA reaction: r = −.05, t = −.69, df = 209, p = .49). This suggests that although the standard WOR performed similarly to the WOR-S in some ways, the degree of overlap between the measures was modest. Moreover, the importance of contextual factors for the relation between coping skills and depressive symptom reactivity was only evident when using the WOR-S.
Last, we examined a model in which both quality scores from the standard WOR (assessed at time 1) and quality scores from the WOR-S served as predictors of depressive symptom reactivity. In this model, both WOR Quality scores remained independent significant predictors of depressive symptom reactivity (standard WOR: r = −.14, t = −2.0, df = 210, p = .04; WOR-S: r = −.21, t = −3.1, df = 210, p = .002).
Discussion
In this study, we report the first evidence that the quality of coping skills used in the wake of moderate, recurring stressors predicts successful regulation of depressive symptoms. By examining change in depressive symptoms immediately surrounding a series of stressors (i.e., examining depressive symptom reactivity), we were able to detect the relatively immediate effects of the use of coping skills. While we focused primarily on repeated assessment of the quality of coping skills utilized surrounding specific stressors, we also used a more traditional one-time coping skill assessment. These two approaches to measuring coping skills (i.e., one-time and stressor-specific) yielded scores that were statistically related, but remarkably independent (r = .11). Both skill assessments (the standard WOR and the modified stressor-specific WOR) independently predicted depressive symptom reactivity.
The low correlation between coping skills as assessed by the WOR and the WOR-S parallels the low correlation Strunk and colleagues (2007) obtained between the WOR and their observer-rated measure of the performance of coping skills. Strunk and colleagues rated recordings of CT sessions to assess patients’ performance of, their reports of the use of, and their stated intentions to continue the use of coping skills. While their measure of patients’ performance of coping skills and the WOR each predicted patients’ risk for relapse after a successful course of treatment, the two predictors were unrelated. In this study, the WOR and the WOR-S emerged as similarly large and independent predictors of depressive symptom reactivity. Compared with the WOR, we suspect that both the measure of patients’ performance of coping skills used by Strunk and colleagues and the stressor-specific measure of coping skills we employed better capture a person’s actual use of coping skills. In contrast, by utilizing a number of different scenarios, the WOR may provide a more precise estimate of one’s level of mastery of coping skills. Our results show these predictors (the WOR and WOR-S) to be distinct, with each independently predicting depressive symptom reactivity following a stressor.
Our results also shed light on the contexts in which the relationship between coping skills and reduced depressive symptom reactivity may be particularly strong. We examined two contextual factors: the severity of participants’ depressive symptoms and the extent to which participants experienced affective shifts in association with a given stressor (i.e., the degree of increased negative affect or reduced positive affect). When we examined the stressor-specific assessments of coping skills, coping skills were more predictive of depressive symptom reactivity among participants with higher levels of depressive symptoms and on occasions of marked affective shifts. Our failure to find these effects with the WOR is consistent with the possibility that stressor-specific assessments of coping skills are needed to identify the contexts in which use of coping skills are most important to successful emotion regulation.
Our findings can be taken as indirect support for some therapeutic practices in CT. Cognitive therapists often help clients learn to identify and challenge their negative thinking by instructing them to pay attention to moments of affective shifts, particularly increases in negative affect (Beck, 1995). In these moments, therapists encourage clients to use coping skills to resolve the upsetting situation or change the negative thoughts contributing to the negative mood. Consistent with these periods of affective shifts marking important occasions for using coping skills, we found that coping skill use was most strongly related to less depressive symptom reactivity on occasions marked by an increase in negative affect (or a decrease in positive affect).
Future research might examine how our findings would apply in the context of depressed clients participating in a course of CT. Through use of experience-sampling methodology, both greater coping skills and less negative affective reactivity to daily stressors have been found to predict greater symptom change in CT (Gunthert, Cohen, Butler, & Beck, 2005; Cohen et al., 2008). Perhaps drawing on methods used in this study, future research might aim to characterize the role of coping skills in managing clients’ emotional reactions over a course of CT. We suspect that clients come to use coping skills more independently over time; and it is the patients who have a greater ability to use coping skills independently who are most protected from future relapse or recurrence. By developing more precise methods of assessing the independent naturalistic use of these skills, we hope to test these ideas and perhaps then begin to examine the therapeutic approaches that most successfully foster these skills.
We note a few key limitations of this study. First, as we utilized a nonclinical sample, we do not know whether our findings would extend to a sample of people formally diagnosed with MDD. However, based on PHQ scores, a significant minority of the sample (18%) would be expected to have met criteria for MDD. Moreover, consistent with the notion that coping skills would serve as a predictor of depressive symptom reactivity in a clinically depressed sample, we found that the relationship between stressor-specific coping skills and depressive symptom reactivity was stronger among those with more severe depressive symptoms.
Second, recall that we limited our analyses to exams that consisted of a disappointment. One might wonder whether our results were a consequence of our particular method of defining disappointing events. While we were especially interested in occasions of disappointment, we also conducted analyses using an unrestricted dataset including all data surrounding exams participants completed. Our primary findings remained unchanged. Thus, the relation of coping to depressive symptom reactivity was not likely to be a result of our specific way of defining disappointing events. Finally, our results were obtained in the context of examining one specific recurring stressor (i.e., college exams). Therefore, it is possible that our findings would not generalize to other stressors. Though we have no reason to believe this would be the case, examination of additional stressors in future research would be useful.
In conclusion, we found that the use of coping skills among a nonclinical sample served as an important predictor of depressive symptom reactivity after naturally occurring stressors. Less skillful coping was implicated in greater depressive symptom reactivity–especially for people with greater initial depressive symptom severity or on occasions marked by greater affect shifts. As both one-time and stressor-specific assessments of coping skills appeared to be independent predictors of depressive symptom reactivity, we encourage future research that complements one-time assessments of mastery of coping skills with assessments of naturalistic skill use.
Appendix
WOR Scoring Procedures
Scoring for the WOR followed standard procedures outlined by Barber and DeRubeis (1992), which included the use of three independent raters that rotated roles (Rater 1, Rater 2, or Rater 3) throughout the rating process. Participants completed a full protocol that included six scenarios. Before the participants’ WORs were coded, each protocol was divided into individual scenarios, given random identification numbers, and randomized. The first rater of each scenario divided the participant’s response into individual thought units and rated each thought unit as exhibiting one of 25 coping skill categories described in the WOR Rater’s Guide. Coping skill categories included both positive and negative categories of coping – positive responses were adaptive responses (e.g., generating a specific plan or an alternative explanation), while negative responses were maladaptive responses (e.g., focusing blame on the self). The first rater also rated the Quality of the coping response on a 7-point scale from 1 (worst possible response, likely to worsen the participant’s mood and situation) to 7 (best possible response, likely to improve the participant’s mood and situation). The second rater used the same thought units as determined by the first rater, but otherwise was blind to any other decisions (i.e., individual category ratings or Quality ratings). The second rater made determinations of individual thought unit ratings and Quality ratings for each scenario. The third rater also made determinations of the quality of coping responses and resolved any discrepancies between the two raters on the individual thought unit ratings of coping skill categories. The third rater’s consensus ratings and the average of all three raters’ Quality ratings were used for analysis. The WOR Total score consisted of the number of positive responses minus the number of negative responses for each protocol. ICCs for the reliability of the WOR categorical judgments were calculated using the first two raters for each protocol. ICCs for the reliability of the WOR Quality ratings were calculated using all three raters for each protocol.
Footnotes
We also examined the role of participants’ rating of the importance of doing well in the class as a potential moderator of the relationship between the use of exam-specific coping skills (WOR-S) and depressive symptom reactivity. Course importance was not a significant moderator, t(212) = −.91, p = .37.
Although not our primary measures of coping skills, we also utilized the WOR and WOR-S Total scores as independent variables in our analyses. The kappa coefficients for the category ratings used to calculate WOR and WOR-S Total scores were .67 and .61, respectively. Similar to the WOR-S Quality score, WOR-S Total score was a significant predictor of depressive symptom reactivity (r = −.19, t = −2.8, df = 212, p = .006), such that lower total ratings predicted elevated depressive symptoms following receipt of exam grades. We also found a significant interaction between PHQ score at Time 1 and WOR-S Total score (r = −.14, t = −2.0, df = 211, p = .04) in predicting depressive symptom reactivity as well as significant interaction effects of WOR-S Total and NA and PA reaction (WOR-S × NA reaction: r = −.20, t = −2.9, df = 211, p = .004;
References
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Barber JP. What is learned in cognitive therapy? An initial validation of The Ways of Responding questionnaire and a test of the compensatory model of change. Dissertation Abstracts International. 1990;50(9-B):4209. (Accession No. 1990–56359–001) [Google Scholar]
- Barber JP, DeRubeis RJ. The ways of responding: A scale to assess compensatory skills taught in cognitive therapy. Behavioral Assessment. 1992;14:93–115. [Google Scholar]
- Beck JS. Guilford Press; New York, NY: 1995. Cognitive therapy: Basics and beyond. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. Guilford; New York, NY: 1979. [Google Scholar]
- Beck AT, Steer RA, Brown BK. Beck depression inventory manual. 2nd ed. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Cohen LH, Gunthert KC, Butler AC, Parrish BP, Wenze SJ, Beck JS. Negative affective spillover from daily events predicts early response to Cognitive Therapy for depression. Journal of Consulting and Clinical Psychology. 2008;76:955–965. doi: 10.1037/a0014131. [DOI] [PubMed] [Google Scholar]
- Gunthert KC, Cohen LH, Butler AC, Beck JS. Predictive role of daily coping and affective reactivity in Cognitive Therapy outcome: Application of a daily process design to psychotherapy research. Behavior Therapy. 2005;36:77–88. [Google Scholar]
- Haaga DAF, Thorndike FP, Friedman-Wheeler DG, Pearlman MY, Wernicke RA. Cognitive coping skills and depression vulnerability among cigarette smokers. Addictive Behaviors. 2004;29:1109–1122. doi: 10.1016/j.addbeh.2004.03.026. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:509–515. [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for mixed models. SAS Institute, Inc; Cary, NC: 1996. [Google Scholar]
- Strunk DR, DeRubeis RJ, Chiu AW, Alvarez J. Patients’ competence in and performance of cognitive therapy skills: Relation to the reduction of relapse risk following treatment for depression. Journal of Consulting and Clinical Psychology. 2007;75:523–530. doi: 10.1037/0022-006X.75.4.523. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology. 2007;3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]