Abstract
Objective
To explore barriers to early presentation and diagnosis with breast cancer among black women.
Design
Systematic review.
Methods
We searched multiple bibliographic databases (January 1991–February 2013) for primary research, published in English, conducted in developed countries and investigating barriers to early presentation and diagnosis with symptomatic breast cancer among black women (≥18 years). Studies were excluded if they did not report separate findings by ethnic group or gender, only reported differences in time to presentation/diagnosis, or reported on interventions and barriers to cancer screening. We followed Cochrane and PRISMA guidance to identify relevant research. Findings were integrated through thematic synthesis. Designs of quantitative studies made meta-analysis impossible.
Results
We identified 18 studies (6183 participants). Delay was multifactorial, individual and complex. Factors contributing to delay included: poor symptom and risk factor knowledge; fear of detecting breast abnormality; fear of cancer treatments; fear of partner abandonment; embarrassment disclosing symptoms to healthcare professionals; taboo and stigmatism. Presentation appears quicker following disclosure. Influence of fatalism and religiosity on delay is unclear from evidence in these studies. We compared older studies (≥10 years) with newer ones (<10 years) to determine changes over time. In older studies, delaying factors included: inaccessibility of healthcare services; competing priorities and concerns about partner abandonment. Partner abandonment was studied in older studies but not in newer ones. Comparisons of healthy women and cancer populations revealed differences between how people perceive they would behave, and actually behave, on finding breast abnormality.
Conclusions
Strategies to improve early presentation and diagnosis with breast cancer among black women need to address symptom recognition and interpretation of risk, as well as fears of the consequences of cancer. The review is limited by the paucity of studies conducted outside the USA and limited detail reported by published studies preventing comparison between ethnic groups.
Keywords: Oncology
Strengths and limitations of this study.
Several of the themes were present in a large number of studies, indicating the strength of the review's findings. Findings from quantitative and qualitative studies were broadly similar, providing further corroborative evidence of this.
However, there were some conflicting findings. These were potentially due to differences in when research was published and whether studies included women who had been diagnosed with cancer or general populations.
Most studies were conducted in the USA, which made it difficult to draw conclusions and assess implications for women across other developed countries due to the particular cultural history of the US population and the way that US healthcare is funded.
Further, studies varied in their definition of, and groupings of, ethnicities. This meant we were unable to explore differences between black ethnic groups.
Studies also varied in their methodological quality; small samples, limited information on data analysis and on demographic characteristics were common.
US studies which reported on the health insurance coverage of participants showed that the majority (between 58% and 92%) were insured. Inclusion of relatively affluent samples in some studies may not reflect the general US black female population. The influence of age on women's perceptions and delay was also not explored systematically in any of the studies.
Background
Breast cancer is the most common cancer among women and leading cause of death worldwide1 although incidence and survival rates vary across ethnic group. Data from the USA determined that African-American women have a 6% lower incidence rate of cancer but a 16% higher death rate than white women. Further, they are less likely than white women to present with localised breast cancer2 Analysis of UK cancer registry data has also shown that despite lower breast cancer incidence rates in the UK among black African and black Caribbean than white women, black women are more likely to be diagnosed with metastatic disease and have poorer survival than white British women.3 This may reflect the higher proportion of black women than white women developing triple negative breast cancer—an aggressive form of the disease associated with poorer outcomes.4 5 A second factor contributing to this disparity in the UK and the USA relates to differing access to, and uptake of, breast cancer screening. In both nations, screening uptake is lower in black than in white populations and communities.6 There is also evidence—largely from the USA—of black and African-American women delaying longer with symptomatic breast cancer before seeking health professional's help than white women. ‘Fatalism’, fear, embarrassment, lack of trust in health services, lower education and limited knowledge about cancer and its symptoms have been cited as barriers to early presentation with breast cancer in black and African-American women.7–10 Provider delays, such as delayed general practitioner referral to hospital diagnostic services, can also contribute to late diagnosis.
The disparity in cancer outcomes between black and white women in the USA and the UK provided the impetus for appraising and synthesising research exploring barriers to early presentation and diagnosis with breast cancer in black women in this review. A search of previous literature reviews on the Cochrane Database of Systematic Reviews and other electronic databases did not identify any reviews relevant to the one undertaken.
Aim of the review
This review aimed to understand barriers to early presentation with, and diagnosis of, ‘symptomatic’ breast cancer among women of black African and black Caribbean descent living in developed countries. In the UK, there is a national breast screening programme. All women aged 50–70 years are invited for breast screening every 3 years. However, separate to this, women present symptomatically to their doctor when they discover a breast change. It is this ‘symptomatic’ presentation which is the focus of this review. The review includes research carried out in developed countries only as delays in presentation and diagnosis with cancer in developing countries are likely to be more influenced by the availability and accessibility of diagnostic services. The review was undertaken to inform a qualitative study exploring issues around symptomatic presentation with breast cancer among black African, black Caribbean and white British women in the UK.
Methods
The review methodology was informed by the Cochrane Handbook for Systematic Reviews of Interventions.11 The following electronic databases were searched on the 27 February 2013 to identify relevant studies: MEDLINE, PsycINFO, The Cumulative Index to Nursing and Allied Health Literature (CINAHL) and SCOPUS. Searches were restricted to research published from 1991 to 2013 and to English-language publications published in peer-reviewed journals. A detailed search strategy (table 1) was used to identify relevant papers in MEDLINE. Similar search strategies were applied in CINAHL, PsycInfo and SCOPUS.
Table 1.
Example of search strategy (MEDLINE)
| Concept 1 | Concept 2 | Concept 3 | Concept 4 |
|---|---|---|---|
| Neoplasms (SH) neoplasm* (free text) cancer* (free text) tumor* (free text) |
African Continental Ancestry Group (SH) West Indian* (free text) ‘Afro Caribbean*’ (free text) ‘Afro American*’ African American* (free text) African Caribbean* (free text) Black* not (Blackwell) (free text), minority group* (free text) ethnic minorit* (free text) ‘Black Minority Ethnic’ (free text) ‘BME’ (free text) |
Perception (SH) Social Perception (SH) perception* (free text) social perception* (free text) opinion* (free text) Attitude to Health (SH) attitude* (free text) social value* (free text) social norm* (free text) Culture (SH) belief* (free text) understanding* (free text) language* (free text) communicat* (free text) fear* (free text) mistrust (free text) trust (free text) cultur* (free text) relig* (free text) knowledge* (free text) barrier* (free text) embarrass* (free text) fatalism (free text) fatalistic (free text) income (free text) socioeconomic* (free text) depriv* (free text) educat* (free text) poor* (free text) poverty (free text) |
Early Diagnosis (SH) Early Detection of Cancer (SH) ‘Late presentation’ (free text) ‘Early presentation’ (free text) ‘Early diagnos*’ (free text) ‘Late diagnos*’ (free text) ‘early detection cancer’ delay* (free text) |
Criteria for including studies in this review
Papers included in the review reported on studies conducted with female adults (≥18 years) who were black, African-American, Caribbean or African.
Inclusion criteria
To be included in the review, papers had to be:
Published in English language peer-reviewed journals in the past 20 years.
Primary research articles.
-
Studies that explored barriers to early presentation and diagnosis with symptomatic breast cancer in black women of 18 years or over of African or Caribbean descent
Including studies that explored factors affecting women's return for follow-up following abnormal test results;
Including studies that explored diagnostic delays due to service-related factors after suspicious findings by health professionals;
Including studies that explored attitudes to, and undertaking of, self-examination (relating to breast cancer);
Including healthy women and those who had cancer.
Conducted in developed countries.
Exclusion criteria
Papers were excluded from the review if they:
Did not report separate findings by ethnic group;
Did not report separate findings for men and women;
Did not report separate findings for breast cancer;
Only reported research carried out in developing countries;
Only reported differences in time to presentation/diagnosis by ethnic group but did not explore factors accounting for these differences;
Only reported uptake of, or barriers to, cancer screening;
Only described interventions to increase uptake of cancer screening and/or improve early presentation/detection rates;
Only described black women's perceptions of cancer without discussing how their perceptions related to/influenced early presentation and diagnosis.
Data collection and analysis
Titles and abstracts of all studies identified by the searches were retrieved and reviewed by CELJ who excluded all irrelevant papers (see online supplementary appendix 1). Abstracts from approximately 10% of all retrieved papers, randomly sampled (n=80), were independently reviewed by ER. Studies not excluded at this point were retrieved in full text and assessed for eligibility by CELJ. Excluded articles were reviewed independently by ER or JM to ensure that studies were not erroneously excluded.
Data extraction and quality appraisal
Data were extracted systematically from eligible papers using Data Extraction Forms (DEFs) developed by the team (see online supplementary appendices 2 and 3). Data were extracted from eligible papers independently by two from the team of reviewers (CELJ, JM, RHJ, LJLF and GL).
Methodological quality was appraised using six attributes of research design that impact directly on the veracity of research findings irrespective of the particular research design (based on refs. 12–14):
Appropriateness of study design;
Suitability of data collection strategy;
Appropriateness of sample and sampling method;
Appropriateness of analytic approach/tools;
Level of control over confounding variables (quantitative studies) or level to which research context was adequately considered (qualitative studies);
Whether interpretation of findings was justified by the data.
No papers were excluded based on quality, but lower quality studies were given less weight in the discussion.
Data synthesis
Thematic synthesis was used to integrate findings from qualitative and quantitative studies.15 This entailed line-by-line coding of text from the qualitative studies. Codes were compared to identify recurrent concepts and patterns between themes which were subsequently organised into a framework of descriptive themes. Findings from the quantitative studies were summarised descriptively (as the design of the quantitative studies rendered it impossible to undertake meta-analysis) and integrated into the thematic framework. We developed new interpretative constructs (we compared studies that were <10 years old with studies conducted ≥10 years ago and studies of women with and without breast cancer to explain our findings) in order to go beyond the primary studies and to generate new explanations and hypotheses.
Results
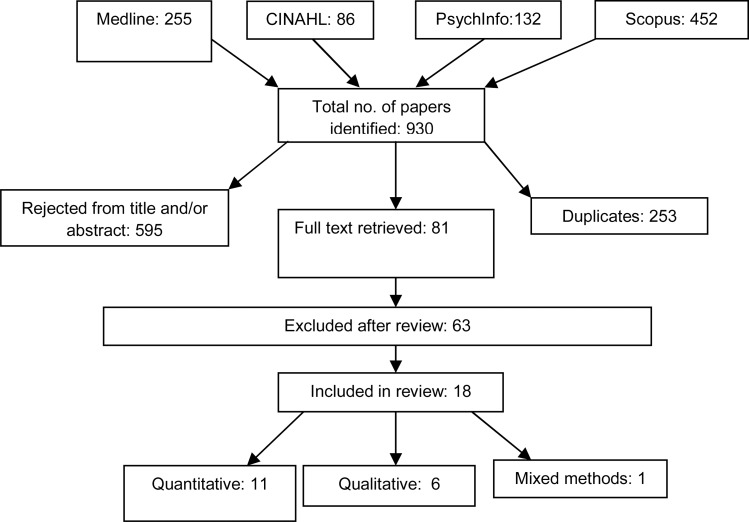
We identified 18 papers that met our inclusion criteria (figure 1) providing data for 6183 individuals who were between 19 and 99 years; of these, 17 studies were conducted in the USA and 1 in the UK. As most studies were conducted in the USA, explicit reference will be made when referring to the UK study. Eleven papers were quantitative, six qualitative and one with mixed methods.
Figure 1.
Data search and retrieval.
Studies included women who had been diagnosed with cancer (8), general population samples (7) and women with abnormal mammogram or clinical breast examinations (1). One study included both women who had been diagnosed with breast cancer and a general control group. In one study, it was unclear whether or not the sample had been diagnosed with cancer.
Five quantitative studies were considered as high quality,16–20 four were deemed to be of medium quality21–24 and two of low quality.25 26 All six qualitative studies were considered as medium quality.27–32 The mixed-methods study was considered as medium quality33 (table 2).
Table 2.
Summary information on selected papers (AA=African-American; online supplementary appendix 4 for results of individual studies)
| Reference | Site of cancer | Country | Type of study | Sampling method | Methods | N | Participants | Quality |
|---|---|---|---|---|---|---|---|---|
| 16 | Breast | USA | Quantitative | Cross-sectional, purposive | Face-to-face interview | 184 | Black women with abnormal mammogram or clinical breast examination | High |
| 17 | Breast | USA | Quantitative | Cross-sectional, case-control | Face-to-face interview | 576 | AA women General population sample | High |
| 18 | Breast | USA | Quantitative | Cross-sectional, convenience | Self-report questionnaire, administered in person by investigator | 129 | AA women with breast cancer | High |
| 19 | Breast | UK | Quantitative | Cross-sectional, population-representative sample plus booster sample for non-white ethnic groups/women >55 years | Face-to-face, computer assisted interview | 1515 | Black (n=265), white (n=806), and South Asian (n=333) women General population sample |
High |
| 20 | Breast | USA | Quantitative | Cross-sectional, convenience and case-control | Face-to-face interview | 954 | AA (n=378), white (n=162) women with breast cancer and community controls (n=414) | High |
| 21 | Breast | USA | Quantitative | Cross-sectional, 70% random sample of black women. Comparison white sample matched by age groups | Face-to-face interview | 367 | Black (n=206) and white (n=161) women with breast cancer | Medium |
| 22 | Breast | USA | Quantitative | Cross-sectional, convenience | Self-report questionnaire, administered in person by investigator | 352 | Black and AA women (breakdown by ethnic group not provided) General population sample |
Medium |
| 23 | Breast | USA | Quantitative | Cross-sectional, convenience | Self-report questionnaire, administered by post | 349 | AA (n=152) and white (n=197) women General population sample |
Medium |
| 24 | Breast | USA | Quantitative | Cross-sectional, convenience | Self-report questionnaire administered in person by investigator | 699 | Black, white and Latino women (breakdown by ethnic group not provided) General population sample |
Medium |
| 25 | Breast | USA | Quantitative | Cross-sectional, random-stratified | Face-to-face structured interview | 682 | AA (n=280), white (n=402) General population sample |
Low |
| 26 | Breast | USA | Quantitative | Cross-sectional, convenience | Self-report questionnaire, administered in person by investigator | 60 | AA women with breast cancer | Low |
| 27 | Breast | USA | Qualitative | Convenience | Focus groups, thematic and pattern analysis | 32 | AA women General population sample |
Medium |
| 28 | Breast | USA | Qualitative | Convenience sample | Focus groups, narrative analysis | 80 | Black (mainly AA) (n=26), white (n=23), Latino (n=31) women with breast cancer | Medium |
| 29 | Breast | USA | Qualitative | Convenience and snowball | Interviews, narrative and content analysis | 20 | Black women with breast cancer | Medium |
| 30 | Breast | USA | Qualitative | Not provided | Focus groups, thematic and pattern analysis | 100 | AA women Not stated whether they had breast cancer or not |
Medium |
| 31 | Breast | USA | Qualitative | Purposive | Ethnographic interviews, observations, fieldnotes, photographs, ethnographic analysis | 13 | AA women with breast cancer | Medium |
| 32 | Breast | USA | Qualitative | Convenience | Interviews, narrative and thematic analysis | 23 | AA women with breast cancer | Medium |
| 33 | Breast | USA | Mixed-methods | Mixed- method (cross-sectional survey with subsequent interviews | Self-report questionnaire, administered by post Follow-up telephone interview |
48 | AA women with breast cancer | Medium |
Ethnic definitions in the findings and discussion are taken from the papers included in the review.
Knowledge
Low awareness of cancer symptoms and/or personal risk
A consistent finding across studies was the low level of knowledge among black and African-American women about symptoms of breast cancer and/or risk factors for developing the disease.19 20 23 27–30 32 Poor knowledge of symptoms and risk factors was associated with delay in presentation among black and African-American women with breast cancer.28 29 31
Poor symptom awareness and knowledge of risk factors/personal risk
Comparisons of risk perceptions among African-American and white women with breast cancer in two studies revealed a significantly lower percentage of African-American women (25%) than white American women (44%) felt susceptible to the disease before they were diagnosed23 and that African-American women were less likely than white women to believe that if a woman has cancer it increases the risk for their daughter.20 In the UK, few black (13%) and white women (12%) without breast cancer knew that women over 70 years are at higher risk of breast cancer than women of any age.19
Further, a number of US studies suggested that black and African-American women were unaware of risk factors for breast cancer and of their personal risk of developing it.27 29 30 32 Some women believed that breast cancer was a ‘white woman's disease’ and others that they were not at risk because they did not have a family history of breast cancer. Two studies reported that these perceptions were reinforced by media messages which focused on white women.27 32 Underestimation of risk appeared to influence delayed presentation.29 Women who thought their chance of getting cancer was low, in some cases, lacked the motivation or inclination to check their breasts.27 29
Recognising significance of cancer symptoms
There was strong evidence to suggest that in the USA, black and African-American women lacked knowledge of, and information about, symptoms of breast cancer.27–29 32 In the UK, black women (16%) were less likely to recognise five or more non-lump symptoms of breast cancer than white women (22%).19 Many of those with cancer had underestimated the significance of their symptoms which contributed to them a delay in presentation. For some African-American women, there was confusion over whether or not pain was a symptom of breast cancer. Presence of pain reassured some African-American women that their breast symptom was not cancer.28 32 One had ‘read that pain [was] not a risk factor’.32 Further, some studies suggested a tendency among African-American women to tolerate or ignore symptoms, until they were severe, before seeking medical attention31 33:
At first, I tried to ignore my pain but it continued to get worse.33
In one study, some African-American women with breast cancer only presented when their symptoms worsened or they developed additional symptoms.31 Another study suggested that African-American women were more likely than white women to delay presentation if their lump was not bothering them.20 Other contributing factors to delay included women who assessed that their symptoms were caused by stress29 or women who had previous diagnoses of a benign breast lump.31
Empowerment and confidence
Making time to check for and/or present with symptoms
One US study identified that women who were unaware of breast cancer symptoms lacked confidence to check their breasts.27 In the UK general population study, breast checking differed by ethnic group; black women were less likely than white women to report breast checking (after controlling for age and socioeconomic status).19 However, similarly high percentages of black (50%) and white (55%) women were fairly or very confident that they would notice a breast change.19
The same UK study found that barriers to symptomatic presentation were not more common in black than in white women. Moreover, black women (32%) were slightly less likely than white women (37%) to report having too many other things to worry about, and similar proportions reported being too busy to make time to see the doctor (34% black, 35% white).19
Evidence from the USA also suggested that women with family commitments would still find time to visit the doctor. In one study, African-American women with cancer said that they presented despite family caring obligations.31
Studies conducted over 10 years ago found some evidence that responsibilities might lead to delayed presentation: some African-American women and one black woman reported lacking time27 29 to check their breasts. Some black and African-American women without breast cancer, but with childcare, employment and partnership responsibilities reported they would be less likely than those without these responsibilities to seek help for breast symptoms should they arise.22
Lack of partner support
Among black and African-American women, with and without breast cancer, lack of partner support and concerns around partner abandonment were raised when discussing the physical effects of breast surgery on their relationships. However, the specific influence of partner support/abandonment on delay was unclear.20 28 30 31 In one study, black and African-American women with breast cancer reported that fear of partner abandonment inhibited help-seeking. However, this also appeared the case for white women.28 In another study, help-seeking was not affected, despite one woman's partner saying he did not want to live with, ‘no one titty bitch’ and others saying they were concerned that they would be less appealing to their partners.31 Limited evidence indicates that African-American women are more likely than white women to delay seeking help due to lack of partner support.20
Stigma, taboo and fear
Stigma and taboo emerged as salient themes among black women in the USA and the UK. They were reluctant to talk about cancer, and reported that in their communities, the word ‘cancer’ was whispered32 and referred to as ‘the big C’.28 Cancer diagnoses often remained undisclosed even to family members.30 However, in a US study, disclosure to others (particularly family or friends) was associated with shorter delays in presentation in African-American women.18 Whether disclosure influenced decisions to seek care or reflected openness to discuss cancer symptoms with others (including healthcare professionals) was less clear. A further study found two-thirds of African-American participants felt they made their own decision to seek help.33 Black and African-American women who were fearful of cancer were significantly more likely to delay presentation than those who were not.16 31 In one study, some African-American women were too scared to check their breasts,27 while in another study, 32% of African-American participants with breast cancer reported feeling scared when they discovered their symptoms.33 However, this and another study found no relationship between fear and delay.26 33
Religiosity
There was limited evidence to suggest that religiosity impacted time to presentation with cancer in symptomatic black and African-American women. Two studies exploring the influence of religiosity found it did not inhibit help-seeking in women with symptomatic breast cancer.18 28 However, there was some evidence that age31 and African-American ethnic group20 25 may predict a belief that religious intervention influences the outcome of cancer rather than medical treatment, as well as a resigned acceptance of death. The link between what has been termed ‘fatalism’—a belief that cancer is preordained—and delayed presentation is unconfirmed. One study of healthy women suggested that fatalism negatively influenced help-seeking intention,22 but a study of women with breast cancer found no association between fatalism and actual delay in presentation.18
Trust in healthcare system
Curability of cancer
There was strong evidence to suggest that black and African-American women with and without cancer believed that cancer could be cured.17 18 22 23 Across three studies, 77–98% of African-American women did not believe that death was an inevitable outcome of cancer.17 18 23 In another study, only a small percentage of African-American (13%) and white women (16%) believed that cancer inevitably led to death.23 However, another study of African-American women reported that they believed cancer was a deadly and incurable disease and very few of those interviewed knew of women who had survived the disease.30 However, the influence of that belief (cancer equates with death) on help-seeking intention was not discussed.30
Fear of conventional treatment
Black and African-American women reported fearing the implications of cancer treatments and surgery17 20 28 31 and some said that they preferred non-conventional therapies.20 Treatment fear prolonged delay among some women with cancer. One study reported that 57% of African-American women with and without breast cancer believed treatments for breast cancer were worse than the disease itself,17 while three studies reported reluctance among African-American women to have surgery.20 28 31 Some African-American women reported fearing unpleasant side effects and were worried about what treatments comprised. One study reported that African-American women were more likely than white women to prefer non-conventional treatments in place of surgery.20
Quality of relationships with healthcare professionals
Concerns about interactions with doctors
In the UK study, concerns about wasting the doctor's time or finding it difficult to talk to a doctor were barriers to early presentation. However, these issues were just as likely to be reported by white women as black women.19
Lack of confidence in healthcare professionals
There was strong evidence suggesting black and African-American women lacked confidence in medical professionals due to breast symptoms being previously misdiagnosed. They expressed concerns over standards of care and the type of care they would receive; they were concerned about discrimination in medical settings. In one study, three African-American women with cancer were initially told their symptoms were benign and this contributed to delayed diagnosis. For example, one was told, “It's just cysts, it's nothing to worry about.”31 Further, some black and African-American women with cancer were concerned about doctors providing substandard, aggressive (‘she wound up with a mastectomy 2 weeks later just because of her mammogram’)28 or experimental care.28 29 The Tuskegee syphilis study34 was cited by black and African-American study participants in support of this belief.28 29 However, one study reported that African-American women felt that healthcare professionals should conduct breast examinations rather than women themselves, which suggested trust in the skills of healthcare professionals.27
Five studies examined black and African-American women's perceptions of discrimination in medical settings.16 22 24 28 29 Of these, two studies determined that although women perceived a degree of racism and discrimination, this did not appear to influence delay or help-seeking intent,16 22 but in another two studies it did influence help-seeking intention and delay.24 28
Practical and service barriers
Financial burden of healthcare and influence of health insurance on patient and provider delays
The impact of the financial burden of healthcare (affordability of healthcare and health insurance coverage) on delay was unclear based on the limited evidence provided by these studies. In one study, there was no statistically significant association between perceived affordability of healthcare and delay.33 In another study, women with health insurance were not significantly more likely to be diagnosed within 90 days than those without insurance.16
There was also a mixed picture of the influence of black and African-American women's socioeconomic status on delay within these studies. In two of them, socioeconomic status did not appear to influence delay among black women with cancer.16 26 However, three studies reported that less affluent black and African-American women were less likely to seek help for cancer symptoms and this did contribute to delayed presentation.18 20 22
Perceptions of access to healthcare services
In the UK study, access issues such as ease of booking appointments, arranging transport and distance between home and health centres appeared no more common in black women than white women. Rather, black women were less likely than white women to report difficulties making an appointment as a barrier to help-seeking (black 30%, white 36%). Difficulties in arranging transport were again less of a barrier (black 14%, white 16%) in black women. Overall, transport appeared a less common barrier than challenges with making appointments to see their doctor.19
In the US studies, the effect of access issues on delay was mixed. In a study of black and African-American women without breast cancer, being more likely to intend to seek help was significantly linked to positive perceptions of accessibility to healthcare.28 Further, in another study, poorer access to healthcare among black women with breast cancer made attending appointments difficult.21 However, two studies reported little evidence indicating access issues impacted on delay among black and African-American women with cancer.16 33
Factors which may explain the review findings
It was evident that some barriers to early presentation with cancer were more prevalent 10 years ago than the current scenario and vice versa. Accessibility of healthcare services21 22 and competing priorities22 27 29 were important issues influencing delay in black and African-American women in older (≥10 years) studies. However, in some recent studies (≤10 years), access to healthcare16 19 33 and competing priorities19 31 were reported to neither influence delay nor help-seeking intention.
Although the influence of partner abandonment was examined in one early quantitative study20 and emerged from women's narratives in three early qualitative studies,28 30 31 this theme was not examined in any recent quantitative studies. This does not mean, however, that it is not a current problem, only that it has not been examined as a potential influence over time.
Several differences were also noted between women with and without cancer. Competing priorities did not influence delay in a recent study of women with symptomatic breast cancer31 but they did influence how healthy women felt they would approach seeking help should they develop cancer symptoms.22 Further, although in some studies, the financial burden of healthcare16 26 33 and access issues16 33 did not influence delay among those women with breast cancer, healthy women cited both of these issues as potential barriers to their future help-seeking.22 These differences highlight that researchers may get different answers depending on whether they ask healthy women or women with cancer about delay/help-seeking intention.
Discussion
Delayed presentation with breast cancer in black women living in the USA and the UK appears to be influenced by multiple factors and to be highly individual and complex. Logically, all women may present late if they have limited awareness of the disease and its symptoms.35 Although, a relatively small number of studies comparing black and white women were included in the review, black women appear more likely than white women to have limited understanding of breast cancer and its risk factors. This might be the case particularly among (1) migrant women from countries where health campaigns about the disease are scarce, (2) women with limited command of the host nation's language and/or low literacy who are, therefore, not reached by the host nation's health messages and (3) women from communities where it is culturally unacceptable to discuss cancer and who, as a result, do not gain understanding of the disease through word of mouth.
This review, consistent with health behaviour models,36 37 illustrates how women's understanding of risk factors and their perceived personal risk influence their sensitivity to breast cancer symptoms and help-seeking on identifying them. Black women rightly perceive their risk of breast cancer to be lower than in white women.2 3 Consequently, they may retain little information provided to them by healthcare professionals or portrayed in breast cancer health promotion campaigns, as they may believe it to be of limited personal relevance.
Findings from studies incorporated in this review determined that many women lack confidence in checking, or are reluctant to check their breasts. However, if women are unaware of how their breasts typically feel, they will, as a consequence, face challenges in recognising subtle changes and may only detect change when the disease is relatively advanced.
Clearly, early presentation with cancer is not solely dependent on knowledge. Women with good knowledge of the disease may not seek help from healthcare professionals on detecting symptoms of breast cancer.38 This review suggests that fear may be an important factor preventing black women from seeking help. It appears multifaceted—women referred to fear of cancer treatments and abandonment by partners. Arguably, health messages communicating negative consequences of delayed presentation with breast cancer may be less effective than those framed in ways outlining benefits of early presentation. Fear-led messages may lead to avoidance and denial in people who fear a cancer diagnosis.36 Further, although it appears that disclosure to others about symptoms indicative of breast cancer can be important in promoting early presentation with the disease,39 it is not uncommon for black women to feel uncomfortable about disclosing symptoms to others, including healthcare professionals. This is due to the taboo and embarrassment associated with the disease.40 Women's previous encounters and rapport with healthcare professionals, and any exposure to discrimination or misdiagnosis, also appear to influence time to presentation.
Beliefs about the curability of breast cancer (a factor impacting positively on early presentation) may be influenced in women born outside the country they live in by experiences from their country of origin, where treatments for cancer may be less effective and death more likely.41 Religiosity might influence help-seeking behaviour but this will depend on how people perceive their own role and that of a higher influence in managing their health.42 The highly individual nature of religious beliefs may explain why the influence of religiosity on delay was unclear in this review. Further, it may reflect the nature of the samples recruited to the reviewed studies.
Papers incorporated into the review did not unequivocally support an association in the USA between financial barriers and late presentation with breast cancer in black and African-American women. It is likely that this finding reflects sampling issues; black women sampled in these studies appeared relatively affluent, 58–92% had health insurance. Work of others, including Schneider, demonstrates clearly the coexistence of socioeconomic factors and ethnicity and their impact on cancer staging and outcomes.43 However, it is important to note that outside the USA, socioeconomic factors may be more or less associated with ethnicity. They may also impact differently on time to presentation with breast cancer in differing healthcare systems.
Evidence from the sole UK study indicated that poor knowledge of breast cancer and its associated symptoms, and practical and financial issues, may act as barriers to early presentation with breast cancer in black African and black Caribbean women. However, this study alone is insufficient to enable conclusions to be drawn on factors impacting delayed diagnosis with breast cancer in black women living in the UK. Further, it grouped all black women together in the analysis. This would suggest that black women are a homogenous group; it is very likely that attitudes, help-seeking intention and help-seeking behaviours will vary considerably within and between black African and black Caribbean women in the UK and possibly between first-generation and second-generation migrants. Merely labelling women as ‘black’ may mask diverse attitudes and behaviours and lead researchers to overlook important nuances.44 Further research is needed in the UK to explore factors impacting early diagnosis with symptomatic breast cancer and to study in detail the similarities and differences by ethnic group.
Unfortunately, while we aimed to compare in detail barriers to early presentation with symptomatic breast cancer between different groups of black women in the USA and the UK, this proved impossible due to paucity of UK studies and poor level of reporting in many of the published US studies. Consequently, the specific nuances between different ethnic groups of black women could not be determined. However, it is striking that so many of the beliefs, taboos and fears were similar among black women, irrespective of their country of residence. These factors are clearly not genetic which suggests cultural factors are durable over many generations.
There was some evidence that some barriers to early diagnosis had lessened during the period of this review. This suggests that awareness-raising campaigns may have been successful in raising the importance of early presentation and overcoming practical challenges and personal concerns. Equally, the findings could reflect the time that black women migrating to developed countries had spent there. Arguably, migrants’ views will change over time as they adapt to their surroundings and become influenced by new cultures and health systems.45 There was also some evidence of differences between women with and without cancer, suggesting a distinction between what women say they would do if they discovered a symptom, versus what they do with the onset of symptoms.
Further high-quality research is needed to better understand barriers to early presentation and diagnosis with breast cancer in black ethnic groups living outside the USA. In particular, studies of, and comparisons between, ethnic groups in the UK are needed to determine influences on delay in presentation and their possible contribution to the poorer survival of black African and black Caribbean women in the UK.3 Researchers need to compare stage at diagnosis and cancer survival between ethnic groups after stratifying for tumour prognostic and biological factors. This would allow the relative influence of cancer biology, women's delay and system delay on outcomes to be determined. Findings of this review have several implications for policy and practice. Our review indicates that black women should feature more prominently in media campaigns and educational materials to prevent breast cancer being perceived as a ‘white women's’ disease. Information about the risk of breast cancer and its early symptoms, concerns about breast checking, surgery and the side effects of treatment also need to be addressed in ways that are culturally sensitive to black women.46 47 Vulnerable women, who fear partner abandonment and who may be reluctant to have treatment for breast cancer as a result, need to be identified and supported by healthcare professionals. Further, enhancing women's experiences of being diagnosed and treated for breast cancer, and encouraging engagement and discussion regarding the disease, may help to address stigma and taboo, promote disclosure and allay women's fears, factors believed to impact positively on early presentation and diagnosis.
Supplementary Material
Footnotes
Contributors: ER, CELJ, JM, RHJ, EAD and LJLF were responsible for the systematic review design. CELJ was responsible for data collection. CELJ, ER, RHJ, LJLF and GL were responsible for data extraction and appraising studies. CELJ, JM and ER were responsible for data analysis and interpretation. All authors contributed in drafting the manuscript. ER is responsible for the overall content as the corresponding author.
Funding: This article was funded by the National Awareness and Early Diagnosis Initiative (NAEDI) (grant number C7000/A12219). The NAEDI funding consortium, under the auspices of the National Cancer Research Institute (NCRI), consists of Cancer Research UK; Department of Health (England); Economic and Social Research Council; Health & Social Care R&D Division, Public Health Agency (Northern Ireland); National Institute for Social Care and Health Research (Wales) and the Scottish Government.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional unpublished data are available.
References
- 1.Worldwide Breast Cancer. Breast cancer statistics worldwide in 2010. http://www.worldwidebreastcancer.com/learn/breast-cancer-statistics-worldwide/ (accessed 19 Dec 2013)
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. Cancer J Clin 2013;63:11–30 [DOI] [PubMed] [Google Scholar]
- 3.Jack RH, Davies EA, MØller H. Breast cancer incidence, stage, treatment and survival in ethnic groups in South East England. Br J Cancer 2009;100:545–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jack RH, Davies EA, Renshaw C, et al. Differences in breast cancer hormone receptor status in Ethnic Groups: a London population. Eur J Cancer 2013;49:696–702 [DOI] [PubMed] [Google Scholar]
- 5.Parise CA, Bauer KR, Brown MM, et al. Breast cancer subtypes as defined by the estrogen receptor (ER), progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2) among women with invasive breast cancer in California, 1999–2004. Breast J 2009;15:593–602 [DOI] [PubMed] [Google Scholar]
- 6.Renshaw C, Jack RH, Dixon S, et al. Estimating attendance for breast cancer screening in ethnic groups in London. BMC Public Health 2010;10:157 http://www.biomedcentral.com/content/pdf/1471-2458-10-157 (accessed 8 Aug 2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lannin DR, Matthews HF, Mitchell J, et al. Impacting cultural attitudes in African-American women to decrease breast cancer mortality. Am J Surg 2002;184:418–23 [DOI] [PubMed] [Google Scholar]
- 8.Long E. Breast cancer in African-American women: review of the literature. Cancer Nurs 1993;16:1–24 [PubMed] [Google Scholar]
- 9.Frisby CM. Messages of hope: health communication strategies that address barriers preventing black women from screening for breast cancer. J Black Stud 2002;32:489–505 [Google Scholar]
- 10.Gullatte MM, Hardin P, Kinney A, et al. Religious beliefs and delay in breast cancer diagnosis for self-detected breast changes in African-American women. J Natl Black Nurses Assoc 2009;20:25–35 [PubMed] [Google Scholar]
- 11.Higgins JPT, Green S. eds. Cochrane handbook for systematic reviews of interventions: Cochrane book series. Chichester, UK: John Wiley & Sons Ltd., 2008:11–29 [Google Scholar]
- 12.Walsh D, Downe S. Meta-synthesis method for qualitative research: a literature review. J Adv Nurs 2005;50:204–11 [DOI] [PubMed] [Google Scholar]
- 13.Pluye P, Gagnon MP, Griffiths F, et al. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in Mixed Studies Reviews. Int J Nurs Stud 2009;46:529–46 [DOI] [PubMed] [Google Scholar]
- 14.Long AF, Godfrey M, Randall T, et al. HCPRDU evaluation tool for mixed methods studies 2002, http://usir.salford.ac.uk/13070/ (accessed 8 Aug 2013)
- 15.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8:45 http://www.biomedcentral.com/content/pdf/1471–2288–8–45 (accessed 8 Aug 2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerner JF, Yedidia M, Padgett D, et al. Realizing the promise of breast cancer screening: clinical follow-up after abnormal screening among black women. Prev Med 2003;37:92–101 [DOI] [PubMed] [Google Scholar]
- 17.Klassen AC, Washington C. How does social integration influence breast cancer control among urban African-American women? Results from a cross-sectional survey. BMC Womens Health 2008;8:4 http://www.biomedcentral.com/1472-6874/8/4 (accessed 8 Aug 2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gullatte MM, Brawley O, Kinney A, et al. Religiosity, spirituality, and cancer fatalism beliefs on delay in breast cancer diagnosis in African American women. J Relig Health 2010;49:62–72 [DOI] [PubMed] [Google Scholar]
- 19.Forbes LJL, Atkins L, Thurnham A, et al. Breast cancer awareness and barriers to symptomatic presentation among women from different ethnic groups in East London. Br J Cancer 2011;105:1474–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lannin DR, Mathews HF, Mitchell J, et al. Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. JAMA 1998;279:1801–7 [DOI] [PubMed] [Google Scholar]
- 21.Caplan LS, Helzlsouer KJ, Shapiro S, et al. Reasons for delay in breast cancer diagnosis. Prev Med 1996;25:218–24 [DOI] [PubMed] [Google Scholar]
- 22.Facione NC, Dodd MJ, Holzemer W, et al. Helpseeking for self-discovered breast symptoms. Implications for early detection. Cancer Pract 1997;5:220–7 [PubMed] [Google Scholar]
- 23.Barroso J, McMillan S, Casey L, et al. Comparison between African-American and white women in their beliefs about breast cancer and their health locus of control. Cancer Nurs 2000;23:268–76 [DOI] [PubMed] [Google Scholar]
- 24.Facione NC, Miaskowski C, Dodd MJ, et al. The self-reported likelihood of patient delay in breast cancer: new thoughts for early detection. Prev Med 2002;34:397–407 [DOI] [PubMed] [Google Scholar]
- 25.Mitchell J, Lannin DR, Mathews HF, et al. Religious beliefs and breast cancer screening. J Womens Health (Larchmt) 2002;11:907–15 [DOI] [PubMed] [Google Scholar]
- 26.Bradley PK. The delay and worry experience of African American women with breast cancer. Oncol Nurs Forum 2005; 32:243–9 [DOI] [PubMed] [Google Scholar]
- 27.Williams AG, Abbott RR, Taylor KD. Using focus group methodology to develop breast cancer screening programs that recruit African American women. J Community Health 1997;22:45–56 [DOI] [PubMed] [Google Scholar]
- 28.Facione NC, Giancarlo CA. Narratives of breast symptom discovery and cancer diagnosis: Psychologic risk for advanced cancer at diagnosis. Cancer Nurs 1998;21:430–40 [DOI] [PubMed] [Google Scholar]
- 29.Lawson EJ. A narrative analysis: a black woman's perceptions of breast cancer risks and early breast cancer detection. Cancer Nurs 1998;21:421–9 [DOI] [PubMed] [Google Scholar]
- 30.Bailey EJ, Erwin DO, Belin P. Using cultural beliefs and patterns to improve mammography utilization among African-American women: the Witness Project. J Natl Med Assoc 2000;92:136–42 [PMC free article] [PubMed] [Google Scholar]
- 31.Gates MF, Lackey NR, Brown G. Caring demands and delay in seeking care in African American women newly diagnosed with breast cancer: an ethnographic, photographic study. Oncol Nurs Forum 2001;28:529–37 [PubMed] [Google Scholar]
- 32.Moore RJ. African American women and breast cancer. Cancer Nurs 2001;24:9–35 [DOI] [PubMed] [Google Scholar]
- 33.Reifenstein K. Care-seeking behaviors of African American women with breast cancer symptoms. Res Nurs Health 2007;30: 542–57 [DOI] [PubMed] [Google Scholar]
- 34.Freimuth VS, Quinn SC, Thomas SB, et al. African Americans’ views on research and the Tuskegee syphilis study. Soc Sci Med 2001;52:797–808 [DOI] [PubMed] [Google Scholar]
- 35.Macleod U, Mitchell ED, Burgess C, et al. Risk factors for delayed presentation and referral of symptomatic cancer: evidence for common cancers. Br J Cancer 2009;101:S92–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cismaru M, Lavack AM, Hadjistavropoulos H, et al. Understanding health behavior: an integrated model for social marketers. Soc Mark Q 2008;14:2–32 [Google Scholar]
- 37.Austin LT, Ahmad F, McNally M-J, et al. Breast and cervical cancer screening in Hispanic women: a literature review using the health belief model. Womens Health Issues 2002;12:122–8 [DOI] [PubMed] [Google Scholar]
- 38.O'Mahony M, Hegarty J, McCarthy G. Women's help seeking behaviour for self discovered breast cancer symptoms. Eur J Oncol Nurs 2011;15:410–18 [DOI] [PubMed] [Google Scholar]
- 39.Burgess CC, Linsell L, Kapari M, et al. Promoting early presentation of breast cancer by older women: a preliminary evaluation of a one-to-one health professional-delivered intervention. J Psychosom Res 2009;67:377–87 [DOI] [PubMed] [Google Scholar]
- 40.Smith LK, Pope C, Botha JL. Patients’ help-seeking experiences and delay in cancer presentation: a qualitative synthesis. Lancet 2005;366:825–31 [DOI] [PubMed] [Google Scholar]
- 41.Muthoni A, Miller AN. An exploration of rural and urban Kenyan women's knowledge and attitudes regarding breast cancer and breast cancer early detection measures. Health Care Women Int 2010;31:801–16 [DOI] [PubMed] [Google Scholar]
- 42.Polzer RL, Miles MS. Spirituality in African Americans with diabetes: self-management through a relationship with god. Qual Health Res 2007;17:176–88 [DOI] [PubMed] [Google Scholar]
- 43.Krieger N, Chen JT, Kosheleva A, et al. Shrinking, widening, reversing, and stagnating trends in US socioeconomic inequities in cancer mortality: 1960–2006. Cancer Causes Control 2012;23:297–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Agyemang C, Bhopal R, Bruijnzeels M. Negro, Black, Black African, African Caribbean, African American or what? Labelling African origin populations in the health arena in the 21st century. J Epidemiol Community Health 2005;59:1014–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zanchetta MS, Pourelsami IM. Health literacy within the reality of immigrants’ culture and language. Can J Public Health 2006;97:S26–8 [PubMed] [Google Scholar]
- 46.Henderson PD, Gore SV, Davis BL, et al. African American women coping with breast cancer: a qualitative analysis. Oncol Nurs Forum 2003;30:641–7 [DOI] [PubMed] [Google Scholar]
- 47.Morgan PD, Fogel J, Rose L, et al. African American couples merging strengths to successfully cope with breast cancer. Oncol Nurs Forum 2005;32:979–87 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.