Abstract
Background: the deleterious changes in body composition that occur during the year after hip fracture are associated with increased disability, recurrent fracture, and mortality. While the majority of these unfavourable changes have been shown to occur during the first 2 months after fracture, potential changes in body composition occurring earlier than 2 months post-fracture have not been studied. Accordingly, the aim of this study was to rigorously assess short-term changes in body composition after hip fracture.
Methods: total body mass, lean mass, fat mass and total hip and femoral neck bone mineral density (BMD) were assessed via dual energy X-ray absorptiometry at 3 days, 10 days and 2 months post-fracture among 155 hip fracture patients from the Baltimore Hip Studies. Longitudinal regression analysis using mixed models was conducted to model short-term changes in body composition.
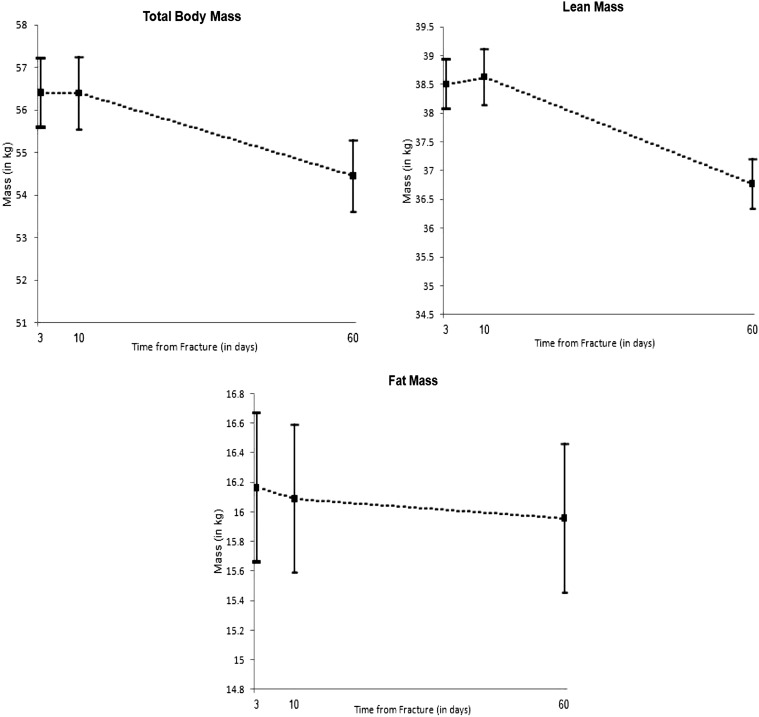
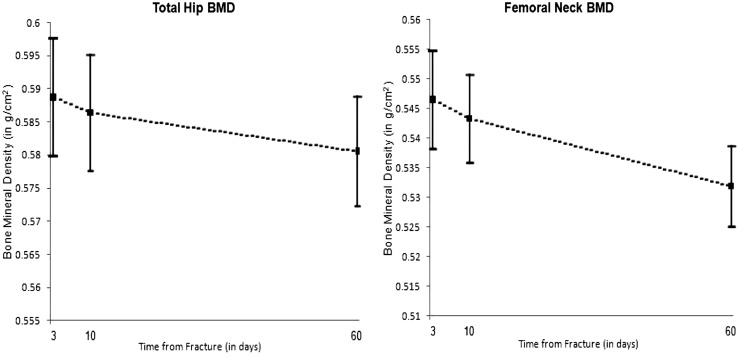
Results: no significant changes in body composition were revealed from 3- to 10 days post-fracture. However, significant decreases from 10 days to 2 months post-fracture were noted in the total body mass (−1.95 kg, P < 0.001), lean mass (−1.73 kg, P < 0.001), total hip BMD (−0.00812 g/cm2, P = 0.04) and femoral neck BMD (−0.015 g/cm2, P = 0.03). No meaningful changes in fat mass were uncovered.
Conclusions: the adverse changes in body composition during the first 2 months after hip fracture appear to have occurred primarily between 10 days and 2 months post-fracture. More research is needed to determine how these findings might help inform the optimal timing of interventions aimed at improving body composition and related outcomes after hip fracture.
Keywords: hip fracture, body composition, bone mineral density, lean mass, dual energy X-ray absorptiometry, older people
Background
Hip fracture is a common injury among older adults, which is associated with profound and lasting repercussions. There are over 300,000 new hip fracture patients in the USA per year [1] and the annual incidence of hip fracture is expected to increase to 700,000 in the USA and almost 4 million worldwide by 2050 [2]. Hip fracture is associated with a high degree of mortality as between 16 and 32% of hip fracture patients die in the year following fracture [3–6]. Survivors are burdened with substantial morbidity and recovery is typically prolonged and incomplete. Among the major contributing factors to the morbidity after hip fracture are deleterious changes in body composition.
The total body mass consists of three components: fat mass, lean mass and bone. Fat mass and lean mass demonstrate opposite and unfavourable patterns of change after hip fracture. Fat mass increases by up to 11% [7] and lean mass decreases by up to 6% [8] in older female hip fracture patients during the year after hip fracture. Healthy older women gain only 1.7% of fat mass and lose just 1% of lean mass per year [9]. Lower post-fracture bone mineral density (BMD) has also been associated with recurrent hip fracture, disability and mortality [10–12]. Thus, preventing deleterious changes in body composition could have profound clinical implications in hip fracture recovery. However, therapeutic interventions aimed at improving body composition after hip fracture have produced mixed results [13–16]. This may be due to the fact that the period during which most of the unfavourable changes in body composition occur after fracture is currently unclear.
While most studies have focused on assessing longer term changes in body composition after hip fracture, one analysis revealed that half of the bone and muscle mass that is lost after hip fracture occurs within the first 2 months [8]. However, it is unclear precisely when during the first 2 months the majority of lean mass is lost as no studies to date have assessed short-term changes in body composition after hip fracture. The goal of this analysis was to determine whether short-term changes in body composition occur after hip fracture.
Methods
Subjects
The study sample consisted of participants from the third cohort of the Baltimore Hip Studies (BHS3), described in detail elsewhere [8]. The final sample for this analysis consisted of 155 unique BHS3 participants from whom the body composition measures were obtained from at least one of the 3-, 10-day or 2 month post-fracture study visits. The study sample did not differ from the full BHS3 cohort in any of the key covariates described below (χ2, P > 0.05). The hip fracture of the proximal femur was surgically repaired in all study participants prior to the 3-day study visit. The study was approved by the Institutional Review Boards of the University of Maryland and the individual study hospitals.
Body composition assessment
The body composition outcomes included in this analysis were total hip and femoral neck BMD, total body mass, lean mass and fat mass. All body composition outcomes were assessed with dual energy X-ray absorptiometry (DXA), using either Hologic QDR 1000W® or QDR 1500® (Hologic, Waltham, MA, USA) densitometers. Body composition measurements were obtained at the 3-day visit (mean 4.9 ± 1.1 days from fracture), 10-day visit (mean 11.9 ± 2.7 days from fracture) and 2-month visit (mean 68.9 ± 9.3 days from fracture) on the same densitometer at each visit for each participant. In order to account for the potential influence of post-surgical swelling on lean and fat mass around the site of the hip fracture [17], the lean mass and fat mass in the non-fractured leg were doubled and used in place of corresponding fracture-side values when calculating the total body composition figures. This technique has been used to account for surgical swelling in previous hip fracture studies [18, 19].
Covariates
A wide variety of potential confounders of short-term changes in body composition after hip fracture were assessed. These included age at the time of fracture, history of osteoporosis, education and a host of medical complications that were assessed after hip fracture. Please see Supplementary data, available at Age and Ageing online, Appendix SI for more information on the specific complications and their prevalence in this sample.
Statistical analyses
Descriptive analyses were performed to characterise the study population and assess the short-term changes in the mean body composition after hip fracture. The time from fracture was estimated by using day of hospitalisation as the starting point was treated as a categorical variable (Day 3, Day 10 or 2 months) in all analyses. The treating time from fracture as a continuous variable did not alter the analyses and these results are not reported. Longitudinal regression analysis of post-fracture body composition was conducted using mixed models with an exchangeable covariance matrix and robust standard errors. Random effects were assumed to have a normal distribution. The following variables were considered as potential covariates in the models to adjust for baseline characteristics: age, education, history of osteoporosis and medical complications (confusion, urinary tract infection, pressure sores, pneumonia and acute delirium). The inclusion of these covariates did not reduce the standard error of the estimates and only the unadjusted regression model results are reported. A sensitivity analysis was also conducted to compare findings among the subgroup of participants with data from all three time points (n = 33) to participants with data from at least one time point (n = 155). No meaningful differences were uncovered and the subgroup analyses are not reported. Associations with P ≤ 0.05 were considered statistically significant. All analyses were conducted using SAS version 9.1 (SAS Institute, Cary, NC, USA).
Results
Table 1 presents the descriptive characteristics of the study population at each visit. One hundred and fifty-five female hip fracture patients with a mean age of 80.7 [standard deviation (SD) = 7.4] years and mean education of 11.6 (SD = 3.3) years were studied. Eleven per cent of the sample reported a history of osteoporosis. Post-fracture medical complications that affected a meaningful number (>3%) of participants are reported.
Table 1.
Participant characteristics
| Variable (units) | Mean (SD) (n) |
||
|---|---|---|---|
| Day 3 | Day 10 | 2 Months | |
| Age at fracture (years) | 80.7 (7.5) (155) | – | – |
| Education (years) | 11.6 (3.3) (142) | – | – |
| History of osteoporosis (% Yes) | 11.1% (155] | – | – |
| Confusion (% Yes) | 18.1% (154) | – | – |
| Urinary tract infection (% Yes) | 7.8% [154) | – | – |
| Pneumonia (% Yes) | 3.9% (154) | – | – |
| Pressure sores (% Yes) | 3.9% (154) | – | – |
| Acute delirium (% Yes) | 3.2% (155) | – | – |
| Body composition outcomes | |||
| Total body mass (kg) | 56.0 (10.4) (91) | 56.2 (11.1) (126) | 54.9 (10.6) (103) |
| Lean mass (kg) | 38.0 (5.1) (91) | 38.8 (6.2) (126) | 36.7 (5.2) (103) |
| Fat mass (kg) | 16.5 (6.4) (91) | 15.7 (6.5) (126) | 16.5 (6.2) (103) |
| Total hip bone mineral density (g/cm2) | 0.59 (0.11) (96) | 0.58 (0.12) (120) | 0.58 (0.11) (93) |
| Femoral neck bone mineral density (g/cm2) | 0.55 (0.09) (96) | 0.54 (0.09) (121) | 0.53 (0.08) (93) |
Figures 1 and 2 illustrate the mean trajectories of the body composition outcomes during the 2 months after hip fracture as predicted by the regression models. More detail on the regression results is provided in Supplementary data are available in Age and Ageing online, Appendix SII.
Figure 1.
Body mass outcomes after hip fracture. Square represents point estimate, upper bar represents point estimate + standard error and lower bar represents point estimate − standard error.
Figure 2.
Bone mineral density outcomes after hip fracture. Square represents point estimate, upper bar represents point estimate + standard error and lower bar represents point estimate − standard error.
Discussion
This was the first study to rigorously assess the potential changes in body composition as soon as 10 days after hip fracture. The deleterious short-term changes in body composition previously noted to occur by 2 months post-fracture were confirmed in this analysis. The findings of this study also suggest that the bulk of these changes occur between 10 days and 2 months after the injury.
There were a number of strengths of this study that contribute to the potential clinical implications offered by these novel data. Corrective hip fracture surgery was performed on all study participants and all of the body composition measurements were assessed after surgery. The fact that all participants underwent corrective surgery is an important feature of the study as major surgical procedures induce weight loss and unfavourable body composition changes, which are often confounded by oedema around the surgical site. Several measures were taken to minimise the effect of post-surgical oedema on body composition estimates. Lean mass and fat mass on the non-operative leg were doubled and substituted for lean mass and fat mass on the fractured leg when calculating the total body mass. This substitution has been employed in previous studies and is believed to reduce the effect of regional oedema occurring around the site of surgery on lean mass estimates [18, 19].
There were also several notable limitations to this study. While a sensitivity analysis revealed no statistically significant differences in changes in body composition among the full sample (n = 155) and participants with data at all three time points (n = 33), future studies should be mindful of the challenges of acquiring body composition data from functionally compromised hip fracture patients. Despite the efforts to account for surgical swelling described previously, there was likely some residual impact on the changes in lean mass from 3- to 10 days post-fracture. However, a review of the influence of water content on body composition as measured by DXA suggests that these results are unlikely to be explained by fluid shifts alone. It is believed that changes in the water content of 5% are likely to affect DXA estimates of body fat by only 1–2.5% [20].
While further study is warranted, the detrimental changes in body composition known to occur by 2 months after hip fracture do not appear to meaningfully occur within the first 10 days after the injury. These novel findings might ultimately help inform both the optimal timing of initiation as well as the specific therapeutic approach of future pharmacological, dietary and physical activity interventions and ultimately contribute to enhanced study compliance and improved outcomes after hip fracture.
Key points.
Deleterious changes in body composition have been noted during the year after hip fracture and associated with adverse outcomes, but potential changes in body composition occurring shortly after hip fracture have not been rigorously studied to date.
While this study confirmed the detrimental changes in body composition by 2 months after hip fracture that had been noted previously in smaller studies, there were no significant changes in body composition revealed from 3- to 10 days post-fracture.
These findings may help inform the optimal timing of interventions aimed at improving body composition and related outcomes after hip fracture.
Conflicts of interest
Dr Magaziner reports consulting agreements with Novartis, Ammonett and OrgaNext, and grant funding from Eli Lilly. Dr Miller is a full-time employee of GlaxoSmithKline.
Funding
This work was supported by National Institutes of Health grants (grant numbers R37 AG009901, T32 AG00262). The financial sponsor played no role in the design, execution, analysis and interpretation of data or writing of the study.
Supplementary data
Supplementary data mentioned in the text is available to subscribers in Age and Ageing online.
References
- 1.Centers for Disease Control and Prevention. 2006. National Hospital Discharge Survey http://www.cdc.gov/nchs/data/ad/ad371.pdf. 2 October 2012, date last accessed.
- 2.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–13. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 3.Bass E, French DD, Bradham DD, Rubenstein LZ. Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol. 2007;17:514–9. doi: 10.1016/j.annepidem.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 4.Deakin DE, Boulton C, Moran CG. Mortality and causes of death among patients with isolated limb and pelvic fractures. Injury. 2007;38:312–7. doi: 10.1016/j.injury.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Lawrence VA, Hilsenbeck SG, Noveck H, et al. Medical complications and outcomes after hip fracture repair. Arch Intern Med. 2002;162:2053–7. doi: 10.1001/archinte.162.18.2053. [DOI] [PubMed] [Google Scholar]
- 6.Jiang HX, Majumdar SR, Dick DA, et al. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20:494–500. doi: 10.1359/JBMR.041133. [DOI] [PubMed] [Google Scholar]
- 7.Karlsson MK, Nilsson JA, Sernbo I, et al. Changes of bone mineral mass and soft tissue composition after hip fracture. Bone. 1996;18:19–22. doi: 10.1016/8756-3282(95)00422-x. [DOI] [PubMed] [Google Scholar]
- 8.Fox KM, Magaziner J, Hawkes WG, et al. Loss of bone density and lean body mass after hip fracture. Osteoporos Int. 2000;11:31–5. doi: 10.1007/s001980050003. [DOI] [PubMed] [Google Scholar]
- 9.Karlsson MK, Obrant KJ, Nilsson BE, Johnell O. Changes in bone mineral, lean body mass and fat content as measured by dual energy X-ray absorptiometry: a longitudinal study. Calcif Tissue Int. 2000;66:97–9. doi: 10.1007/s002230010020. [DOI] [PubMed] [Google Scholar]
- 10.Stevens JA, Olson S. Reducing falls and resulting hip fractures among older women. Morb Mort Wkly Rep. 2000;49(RR-2):3–12. [PubMed] [Google Scholar]
- 11.Visser M, Harris TB, Fox KM, et al. Change in muscle mass and muscle strength after a hip fracture: relationship to mobility recovery. J Gerontol Med Sci. 2000;55A:M434–40. doi: 10.1093/gerona/55.8.m434. [DOI] [PubMed] [Google Scholar]
- 12.Suzuki T, Yoshida H. Low bone mineral density at femoral neck is a predictor of increased mortality in elderly Japanese women. Osteoporos Int. 2010;21:71–9. doi: 10.1007/s00198-009-0970-6. [DOI] [PubMed] [Google Scholar]
- 13.Binder EF, Brown M, Sinacore DR, et al. Effects of extended outpatient rehabilitation after hip fracture: a randomized controlled trial. J Am Med Assoc. 2004;292:837–46. doi: 10.1001/jama.292.7.837. [DOI] [PubMed] [Google Scholar]
- 14.Eriksen EF, Lyles KW, Colón-Emeric CS, et al. Antifracture efficacy and reduction of mortality in relation to timing of the first dose of zoledronic acid after hip fracture. J Bone Miner Res. 2009;24:1308–13. doi: 10.1359/jbmr.090209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boonen S, Orwoll E, Magaziner J, et al. Once-yearly zoledronic acid in older men compared with women with recent hip fracture. J Am Geriatr Soc. 2011;59:2084–90. doi: 10.1111/j.1532-5415.2011.03666.x. [DOI] [PubMed] [Google Scholar]
- 16.Orwig DL, Hochberg M, Yu-Yahiro J, et al. Delivery and outcomes of a yearlong home exercise program after hip fracture: a randomized controlled trial. Arch Intern Med. 2011;171:323–31. doi: 10.1001/archinternmed.2011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giangregorio LM, Webber CE. Effects of metal implants on whole-body dual energy x-ray absorptiometry measurements of bone mineral content and body composition. Can Assoc Radiol J. 2003;54:305–9. [PubMed] [Google Scholar]
- 18.Miller R, Shardell M, Hicks G, et al. Association between interleukin-6 and lower extremity function after hip fracture—the role of muscle mass and strength. J Am Geriatr Soc. 2008;56:1050–6. doi: 10.1111/j.1532-5415.2008.01708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Monaco M, Vallero F, Di Monaco R, et al. Muscle mass and functional recovery in women with hip fracture. Am J Phys Med Rehabil. 2006;85:209–15. doi: 10.1097/01.phm.0000200387.01559.c0. [DOI] [PubMed] [Google Scholar]
- 20.Lohman TG, Harris M, Teixeira PJ, et al. Assessing Body Composition and Changes in Body Composition: Another Look at Dual-Energy X-ray Absorptiometry. Ann N Y Acad Sci. 2000;904:45–54. doi: 10.1111/j.1749-6632.2000.tb06420.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.