Abstract
Perceived control has been proposed to be a general psychological vulnerability factor that confers an elevated risk for developing anxiety disorders, but there is limited research examining perceived control during cognitive-behavioral therapies (CBT). The present study examined whether treatment resulted in improvements in perceived control, and the indirect effects of CBT on changes in symptoms of obsessive-compulsive disorder, social phobia, generalized anxiety disorder, and panic disorder via changes in perceived control. Participants (n = 606) were a large clinical sample presenting for treatment at an outpatient anxiety disorders clinic. Participants completed a series of self-report questionnaires and a structured clinical interview at an intake evaluation and at two follow-up assessments 12 and 24 months later, with the majority of participants initiating CBT between the first two assessments. Results of latent growth curve models indicated that individuals initiating CBT subsequently reported large increases in perceived control and significant indirect effects of treatment on intraindividual changes in each of the four anxiety disorders examined via intraindividual changes in perceived control. These results suggest that the promotion of more adaptive perceptions of control is associated with recovery from anxiety disorders. Furthermore, the consistent finding of indirect effects across the four anxiety disorders examined underscores the transdiagnostic importance of perceived control in predicting CBT outcomes.
Keywords: perceived control, anxiety, CBT, treatment outcome, transdiagnostic
Perceptions of control have long been considered an important determinant of mental health (Rotter, 1954, 1966). Whereas early theories focused on the importance of globalized perceptions of control, contemporary theories emphasize perceptions of control regarding aversive emotional experiences as crucial factors in the development of anxiety disorders (Barlow, 2002). Within the triple vulnerabilities model of psychopathology, perceived control is defined in terms of evaluations of control over internal emotional experiences, and external threats or stressful experiences (Barlow, 2002). Diminished perceptions of control over aversive events and emotional experiences are posited to be a generalized psychological vulnerability factor that develops due to early experiences such as a controlling family environment during childhood that fails to foster autonomy (Chorpita & Barlow, 1998). Diminished perceptions of control initially function as a mediator of the relationship between negative early experiences and anxiety, but over time become a relatively crystallized trait that moderates the influence of environmental stressors on the expression and development of anxiety (Barlow, 2002). Perceived control is therefore thought to be an important etiological factor with transdiagnostic implications for conferring an elevated risk of developing an anxiety disorder (Barlow, 2002; Suarez, Bennett, Goldstein, & Barlow, 2009).
Research to date has supported the contention that perceived control is an important risk factor across the anxiety disorders. Deficits in perceived emotional control have been shown to predict higher levels of panic disorder (e.g., Bentley, Gallagher, Boswell, Gorman, Shear, Woods & Barlow, 2013; White, Brown, Somers, & Barlow, 2006), obsessive-compulsive disorder (e.g., Moulding & Kyrios, 2007; Moulding, Kyrios, Doron, & Nedeljkovic, 2009), posttraumatic stress disorder (e.g., Vujanovic, Marshall, Gibson & Zvolensky, 2010; Vujanovic, Zvolensky, & Bernstein, 2008), social phobia (e.g., Glick & Orsillo, 2011; Hofmann, 2005), generalized anxiety disorder (e.g., Cannon & Weems, 2010; Stapinski, Abbott, & Rapee, 2010), and trait measures of anxiety (e.g., Brown, White, Forsyth, & Barlow, 2004; Rapee, Craske, Brown, & Barlow, 1996). A recent meta-analysis of the perceived control literature revealed large associations between perceived control and trait measures of anxiety, and moderate to large associations between perceived control and disorder-specific measures of anxiety (Gallagher, Bentley, & Barlow, 2013). The largest effects in this meta-analysis were found for perceived control and generalized anxiety disorder, but results indicated that perceived control is a robust predictor of each of the anxiety disorders examined, and that these effects were not moderated by sample characteristics such as gender, ethnicity, or the use of clinical vs. non-clinical samples.
The importance of perceived control as a transdiagnostic correlate of anxiety disorder symptoms is therefore well-established. However, the role of changes in perceived control as a potential predictor of recovery from anxiety disorders during treatment is not yet well understood. Cognitive-behavior therapies (CBT) are currently considered the gold standard psychological treatment for anxiety disorders, and although differences exist between different CBT protocols across the anxiety disorders, the common components of CBT protocols should result in the promotion of more adaptive perceptions of control. First, psychoeducation regarding the nature of anxiety is an important early component of CBT protocols and provides a foundation for helping patients develop a better understanding of the nature of anxiety, which could in turn promote increases in perceived control regarding emotional experiences. Second, cognitive reappraisal strategies are another standard component of CBT that should help patients to identify their maladaptive perceptions of control regarding emotional experiences and to then work on developing more balanced and adaptive perceptions of control. Finally, exposure exercises are a common component of most CBT protocols for anxiety disorders and may also provide an important means of promoting adaptive perceptions of control. Exposure exercises typically involve behavioral experiments that help patients to develop an increased tolerance of uncomfortable feelings by confronting and disconfirming their negative expectations related to feared stimuli. Together, these common components of CBT (Barlow, 2008) may serve to promote increases in perceived control regarding emotional experiences in individuals suffering from anxiety disorders. The increased perceptions of control that may develop during treatment could, in turn, play an important role in promoting and predicting treatment outcome by influencing how individuals may approach, experience, and respond to anxiety and stressful experiences that may evoke anxiety. However, to date there has been limited research examining the potential role of perceived control during CBT.
One notable exception is a recent study that examined the role of perceived control as a mediator in the treatment of panic disorder (Meuret, Rosenfield, Seidel, Bhaskara, & Hofmann, 2010). This study examined whether perceived control functioned as a nonspecific mediator of two distinct treatment protocols for panic disorder (cognitive training and capnometry-assisted respiratory training) in a randomized controlled trial of 47 individuals meeting DSM-IV criteria for panic disorder. The results indicated that both treatment protocols produced increases in perceived control and that increases in perceived control during treatment mediated the effects of treatment on panic disorder symptom severity. Particularly noteworthy was the finding that the mediating role of perceived control was maintained even after controlling for treatment modality-specific mediators (e.g., respiratory rate). Although these results provide promising evidence that perceived control may be an important mediator of recovery from anxiety disorders, the findings are limited to panic disorder. The extent to which perceived control mediates the effects of CBT for other anxiety disorders (e.g., social phobia; Hofmann, 2000) remains uncertain, despite theories that posit it to be a transdiagnostic contributor to anxiety disorders.
The goal of the present study was to determine whether perceived control functions as a transdiagnostic predictor of recovery from anxiety disorders following a course of CBT. Specifically, we were interested in examining (1) whether initiating CBT leads to increases in perceived control in a diverse sample of treatment-seeking individuals with anxiety disorders, (2) whether CBT has an indirect effect on anxiety symptoms via perceived control, and (3) whether the indirect effect of CBT on anxiety symptoms via perceived control is consistently present and of a similar magnitude across disorders. We hypothesized that (1) individuals initiating CBT would report large increases in perceived control relative to those individuals who did not initiate treatment, (2) that there would be significant indirect effects of CBT on intraindividual changes in anxiety symptoms via intraindividual changes in perceived control and (3) that evidence of the indirect effect of perceived control would be consistent across the four anxiety disorders we examined: social phobia, panic disorder with or without agoraphobia, generalized anxiety disorder, and obsessive-compulsive disorder.
Method
Participants and Procedure
The sample consisted of 606 outpatients who presented for assessment or treatment at the Center for Anxiety and Related Disorders (CARD)1 between October, 1996 and January, 2002. The majority (62.9%) of participants was female. The average age of participants at the intake assessment was 34.72 years (SD = 11.89, range = 18 to 74). The majority of participants identified as Caucasian (89%), with the remaining identifying as African-American (4%), Asian (3%), or Latino/Hispanic (3%). The institutional review board of Boston University approved all study procedures.
Participants completed a series of self-report questionnaires and a structured clinical interview at three time points: intake (T1), 12-month follow-up (T2), and 24-month follow-up (T3). The 12-month follow-up (T2), and 24-month follow-up (T3) assessments were conducted regardless of whether participants initiated treatment at CARD and were scheduled relative to when they completed their intake interview at CARD. Diagnoses at intake were established using the Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994), a semistructured interview designed to ascertain reliable diagnosis of the DSM–IV anxiety, mood, somatoform, and substance use disorders and to screen for the presence of other conditions (e.g., psychotic disorders). Patients were reevaluated at the two follow-up assessments using the follow-up version of the ADIS-IV (ADIS-IV-FU), which is identical to the ADIS-IV-L except that (a) the sections assessing past diagnoses are omitted, and (b) a section is included to assess treatments received since intake. Both versions of the ADIS-IV provide dimensional ratings of the key and associated features of disorders (0–8 ratings); such features are dimensionally rated regardless of whether a formal DSM–IV diagnosis is under consideration. A reliability study of a subset of the current sample (n = 362), which had two independent administrations of the ADIS–IV–L, indicated good to excellent interrater agreement for social phobia (κ = .77), panic disorder with or without agoraphobia (κ = .79), generalized anxiety disorder (κ = .65), and obsessive-compulsive disorder (κ = .75; Brown, Dinardo, Lehman, & Campbell, 2001).
The majority (76.2%) of participants chose to initiate CBT treatment at CARD following the initial assessment. The CBT treatment provided at CARD consisted of a time-limited course (typically a maximum of 16 sessions) of a specific CBT protocol for individuals’ principal diagnosis (e.g., Mastery of your anxiety and panic, Barlow & Craske, 2006, for individuals with panic disorder). This treatment was delivered by a mix of predoctoral and postdoctoral therapists, with the majority of treatment delivered in individual sessions. Individuals who initiated treatment at CARD were asked about the use of specific techniques during treatment at the 12-month follow-up (T2) assessment. 23.1% reported the use of relaxation, 32.3% reported the use of breathing control techniques (e.g., diaphragmatic breathing), 72.0% reported the use of cognitive restructuring techniques, 58.4% reported the use of situational exposure exercises, 11.3% reported the use of interoceptive exposure exercises, 10.7% reported the use of imaginal exposure exercises, and 16.7% reported the use of strategies to prevent safety behaviors. The remaining 144 (23.8%) of participants did not initiate CBT at CARD and were included in our analyses as a control condition.
Measures
Generalized anxiety disorder
The latent variable of Generalized Anxiety Disorder (GAD) was created using three ADIS–IV dimensional rating measures (all 0–8 scales): (a) the mean of excessiveness of worry in eight areas (e.g., work/school, physical health), (b) a single rating of difficulty controlling worry, and (c) the mean of frequency and severity ratings of the six symptoms comprising the DSM–IV associated symptom criterion of GAD.
Panic disorder with agoraphobia
The latent variable of Panic Disorder with Agoraphobia (PDA) was formed using two self-report questionnaires and one clinical rating measure. The self-report questionnaires were the Agoraphobia and Interoceptive subscales of the Albany Panic and Phobia Questionnaire (Rapee, Craske, & Barlow, 1994/1995; Brown, White, & Barlow, 2005). The clinician-rated measure of PDA was the sum of ADIS-IV dimensional ratings of agoraphobic avoidance of 23 situations that individuals with panic disorder commonly fear entering (e.g., public transportation, elevators).
Obsessive-compulsive disorder
The latent variable of Obsessive-Compulsive Disorder (OCD) was formed using two self-report questionnaires and two clinician rated measures. The self-report questionnaires were the Doubting and the Checking subscales of the Maudsley Obsessive-Compulsive Inventory (MOCl; Hodgson & Rachman, 1977). These two subscales were chosen from the five subscales of the MOCI because they do not contain any overlapping items and because they have previously been shown to have favorable psychometric properties (Emmelkamp, 1988). The two clinician-rated measures were the mean of the nine ADIS-IV dimensional ratings of the severity of obsessions and the mean of the six ADIS-IV dimensional ratings of the severity of compulsions.
Social phobia
The latent variable of Social Phobia (SOC) was formed using two self-report questionnaires and one clinical rating measure. The self-report questionnaires were (a) the Social Interaction Anxiety Scale (Mattick & Clarke, 1998; cf. E. J. Brown et al., 1997) and (b) the Social Phobia Scale of the Albany Panic and Phobia Questionnaire (Rapee, Craske, & Barlow, 1994/1995; cf. Brown, White, & Barlow, 2005). In addition, patients’ fear of 13 social situations (e.g., speaking with unfamiliar people, initiating a conversation) was rated by the clinician during administration of the ADIS–IV–L and ADIS–IV–FU (0 = no fear to 8 = very severe fear).
Perceived control
The latent variable of Perceived Control was constructed using the three subscales (Emotion Control, Threat Control, Stress Control) of the revised anxiety control questionnaire (ACQ-R; Brown, White, Forsyth, & Barlow, 2004) as indicators. Previous factor analytic work has demonstrated that the three lower-order facets of control load on a higher-order factor of Perceived Control (Brown et al., 2004). All analyses in the present study focused on the higher order construct of Perceived Control, with the subscales of the ACQ-R merely being used as indicators of this higher order construct in the latent variable analyses. Descriptive statistics for the ACQ-R across time by diagnosis are presented in Table 1.
Table 1.
Perceived Control Means Across Time by Diagnosis and Treatment Status at Initial and Follow-up Assessments
| Time | PDA (n = 219 ) | GAD (n = 131) | SOC (n = 251) | OCD (n = 72) | Full Sample (n = 593) | Initiated CBT (n=445) | No CBT (n=139) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Initial Assessment | 30.82 | 10.29 | 29.24 | 9.77 | 30.75 | 11.19 | 30.74 | 11.20 | 32.88 | 11.36 | 33.05 | 11.20 | 32.83 | 11.49 |
| 12 Month Follow-up | 42.39 | 12.26 | 40.63 | 11.85 | 40.17 | 12.62 | 39.61 | 12.04 | 42.43 | 12.71 | 43.54 | 12.55 | 38.94 | 12.69 |
| 24 Month Follow-up | 44.91 | 13.50 | 42.42 | 14.09 | 39.92 | 14.82 | 39.82 | 15.03 | 43.46 | 13.88 | 44.50 | 13.52 | 40.10 | 13.62 |
Note: PDA = Panic Disorder with or without Agoraphobia; GAD = Generalized Anxiety Disorder; SOC = Social Phobia; OCD = Obsessive-Compulsive Disorder. Reported n's indicate number of individuals in each category at initial assessment.
Data Analysis
All analyses were conducted using a latent variable software program and maximum-likelihood minimization functions (Mplus 5.0; Muthén & Muthén, 1998–2007). Attrition was negligible at T2 (7%), but increased to 50% at T3. There were no differences in attrition at T3 between those who initiated CBT treatment at CARD and those who did not initiate treatment (χ2 (df = 1) 1.53, p =.24). Thus, missing data were accommodated in all models using direct maximum likelihood (Allison, 2003; Raykov, 2005). Goodness of fit of the models was evaluated using the root-mean-square error of approximation (RMSEA; Steiger, 1990) and its 90% confidence interval (CI), the Tucker–Lewis index (TLI; Tucker & Lewis, 1973), the comparative fit index (CFI; Bentler, 1990), and the standardized root-mean-square residual (SRMR; Jöreskog & Sörbom, 1996). Acceptable model fit was defined in part by the criteria forwarded by Hu and Bentler (1999): RMSEA values close to 0.06 or below, CFI and TLI values close to .95 or above, and SRMR values close to .08 or below. In instances in which competing models were nested, comparative fit was evaluated with nested χ2 tests (χ2diff). The acceptability of the models was further evaluated by the presence or absence of salient localized areas of strains in the solutions (e.g., modification indices) and the strength and interpretability of the parameter estimates. The marker variable method was used to define the metric of latent variables in all models. The latent variables of GAD, SOC, PDA, and OCD were estimated for the entire sample of participants in all analyses.
Diagnostic Status Across Time
As assessed by the ADIS-IV, the rates of current clinical disorders for the four disorders of interest in this study at the intake, 12 months, and 24 month evaluations were as follows: social phobia, 42%, 28%, and 26%; panic disorder with or without agoraphobia, 38%, 17.1%, and 15.1%; generalized anxiety disorder (excluding DSM-IV hierarchy rules), 34%, 22%, and 20%, and obsessive-compulsive disorder, 12%, 7.5%, and 4.7%. Although not the focus of the present study, mood disorders (i.e., major depression, dysthymic disorder, depressive disorder not otherwise specified; 36%), and specific phobias (20%) were also common at the initial evaluation.
Results
Perceived Control and Anxiety at Intake
We began by examining the relationship between perceived control and anxiety at the intake assessment. A confirmatory factor analysis (CFA) model was estimated in which the latent variables of Perceived Control, OCD, PDA, SOC, and GAD were allowed to freely covary with one another. The model fit for this CFA was acceptable: χ2 (df = 91) = 334.84, p < .01, RMSEA = 0.07 (90% CI 0.06 – 0.07), TLI = 0.93, CFI = .94. All loadings were statistically significant and an examination of modification indices did not suggest any model revisions that were substantively meaningful. The correlations among the latent constructs are presented in Table 2. As expected, the results indicated significant negative associations between Perceived Control and each of the four anxiety disorders examined (r's ranged from −.32 to −.50). The magnitude of the associations between Perceived Control and anxiety disorder factors ranged from medium effects (PDA) to large effects (SOC and GAD). An examination of the confidence intervals of the effect sizes indicated that the association between Perceived Control and PDA at intake (r = −.32, 95% CI −.22 : −.41) was significantly smaller than the associations between Perceived Control and SOC, GAD, and OCD. These results support our hypothesis that perceived control is a transdiagnostic correlate of anxiety, but suggest that the effect of perceived control on anxiety symptom severity may vary across disorders.
Table 2.
Correlations Among Latent Variables of Perceived Control, Obsessive-Compulsive Disorder, Social Phobia, Generalized Anxiety Disorder, and Panic Disorder with or without Agoraphobia at Intake Evaluation
| Variable | Perceived Control | PDA | GAD | SOC | OCD |
|---|---|---|---|---|---|
| Perceived Control | -- | ||||
| PDA | −.32*** | -- | |||
| GAD | −.50*** | .13** | -- | ||
| SOC | −.50*** | .06 | .26*** | -- | |
| OCD | −.46*** | .12* | .35*** | .29*** | -- |
Note: n = 606
p < .05
p < .01
p < .001
PDA = Panic Disorder with or without Agoraphobia; GAD = Generalized Anxiety Disorder; SOC = Social Phobia; OCD = Obsessive-Compulsive Disorder.
Longitudinal Measurement Models
As a precursor to examining the relationships between perceived control and anxiety across time, we next examined a series of longitudinal measurement models in order to establish measurement invariance of the five constructs of interest. The demonstration of measurement invariance is crucial for ensuring that change in longitudinal models represents true change in the latent constructs rather than change in the measurement of the latent constructs. Baseline models were first estimated in which residual covariances were specified between indicators of the same variable across time (e.g., ACQ-Threat1, ACQ-Threat2, ACQ-Threat3), but no constraints were placed on factor loadings or indicator intercepts. The next model for each construct tested the invariance of the factor loadings across time, with the final model testing the invariance of the indicator intercepts across time. The evaluation of measurement invariance was conducted using nested χ2 tests, with nonsignificant results indicating measurement invariance. Modifications to each measurement model were included when necessary based on modification indices.
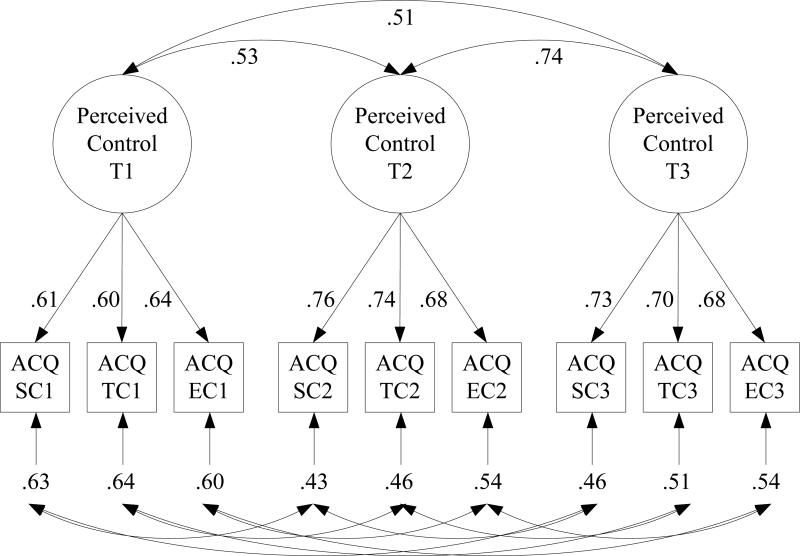
Results from the final measurement models for each latent construct are presented in Table 3. As an example, the results of the longitudinal measurement model for Perceived Control are presented in Figure 1. All standardized factor loadings were strong (λ ranging from .51 to .92) and statistically significant (p < .001). Model fit for each of the longitudinal measurement models was excellent. For each latent construct, the longitudinal measurement models indicated partial measurement invariance (i.e., at least one time-invariant indicator in addition to the marker indicator; Brown, 2006; Byrne, Shavelson, & Muthén, 1989), thereby providing the foundation for examining the temporal relationships in these constructs.
Table 3.
Longitudinal Measurement Models of Perceived Control, Generalized Anxiety Disorder, Panic Disorder, Social Phobia, and Obsessive-Compulsive Disorder
| Factor Loading | T1 | T2 | T3 | Model Constraint |
|---|---|---|---|---|
| Perceived Control | ||||
| ACQ-SC | .613 | .756 | .734 | All held equal except intercept of ACQ-EC at T1-T3. Model fit: χ2 (df = 21) = 31.52, p = .07, RMSEA = 0.03 (90% CI = 0.00–0.05), TLI = 0.99, CFI = .99. |
| ACQ-EC | .602 | .676 | .676 | |
| ACQ-TC | .636 | .736 | .700 | |
|
Panic Disorder with or without Agoraphobia | ||||
| APPQ-A | .893 | .896 | .885 | All held equal except loadings of ADIS Ag-score at T1-T3. Model fit: χ2 (df = 18) = 39.95, p = .002, RMSEA = 0.05 (90% CI = 0.03–0.06), TLI = 0.99, CFI = .99. |
| APPQ-I | .697 | .705 | .692 | |
| ADIS-Ag score | .742 | .734 | .759 | |
|
Generalized Anxiety Disorder | ||||
| ADIS-EX | .844 | .856 | .878 | All held equal except intercept of ADIS–As at T1 Model fit: χ2 (df = 22) = 23.44, p = .38, RMSEA = 0.01 (90% CI = 0.00–0.04), TLI = 1.0, CFI = 1.0 |
| ADIS-CO | .888 | .918 | .919 | |
| ADIS-AS | .763 | .743 | .741 | |
|
Obsessive-Compulsive Disorder | ||||
| ADIS-Obsessions | .556 | .631 | .587 | All held equal except loadings of MOCI-Doubting at T1-T3. Model fit: χ2 (df = 43) = 80.79, p < .001, RMSEA = 0.04 (90% CI= 0.03–0.05), TLI = 0.98, CFI = .99 |
| ADIS-Compulsions | .678 | .739 | .689 | |
| MOCI-Doubting | .509 | .576 | .644 | |
| MOCI-Checking | .772 | .769 | .763 | |
|
Social Phobia | ||||
| SIAS | .911 | .889 | .903 | All held equal except intercept of APPQ-S at T1-T3, loading of APPQ-S at T2. Model fit: χ2 (df = 20) =52.56, p < .001, RMSEA = 0.05 (90% CI = 0.04–0.07), TLI = 0.99, CFI =.99 |
| ADIS-S | .849 | .864 | .859 | |
| APPQ-S | .898 | .864 | .880 | |
Note: n = 606 for all models; The first variable listed for each construct served as the marker variable. Factor loadings obtained from the completely standardized solutions. ACQ-SC = Stress Control subscale of the Anxiety Control Questionnaire-Revised; ACQ-TC = Threat Control subscale of the Anxiety Control Questionnaire-Revised; ACQ-EC = Emotion Control subscale of the Anxiety Control Questionnaire-Revised; APPQ-A = Agoraphobia subscale of the Albany Panic and Phobia Questionnaire; APPQ-I = Interoceptive subscale of the Albany Panic and Phobia Questionnaire; ADIS-Ag score = ADIS-IV rating of agoraphobic avoidance; ADIS-EX = ADIS-IV ratings of excessiveness of worry; ADIS-CO = ADIS-IV ratings of uncontrollability of worry; ADIS-AS = ADIS-IV ratings of associated symptoms of generalize anxiety disorder; ADIS-Obsessions = average ADIS-IV rating of nine obsessions; ADIS-IV Compulsions = average ADIS-IV rating of six compulsions; MOCI-Doubting = Doubting subscale of the Maudsley Obsessive-Compulsive Inventory; MOCI-Checking = Checking subscale of the Maudsley Obsessive-Compulsive Inventory; SIAS = Social Interaction Anxiety Scale; ADIS–S = ADIS–IV ratings of situational social fear; APPQ–S = Social Phobia Scale of Albany Panic and Phobia Questionnaire; RMSEA = root-mean-square error of approximation; CFI = comparative fit index; TLI = Tucker–Lewis index; SRMR = standardized root mean square residual; T1 (Time 1) = intake; T2 (Time 2) = 12-month follow-up; T3 (Time 3) = 24-month follow-up.
Figure 1.
Longitudinal measurement model of perceived control. Completely standardized parameter estimates are provided (all significant at p < .001). To simplify presentation, estimates of correlated residuals are not presented. ACQ-SC = Stress Control subscale of the Anxiety Control Questionnaire-Revised; ACQ-TC = Threat Control subscale of the Anxiety Control Questionnaire-Revised; ACQ-EC = Emotion Control subscale of the Anxiety Control Questionnaire-Revised; T1 (Time 1) = intake; T2 (Time 2) = 12-month follow-up; T3 (Time 3) = 24-month follow-up.
Temporal Variation in Perceived Control and Anxiety
The test-retest correlations from the longitudinal measurement models are presented in Table 4. As expected, the magnitude of the test-retest correlation from T1-T2 was smaller than the test-retest correlation from T2-T3 for each latent construct. The differences between these test-retest correlations likely reflect the fact that the majority of individuals sought treatment between the first and second assessment, and the majority of change in each construct occurred between the first and second assessment. The magnitude of the T1-T2 test-retest correlation for Perceived Control (r = .53; 95% CI .43 : .62) was smaller than the T1-T2 test-retest correlation of the four anxiety disorder constructs (rs = .66 to .90), which suggests that perceived control was the least temporally stable latent construct during the period in which the majority of participants completed treatment.
Table 4.
Temporal Variation in Latent Variables of Perceived Control, Generalized Anxiety Disorder, Panic Disorder, Social Phobia, and Obsessive-Compulsive Disorder
| Parameter Estimate | PC | PDA | GAD | OCD | SOC |
|---|---|---|---|---|---|
| Test-retest correlations | |||||
| T1-T2 | .53*** | .75*** | .66*** | .90*** | .82*** |
| T2-T3 | .73*** | .93*** | .69*** | .89*** | .94*** |
| T1-T3 | .51*** | .71*** | .58*** | .90*** | .79*** |
| Effect Size (d) | 0.74 | 0.47 | 0.42 | 0.46 | 0.39 |
| Growth Intercepta | |||||
| Variance | 4.16*** | 168.65*** | 58.88*** | 5.85*** | 294.71*** |
| Growth Slope | |||||
| Mean | 2.39*** | −5.96*** | −3.79*** | −1.07*** | −6.30*** |
| Variance | 3.51*** | 71.83*** | 15.63** | 0.24 | 90.51*** |
| T2 Slope loading | .90 | .94 | .92 | .91 | .90 |
| Intercept-Slope | |||||
| Covariance | 0.42 | −60.14*** | −.12.80** | −0.95* | −78.49*** |
| Correlation | .11 | −.55*** | −.42*** | −.80*** | −.48*** |
| Model fit | |||||
| χ2 (df) | 40.50 (24) | 40.84 (20) | 26.96 (24) | 81.83 (45) | 53.02 (22) |
| RMSEA | 0.03 | 0.04 | 0.01 | 0.04 | 0.05 |
| RMSEA 90% CI | 0.01 : 0.05 | 0.02 : 0.06 | 0.00 : 0.04 | 0.02 : 0.05 | 0.03 : 0.07 |
| CFI | .99 | .99 | 1.0 | .99 | .99 |
| TLI | 0.98 | 0.99 | 1.0 | 0.98 | 0.99 |
| SRMR | .04 | .03 | .03 | .04 | .02 |
Note:
mean of intercept fixed at zero; n = 606 for all models
p < .05
p < .01
p < .001
PC = Perceived Control; PDA = Panic Disorder with or without Agoraphobia; GAD = Generalized Anxiety Disorder; SOC = Social Phobia; OCD = Obsessive-Compulsive Disorder; RMSEA = root mean square error of approximation; CFI = comparative fit index; TLI = Tucker–Lewis index; SRMR = standardized root mean square residual; T1 (Time 1) = intake; T2 (Time 2) = 12-month follow-up; T3 (Time 3) = 24-month follow-up.
Effect sizes (Cohen's d) for the total change in perceived control and the four anxiety disorder constructs across the two year assessment period were calculated using the parameter estimates from the longitudinal measurement models. These effect sizes are presented in Table 4 and quantify the overall magnitude of change in perceived control and the four anxiety disorder constructs for participants who both initiated CBT treatment (76.2%), and those who did not initiate treatment at CARD (23.8%). The effect sizes for the four anxiety outcomes were all small to medium (range = 0.39 to 0.47) based on Cohen's (1988) standards, while the effect size for perceived control approached a large effect (0.74). These effect sizes provide additional evidence that individual levels of perceived control changed more over the course of the assessments than did the four anxiety disorder outcomes.
Univariate unconditional latent growth curve models were specified to model intraindividual change in perceived control and the four anxiety outcomes. Because the majority of change in perceived control and the four anxiety outcomes occurred between the first two assessments, a non-linear growth model was used for each construct by specifying the slope factor loadings of the T1, T2, and T3 assessments as 0, *, and 1, respectively (* = freely estimated). The Intercept factors for these models were therefore centered at the initial assessment, with the mean of the Slope factor representing the total change in the latent constructs over the three assessments. The intercepts of the Perceived Control and anxiety disorder construct factors at each time point were fixed to zero and the residual variances of the Perceived Control and anxiety disorder construct factors were constrained to equality in each model to aid with model identification and parsimony.
The results of the unconditional latent growth curve model for each construct can be seen in Table 4. Model fit was excellent for each of the latent growth models. The means of the Slope parameters were statistically significant (ps <.001) in each model, indicating that, on average, participants reported an increase in perceived control across time and a decrease in anxiety symptoms across time. With the exception of OCD, the variances of the Slope parameters were statistically significant (ps <.001) in each model, indicating significant interindividual variability in the degree of change in perceived control and anxiety. Finally, results in Table 4 indicate that, with the exception of Perceived Control, the Intercept and Slope factors were significantly correlated. These results indicate that individuals with higher initial levels of each anxiety outcome tended to show greater reductions in these symptoms across time, but there was no relationship between initial levels of perceived control and intraindividual changes in perceived control over time.
Effect of Treatment on Perceived Control and Anxiety
The effect of initiating CBT treatment on perceived control (Hypothesis 1) and anxiety was examined next using conditional latent growth curve models in which the Slope factors of Perceived Control and the four anxiety outcomes were regressed on a treatment dummy code variable (0 = no CARD treatment, 1 = initiated CARD treatment). These analyses allowed us to examine differential patterns of change between the 76.2% of our sample that initiated CBT treatment at CARD and the 23.8% of our sample that did not initiate CBT treatment at CARD. The Slope factor was also regressed on the Intercept factor in each model to control for initial levels of each construct. The results of these models can be seen in Table 5. The model fit for each model was excellent. With the exception of OCD, the effect of treatment on the Slope was statistically significant. The direction of these effects indicated that, holding initial symptom levels constant, individuals who initiated treatment at CARD reported greater increases in perceived control and greater reductions in anxiety symptoms than individuals who did not receive treatment at CARD. Table 5 also includes the partially standardized path coefficient for the effect of treatment on the Slope factors, which can be interpreted in the Cohen's d effect size metric.
Table 5.
Effects of Treatment on Temporal Variation in Latent Variables of Perceived Control, Generalized Anxiety Disorder, Panic Disorder, Social Phobia, and Obsessive-Compulsive Disorder
| Parameter Estimate | PC | PDA | GAD | OCD | SOC |
|---|---|---|---|---|---|
| Treatment Effect on Slope | |||||
| Unstandardized | 1.33*** | −2.66*** | −1.51* | −0.30 | −4.53*** |
| Standard Error | 0.40 | 0.87 | 0.74 | 0.19 | 1.06 |
| Partially Standardized | 0.71*** | −0.32*** | −0.38* | −0.63 | −0.47*** |
| Completely Standardized | .30*** | −.13*** | −.16* | −.27 | −.20*** |
| Treatment and Intercept | |||||
| Covariance | −0.00 | −0.04 | −0.22 | −0.04 | 0.28 |
| Correlation | −.00 | −.01 | −.07 | −.04 | −.04 |
| Model fit | |||||
| χ2 (df) | 55.28 (31) | 45.64 (27) | 39.12 (31) | 90.50 (55) | 58.80 (29) |
| RMSEA | 0.03 | 0.03 | 0.02 | 0.03 | 0.04 |
| RMSEA 90% CI | 0.02 : 0.05 | 0.02 : 0.05 | 0.00 : 0.04 | 0.02 : 0.04 | 0.03 : 0.06 |
| CFI | .98 | .99 | 1.0 | .99 | .99 |
| TLI | 0.98 | 0.99 | 1.0 | 0.98 | 0.99 |
| SRMR | .04 | .02 | .03 | .04 | .02 |
Note: n = 606 for all models
p < .05
** p < .01
p < .005
PC = Perceived Control; PDA = Panic Disorder with or without Agoraphobia; GAD = Generalized Anxiety Disorder; SOC = Social Phobia; OCD = Obsessive-Compulsive Disorder; RMSEA = root mean square error of approximation; CFI = comparative fit index; TLI = Tucker–Lewis index; SRMR = standardized root mean square residual.
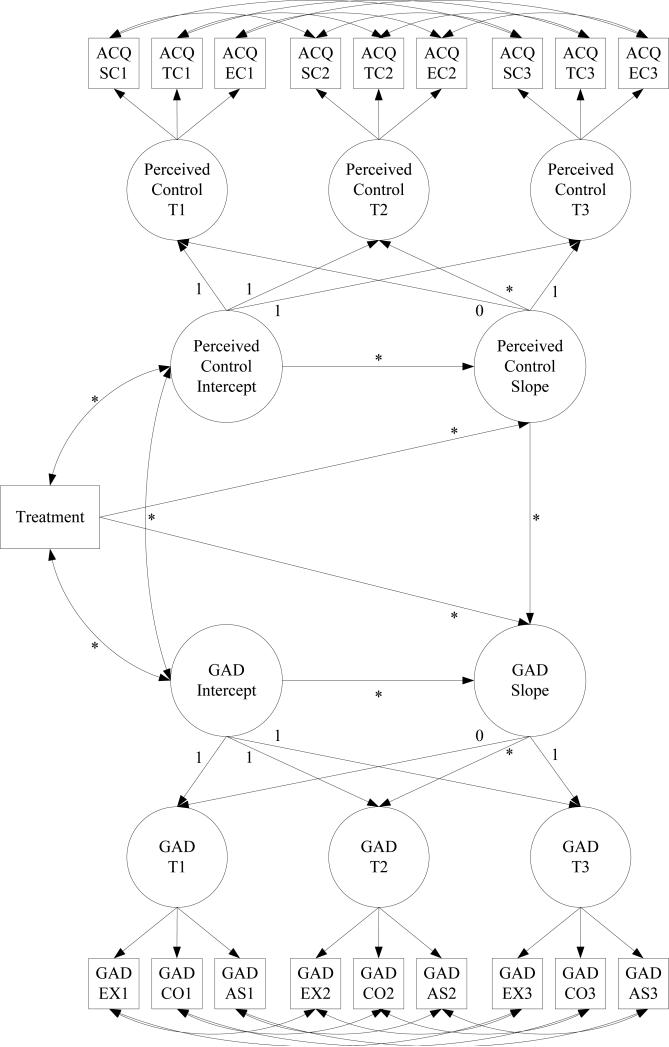
Indirect Effect of Treatment on Anxiety via Perceived Control using Parallel Process LGCs
Our final analyses examined the indirect effect of treatment on intraindividual changes in the four anxiety disorder outcomes via intraindividual changes in perceived control (Hypothesis 2), and whether these indirect effects were consistent across the four anxiety disorder outcomes (Hypothesis 3). Four parallel process latent growth curve models were specified to evaluate the indirect effect of perceived control with each anxiety disorder outcome. An example of these models is presented in Figure 2. For each model, the Slope of the anxiety disorder outcome was regressed onto the treatment dummy code variable, the Slope of Perceived Control, and the Intercept of the anxiety disorder outcome. The Slope of Perceived Control was regressed onto the treatment dummy code and the Perceived Control Intercept, and the perceived control and anxiety Intercepts were allowed to freely covary. The indirect effect (ab) was then calculated using the product of the effect of treatment on changes in Perceived Control (a) and the effect of changes in Perceived Control on changes in the anxiety disorder outcomes (b). The significance of the indirect effect was evaluated first with the product of coefficients approach by using the Mplus MODEL INDIRECT command. Bias-corrected bootstrapped (using 10,000 resamplings) confidence intervals of the indirect effect were then calculated within Mplus for each model.
Figure 2.
Example Parallel-Process Latent Growth Curve Model Examining the Indirect Effect of Treatment on Generalized Anxiety Disorder via Perceived Control. * = freely estimated parameter. ACQ-SC = Stress Control subscale of the Anxiety Control Questionnaire-Revised; ACQ-TC = Threat Control subscale of the Anxiety Control Questionnaire-Revised; ACQ-EC = Emotion Control subscale of the Anxiety Control Questionnaire-Revised; GAD = Generalized Anxiety Disorder; GAD-EX = ADIS-IV ratings of excessiveness of worry; GAD-CO = ADIS-IV ratings of uncontrollability of worry; GAD = ADIS-IV ratings of associated symptoms of generalized anxiety disorder; T1 (Time 1) = intake; T2 (Time 2) = 12-month follow-up; T3 (Time 3) = 24-month follow-up.
The results of these models are presented in Table 6. The model fit for each of the four parallel process models was acceptable. The effects of treatment on the Perceived Control Slope (a) and the effects of changes in Perceived Control on changes in anxiety (b) were both statistically significant (ps < .001) in each model. The indirect effect of treatment on change in anxiety via change in perceived control was also statistically significant in each model according to both the product of coefficients test and the bias-corrected bootstrapped confidence intervals of the indirect effect. The completely standardized estimates of the indirect effect all ranged from −.20 to −.26, suggesting that the magnitude of the indirect effect of treatment on anxiety via perceived control was similar for each of the four anxiety outcomes. The proportion of explained variance (R2) in the anxiety Slope factors ranged from .78 to .84, indicating that the combined effect of the treatment dummy code variable, initial status in the anxiety outcomes, and the Slope factor of perceived control together predicted approximately 80% of the variance in the four anxiety disorder outcomes examined. Alternative models were specified in which the anxiety Slope factors were only regressed on treatment and initial status in the anxiety disorder outcomes to determine the proportion of variance that was specifically due to the inclusion of the perceived control Slope as a predictor of the anxiety Slope factors. These incremental R2 are presented in Table 6 and ranged from .53 to .59. The very large magnitude of these incremental effects underscore the importance of intraindividual changes in perceived control in predicting intraindividual changes in anxiety following treatment.
Table 6.
Results from Parallel-Process Latent Growth Curve Models Examining the Indirect Effect of Treatment on Generalized Anxiety Disorder, Panic Disorder, Social Phobia, and Obsessive-Compulsive Disorder via Perceived Control
| Parameter Estimate | PDA | GAD | SOC | OCD |
|---|---|---|---|---|
| Treatment → Perceived Control Slope (a) | ||||
| Unstandardized | 1.37*** | 1.43*** | 1.40*** | 1.51*** |
| Standard Error | 0.37 | 0.38 | 0.41 | 0.44 |
| Completely Standardized | .27*** | .28** | .26*** | .32*** |
| Perceived Control Slope → Anxiety Slope (b) | ||||
| Unstandardized | −2.98*** | −1.39*** | −3.17*** | −.27*** |
| Standard Error | 0.60 | 0.34 | 0.72 | 0.10 |
| Completely Standardized | −.76*** | −.80*** | −.77*** | −.80*** |
| Treatment → Anxiety Slope (c’) | ||||
| Unstandardized | 1.35 | 0.40 | −0.13 | 0.19 |
| Standard Error | 1.42 | 0.85 | 1.65 | 0.12 |
| Completely Standardized | .07 | .04 | −.01 | .12 |
| Indirect Effect | ||||
| ab | −4.07** | −1.99** | −4.43** | −.40* |
| Standard error (ab) | 1.41 | .76 | 1.64 | .11 |
| Bias Corrected Bootstrapped 95% CI of ab | −1.94 : −7.56 | −.87 : −3.91 | −1.95 : −8.34 | −.12 : −.86 |
| Completely Standardized ab | −.20*** | −.22** | −.20** | −.26* |
| Variance Explained (R2) | ||||
| Perceived Control Slope | .08 | .08 | .08 | .11 |
| Anxiety Slope | .83 | .78 | .82 | .84 |
| Incremental R2 of Perceived Control Slope on Anxiety Slope | .53 | .58 | .56 | .59 |
| Model fit | ||||
| χ 2 | 226.97*** | 305.15*** | 317.79*** | 369.20*** |
| df | 136 | 140 | 139 | 197 |
| RMSEA | 0.03 | 0.04 | 0.046 | .038 |
| RMSEA 90% CI | 0.03 : 0.04 | 0.04 : 0.05 | 0.04 : 0.05 | 0.03 : 0.04 |
| CFI | .98 | .96 | .97 | .96 |
| TLI | 0.98 | 0.95 | 0.96 | 0.95 |
| SRMR | .04 | .06 | .05 | .07 |
Note: n = 606 for all models
p < .05
p < .01
p < .001
PDA = Panic Disorder with or without Agoraphobia; GAD = Generalized Anxiety Disorder; SOC = Social Phobia; OCD = Obsessive-Compulsive Disorder; RMSEA = root-mean-square error of approximation; CFI = comparative fit index; TLI = Tucker–Lewis index; SRMR = standardized root-mean-square residual.
Discussion
There is extensive research demonstrating the importance of perceived control as a transdiagnostic vulnerability factor for anxiety disorders (Barlow, 2002; Gallagher et al., 2013). Consistent with our hypotheses, previous research, and the triple vulnerabilities model, we found moderate to large associations between perceived control and the four anxiety disorder constructs examined at the initial evaluation. These findings support the notion that perceived control regarding emotional experiences is an important, transdiagnostic predictor of symptom severity across the anxiety disorders.
The present study also builds upon previous research by longitudinally examining the associations between perceived control and anxiety disorders following the initiation of CBT. Previous research has examined the role of perceived control during CBT for panic disorder (Meuret et al., 2010), but the present study is the first to examine the role of perceived control during the treatment of multiple anxiety disorders. Our results indicate that, in a large, diagnostically diverse clinical sample of patients presenting to an anxiety disorders specialty clinic, those individuals who initiate a course of CBT subsequently report more adaptive perceptions of control. Although the absence of repeated assessments of perceived control during treatment precludes more definitive conclusions regarding the timing of change, our results are nevertheless promising. As hypothesized, intraindividual changes in perceived control across two years of follow-up assessments were robust predictors of intraindividual changes in symptoms of OCD, PDA, SOC, and GAD. Also as hypothesized, our results demonstrated indirect effects of CBT treatment on intraindividual changes in symptoms of OCD, PDA, SOC, and GAD via intraindividual changes in perceived control. The most noteworthy aspects of these findings were the consistency of the evidence of indirect effects across the four anxiety disorders examined and the very large magnitude of the observed effects of changes in perceived control on changes in anxiety symptoms.
These results are consistent with past empirical examinations (Meuret et al., 2010) and theoretical discussions (Hofmann, 2000) of the role of perceived control as a potential mechanism of change of CBT for anxiety disorders, although our use of concurrent assessments of perceived control and the anxiety disorder outcomes precludes definitive conclusions about whether perceived control functioned as a mechanism of change of CBT in the present study. The strengths of the present study include the use of a large and diverse clinical sample and the use of assessment procedures that involved both self-report and clinician-rated measures of anxiety. These characteristics strengthen conclusions regarding the relevance of perceived control as a transdiagnostic predictor of CBT outcomes, as the reported effects are unlikely to be artificially inflated by method effects and do not appear to be unique to a particular anxiety disorder.
Limitations and Future Directions
Although the present study provides promising evidence that perceived control may be an important predictor of recovery from anxiety disorders following CBT, certain limitations of our study should be noted. The primary limitation is the timing of the assessments. Although the use of one and two year follow-up assessments provides valuable information about the longitudinal course of perceived control and anxiety, the absence of repeated assessments during the active treatment phase precludes more definitive conclusions regarding whether perceived control is truly a mechanism of change of CBT for anxiety disorders. Temporality of assessments is a crucial issue in the identification of mechanisms of change (Kazdin, 2007) as without evidence that a proposed mechanism changes prior to an outcome, it is impossible to determine whether the proposed mechanism might instead merely be a corollary or consequence of change in the outcome rather than an important determinant of change. It will therefore be important for future research to use more intensive data collection schedules to examine the course of intraindividual changes in perceived control during CBT.
Another important limitation involves the level of detail regarding the treatment that participants received in the present study. Treatment was coded as a dichotomous variable that simply reflected whether or not individuals chose to initiate treatment at CARD. Given that CARD is an anxiety disorder clinic specializing in the development and delivery of CBT protocols for anxiety disorders, it is reasonable to assume that any individual initiating treatment at CARD would have received some form of CBT through the clinic or an ongoing research study. However, exact information (e.g., treatment duration) about the specific treatment received by the participants in this study was not available, which prevents conclusions regarding the role of perceived control in promoting recovery during specific CBT treatment protocols. Previous research has suggested that perceived control may be a common mechanism of change across distinct CBT treatment protocols (Meuret et al., 2010), but it will be important for future research to examine in more detail whether the role of perceived control as a mechanism of change varies across distinct treatment protocols.
Another limitation relates to how the latent construct of GAD was modeled. Unlike the other three disorder constructs that were modeled using a combination of self-report and clinician-rated indicators from the ADIS-IV, the latent construct of GAD was modeled using exclusively ADIS-IV indicators. It is possible that these different methods of modeling the disorder constructs may have biased our findings. Finally, our findings are limited by the absence of any alternative mediators in the examinations of the indirect effects of perceived control on changes in anxiety. We chose to focus on perceived control in the present study given the previous theoretical and empirical work indicating the transdiagnostic relevance of perceived control across the anxiety disorders (Barlow, 2002; Gallagher et al., 2013), but it will be important for future studies to examine the effects of perceived control in conjunction with constructs thought to function as disorder-specific vulnerabilities (e.g., anxiety sensitivity for panic disorder).
Conclusions
There have been increasing efforts in recent years to identify mechanisms of change of empirically supported treatments as it has become clear that, although we have extensive evidence of efficacy for many treatments, relatively little is known about how or why our treatments produce change (Kazdin, 2007). The present study provides promising evidence that, in addition to playing an important role in the development of anxiety disorders, perceived control may play an important role in CBT for anxiety disorders. Although the present study did not include any examination of the effects of specific treatment protocols on perceived control, our results are consistent with recent trends in the development of treatment protocols for anxiety disorders. There is promising recent evidence of the utility of transdiagnostic treatment protocols for anxiety disorders such as the Unified Protocol (UP; Barlow et al., 2011; Ellard et al., 2010; Farchione et al., 2012). The UP was designed to target shared etiological factors such as perceived control and neuroticism that are thought to play an important role across emotional disorders (Allen, McHugh, & Barlow, 2009). Our results are consistent with the theoretical framework of the UP that emphasizes commonalities across the anxiety disorders, and also demonstrate the utility of focusing on constructs with transdiagnostic relevance such as perceived control.
Footnotes
Data from this sample was previously published in Brown (2007) and Naragon-Gainey et al., (in press). The Brown (2007) study focused on the role of temperament in predicting the longitudinal course of depression, social phobia, and generalized anxiety disorder. The Brown (2007) manuscript did not include any examination of perceived control, panic disorder, or obsessive-compulsive disorder, but certain preliminary analyses reported in the present study overlap with the 2007 manuscript as the latent variables of social phobia and generalized anxiety disorder are estimated using the same indicators that were used in Brown (2007). Specifically, results of the longitudinal measurement models (Table 2) and the individual latent growth curve models examining temporal variation (Tables 3/4) for the latent variables of social phobia and generalized anxiety disorder were previously reported. The Naragon-Gainey et al., (in press) study focused on the impact of anxiety disorders on functional impairment and did not include any examination of perceived control.
Conflicts of Interest Disclosure: None
Contributor Information
Matthew W. Gallagher, National Center for PTSD, VA Boston Healthcare System, & Boston University School of Medicine
Kristin Naragon-Gainey, University at Buffalo, The State University of New York.
Timothy A. Brown, Center for Anxiety and Related Disorders, Boston University
References
- Allen LB, McHugh RK, Barlow DH. Emotional disorders: A unified protocol. In: Barlow DH, editor. Clinical handbook of psychological disorders: A step-by-step treatment manual. 4th ed Guilford Press; New York: 2008. pp. 216–249. [Google Scholar]
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd ed. Guilford Press; New York: 2002. [Google Scholar]
- Barlow DH, editor. Clinical handbook of psychological disorders: A step-by-step treatment manual. 4th ed. Guilford Press; New York: 2008. [Google Scholar]
- Bentler PM. Comparative fit indices in structural equation models. Psychological Bulletin. 1990;28:97–104. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentley KH, Gallagher MW, Boswell JF, Gorman JM, Shear MK, Woods SW, Barlow DH. The interactive contributions of perceived control and anxiety sensitivity in panic disorder: A triple vulnerabilities perspective. Journal of Psychopathology and Behavioral Assessment. 2013;35:57–64. [Google Scholar]
- Brown EJ, Turovsky J, Heimberg RG, Juster HR, Brown TA, Barlow DH. Validation of the Social Interaction Anxiety Scale and the Social Phobia Scale across the anxiety disorders. Psychological Assessment. 1997;9:21–27. [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. Guilford Press; New York: 2006. [Google Scholar]
- Brown TA. Temporal course and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. Journal of Abnormal Psychology. 2007;116:313–328. doi: 10.1037/0021-843X.116.2.313. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM–IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Brown TA, White KS, Barlow DH. A psychometric reanalysis of the Albany Panic and Phobia Questionnaire. Behaviour Research and Therapy. 2005;43:337–355. doi: 10.1016/j.brat.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Brown TA, White KS, Forsyth JP, Barlow DH. The structure of perceived emotional control: Psychometric properties of a revised Anxiety Control Questionnaire. Behavior Therapy. 2004;35:75–99. [Google Scholar]
- Byrne BM, Shavelson RJ, Muthén B. Testing for the equivalence of factor covariance and mean structures: The issue of partial measurement invariance. Psychological Bulletin. 1989;105:456–466. [Google Scholar]
- Cannon MF, Weems CF. Cognitive biases in childhood anxiety disorders: Do interpretive and judgment biases distinguish anxious youth from their non-anxious peers? Journal of Anxiety Disorders. 2010;24:751–758. doi: 10.1016/j.janxdis.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Barlow DH. The development of anxiety: The role of control in the early environment. Psychological Bulletin. 1998;124:3–21. doi: 10.1037/0033-2909.124.1.3. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM–IV: Lifetime Version (ADIS–IV–L) Oxford University Press; New York: 1994. [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH. Unified Protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice. 2010;17:88–101. doi: 10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmelkamp PMG. Maudsley Obsessional-Compulsive Inventory. In: Hersen M, Bellack AS, editors. Dictionary of behavioral assessment techniques. Pergamon Press; New York: 1988. pp. 294–295. [Google Scholar]
- Farchione TF, Fairholme CF, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, Gallagher MW, Barlow DH. The unified protocol for the transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy. 2012;43:666–678. doi: 10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher MW, Bentley KH, Barlow DH. Perceived control and vulnerability to anxiety disorders: A meta-analytic review. 2013. Manuscript under review.
- Glick DM, Orsillo SM. Relationships among social anxiety, self-focused attention, and experiential distress and avoidance. Journal of Cognitive and Behavioral Psychotherapies. 2011;11:1–12. [Google Scholar]
- Hodgson RJ, Rachman SJ. Obsessional-compulsive complaints. Behaviour Research and Therapy. 1977;15:389–395. doi: 10.1016/0005-7967(77)90042-0. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Treatment of social phobia: Potential mediators and moderators. Clinical Psychology: Science and Practice. 2000;7:3–16. doi: 10.1093/clipsy/7.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG. Perception of control over anxiety mediates the relation between catastrophic thinking and social anxiety in social phobia. Behaviour Research and Therapy. 2005;43:885–895. doi: 10.1016/j.brat.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8: User's reference guide. Scientific Software International; Chicago: 1996. [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety fear. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Meuret AE, Rosenfield D, Seidel A, Bhaskara L, Hofmann SG. Respiratory and cognitive mediators of treatment change in panic disorder: Evidence for intervention specificity. Journal of Consulting and Clinical Psychology. 2010;78:691–704. doi: 10.1037/a0019552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore MC, Zebb BJ. The catastrophic misinterpretation of physiological distress. Behaviour Research and Therapy. 1999;37:1105–1118. doi: 10.1016/s0005-7967(98)00197-1. [DOI] [PubMed] [Google Scholar]
- Moulding R, Kyrios M. Desire for control, sense of control and obsessive-compulsive symptoms. Cognitive Therapy and Research. 2007;31:759–772. [Google Scholar]
- Moulding R, Kyrios M, Doron G, Nedeljkovic M. Mediated and direct effects of general control beliefs on obsessive compulsive symptoms. Canadian Journal of Behavioural Science. 2009;41:84–92. [Google Scholar]
- Muthén LK, Muthén BO. Mplus 5.0 [Computer software]. Author; Los Angeles: 1998–2007. [Google Scholar]
- Naragon-Gainey K, Gallagher MW, Brown TA. A longitudinal examination of psychosocial impairment across the anxiety disorders. Psychological Medicine. doi: 10.1017/S0033291713001967. (in press) [DOI] [PubMed] [Google Scholar]
- Rapee RM, Craske MG, Barlow DH. Assessment instrument for panic disorder that includes fear of sensation-producing activities: The Albany Panic and Phobia Questionnaire. Anxiety. 1994/1995);1:114–122. doi: 10.1002/anxi.3070010303. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Craske MG, Brown TA, Barlow DH. Measurement of perceived control over anxiety related events. Behavior Therapy. 1996;27:279–293. [Google Scholar]
- Raykov T. Analysis of longitudinal studies with missing data using covariance structure modeling with full-information maximum likelihood. Structural Equation Modeling. 2005;12:493–505. [Google Scholar]
- Rotter JB. Social learning and clinical psychology. Prentice-Hall; Englewood Cliffs, NJ: 1954. [Google Scholar]
- Rotter JB. Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs. 1966;80:1–28. [PubMed] [Google Scholar]
- Skinner EA. A guide to constructs of control. Journal of Personality and Social Psychology. 1996;71:549–570. doi: 10.1037//0022-3514.71.3.549. [DOI] [PubMed] [Google Scholar]
- Stapinski LA, Abbott MJ, Rapee RM. Fear and perceived uncontrollability of emotion: Evaluating the unique contribution of emotion appraisal variables to prediction of worry and generalized anxiety disorder. Behaviour Research and Therapy. 2010;48:1097–1104. doi: 10.1016/j.brat.2010.07.012. [DOI] [PubMed] [Google Scholar]
- Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Suárez L, Bennett S, Goldstein C, Barlow DH. Understanding anxiety disorders from a “triple vulnerabilities” framework. In: Antony MM, Stein MB, editors. Oxford handbook of anxiety and related disorders. Oxford; New York: 2009. pp. 153–172. [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:10. [Google Scholar]
- Vujanovic AA, Marshall EC, Gibson LE, Zvolensky MJ. Cognitive-affective characteristics of smokers with and without posttraumatic stress disorder and panic psychopathology. Addictive Behaviors. 2010;35:419–425. doi: 10.1016/j.addbeh.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Zvolensky MJ, Bernstein A. Incremental associations between facets of anxiety sensitivity and posttraumatic stress and panic symptoms among trauma-exposed adults. Cognitive Behaviour Therapy. 2008;37:76–89. doi: 10.1080/16506070801969039. [DOI] [PubMed] [Google Scholar]
- White KS, Brown TA, Somers TJ, Barlow DH. Avoidance behavior in panic disorder: The moderating influence of perceived control. Behaviour Research and Therapy. 2006;44:147–157. doi: 10.1016/j.brat.2005.07.009. [DOI] [PubMed] [Google Scholar]