Abstract
Purpose
To compare the tensile properties of a 3-0, 4-strand flexor tendon repair to a 4-0, 4 strand repair and a 4-0, 8-strand repair.
Methods
Following evaluation of the intrinsic material properties of the 2 core suture calibers most commonly used in tendon repair (3-0 and 4-0), we tested the mechanical properties of 40 cadaver flexor digitorum profundus tendons after zone II repair with one of 3 techniques: a 3-0, 4-strand core repair, a 4-0, 8-strand repair, or a 4-0, 4-strand repair. We compared results across suture caliber for the 2 sutures and across tendon repair methods.
Results
Maximum load to failure of 3-0 polyfilament caprolactam suture was 49% greater than that of 4-0 polyfilament caprolactam suture. The cross sectional area of 3-0 Supramid was 42% greater than that of 4-0 Supramid. The 4-0, 8 strand, repair produced greater maximum load to failure when compared to the 2 4-strand techniques. Load at 2 mm gap, stiffness, and work to yield were significantly greater in the 4-0, 8-strand repair when compared to the 3-0, 4-strand repair.
Discussion
In an ex vivo model, an 8-strand repair using 4-0 suture was 43% stronger than a 4-strand repair using 3-0 suture, despite the finding that 3-0 polyfilament caprolactam was 49% stronger than was 4-0 polyfilament caprolactam. These results suggest that, although larger caliber suture has superior tensile properties, the number of core suture strands across a repair site has an important effect on time zero, ex vivo flexor tendon repair strength.
Clinical Relevance
Surgeons should consider using techniques that prioritize multi-strand core suture repair over an increase in suture caliber.
Keywords: core suture, flexor tendon repair, intrasynovial, multi-strand repair, zone II
Introduction
Defining the optimal operative repair techniques for intrasynovial flexor tendon repair has been challenging. Prior investigations have demonstrated that the tensile properties of repair are directly related to suture caliber(1), number of strands that extend across the repair site(2–5), core suture depth(6, 7), and peripheral suture depth(8, 9). Further, suture repair techniques incorporating locked stitches, preloading of the core suture(10), and over-tensioning the core suture across the repair site(11) have been associated with improved tensile properties in repaired tendons. While many of the commonly used flexor tendon repair techniques appear to provide sufficient time zero tensile strength for the initiation of passive motion rehabilitation, enhancement of the mechanical properties of flexor tendon repair has been related to decreased risk of gap formation and repair failure (2–4, 6, 11, 12).
Superior values for time zero, ex vivo tensile properties in flexor tendon repair have been observed when a nonabsorbable 4-0 double-stranded (looped) suture is used to perform an 8-strand core suture repair method that employs a deep, 1.2-cm core suture purchase depth and a deep, 2-mm epitendinous suture purchase(12, 13). Although similar results were obtained in a recent in vivo study using a large animal model(12) , many surgeons prefer 4-strand repair techniques, presumably due to their familiarity and ease. With the understanding that both increased suture caliber and a greater number of strands crossing the flexor tendon repair site are known to improve repair mechanical properties, we questioned how the tensile properties of a flexor tendon repair with thicker suture and fewer strands across the repair site would compare with a thinner suture with a greater number of strands. We tested the null hypothesis that a 3-0, 4-strand repair would have similar tensile properties as a 4-0, 8-strand repair.
Methods
Study Design
Initially, we evaluated the 2 caliber sutures (3-0 versus 4-0 polyfilament caprolactam [Supramid, S. Jackson, Alexandria, VA] suture) that we planned to use in the experimental repairs. The sutures were mounted on a materials testing machine (Instron 5866, Instron, Norwood, MA) and tensioned at a strain rate of 1mm/s until failure. To minimize the effect of the knot on testing of the sutures, a jig consisting of a clamp and cylindrical spool was used (Figure 1). The low friction spool allowed for free rotation of the suture and allowed the strands to distribute the load evenly between strands. Mechanical properties were measured using previously described software code(13). Comparison of the 2 suture calibers was performed with 1, 2, 4, and 8 strands of suture in order to evaluate how the material properties of the suture influence the tensile properties of a clinically relevant tendon repair model.
Figure 1.
Apparatus for suture material properties testing
Fresh-frozen human upper limbs were obtained for the tendon repair portion of study. Flexor digitorum profundus tendons from the index, long, and ring finger were harvested from each limb. Each tendon (N=40) underwent surgical transection within zone II 40–55 mm proximal to its insertion. Repair, by one of 3 methods was then carried out. Using a stratified number generator that controlled for both digit type and repair method, each tendon was randomized to one of 3 repair techniques: 3-0 polyfilament caprolactam, 4-strand repair, 4-0 polyfilament caprolactam, 8-strand repair; or 4-0 polyfilament caprolactam, 4-strand repair. Post randomization analysis showed a similar distribution of tendons in each experimental group with respect to digit type. Each core repair method was supplemented with 5-0 monofilament polypropylene (Prolene, Ethicon, Somerville, NJ) running, unlocked peripheral epitendinous suture. Tendon cross sectional area was approximated as elliptical and measured using a laser micrometer 3–8 mm distal to the repair grasping loops. Mean cross sectional area was similar across experimental groups (4-0 4 strand, 12.1±3.6 mm; 3-0 4 strand, 12.5±3.4 mm; 4-0 8 strand, 11.2± 2.7mm, p> 0.05)
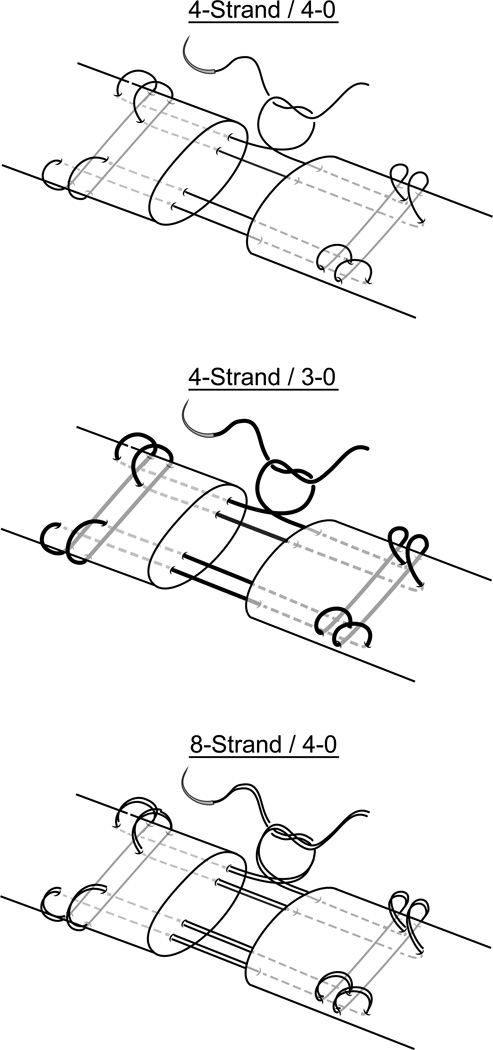
All tendons were repaired with core suture purchase of 1.0 cm and a peripheral suture purchase that extended 2 mm into the depth of the tendon stumps. Suture purchase depth was measured using Jameson medical calipers (Hayden Medical Inc., Santa Clarita, CA). Flexor tendon repairs were performed by 2 hand fellowship trained orthopedic surgeons using the technique described by Winters et al (5). Repair technique was technically equivalent across the 3 groups. The 8-strand repair differed only in the use of a double-stranded polyfilament caprolactam suture. Both 4-strand repair methods were performed using a single stranded suture (Figure 2). The repaired tendons were mounted into the materials testing machine using a custom grip to hold the distal phalanx and a triangle toothed grip for the proximal tendon stump. Tendons were then tensioned at a strain rate of 0.005/s until failure. Failure mode was recorded for all tendons. Tensile properties were recorded for the 3 repair techniques.
Figure 2.
Schematic representation of core suture repair technique.
Statistics
Sample size estimation for analysis of tendon repair methods was based on historical data from our laboratory, which found that n=8 per group was required to detect a clinically relevant change in maximum load (30%) between repair groups (alpha=0.05, beta=0.20).
Two-sided 1-way analysis of variance was used to evaluate the association between repair method and each mechanical property with significance defined at the alpha less than 0.05 level. For suture material properties testing, descriptive statistics were used to characterize the differences in mean and standard deviation for all outcome variables. Statistical analysis was performed using a 2-sided Student t-test with significance defined at the alpha less than 0.05 level.
Results
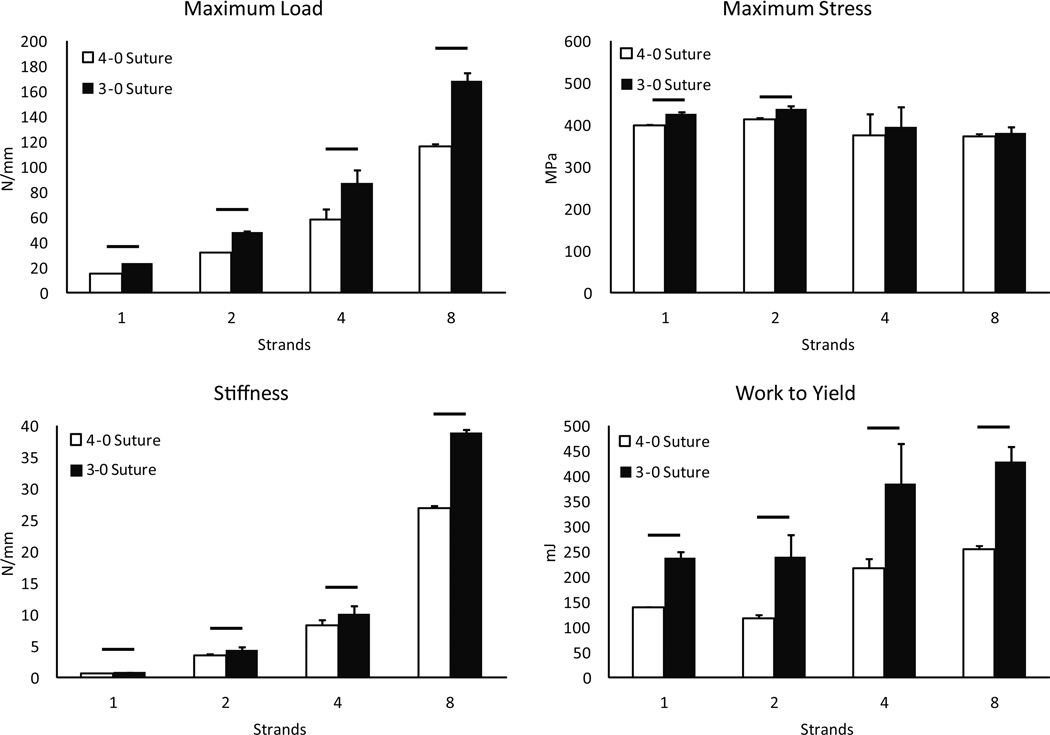
Suture testing comparison
Material properties for 3-0 and 4-0 polyfilament caprolactam are depicted in Figure 3. The cross sectional area of 3-0 polyfilament caprolactam is 142% of 4-0 polyfilament caprolactam (cross sectional area 0.0551 mm2 versus 0.0389 mm2, respectively). Maximum load to failure of 3-0 polyfilament caprolactam was 149% that of 4-0 polyfilament caprolactam (23.5 N versus 15.5 N, p=0.002).
Figure 3.
Material properties testing of polyfilament caprolactam.
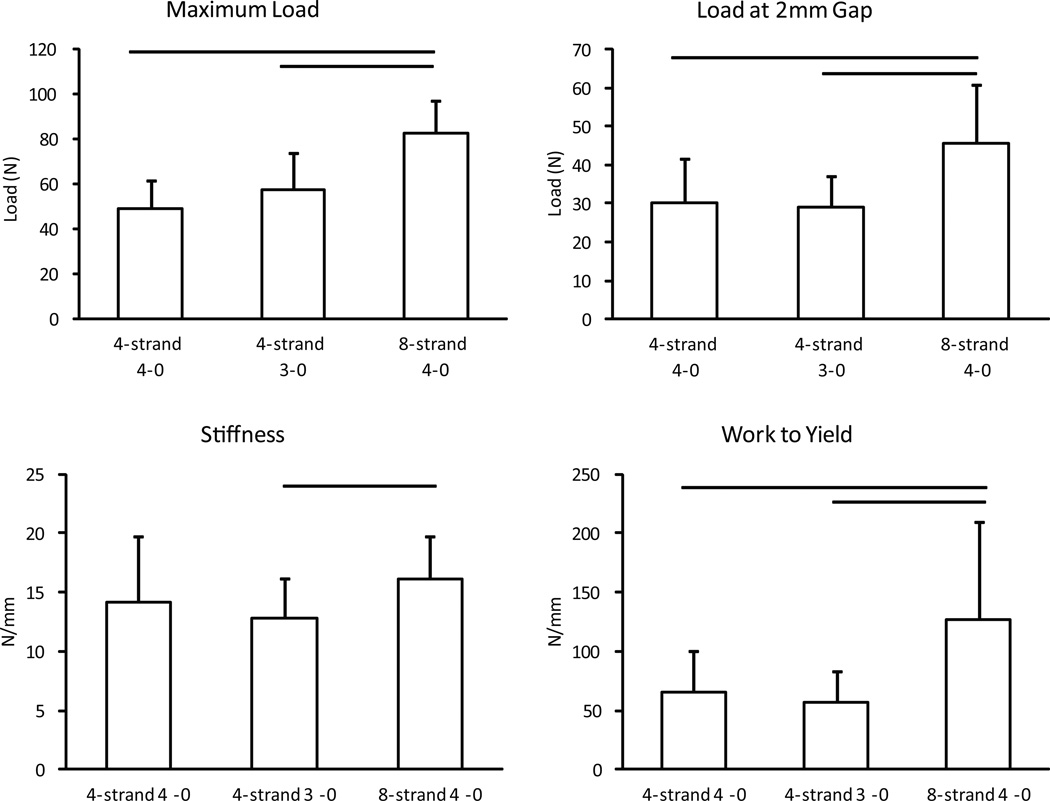
Flexor tendon repair comparison
Results of flexor tendon repair are shown in Figure 4. Linear regression modeling showed no correlation between maximum load and flexor tendon cross sectional area (R2= 0.01). Suture rupture was the cause of failure in the majority of repairs across all groups. Two repairs in the 3-0, 4 strand group and 1 repair in the 4-0, 8-strand group failed by a combination mechanism (partial suture rupture, partial suture pullout). No repairs in the 4-0, 4-strand group failed by suture pullout. The 4-0, 8-strand, looped repairs produced greater maximum load to failure when compared to the 3-0, 4-strand and 4-0, 4-strand techniques. Load at 2 mm gap, stiffness, and work to yield were significantly greater in the 4-0, 8-strand repair when compared to the 3-0, 4-strand repair. When comparing 3-0, 4-strand repair to 4-0, 4-strand repair, maximum load, load at 2 mm gap, stiffness and work to yield were not significantly increased.
Figure 4.
Mechanical properties by flexor tendon repair type.
Discussion
Previous investigations have highlighted a number of factors that are positively correlated with improved tensile properties of intrasynovial flexor tendon repair. Some studies have isolated the effect of a single variable such as suture caliber(1, 9), suture material (14, 15), repair technique(16–19), suture purchase(7, 8, 20), use of locked stitches(21, 22), degree of tensioning of the core suture repair(10, 11), or number of strands across the repair site(2, 5). Other authors have examined several factors together as a combined operative technique(12, 13). In practice, most surgeons use the technique that they find to be reproducible, technically feasible, and capable of producing satisfactory results. As such, a study that focuses on a practical decision-making dilemma regarding suture caliber and the number of core suture strands may be of considerable clinical importance.
Taras et al. showed in a cadaver study that 3-0 nonabsorbable braided polyethylene terephthalate (Ethibond, Ethicon, Somerville, NJ) repairs were 52% stronger than 4-0 braided polyethylene terephthalate repair and that there was a linear increase in mean repair tensile strength as suture caliber was increased from 5-0 to 2-0 without epitendinous suture(1). Our suture material property findings are similar to the findings of Taras et al., as we noted a 49% increase in suture strength when caliber was increased from 4-0 to 3-0. This finding suggests that the strength of a braided, non-absorbable suture is related to its cross sectional area.
Nelson et al. in an ex vivo model (13)and Fufa et al. in a clinically relevant in vivo model(12) demonstrated that superior tensile repair properties could be obtained by combining all of these repair principles. They found that core suture caliber, number of core suture strands, and peripheral suture purchase greatly affected tensile properties while core suture purchase and peripheral suture caliber were secondary factors. While informative, this investigation left unanswered the question regarding which of the repair technique factors is most important. The data provided in this experiment add to the findings of Nelson et al by demonstrating that an increase in the number of core suture strands from 4 to 8 overcomes the effect of strand caliber. These findings complement the conclusions of Winters et al that at an 8-strand repair is significantly stronger than a 4-strand repair at 3 weeks (49% greater ultimate load) and 6 weeks (117% greater ultimate load)(5).
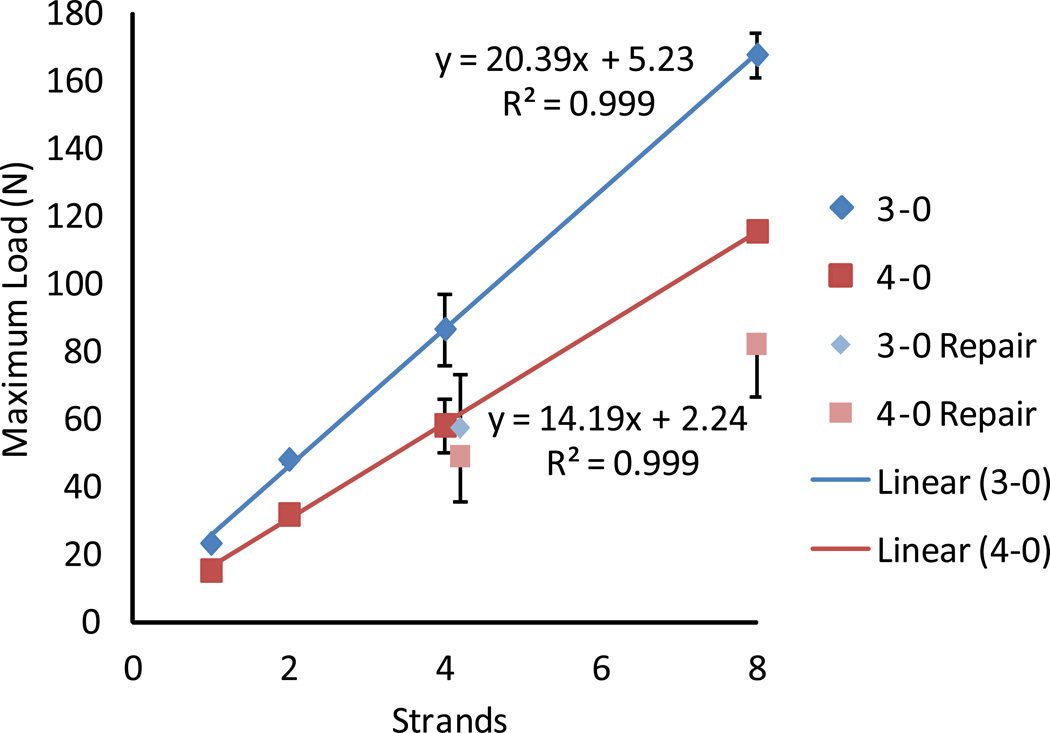
In clinical practice, an 8-strand flexor tendon repair with 3-0 suture is difficult to carry out, as the increase caliber may be disproportionately large compared to the cross sectional area of the intrasynovial tendon. Many surgeons still favor a 4-strand repair over an 8-strand repair. While this investigation confirmed the finding of other authors that the use of 3-0 suture is mechanically advantageous, it is noteworthy that in comparing techniques, a 4-0, 8-strand repair is 43% stronger than 3-0, 4-strand repair. Correlation of the suture material property testing with the tendon repair testing in this investigation helps provide insight into these findings. The results of suture material property testing are fairly intuitive--doubling the number of strands leads to roughly a doubling of the maximum load to failure. Conversely, increasing the suture caliber from 4-0 to 3-0 only increases the cross sectional area by 42%, leading to a nearly proportional increase in maximum load to failure (Table 1). In examining the suture repair data, load to failure of the 4-0, 8-strand repair and 3-0, 4-strand repair was 1.7 and 1.2 times that of 4-0, 4-strand repair, respectively. While the clinical repair mechanical property values do not reach the theoretical levels predicted by suture material properties testing, a similar trend is observed between repair models, suggesting a strong correlation between the flexor tendon repair tensile properties and the material properties of the suture used in the repairs (Figure 5).
Table 1.
Maximum Load to failure: Expected vs Empiric.
| Suture Caliber/ Strands |
Expected Max Load (N) |
Suture Empiric Max Load (N) |
Tendon Repair Empiric Max Load (N) |
|---|---|---|---|
| 4-0 4-strand | x | 58.4±7.7 (x) | 49.0±12.8 (x) |
| 3-0 4-strand | 1.4x | 86.9±10.8 (1.5x) | 57.4±16.2 (1.2x) |
| 4-0 8-strand | 2.0x | 115.8±2.0 (2.0x) | 82.2±15.0 (1.7x) |
Figure 5.
Correlation matrix of suture mechanical properties and flexor tendon repair tensile properties.
There are limitations to this study. In this ex vivo, cadaveric investigation, we tested time zero tendon repair tensile properties. As we have noted in previous studies, this model may not accurately represent the cyclical loading seen in vivo. No attempt was made to control for or account for differences in tendon gliding properties or other differences that may occur under physiologic conditions. In vivo studies would be beneficial to further examine the relative effect of suture caliber and number of strands in flexor tendon repair. Second, tendon repairs were performed by 2 surgeons. While both surgeons were hand fellowship trained and experienced in flexor tendon repair, surgeon effect on tendon repair strength was an unmeasured variable. The potential effect of surgeon on repair properties was minimized by ensuring that both surgeons fixed equal numbers of tendons in all 3 repair groups. Furthermore, using a similar 2 surgeon study design, Nelson et al. showed that while the effect of surgeon does play a role in tendon repair strength, the trends in relative repair strength among experimental groups for each surgeon were the same (13). Finally, we compared an 8-strand repair that used a double-stranded polyfilament caprolactam core suture to 2 4-strand repairs that used a single stranded suture. With double-stranded suture, 2 strands pass through the lacerated surface of the tendon at the same point, minimizing the tendon/suture interface. It is still unclear how the suture tendon interaction affects time zero tensile properties and how an increase of suture caliber or an increase in the number of suture strands interacting with the tendon at the repair site changes each factor’s contribution to repair strength. Brockardt et al. demonstrated in an ex vivo study that double-stranded polyfilament caprolactam and double-stranded long chain ultra-high molecular weight polyethylene (Fiberwire, Arthrex, Naples, FL) decreased force to 2 mm gap and decreased ultimate strength compared with single stranded polyfilament caprolactam and long chain ultra-high molecular weight polyethylene, respectively(23). Because of this, we felt that any effect of the double-stranded suture used in the 8-strand repair would serve to impair the tensile properties of the 8-strand repair. As such, this may further strengthen the observations in this study. Further studies that investigate the relative role of double-stranded suture in the setting of other surgical factors may enhance our understanding of how each factor affects overall repair performance.
Acknowledgments
Funding Sources: This publication was supported by grants from the National Institutes of Health (AR062947, RHG and ST) and the Washington University Institute of Clinical and Translational Sciences (UL1 TR000448, DAO), from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Taras JS, Raphael JS, Marczyk SC, Bauerle WB. Evaluation of suture caliber in flexor tendon repair. J Hand Surg. Am. 2001;26(6):1100–1104. doi: 10.1053/jhsu.2001.28946. [DOI] [PubMed] [Google Scholar]
- 2.Barrie KA, Tomak SL, Cholewicki J, Wolfe SW. The role of multiple strands and locking sutures on gap formation of flexor tendon repairs during cyclical loading. J Hand Surg Am. 2000;25(4):714–720. doi: 10.1053/jhsu.2000.9414. [DOI] [PubMed] [Google Scholar]
- 3.Dinopoulos HT, Boyer MI, Burns ME, Gelberman RH, Silva MJ. The resistance of a four- and eight-strand suture technique to gap formation during tensile testing: an experimental study of repaired canine flexor tendons after 10 days of in vivo healing. J Hand Surg Am. 2000;25(3):489–498. doi: 10.1053/jhsu.2000.6456. [DOI] [PubMed] [Google Scholar]
- 4.Gelberman RH, Boyer MI, Brodt MD, Winters SC, Silva MJ. The effect of gap formation at the repair site on the strength and excursion of intrasynovial flexor tendons. An experimental study on the early stages of tendon-healing in dogs. J Bone Joint Surg Am. 1999;81(7):975–982. doi: 10.2106/00004623-199907000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Winters SC, Gelberman RH, Woo SL, Chan SS, Grewal R, Seiler JG., 3rd The effects of multiple-strand suture methods on the strength and excursion of repaired intrasynovial flexor tendons: a biomechanical study in dogs. J Hand Surg. Am. 1998;23(1):97–104. doi: 10.1016/s0363-5023(98)80096-8. [DOI] [PubMed] [Google Scholar]
- 6.Lee SK, Goldstein RY, Zingman A, Terranova C, Nasser P, Hausman MR. The effects of core suture purchase on the biomechanical characteristics of a multistrand locking flexor tendon repair: a cadaveric study. J Hand Surg. Am. 2010;35(7):1165–1171. doi: 10.1016/j.jhsa.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Tang JB, Zhang Y, Cao Y, Xie RG. Core suture purchase affects strength of tendon repairs. J Hand Surg Am. 2005;30(6):1262–1266. doi: 10.1016/j.jhsa.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Diao E, Hariharan JS, Soejima O, Lotz JC. Effect of peripheral suture depth on strength of tendon repairs. J Hand Surg Am. 1996;21(2):234–239. doi: 10.1016/S0363-5023(96)80106-7. [DOI] [PubMed] [Google Scholar]
- 9.Barrie KA, Tomak SL, Cholewicki J, Merrell GA, Wolfe SW. Effect of suture locking and suture caliber on fatigue strength of flexor tendon repairs. J Hand Surg. Am. 2001;26(2):340–346. doi: 10.1053/jhsu.2001.22926. [DOI] [PubMed] [Google Scholar]
- 10.Vanhees M, Thoreson AR, Larson DR, Amadio PC, An KN, Zhao C. The effect of suture preloading on the force to failure and gap formation after flexor tendon repair. J Hand Surg. Am. 2013;38(1):56–61. doi: 10.1016/j.jhsa.2012.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu YF, Tang JB. Effects of tension across the tendon repair site on tendon gap and ultimate strength. J Hand Surg. Am. 2012;37(5):906–912. doi: 10.1016/j.jhsa.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Fufa DT, Osei DA, Calfee RP, Silva MJ, Thomopoulos S, Gelberman RH. The effect of core and epitendinous suture modifications on repair of intrasynovial flexor tendons in an in vivo canine model. J Hand Surg. Am. 2012;37(12):2526–2531. doi: 10.1016/j.jhsa.2012.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nelson GN, Potter R, Ntouvali E, Silva MJ, Boyer MI, Gelberman RH, et al. Intrasynovial flexor tendon repair: a biomechanical study of variations in suture application in human cadavera. J Orthop Res. 2012;30(10):1652–1659. doi: 10.1002/jor.22108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lawrence TM, Davis TR. A biomechanical analysis of suture materials and their influence on a four-strand flexor tendon repair. J Hand Surg. Am. 2005;30(4):836–841. doi: 10.1016/j.jhsa.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Zeplin PH, Zahn RK, Meffert RH, Schmidt K. Biomechanical evaluation of flexor tendon repair using barbed suture material: a comparative ex vivo study. J Hand Surg. Am. 2011;36(3):446–449. doi: 10.1016/j.jhsa.2010.11.031. [DOI] [PubMed] [Google Scholar]
- 16.Karjalainen T, He M, Chong AK, Lim AY, Ryhanen J. An analysis of the pull-out strength of 6 suture loop configurations in flexor tendons. J Hand Surg. Am. 2012;37(2):217–223. doi: 10.1016/j.jhsa.2011.10.039. [DOI] [PubMed] [Google Scholar]
- 17.Lee SK, Fajardo M, Kardashian G, Klein J, Tsai P, Christoforou D. Repair of flexor digitorum profundus to distal phalanx: a biomechanical evaluation of four techniques. J Hand Surg. Am. 2011;36(10):1604–1609. doi: 10.1016/j.jhsa.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 18.Trail IA, Powell ES, Noble J. The mechanical strength of various suture techniques. J Hand Surg. Br. 1992;17(1):89–91. doi: 10.1016/0266-7681(92)90019-x. [DOI] [PubMed] [Google Scholar]
- 19.Viinikainen A, Goransson H, Huovinen K, Kellomaki M, Rokkanen P. A comparative analysis of the biomechanical behaviour of five flexor tendon core sutures. J Hand Surg Br. 2004;29(6):536–543. doi: 10.1016/j.jhsb.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 20.Cao Y, Zhu B, Xie RG, Tang JB. Influence of core suture purchase length on strength of four-strand tendon repairs. J Hand Surg. Am. 2006;31(1):107–112. doi: 10.1016/j.jhsa.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Xie RG, Tang JB. Investigation of locking configurations for tendon repair. J Hand Surg. Am. 2005;30(3):461–465. doi: 10.1016/j.jhsa.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Wu YF, Tang JB. How much does a Pennington lock add to strength of a tendon repair? J Hand Surg Eur Vol. 2011;36(6):476–484. doi: 10.1177/1753193411403691. [DOI] [PubMed] [Google Scholar]
- 23.Brockardt CJ, Sullivan LG, Watkins BE, Wongworawat MD. Evaluation of simple and looped suture and new material for flexor tendon repair. J Hand Surg Eur Vol. 2009;34(3):329–332. doi: 10.1177/1753193408097319. [DOI] [PubMed] [Google Scholar]