Abstract
Gender-based violence (GBV) is widespread globally and has myriad adverse health effects but is vastly underreported. Few studies address the extent of reporting bias in existing estimates. We provide bounds for underestimation of reporting of GBV to formal and informal sources conditional on having experienced GBV and characterize differences between women who report and those who do not. We analyzed Demographic and Health Survey data from 284,281 women in 24 countries collected between 2004 and 2011. We performed descriptive analysis and multivariate logistic regressions examining characteristics associated with reporting to formal sources. Forty percent of women experiencing GBV previously disclosed to someone; however, only 7% reported to a formal source (regional variation, 2% in India and East Asia to 14% in Latin America and the Caribbean). Formerly married and never married status, urban residence, and increasing age were characteristics associated with increased likelihood of formal reporting. Our results imply that estimates of GBV prevalence based on health systems data or on police reports may underestimate the total prevalence of GBV, ranging from 11- to 128-fold, depending on the region and type of reporting. In addition, women who report GBV differ from those who do not, with implications for program targeting and design of interventions.
Keywords: gender-based violence, global prevalence, reporting
Editor's note:An invited commentary on this article appears on page 613, and the authors' response is published on page 619.
Globally, gender-based violence (GBV) is widespread. It is estimated that, worldwide, 30% of ever-partnered women aged 15 years and older have experienced physical and/or sexual intimate partner violence (IPV) in their lifetimes, with regional rates ranging from 16.3% in East Asia to 65.64% in Central sub-Saharan Africa (1). Adverse public health effects of GBV include exposure to sexually transmitted infections, gynecological fistula, unwanted pregnancy, psychological sequelae, chronic pain, physical disability, and substance abuse (2–8). Additionally, there are negative social and economic impacts of GBV on survivors and their families (9–12). Appropriate and effective policy responses to prevent and address the effects of GBV depend on an accurate and complete understanding of the prevalence, dynamics, and root causes. However, reliable data are often lacking.
Despite calls for more accurate data and comprehensive reporting systems (13), the magnitude of GBV, especially in situations of civil conflict or contexts with poor health care, legal, and social infrastructure, remains unknown. Devries et al. (1) synthesized population-based evidence in the most comprehensive study of IPV to date by using meta-regression methods to provide global and regional estimates of IPV. However, local evidence on GBV prevalence and trends, which informs programming, is often drawn from the subsample of individuals who disclose victimization (14–16). This is problematic because GBV is typically underreported, and individuals who report or disclose GBV may systematically differ from those who do not. The latter group may remain unreached by services and support if programs have been designed on the basis of characteristics of the former. Furthermore, such programs may not be properly resourced to meet demand. Understanding the proportion of individuals reporting has direct implications for funding, resource allocation, and policy, whereas understanding characteristics of those less likely to report has direct implications for program design and impact evaluation of prevention and treatment services.
Underreporting and failure to seek help occur worldwide (17–30). Barriers to reporting or seeking care from formal sources include shame and stigma (24, 27), financial barriers (31, 32), perceived impunity for perpetrators (26, 33), lack of awareness of available services (17, 23, 25) or access to such services (27, 32), cultural beliefs (32, 34), threat of losing children (24), fear of getting the offender in trouble (35, 36), fear of retaliation (24, 27, 37), discriminatory and stereotypical attitudes toward victims in courts and law enforcement settings (24, 38–40), and distrust of health care workers (37). In addition, many women simply do not report or seek care because they believe that the violence is normal or not serious enough to report (24, 36, 41).
Reporting behavior among GBV survivors in developing countries has received scant attention in the literature. Over the past decade, although international organizations have published technical reports describing prevalence of reporting in select developing countries (25, 28–30), including several cross-country comparisons (22, 24, 27), peer-reviewed literature provides few examples of quantitative estimates. Furthermore, estimates of reporting prevalence in developing countries are limited to single-country examples, namely from Pakistan, Democratic Republic of Congo, and East Timor (21, 23, 26). In peer-reviewed and gray literature (i.e., non–peer reviewed literature such as technical reports) published between 2002 and 2012 (20–30), among women experiencing GBV, the percentage disclosing violence to anyone ranged from 23% in Cambodia to 79% in urban Namibia (24, 27); however, only 0.2%–58.6% reported to formal sources (21, 24) (Web Table 1, available at http://aje.oxfordjournals.org/). A technical report from the World Health Organization's Multi-Country Study on Women's Health and Domestic Violence revealed that 34%–79% of women experiencing physical abuse by an intimate partner had ever disclosed to anyone, and reports to formal sources ranged from 0.3% to 9.8% to police, 0% to 1.2% to nongovernmental organizations, and 1.3% to 6% to medical services (24, 42). Across 8 countries, Kishor and Hindin (27) found that formal reporting ranged from 4.2% in Cambodia to 32.8% in Nicaragua. In a study of 8 countries in Latin America and the Caribbean (LAC), Bott et al. (22) found that formal reporting ranged from 8.2% in Ecuador to 30.7% in Guatemala.
Few peer-reviewed studies to date have focused specifically on reporting or care seeking among survivors of GBV using population-based data, and none has provided global or regional comparisons of formal reporting rates. To address this gap, we aimed to 1) quantify the bounds on underreporting of GBV experienced by women of reproductive age in 24 developing countries from 4 regions using standardized data, and 2) describe differences between survivors who report to formal sources and those who do not. We do not include men in this analysis because of data limitations. Results inform the magnitude and nature of underreporting and provide evidence to policy makers and program implementers toward understanding the hidden epidemic of GBV.
METHODS
Data
Data used in this study came from cross-sectional, nationally representative Demographic and Health Surveys in 24 countries. For further information on sampling and questionnaire design, see http://www.measuredhs.com. Measure DHS (Calverton, Maryland) routinely implements a standard GBV module with valid and reliable measurement of GBV with some variation across countries (43). We analyzed Demographic and Health Surveys conducted since 2000, which included GBV modules and questions on reporting or care seeking and were administered to women of reproductive age (15–49 years). We excluded from our analysis those aged 13 or 14 years sampled in Colombia for comparability across samples. The 24 countries analyzed are in the following 4 regions: Central Asia and Eastern Europe (3 countries), LAC (4 countries), India and East Asia (5 countries), and Africa (12 countries) (Table 1).
Table 1.
Reporting Descriptives Among Women Experiencing Any Violence (Physical or Sexual) by Country, 2004–2011
| Country by Region | Year | Sample Size | Any Report |
Formal Report |
Formal Report Subtype |
Informal Report |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Police |
Medical |
Social Services |
||||||||||||
| % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | |||
| Latin America and Caribbean | ||||||||||||||
| Bolivia | 2008 | 3,521 | 26.31 | 1.00 | 15.99 | 0.80 | 8.66 | 0.60 | 10.46 | 0.60 | 8.09 | 0.60 | 20.05 | 0.90 |
| Colombia | 2010 | 18,376 | 51.87 | 0.50 | 26.03 | 0.40 | 17.01 | 0.40 | 0.56 | 0.10 | 11.30 | 0.30 | 42.77 | 0.50 |
| Haiti | 2005–2006 | 1,318 | 35.91 | 2.30 | 1.98 | 0.60 | 1.79 | 0.60 | 0.00 | 0.00 | 0.19 | 0.10 | 34.76 | 2.20 |
| Honduras | 2005–2006 | 3,682 | 18.56 | 0.80 | 10.38 | 0.60 | 4.23 | 0.40 | 3.27 | 0.40 | 5.92 | 0.50 | 14.97 | 0.70 |
| Regional meansa | 26,897 | 33.16 | 0.42 | 13.60 | 0.24 | 7.92 | 0.18 | 3.57 | 0.15 | 6.38 | 0.16 | 28.14 | 0.41 | |
| India and East Asia | ||||||||||||||
| Cambodia | 2005 | 628 | 30.92 | 2.50 | 3.09 | 0.90 | 0.18 | 0.10 | 2.91 | 0.90 | 30.78 | 2.50 | ||
| India | 2005–2006 | 27,175 | 31.52 | 0.60 | 0.97 | 0.10 | 0.56 | 0.10 | 0.10 | 0.00 | 0.38 | 0.10 | 31.20 | 0.60 |
| Nepal | 2011 | 1,751 | 25.18 | 1.46 | 1.76 | 0.48 | 0.86 | 0.30 | 0.48 | 0.35 | 0.42 | 0.19 | 24.17 | 1.48 |
| Philippines | 2008 | 2,355 | 33.28 | 1.20 | 4.06 | 0.40 | 3.31 | 0.40 | 0.40 | 0.10 | 1.09 | 0.30 | 30.97 | 1.10 |
| Timor-Leste | 2009–2010 | 1,202 | 39.05 | 2.10 | 1.55 | 0.50 | 0.93 | 0.40 | 0.00 | 0.00 | 0.62 | 0.30 | 38.80 | 2.10 |
| Regional meansa | 33,111 | 31.99 | 0.55 | 2.29 | 0.19 | 1.17 | 0.11 | 0.78 | 0.14 | 0.63 | 0.09 | 31.18 | 0.54 | |
| Central Asia and Eastern Europe | ||||||||||||||
| Azerbaijan | 2006 | 951 | 29.40 | 2.20 | 2.56 | 0.60 | 2.08 | 0.60 | 0.48 | 0.30 | 0.33 | 0.20 | 28.35 | 2.30 |
| Moldova | 2005 | 1,514 | 48.47 | 1.60 | 13.83 | 1.00 | 12.03 | 1.00 | 2.38 | 0.40 | 0.69 | 0.30 | 40.90 | 1.60 |
| Ukraine | 2007 | 562 | 65.05 | 2.80 | 13.57 | 1.90 | 12.55 | 1.90 | 1.01 | 0.40 | 1.23 | 0.50 | 60.16 | 2.90 |
| Regional meansa | 3,027 | 47.64 | 0.94 | 9.99 | 0.59 | 8.89 | 0.56 | 1.29 | 0.21 | 0.75 | 0.18 | 43.14 | 0.94 | |
| Africa | ||||||||||||||
| Cameroon | 2004 | 1,759 | 37.21 | 1.40 | 7.76 | 0.80 | 1.68 | 0.40 | 6.06 | 0.70 | 0.53 | 0.20 | 36.04 | 1.40 |
| Ghana | 2008 | 1,075 | 42.66 | 1.90 | 4.54 | 0.80 | 2.15 | 0.60 | 0.25 | 0.20 | 2.43 | 0.60 | 39.82 | 1.80 |
| Kenya | 2008–2009 | 2,869 | 43.01 | 1.50 | 6.80 | 1.30 | 2.38 | 0.90 | 0.88 | 0.30 | 4.67 | 1.00 | 40.21 | 14.00 |
| Malawi | 2010 | 2,527 | 45.23 | 1.60 | 6.51 | 0.60 | 5.50 | 0.60 | 0.46 | 0.10 | 0.92 | 0.20 | 40.86 | 1.50 |
| Mali | 2006 | 2,699 | 40.40 | 1.80 | 3.14 | 0.50 | 0.10 | 0.10 | 2.87 | 0.50 | 0.28 | 0.10 | 38.69 | 2.00 |
| Nigeria | 2008 | 6,640 | 41.87 | 1.00 | 1.89 | 0.20 | 0.76 | 0.10 | 0.13 | 0.10 | 1.03 | 0.10 | 40.84 | 1.00 |
| Rwanda | 2010 | 2,361 | 42.91 | 1.15 | 2.76 | 0.46 | 2.76 | 0.46 | 42.91 | 1.15 | ||||
| Sao Tome and Principe | 2008–2009 | 765 | 44.35 | 3.20 | 5.53 | 1.10 | 4.35 | 1.00 | 0.00 | 0.00 | 1.75 | 0.80 | 40.94 | 2.80 |
| Tanzania | 2010 | 2,890 | 54.45 | 1.10 | 15.85 | 0.90 | 2.72 | 0.40 | 0.51 | 0.10 | 14.25 | 0.90 | 45.03 | 1.20 |
| Uganda | 2006 | 1,475 | 34.98 | 1.60 | 8.43 | 0.90 | 2.00 | 0.40 | 0.44 | 0.20 | 6.48 | 0.80 | 30.24 | 1.60 |
| Zambia | 2007 | 2,745 | 52.26 | 1.35 | 5.66 | 0.57 | 3.35 | 0.48 | 0.39 | 0.10 | 2.75 | 0.40 | 49.90 | 1.27 |
| Zimbabwe | 2010–2011 | 2,816 | 41.70 | 1.16 | 5.49 | 0.50 | 3.90 | 0.40 | 0.52 | 0.18 | 1.70 | 0.30 | 38.74 | 1.11 |
| Regional meansa | 30,621 | 43.42 | 0.32 | 6.20 | 0.16 | 2.64 | 0.11 | 1.14 | 0.07 | 3.34 | 0.12 | 40.35 | 0.32 | |
| Global meansa | 93,656 | 39.86 | 0.26 | 7.09 | 0.15 | 3.99 | 0.14 | 1.50 | 0.06 | 3.05 | 0.06 | 36.75 | 0.25 | |
Abbreviation: SE, standard error.
a Regional and global means are unweighted.
Measures
We defined sexual violence as violence of a sexual nature perpetrated by intimate partners or others, forced sexual debut, or other forced sexual acts. We defined physical violence as physical IPV; anyone other than a respondent's current/last partner having hit, slapped, kicked or physically hurt the respondent since age 15 years; or anyone other than her partner having hit, slapped, kicked, or physically hurt her during pregnancy. The physical violence questions were based on a modified version of the Conflict Tactics Scales (27), and wording varied slightly across countries. “Any GBV” was defined as having ever experienced physical or sexual violence as specified above.
Our outcome, reporting of GBV, was based on variations of the following question: “Thinking about what you yourself have experienced among the different things we have been talking about, have you ever tried to seek help to stop (the/these) person(s) from doing this to you again?” If the woman answered yes to this screening question, she was then asked, “From whom have you sought help?” Possible responses varied by country and included the woman's own family, her husband/partner's family, her current/late/last husband/partner, a male friend, a female friend, a neighbor, a religious leader, a doctor/medical personnel, police, a lawyer, a social service organization, a community leader, or other. A second health facility–specific reporting question was asked in 6 countries (Bolivia, Cambodia, Cameroon, Honduras, Mali, and Rwanda) and was generally phrased as follows: “Has the following ever happened because of something your (last) husband/partner did to you: You went to the doctor or health center?” Conditional on having experienced GBV, respondents were classified as having formally reported GBV if they disclosed to any of the following sources: doctor/medical personnel, police, lawyer, social service organization, community leader, or religious leader, or if they had visited a health clinic as a result of the violence. Additionally, we constructed a variable for informal reporting as disclosure to any of the following sources: own family, husband/partner's family, current/late/last husband/partner, male friend, female friend, or neighbor. There was an additional question asking whether the woman told “anyone else about this” in the following countries: Haiti, Nepal, the Philippines, Azerbaijan, Ukraine, Ghana, Kenya, Malawi, Nigeria, Sao Tome and Principe, Tanzania, Zambia, and Zimbabwe. Women who responded affirmatively to this question qualified as having informally reported. These formal and informal reporting categories are not mutually exclusive because women could select multiple sources of reporting. Because the reporting question was asked only once and referred to all types of physical and sexual violence addressed in the violence module, we were not able to distinguish differences in reporting behaviors by type of violence or by perpetrator.
Statistical analysis
For the women who had experienced GBV, we estimated weighted country-level and unweighted regional and global proportions of women who reported to any source and to formal and informal sources. Unweighted regional and global proportions were calculated as follows:
| (1) |
where  is the point estimate for an individual country. The variance for these regional/global estimates was calculated as follows:
is the point estimate for an individual country. The variance for these regional/global estimates was calculated as follows:
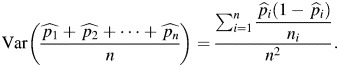 |
(2) |
Next, we conducted country-level multivariate logistic regression analysis to explore socioeconomic and demographic characteristics associated with reporting to formal sources, conditional on having experienced GBV. Independent variables included individual-level characteristics (age, educational level, and marital status), household-level characteristics (wealth and distance to a health facility), and community-level characteristics (urban/rural residence and region). Distance to a health facility was unavailable in 3 countries (Colombia, Ukraine, and Kenya). Independent variables differed slightly across countries on the basis of indicator availability. Because of low overall rates of formal reporting, we are not able to analyze sources of reporting separately (e.g., medical vs. police) in multivariate regressions. Similarly, because of low rates of reporting within categories of independent variables, we combined “no education” with “some or complete primary education” in Ukraine, Azerbaijan, and Philippines; we combined “some secondary or higher education” with “some or complete primary education” in Cambodia, Cameroon, and Sao Tome and Principe; and we combined “never married” with “currently married” in Cambodia, Nepal, Azerbaijan, Mali, and Sao Tome and Principe. Finally, to add context to our findings, we summarized reasons women chose not to report in countries with such information available (Bolivia, Cambodia, Cameroon, and Mali). All analyses accounted for complex survey design and sample weights with the exception of regional and global means, which were calculated as described above. This study was exempted from ethical review by Stony Brook University's institutional review board. The funding agency, the National Institutes of Health (Bethesda, Maryland), had no role in the design, implementation, or reporting of this study.
RESULTS
GBV subsample
Among a pooled total of 446,821 women globally, just over half (n = 284,281) were selected and interviewed for GBV modules (see Web Table 2 for sample sizes and selection criteria). The global prevalence of any physical or sexual GBV (unweighted) was 36.43% (95% confidence interval (CI): 36.21, 36.65), ranging from 14.98% (95% CI: 13.41, 16.55) in Azerbaijan to 70.36% (95% CI: 67.62, 73.10) in Uganda (Web Table 2).
Prevalence of reporting
Table 1 shows percentages of women who reported to formal and informal sources. Conditional on experience of GBV, the total pooled sample size for the reporting analysis was 93,656 women (Table 1). Globally, the rate of reporting to any source was 39.86% (95% CI: 39.35, 40.37) and ranged from 31.99% (95% CI: 30.91, 33.07) in India and East Asia to 47.64% (95% CI: 45.80, 49.48) in Central Asia and Eastern Europe. Globally, the majority of reporting was to informal sources (mean = 36.75%, 95% CI: 36.26, 37.24), with regional means of 28.14% (95% CI: 27.34, 28.94) in LAC, 31.18% (95% CI: 30.12, 32.24) in India and East Asia, 40.35% (95% CI: 39.72, 40.98) in Africa, and 43.14% (95% CI: 41.30, 44.98) in Central Asia and Eastern Europe (Table 1).
Global rates of reporting to formal sources were low (mean = 7.09%, 95% CI: 6.80, 7.38), with regional means of 2.29% (95% CI: 1.92, 2.66) in India and East Asia, 6.20% (95% CI: 5.89, 6.51) in Africa, 9.99% (95% CI: 8.83, 11.15) in Central Asia and Eastern Europe, and 13.6% (95% CI: 13.13, 14.07) in LAC (Table 1). Among reporting subtypes, rates of reporting police were highest in Central Asia and Eastern Europe (mean = 8.89%, 95% CI: 7.79, 9.99) and in LAC (mean = 7.92%, 95% CI: 7.63, 8.21). In other regions, 2.64% (95% CI: 2.42, 2.86) of women reported to police in Africa, and 1.17% (95% CI: 0.95, 1.39) reported to police in India and East Asia. Similarly, we found the following low rates of reporting to medical services: 3.57% (95% CI: 3.28, 3.86) in LAC, 0.78% (95% CI: 0.51, 1.05) in India and East Asia, 1.29% (95% CI: 0.88, 1.70) in Central Asia and Eastern Europe, and 1.14% (95% CI: 1.00, 1.28) in Africa. Finally, reporting to social services organizations across regions ranged from 6.38% in LAC (95% CI: 6.07, 6.69) and 3.34% (95% CI: 3.10, 3.57) in Africa to less than 1% in both India and East Asia (95% CI: 0.45, 0.81) and Central Asia and Eastern Europe (95% CI: 0.40, 1.10).
We replicated descriptive statistics for reporting by women experiencing any physical violence (Web Table 3) and any sexual violence (Web Table 4) separately; note that these categories are not mutually exclusive. Rates of formal reporting were higher among women experiencing any sexual violence than among those experiencing any physical violence, with 6 exceptions (Haiti, Nepal, Ghana, Malawi, Tanzania, and Zimbabwe).
Characteristics associated with formal reporting
Tables 2–5 show results of logistic regressions examining characteristics associated with women's formal reporting by region, conditional on having experienced GBV (see Web Tables 5 and 6 for sample characteristics). Globally, in 15 of the 24 countries studied, formerly married women (including widows and separated and divorced women) were significantly more likely than currently married women to report to formal sources (odds ratios (ORs) ranging from 1.5 (95% CI: 1.36, 1.66) in Colombia to 17.26 (95% CI: 5.29, 56.36) in Azerbaijan). Additionally, in 7 countries (Bolivia, Cameroon, Colombia, Honduras, Timor Leste, Uganda, and Zambia), never married women were less likely than currently married women to report to formal sources (ORs ranging from 0.05 (95% CI: 0.01, 0.41) in Uganda to 0.75 (95% CI: 0.64, 0.89) in Colombia). Increasing age was positively associated with formal reporting in half of the countries included in the analysis (ORs ranging from 1.02 (95% CI: 1.0, 1.05) in India to 1.06 (95% CI: 1.01, 1.11) in Sao Tome and Principe). Educational attainment was positively associated with formal reporting in 4 of 24 countries (Cameroon, Haiti, India, and Nigeria). Women with some secondary or higher education were more likely to report than were those with some/complete primary education in 2 countries (in Nigeria, OR = 1.74 (95% CI: 1.07, 2.84); in Haiti, OR = 16.85 (95% CI: 2.94, 96.74)), and women with no education were less likely to report than were those with some/complete primary education in 2 countries (in Cameroon, OR = 0.28 (95% CI: 0.09, 0.85); in India, OR = 0.60 (95% CI: 0.42, 0.88)). Conversely, women with secondary/higher education were less likely than those with some/complete primary education to have reported to formal sources in 3 countries (Moldova, Tanzania, and Philippines) with odds ratios ranging from 0.11 (95% CI: 0.01, 0.92) in Tanzania to 0.70 (95% CI: 0.51, 0.98) in Moldova. Wealth was significantly associated with formal reporting only in Africa, where the poorest 40% of women were more likely to report in 2 countries (in Tanzania, OR = 1.47 (95% CI: 1.07, 2.0); in Sao Tome and Principe, OR = 3.41 (95% CI: 1.10, 10.57)) and less likely to report in Mali (OR = 0.49 (95% CI: 0.24, 1.0)). Women living in urban areas were more likely to formally report in more than 20% of the countries studied (ORs ranging from 1.43 (95% CI: 1.24, 1.65) in Colombia to 4.55 (95% CI: 1.44, 14.35) in Azerbaijan). Distance to a health facility was not consistently associated with formal reporting.
Table 2.
Logistic Regression Odds Ratiosa of Formal Reporting for Women Experiencing Any Violence (Physical or Sexual) by Country, Latin America and the Caribbean and Central Asia and Eastern Europe, 2005–2008
| Covariate | Latin America and the Caribbean |
Central Asia and Eastern Europe |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bolivia (in 2008) |
Colombia (in 2010)b |
Haiti (in 2005–2006) |
Honduras (in 2005–2006) |
Azerbaijan (in 2006) |
Moldova (in 2005) |
Ukraine (in 2007)b |
||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | CI | OR | 95% CI | |
| Marital status | ||||||||||||||
| Never married | 0.38c | 0.25, 0.58 | 0.75c | 0.64, 0.89 | 1.18 | 0.22, 6.36 | 0.16c | 0.07, 0.35 | 0.84 | 0.38, 1.89 | 1.19 | 0.31, 4.55 | ||
| Formerly married | 1.12 | 0.76, 1.65 | 1.50c | 1.36, 1.66 | 1.08 | 0.21, 5.58 | 0.77 | 0.53, 1.10 | 17.26c,d | 5.29, 56.36 | 1.94e | 1.30, 2.91 | 2.51e | 1.25, 5.04 |
| Age, years | 1.01 | 0.99, 1.02 | 1.02c | 1.01, 1.02 | 1.03 | 0.96, 1.11 | 1.01 | 0.99, 1.02 | 0.98 | 0.92, 1.04 | 1.04c | 1.02, 1.06 | 1.01 | 0.97, 1.06 |
| Education | ||||||||||||||
| No education | 1.19 | 0.74, 1.91 | 0.77 | 0.57, 1.03 | 1.28 | 0.26, 6.32 | 0.78 | 0.48, 1.29 | 1.28 | 0.10, 17.14 | ||||
| Some secondary or higher education | 0.89 | 0.69, 1.14 | 0.97 | 0.88, 1.06 | 16.85e | 2.94, 96.74 | 0.79 | 0.51, 1.22 | 1.75f | 0.79, 3.87 | 0.70g | 0.51, 0.98 | 0.69f | 0.35, 1.39 |
| Bottom 40% of wealth | 0.83 | 0.60, 1.14 | 1.03 | 0.92, 1.16 | 0.44 | 0.16, 1.20 | 0.95 | 0.67, 1.35 | 2.52 | 0.84, 7.55 | 0.80 | 0.52, 1.24 | 1.37 | 0.67, 2.81 |
| Urban | 1.17 | 0.86, 1.59 | 1.43c | 1.24, 1.65 | 0.37 | 0.09, 1.46 | 1.12 | 0.80, 1.55 | 4.55e | 1.44, 14.35 | 1.03 | 0.50, 2.12 | 1.47 | 0.74, 2.95 |
| Distance to health facilities a big problem | 1.09 | 0.85, 1.39 | 0.27g | 0.09, 0.80 | 0.82 | 0.63, 1.08 | 1.59 | 0.55, 4.61 | 1.11 | 0.74, 1.67 | ||||
| F-statistic, district/regional indicators | 2.71 | 8.84 | 1.80 | 1.77 | 1.00 | 1.05 | 0.73 | |||||||
| No. of observations | 3,521 | 18,376 | 1,318 | 3,682 | 951 | 1,514 | 562 | |||||||
Abbreviations: CI, confidence interval; OR, odds ratio.
a Reference categories are as follows: for marital status, currently married; for education, some or complete primary; for wealth, top 60%; and for distance to health facility, not a problem. All models control for district or regional indicators.
b Distance to health care facility excluded from questionnaire.
c P < 0.001.
d Because of low rates of reporting, never married women were combined with currently married women as the reference category.
e P < 0.01.
f Because of low rates of reporting, no education was combined with some or complete primary education as the reference category.
g P < 0.05.
Table 3.
Logistic Regression Odds Ratiosa of Formal Reporting for Women Experiencing Any Violence (Physical or Sexual) by Country, India and East Asia, 2005–2011
| Covariate | Cambodia (in 2005) |
India (in 2005) |
Nepal (in 2011) |
Philippines (in 2008) |
Timor Leste (in 2009–2010) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Marital status | ||||||||||
| Never married | 0.79 | 0.30, 2.09 | 0.82 | 0.30, 2.26 | 0.06b | 0.01, 0.61 | ||||
| Formerly married | 1.71c | 0.54, 5.41 | 4.47d | 3.06, 6.54 | 4.15b,c | 1.10, 15.70 | 1.78 | 0.95, 3.32 | 9.70d | 2.80, 33.59 |
| Age, years | 1.08b | 1.00, 1.17 | 1.02b | 1.00, 1.05 | 1.00 | 0.96, 1.04 | 1.03b | 1.00, 1.07 | 0.96 | 0.90, 1.03 |
| Education | ||||||||||
| No education | 0.78e | 0.13, 4.72 | 0.60f | 0.42, 0.88 | 0.37 | 0.14, 1.00 | 0.48 | 0.11, 2.05 | ||
| Some secondary or higher education | 0.68 | 0.34, 1.34 | 0.22 | 0.04, 1.27 | 0.57b,g | 0.35, 0.95 | 0.94 | 0.15, 6.01 | ||
| Bottom 40% of wealth | 2.10 | 0.64, 6.90 | 1.00 | 0.66, 1.52 | 0.68 | 0.24, 1.94 | 1.14 | 0.67, 1.95 | 2.89 | 0.78, 10.67 |
| Urban | 2.41 | 0.70, 8.30 | 1.44 | 0.98, 2.10 | 0.98 | 0.28, 3.48 | 2.22f | 1.38, 3.58 | 0.61 | 0.08, 4.38 |
| Distance to health facilities a big problem | 3.06 | 0.81, 11.52 | 1.47b | 1.02, 2.14 | 0.90 | 0.28, 2.95 | 0.75 | 0.46, 1.21 | 0.49 | 0.09, 2.76 |
| F-statistic, district/regional indicators | 0.82 | 3.88 | 1.03 | 1.08 | 3.12 | |||||
| No. of observations | 628 | 27,175 | 1,751 | 2,355 | 1,202 | |||||
Abbreviations: CI, confidence interval; OR, odds ratio.
a Reference categories are as follows: for marital status, currently married; for education, some or complete primary; for wealth, top 60%; and for distance to health facility, not a problem. All models control for district or regional indicators.
b P < 0.05.
c Because of low rates of reporting, never married women were combined with currently married women as the reference category.
d P < 0.001.
e Because of low rates of reporting, some secondary or higher education was combined with some or complete primary education as the reference category.
f P < 0.01.
g Because of low rates of reporting, no education was combined with some or complete primary education as the reference category.
Table 4.
Logistic Regression Odds Ratiosa of Formal Reporting for Women Experiencing Any Violence (Physical or Sexual) by Country, Eastern and Southern Africa, 2006–2011
| Covariate | Kenya (in 2008–2009)b |
Malawi (in 2010) |
Rwanda (in 2010) |
Tanzania (in 2010) |
Uganda (in 2006) |
Zambia (in 2007) |
Zimbabwe (in 2010–2011) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Marital status | ||||||||||||||
| Never married | 0.80 | 0.31, 2.11 | 0.49 | 0.11, 2.06 | 1.35 | 0.50, 3.66 | 0.63 | 0.33, 1.20 | 0.05c | 0.01, 0.41 | 0.27c | 0.12, 0.63 | 1.17 | 0.55, 2.50 |
| Formerly married | 3.54c | 1.36, 9.21 | 2.13d | 1.41, 3.20 | 2.59c | 1.34, 5.01 | 1.98d | 1.42, 2.76 | 2.06e | 1.19, 3.58 | 1.93e | 1.05, 3.55 | 1.99c | 1.25, 3.18 |
| Age, years | 1.05d | 1.03, 1.08 | 1.02 | 1.00, 1.05 | 1.01 | 0.97, 1.06 | 1.04d | 1.02, 1.05 | 1.01 | 0.98, 1.04 | 1.01 | 0.99, 1.04 | 1.03e | 1.01, 1.06 |
| Education | ||||||||||||||
| No education | 0.62 | 0.30, 1.30 | 0.95 | 0.54, 1.68 | 0.86 | 0.40, 1.85 | 0.98 | 0.72, 1.34 | 0.55 | 0.29, 1.04 | 1.00 | 0.51, 1.94 | 0.51 | 0.19, 1.34 |
| Some secondary or higher education | 0.89 | 0.54, 1.44 | 0.74 | 0.31, 1.77 | 1.03 | 0.11, 9.73 | 0.11e | 0.01, 0.92 | 0.36 | 0.08, 1.71 | 0.90 | 0.44, 1.84 | 1.62 | 0.61, 4.33 |
| Bottom 40% of wealth | 0.79 | 0.35, 1.76 | 0.90 | 0.61, 1.34 | 0.77 | 0.39, 1.54 | 1.47e | 1.07, 2.00 | 0.99 | 0.55, 1.76 | 0.61 | 0.33, 1.11 | 1.84 | 1.00, 3.39 |
| Urban | 2.25 | 0.97, 5.22 | 1.52 | 0.86, 2.70 | 1.83 | 0.70, 4.78 | 0.87 | 0.59, 1.29 | 1.50 | 0.62, 3.63 | 1.59 | 0.86, 2.95 | 2.71e | 1.24, 5.93 |
| Distance to health facilities a big problem | 0.98 | 0.64, 1.52 | 0.85 | 0.44, 1.65 | 0.90 | 0.64, 1.25 | 0.95 | 0.60, 1.50 | 0.89 | 0.53, 1.48 | 1.54e | 1.04, 2.27 | ||
| F-statistic, district/regional indicators | 1.84 | 0.67 | 2.85 | 3.55 | 1.28 | 5.76 | 2.42 | |||||||
| No. of observations | 2,869 | 2,527 | 2,361 | 2,890 | 1,475 | 2,745 | 2,816 | |||||||
Abbreviations: CI, confidence interval; OR, odds ratio.
a Reference categories are as follows: for marital status, currently married; for education, some or complete primary; for wealth, top 60%; and for distance to health facility, not a problem. All models control for district or regional indicators.
b Distance to health care facility was excluded from questionnaire.
c P < 0.01.
d P < 0.001.
e P < 0.05.
Table 5.
Logistic Regression Odds Ratiosa of Formal Reporting for Women Experiencing Any Violence (Physical or Sexual) by Country, West and Central Africa, 2004–2009
| Covariate | Cameroon (in 2004) |
Ghana (in 2008) |
Mali (in 2006) |
Nigeria (in 2008) |
Sao Tome and Principe (in 2008–2009) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Marital status | ||||||||||
| Never married | 0.40b | 0.17, 0.97 | 1.63 | 0.55, 4.80 | 1.43 | 0.74, 2.76 | ||||
| Formerly married | 1.13 | 0.63, 2.02 | 1.80 | 0.65, 4.97 | 3.57c | 0.48, 26.44 | 2.19b | 1.10, 4.37 | 0.71a | 0.25, 1.97 |
| Age, years | 1.04d | 1.02, 1.07 | 1.02 | 0.97, 1.08 | 1.04b | 1.01, 1.07 | 1.04e | 1.01, 1.07 | 1.06b | 1.01, 1.11 |
| Education | ||||||||||
| No education | 0.28b,f | 0.09, 0.85 | 0.33 | 0.08, 1.32 | 1.35 | 0.69, 2.64 | 0.67 | 0.35, 1.28 | 0.36c | 0.07, 1.75 |
| Some secondary or higher education | 1.10 | 0.39, 3.15 | 3.14 | 0.53, 18.78 | 1.74b | 1.07, 2.84 | ||||
| Bottom 40% of wealth | 1.43 | 0.79, 2.59 | 0.92 | 0.33, 2.55 | 0.49b | 0.24, 1.00 | 0.90 | 0.45, 1.82 | 3.41b | 1.10, 10.57 |
| Urban | 0.87 | 0.45, 1.69 | 0.99 | 0.42, 2.31 | 0.96 | 0.51, 1.80 | 0.93 | 0.56, 1.55 | 3.27e | 1.42, 7.53 |
| Distance to health facilities a big problem | 1.06 | 0.68, 1.67 | 1.08 | 0.47, 2.45 | 0.67 | 0.34, 1.30 | 1.44 | 0.89, 2.32 | 0.55 | 0.15, 2.01 |
| F-statistic, district/regional indicators | 4.09 | 1.24 | 4.17 | 0.96 | 1.77 | |||||
| No. of observations | 1,759 | 1,075 | 2,699 | 6,640 | 765 | |||||
Abbreviations: CI, confidence interval; OR, odds ratio.
a Reference categories are as follows: for marital status, currently married; for education, some or complete primary; for wealth, top 60%; and for distance to health facility, not a problem. All models control for district or regional indicators.
b P < 0.05.
c Because of low rates of reporting, never married women were combined with currently married women as the reference category.
d P < 0.001.
e P < 0.01.
f Because of low rates of reporting, some secondary or higher education was combined with some or complete primary education as the reference category.
Reasons for not reporting
Reasons for not reporting GBV are presented in Web Table 7. The most common reasons were embarrassment (25% in Bolivia and 41% in Cambodia) and a belief that there was no use in reporting (47% in Cameroon and 30% in Mali). Other reasons included a belief that violence was a normal part of life that women must bear and various concerns for the well-being of others.
DISCUSSION
The global rate of formal reporting among women in our sample was 7%, and regional rates of formal reporting ranged from 2% to 14%. This implies that levels of physical and sexual GBV among women of reproductive ages within our sample countries would be 14 (1 / 0.07 = 14.3) times higher than the number of incidents estimated from combined formal sources, 25 times higher than estimates from police reports, 67 times higher than estimates from medical facilities, and 33 times higher than estimates from social services sources. Regionally, these combined multipliers (to any formal source) are 7 in LAC, 44 in India and East Asia, 10 in Central Asia and Eastern Europe, and 16 in Africa. These multipliers are even larger when restricting to reporting subtype within each region.
Our study is the largest multicountry comparison to date, and our results are generally consistent with previous studies originating mainly from the gray literature, which show that informal reporting is vastly more common than formal reporting (24–27, 43). In both our study and the World Health Organization's Multi-Country Study on Women's Health and Domestic Violence, the highest rates of formal reporting came from LAC, and the lowest rates of formal reporting came from Asia. Differences between our estimates and those reviewed in Web Table 1 may be partially attributed to differences in sampling. For example, Casey et al. (23) found a higher rate of reporting to medical services (59%), but they examined only women experiencing sexual assault perpetrated by strangers, and women may be more likely to report sexual assault perpetrated by strangers in scenarios that fit the so-called “classic rape” (44–47).
The robust positive correlation between being formerly married and reporting may be because women experiencing more severe cases of IPV are more likely to seek help and leave the abusive relationship, or because those able to seek help (regardless of severity of abuse) are more likely to leave relationships. Alternatively, men may reject their partners who have been raped (48). We were unable to test these hypotheses because of lack of information on timing of abuse and reporting in our data. The positive correlation between increasing age and formal reporting may reflect increased autonomy and less dependence on cohabiting partners over time. Finally, women in urban centers may have better access to social, legal, and health services.
Results regarding wealth and education were not straightforward. Economic considerations are important factors in deciding whether to leave an abusive relationship. Women at the higher end of the range of income distribution may be more dependent on partners to maintain current standards of living, whereas for the poorest women, the marginal cost of leaving may be small in comparison to expected benefits. We were unable to disentangle causal effects of education and timing of GBV because of the cross-sectional nature of the data.
Regional differences in reporting likely reflect important cultural, political, or religious differences in the regions studied. A strength of our modeling is that we included subnational “fixed effects,” which may in part control for unobserved confounders such as religion and cultural differences within each country. Some of these cultural norms may also be important sources of variation at the regional level. For example, the comparatively high rates of formal reporting in LAC may reflect stronger, homegrown women's rights movements in the region, as well as a history of political movements advocating for human rights, often in response to abusive governments. In addition, more developed countries tend to have stronger institutions, and the strength of institutions such as police and judicial systems is important for reporting. Indeed, the 2 regions in our analysis (Central Asia/Eastern Europe and LAC) with the highest levels of development as measured by the Human Development Index (http://hdr.undp.org/en/statistics/hdi/), which considers life expectancy, educational attainment, and income, had the highest regional rates of reporting. It is important to note, however, that average regional development masks wide variation within regions, particularly in LAC and India and East Asia. Furthermore, cultural norms surrounding family, divorce, and women's autonomy may also influence individual women's reporting behaviors. Although we are not able to directly model these relationships, we acknowledge their role, particularly in the design and development of programs to increase safe and effective reporting and care seeking.
There are several limitations to our study. First, the low rates of reporting found in our analysis may be an artifact of questionnaire wording. Women were asked if they ever reported the violence to anyone or sought help to stop the violence from occurring. If a woman had reported or told someone about the abuse with different intentions, she may not have answered affirmatively to the question. It is also possible that women who have formally reported are more likely to disclose GBV when asked in surveys. In this case, our point estimates would be a lower bound, because our sample would fail to capture the reporting behaviors of women who are comparatively less likely to report both formally and in surveys. Another limitation was our inability to distinguish between intimate partners and other perpetrators in relation to reporting. Finally, we are limited by the cross-sectional nature of the data and the age range and sex of respondents.
Results from this study help fill important gaps in the literature on underreporting of GBV in several ways. First, we have shown that conservative estimates indicate that rates of physical or sexual GBV in the population may be 7–44 times the number of incidents reported to formal sources combined. Second, we found that the average woman left uncounted was younger, never or currently married, and living in a rural community. Third, reasons described for not reporting suggest that policy initiatives should address impunity of perpetrators; ensure that GBV, particularly within marriage, is a prosecutable crime; and provide subsidies for GBV-related health costs. Additionally, programmatic activities should emphasize the following: dissemination of information on services, assistance in navigating the legal framework, establishment of “1-stop” centers for survivors, and efforts to reduce stigma. Over the past 15 years, GBV has been increasingly featured on the agenda of high-level international organizations, and many countries have implemented policies regarding violence against women (49). However, implementation and enforcement continue to be informed by studies using small samples of data collected at reporting points without clear understanding of how these women represent the larger affected population. Further studies advancing knowledge on underreporting in different contexts are warranted.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Preventive Medicine/Program in Public Health, Stony Brook University, Stony Brook, New York (Tia Palermo); Department of Community and Family Health, University of South Florida, Tampa, Florida (Jennifer Bleck); and Department of Public Policy, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina (Amber Peterman).
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (award R03HD073461).
We thank Caryn Bredenkamp for helpful comments.
Preliminary results from this study were presented orally at the American Public Health Association's 140th Annual Meeting in San Francisco, California, on October 30, 2012, and in poster format at the Missing Peace: Sexual Violence in Conflict and Post-Conflict Settings Conference at the US Institute of Peace in Washington, DC, on February 14–16, 2013.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest: none declared.
REFERENCES
- 1.Devries KM, Mak JYT, Garcia-Moreno C, et al. The global prevalence of intimate partner violence against women. Science. 2013;340(6140):1527–1528. doi: 10.1126/science.1240937. [DOI] [PubMed] [Google Scholar]
- 2.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 3.Campbell JC, Soeken KL. Forced sex and intimate partner violence effects on women's risk and women's health. Violence Against Women. 1999;5(9):1017–1035. [Google Scholar]
- 4.Ellsberg M, Jansen HAFM, Heise L, et al. Intimate partner violence and women's physical and mental health in the WHO Multi-Country Study on Women's Health and Domestic Violence: an observational study. Lancet. 2008;371(9619):1165–1172. doi: 10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- 5.Heise L, Ellsberg M, Gottmoeller M. A global overview of gender-based violence. Int J Gynecol Obstet. 2002;78(suppl 1):S5–S14. doi: 10.1016/S0020-7292(02)00038-3. [DOI] [PubMed] [Google Scholar]
- 6.Peterman A, Johnson K. Incontinence and trauma: sexual violence, female genital cutting and proxy measures of gynecological fistula. Soc Sci Med. 2009;68(5):971–979. doi: 10.1016/j.socscimed.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Rees S, Silove D, Chey T, et al. Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. JAMA. 2011;306(4):513–521. doi: 10.1001/jama.2011.1098. [DOI] [PubMed] [Google Scholar]
- 8.Thompson MP, Kaslow NJ, Kingree JB, et al. Partner abuse and posttraumatic stress disorder as risk factors for suicide attempts in a sample of low-income, inner city women. J Trauma Stress. 1999;12(1):59–72. doi: 10.1023/A:1024742215337. [DOI] [PubMed] [Google Scholar]
- 9.Kelly J, VanRooyen M, Kabanga J, et al. Hope for the Future Again: Tracing the Effects of Sexual Violence and Conflict on Families and Communities in Eastern Democratic Republic of the Congo. Cambridge, MA: Harvard Humanitarian Initiative; 2011. [Google Scholar]
- 10.Swiss S, Jennings P. Documenting the Impact of Conflict on Women Living in Internally Displaced Persons Camps in Sri Lanka: Some Ethical Considerations. Albuquerque, NM: Women's Rights International; 2006. [PMC free article] [PubMed] [Google Scholar]
- 11.Morrison AR, Orlando MB. Social and economic costs of domestic violence: Chile and Nicaragua. In: Morrison AR, Orlando MB, editors. Too Close to Home: Domestic Violence in the Americas. Washington, DC: Inter-American Development Bank; 1999. pp. 51–80. [Google Scholar]
- 12.Graves L, Hankivsky O, Kingston-Riechers J. Selected Estimates of the Costs of Violence Against Women. London, United Kingdom: Centre for Research on Violence Against Women and Children; 1995. [Google Scholar]
- 13.United Nations Security Council. Resolution 1960 (2010) http://www.securitycouncilreport.org/atf/cf/%7B65BFCF9B-6D27-4E9C-8CD3-CF6E4FF96FF9%7D/WPS%20SRES%201960.pdf . Published December 16, 2010. Accessed January 15, 2013.
- 14.Bartels SA, Scott JA, Leaning J, et al. Sexual violence trends between 2004 and 2008 in South Kivu, Democratic Republic of Congo. Prehosp Disaster Med. 2011;1(1):1–6. doi: 10.1017/S1049023X12000179. [DOI] [PubMed] [Google Scholar]
- 15.Human Righ ts Watch. Shattered Lives: Sexual Violence During the Rwandan Genocide and its Aftermath. New York, NY: Human Rights Watch; 1996. [Google Scholar]
- 16.Cohen DK, Green AH. Dueling incentives: sexual violence in Liberia and the politics of human rights advocacy. J Peace Res. 2012;49(3):445–458. [Google Scholar]
- 17.Du Mont J, Forte T, Cohen MM, et al. Changing help-seeking rates for intimate partner violence in Canada. Women Health. 2005;41(1):1–19. doi: 10.1300/J013v41n01_01. [DOI] [PubMed] [Google Scholar]
- 18.Hyman I, Forte T, Du Mont J, et al. Help-seeking rates for intimate partner violence (IPV) among Canadian immigrant women. Health Care Women Int. 2006;27(8):682–694. doi: 10.1080/07399330600817618. [DOI] [PubMed] [Google Scholar]
- 19.Langton L, Berzofsky M, Krebs C, et al. Victimizations Not Reported to the Police, 2006–2010. Washington, DC: US Department of Justice; 2012. [Google Scholar]
- 20.Statistics Canada. Violence Against Women Survey (VAWS) http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3896&Item_Id=1712 . Accessed June 15, 2013. [PubMed]
- 21.Andersson N, Cockcroft A, Ansari N, et al. Collecting reliable information about violence against women safely in household interviews: experience from a large-scale national survey in South Asia. Violence Against Women. 2009;15(4):482–496. doi: 10.1177/1077801208331063. [DOI] [PubMed] [Google Scholar]
- 22.Bott S, Guedes A, Goodwin M, et al. Violence Against Women in Latin America and the Caribbean: A Comparative Analysis of Population-Based Data From 12 Countries. Washington, DC: PanAmerican Health Organization; Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 23.Casey SE, Gallagher MC, Rukengeza Makanda B, et al. Care-seeking behavior by survivors of sexual assault in the Democratic Republic of the Congo. Am J Public Health. 2011;101(6):1054–1055. doi: 10.2105/AJPH.2010.300045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia-Moreno C, Jansen HAFM, Ellsberg M, et al. WHO Multi-Country Study on Women's Health and Domestic Violence Against Women: Initial Results on Prevalence, Health Outcomes and Women's Responses. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]
- 25.Hossain M, Zimmerman C, Kiss L, et al. Violence Against Women and Men in Cote d'Ivoire: A Cluster Randomized Controlled Trial to Assess Impact of the ‘Men & Women in Partnership’ Intervention on the Reduction of Violence Against Women and Girls in Rural Cote d'Ivoire—Results From a Community Survey. London, United Kingdom: London School of Hygiene and Tropical Medicine; 2010. [Google Scholar]
- 26.Hynes M, Ward J, Robertson C, et al. A determination of the prevalence of gender-based violence among conflict-affected populations in East Timor. Disasters. 2004;28(3):294–321. doi: 10.1111/j.0361-3666.2004.00260.x. [DOI] [PubMed] [Google Scholar]
- 27.Kishor S, Hindin MJ. Profiling Domestic Violence: A Multi-Country Study. Calverton, MD: Measure DHS and ORC Macro; 2004. [Google Scholar]
- 28.Reza A, Breiding M, Blanton C, et al. Violence Against Children in Swaziland: Findings From a National Survey on Violence Against Children in Swaziland May 15–June 16, 2007. Mbabane, Swaziland: Centers for Disease Control and Prevention and Swaziland United Nations Children's Fund; 2007. [Google Scholar]
- 29.United National's Children's Fund Kenya Country Office, United States Centers for Disease Control and Prevention, Kenya Bureau of Statistics. Violence Against Children in Kenya: Findings From a National Survey, 2010. Nairobi, Kenya. Nairobi, Kenya: United Nations Children's Fund Kenya Country Office; 2012. [Google Scholar]
- 30.United Nations Children's Fund Tanzania Country Office, United States Centers for Disease Control and Prevention, Muhimbili University of Health and Allied Sciences. Violence Against Children in Tanzania: Findings From a National Survey, 2009. Summary Report on the Prevalence of Sexual, Physical and Emotional Violence, Context of Sexual Violence, and Health and Behavioural Consequences of Violence Experienced in Childhood. Dar es Salaam, Tanzania: United Nations Children's Fund Tanzania; 2011. [Google Scholar]
- 31.International Center for Research on Women, GBV Prevention Network, MRC South Africa. Strengthening Research and Action on Gender-Based Violence in Africa. Washington, DC: International Center for Research on Women; 2012. [Google Scholar]
- 32.Wolf ME, Ly U, Hobart MA, et al. Barriers to seeking police help for intimate partner violence. J Fam Violence. 2003;18(2):121–129. [Google Scholar]
- 33.Ohambe MCO, Muhigwa JBB, Wa Mamba BM. Women's Bodies as a Battleground: Sexual Violence Against Women and Girls During the War in the Democratic Republic of Congo. South Kivu (1996–2003) Uvira and Bukavu, Democratic Republic of Congo: Réseau des Femmes pour un Développement Associatif, Réseau des Femmes pour la Défense des Droits et la Paix, International Alert; 2005. [Google Scholar]
- 34.Njuki R, Okal J, Warren CE, et al. Exploring the effectiveness of the output-based aid voucher program to increase uptake of gender-based violence recovery services in Kenya: a qualitative evaluation. BMC Public Health. 2012;12(1):426. doi: 10.1186/1471-2458-12-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dutton MA, Green BL, Kaltman SI, et al. Intimate partner violence, PTSD, and adverse health outcomes. J Interpers Violence. 2006;21(7):955–968. doi: 10.1177/0886260506289178. [DOI] [PubMed] [Google Scholar]
- 36.Lundgren E, Heimer G, Westerstrand J, et al. Captured Queen: Men's Violence Against Women in ‘Equal’ Sweden—a Prevalence Study. Stockholm, Sweden: Fritzes Offentiliga Publikationer; 2001. [Google Scholar]
- 37.Rodriguez MA, Quiroga SS, Bauer HM. Breaking the silence: battered women's perspectives on medical care. Arch Fam Med. 1996;5(3):153–158. doi: 10.1001/archfami.5.3.153. [DOI] [PubMed] [Google Scholar]
- 38.Amnesty International. I Can't Afford Justice: Violence Against Women in Uganda. London, United Kingdom: Amnesty International; 2010. [Google Scholar]
- 39.Amnesty International. Colombia: Hidden From Justice, Impunity for Conflict-Related Sexual Violence, a Follow-up Report. London, United Kingdom: Amnesty International; 2012. [Google Scholar]
- 40.Belknap J. Rape: too hard to report and too easy to discredit victims. Violence Against Women. 2010;16(12):1335–1344. doi: 10.1177/1077801210387749. [DOI] [PubMed] [Google Scholar]
- 41.Fugate M, Landis L, Riordan K, et al. Barriers to domestic violence help seeking: implications for intervention. Violence Against Women. 2005;11(3):290–310. doi: 10.1177/1077801204271959. [DOI] [PubMed] [Google Scholar]
- 42.Garcia-Moreno C, Jansen HAFM, Ellsberg M, et al. Prevalence of intimate partner violence: findings from the WHO Multi-Country Study on Women's Health and Domestic Violence. Lancet. 2006;368(9543):1260. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- 43.Hindin MJ, Kishor S, Ansara DL. Intimate Partner Violence Among Couples in 10 DHS Countries: Predictors and Health Outcomes. Calverton, MD: Macro International Inc; 2008. [Google Scholar]
- 44.McGregor MJ, Wiebe E, Marion SA, et al. Why don't more women report sexual assault to the police? Can Med Assoc J. 2000;162(5):659–660. [PMC free article] [PubMed] [Google Scholar]
- 45.Johnson BE, Kuck DL, Schander PR. Rape myth acceptance and sociodemographic characteristics: a multidimensional analysis. Sex Roles. 1997;36(11):693–707. [Google Scholar]
- 46.Du Mont J, Miller KL, Myhr TL. The role of “real rape” and “real victim” stereotypes in the police reporting practices of sexually assaulted women. Violence Against Women. 2003;9(4):466–486. [Google Scholar]
- 47.Felson RB, Paré PP. The reporting of domestic violence and sexual assault by nonstrangers to the police. J Marriage Fam. 2005;67(3):597–610. [Google Scholar]
- 48.Kelly J, Kabanga J, Cragin W, et al. ‘If your husband doesn't humiliate you, other people won't’: gendered attitudes towards sexual violence in eastern Democratic Republic of Congo. Glob Public Health. 2011;7(3):285–298. doi: 10.1080/17441692.2011.585344. [DOI] [PubMed] [Google Scholar]
- 49.Ellsberg M. Panel discussion. Presented at: From Evidence to Action: Unleasing the Power of Research to Combat Gender-Based Violence; December 5, 2012; Washington, DC: George Washington University; [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


