Abstract
Background and Purpose
The natural history of WMH progression due to normal aging versus comorbid vascular insults remains unclear. We therefore investigated age related differences in WMH volumes among a group with comorbid hypertension, abnormal BMI and/or diabetes to a normal aging group drawn from the same population lacking any of these comorbidities.
Methods
WMH volumes were acquired using 3T MRI for 2011 Dallas Heart Study participants. The slope of the WMH vs. age regression was compared between normal and comorbidities groups before and after age 50 where a change in slope was demonstrated.
Results
Aging was linearly associated with greater log WMH volume for both normal (p=0.02) and comorbidity (p < 0.0001) groups. Above 50 years more rapid increases in WMH volumes for age were seen in the group with comorbidities (p <.0001) but not the normal group (p-value=0.173). The between-group difference in slope of expected WMH for age was significantly greater in the comorbidities group beyond age 50 (p=0.0008) but not before (p=0.752).
Conclusions
After age 50, but not before, comorbid hypertension, obesity and diabetes was associated with significantly larger WMH volumes for age compared to a normal aging group lacking these conditions. These results support the assertion that age related differences in WMH volumes are significantly increased in the presence of comorbidities, but the effect is only detectable after age 50.
Keywords: White Matter Hyperintensity, Aging
Introduction
White matter hyperintensity (WMH) seen on MRI is a marker of cerebral microvascular disease and confers risk for developing cognitive impairment1 and Alzheimer's disease 2. The natural history of WMH progression due to normal aging3 itself versus the cumulative consequence of vascular insults4 linked to comorbidities such as hypertension, obesity and diabetes remains unclear. We therefore investigated age-related differences in WMH volumes on 3T MRI in the multi-ethnic population based Dallas Heart Study (DHS) between a normal aging group versus the remaining participants aging with comorbid hypertension, obesity or diabetes.
Methods
Study Population and Participants
The DHS is a large multi-ethnic probability-based population sample of adult English- or Spanish-speaking Dallas County residents5. The DHS was approved by the University of Texas Southwestern Medical Center Institutional Review Board, and each participant gave written informed consent to participate. Between September 2007 and December 2009, 3T brain MRI and clinical evaluation was obtained for 2077 participants. 29 participants were excluded for identified pathology, imaging artifact or error precluding automated WMH analysis and 37 were excluded for self-reported stroke resulting in 2,011 participants for this study. For more details regarding the study population, please see supplementary methods online at http://stroke.ahajournals.org.
Normal and Pathologic Aging Definitions
Hypertension was defined as an average systolic blood pressure ≥140 mm Hg or an average diastolic blood pressure ≥90 mm Hg from 3 separate measurements or current treatment with antihypertensive medication. Diabetes mellitus was defined by self-report accompanied by use of anti-hyperglycemic medication, elevated serum glucose (fasting > 126 mg/dL [7.0 mmol/L] or non-fasting glucose > 200 mg/dL [11.1mmol/L])6, including type 1 and 2 together. In the remaining 1725 (86%) participants with comorbidities, there were 973 (56%) with hypertension, 245 with diabetes (14%), and 1578 (91%) with abnormal BMI.
Procedures and Measures
Systolic and diastolic blood pressures (mmHg) were reported as the mean of the final three out of 5 recordings. Hypertension therapy, sex and ethnicity were self-reported. BMI was calculated based on measured height and weight. Serum glucose was obtained from early morning venous sampling and fasting state verified.
Outcome Variable
The outcome measure for our study was WMH volume (mL) automatically quantified from 2D FLAIR and 3D MP-Rage brain imaging acquired during DHS2 on a 3T MRI system (Achieva, Philips Medical Systems) whose details have previously been described7.
Statistical Analysis
Interaction testing was performed for presence of comorbidities and age in predicting WMH. To explore an age-related threshold effect for WMH, an analysis using cubic splines was performed to obtain a mathematically optimal fitted curve of log WMH by age for the entire cohort. Within and between group difference in slope of the WMH vs age regression was compared for the normal and comorbidities group using a linear contrast test of the beta coefficients and interaction terms before and after age 50 where a threshold was identified in spline analysis. Analyses were adjusted for gender, ethnicity and intracranial volume as estimated by FSL. Predicted WMH volumes were obtained from the linear regression analysis by substituting 5 year increments of age into the model. Statistical analyses were performed using SAS software, version 9.2 (SAS Institute, Inc., Cary, NC).
Results
Characteristics for the 2011 participants are shown in table 1. In addition to having significantly greater BMI, blood pressure and serum glucose, the comorbidities group also had a higher proportion of Blacks, fewer Whites and fewer females (p<0.001 for each).
Table 1.
Basic demographics for Normal Aging and Aging with Comorbidities Groups
| Characteristic | Normal Aging (n=285) | Aging with Comorbidities (n=1726) |
|---|---|---|
| Black | 89 (31%) | 802 (47%) |
| White | 131 (46%) | 555 (32%) |
| Hispanic | 46 (16%) | 287 (17%) |
| Other / Missing | 19 (7%) | 82 (5%) |
| Female | 173 (61%) | 1000 (58%) |
| Age | 46.4±10.1 | 50.6±10.5 |
| Age >= 50 | 103 (36%) | 800 (54%) |
| BMI | 22.5±1.8 | 30.7±5.2 |
| Systolic BP | 117.5±11.2 | 132.6±18.4 |
| Diastolic BP | 74.4±7.2 | 81.3±8.8 |
| Blood glucose | 89.0±8.5 | 102.5±37.6 |
Frequency data are n(%) and continuous data is n±SD. Definition of normal and comorbidities groups based on absence or presence, respectively, of hypertension, diabetes and / or abnormal BMI.
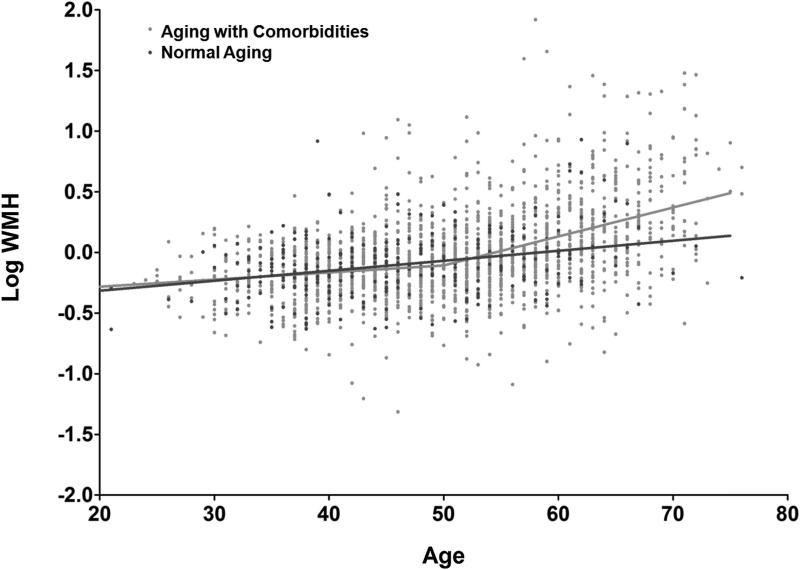
A significant interaction was seen between age and presence of comorbidities in predicting WMH (p= 0.005), indicating the relationship varied with increasing age. A threshold effect was seen with greater increase in log WMH per year starting in the sixth decade, so the analysis was stratified at that point. For the normal aging group, each year of age was associated with 0.006 greater log of WMH volume (SD 0.003, p=0.029). No significant age-related threshold of greater WMH volume after 50 years was seen in the normal group (p=0.173). For individuals with comorbidities, each year of total age was associated with 0.007 greater log WMH (SD 0.001, p<0.0001) with a further increase for each year after age 50 of 0.018 log WMH (SD 0.002, p<0.001), see Figure 1. Prior to age 50 there was no statistically significant difference between normal and comorbidities groups in slope (p=0.752) but beyond age 50, the slopes differed significantly (p=0.008). No significant age related differences were seen for between groups categorized by presence or absence of each of the 3 individual comorbidities (for more details, please see supplementary results online at http://stroke.ahajournals.org). Estimated WMH volumes for normal and comorbidities groups and between-group differences are depicted in Table 2.
Figure 1.
WMH values for age among those with and without comorbid hypertension, abnormal BMI and diabetes.
Participants with comorbidities are in light gray while those in a normal aging group without comorbidities are in dark gray. A significant threshold was seen at age 50 for the group with comorbidities, with greater log WMH volumes per year of age after this point.
Table 2.
Expected WMH Volumes for Selected Ages WMH ml (SE)
| Age | Normal | Comorbidities | Difference |
|---|---|---|---|
| 30 | 0.62 (0.05) | 0.6 (0.03) | 0.02 (0.06) |
| 35 | 0.66 (0.04) | 0.64 (0.02) | 0.02 (0.04) |
| 40 | 0.71 (0.03) | 0.68 (0.02) | 0.03 (0.04) |
| 45 | 0.76 (0.03) | 0.73 (0.02) | 0.03 (0.04) |
| 50 | 0.81 (0.05) | 0.78 (0.02) | 0.03 (0.05) |
| 55 | 0.93 (0.04) | 1.03 (0.02) | 0.1 (0.04) |
| 60 | 1.06 (0.07) | 1.36 (0.03) | 0.3 (0.08) |
| 65 | 1.21 (0.12) | 1.79 (0.06) | 0.58 (0.13) |
| 70 | 1.39 (0.19) | 2.35 (0.11) | 0.96 (0.22) |
Discussion
After age 50, but not before, our results show comorbid hypertension, abnormal BMI and/or diabetes to be associated with significantly larger WMH volumes for age. Small age related differences in WMH volume were seen prior to age 50, with no significant difference between normal aging and aging with comorbid hypertension, abnormal BMI and/ or diabetes. The presence of these comorbidities resulted in significantly larger age related differences in WMH volumes after age 50. No significant age related differences were seen for each of the comorbidities when evaluated individually, highlighting the importance of considering synergism among comorbidities. Compared with normal aging, aging with these comorbidities resulted on average in 0.3 ± 0.08 ml or 1.3× more WMH at age 60, 0.58 ± 0.13 ml or 1.5× more at age 65 and 0.96 ± 0.22 ml or 1.7× more at age 70.
The age of onset for expression of WMH in the population and the expected volume for age, particularly for younger individuals, has been uncertain8. Our study provides a set of normative values for WMH volumes both for healthy aging and aging in the presence of comorbidities in a multi-ethnic cohort.
Supplementary Material
Acknowledgments
None.
Sources of Funding: Grant UL1TR000451 and KL2TR000453 from the National Center for Advancing Translational Sciences, National Institutes of Health.
Footnotes
Disclosures: None.
References
- 1.Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: Systematic review and meta-analysis. BMJ. 2010;341:c3666–c3666. doi: 10.1136/bmj.c3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Provenzano FA, Muraskin J, Tosto G, Narkhede A, Wasserman BT, Griffith EY, et al. White matter hyperintensities and cerebral amyloidosis: Necessary and sufficient for clinical expression of alzheimer disease? JAMA Neurol. 2013:1–7. doi: 10.1001/jamaneurol.2013.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chowdhury MH, Nagai A, Bokura H, Nakamura E, Kobayashi S, Yamaguchi S. Age-related changes in white matter lesions, hippocampal atrophy, and cerebral microbleeds in healthy subjects without major cerebrovascular risk factors. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2011;20:302–309. doi: 10.1016/j.jstrokecerebrovasdis.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 4.Fillit H, Nash DT, Rundek T, Zuckerman A. Cardiovascular risk factors and dementia. Am J Geriatr Pharmacother. 2008;6:100–118. doi: 10.1016/j.amjopharm.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Victor RG, Haley RW, Willett DL, Peshock RM, Vaeth PC, Leonard D, et al. The dallas heart study: A population-based probability sample for the multidisciplinary study of ethnic differences in cardiovascular health. Am J Cardiol. 2004;93:1473–1480. doi: 10.1016/j.amjcard.2004.02.058. [DOI] [PubMed] [Google Scholar]
- 6.Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 1997;20:1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 7.Hulsey KM, Gupta M, King KS, Peshock RM, Whittemore AR, McColl RW. Automated quantification of white matter disease extent at 3 t: Comparison with volumetric readings. Journal of Magnetic Resonance Imaging. 2012;36:305–311. doi: 10.1002/jmri.23659. [DOI] [PubMed] [Google Scholar]
- 8.Grueter BE, Schulz UG. Age-related cerebral white matter disease (leukoaraiosis): A review. Postgrad Med J. 2012;88:79–87. doi: 10.1136/postgradmedj-2011-130307. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.