Abstract
Oral polio vaccine has been used successfully as a powerful tool to control the spread of wild polioviruses throughout the world; however, during replication in under immunized children, some vaccine viruses revert and acquire the neurovirulent phenotypic properties. In this study, we describe the evolution and circulation of Vaccine-Derived Polioviruses (VDPVs) in Helmand province of Afghanistan. We investigated 2646 AFP cases of Afghan children from June 2009–February 2011 and isolated 103 (04%) vaccine viruses, 45(1.7%) wild type polioviruses and six (0.22%) type 2 circulating vaccine-derived polioviruses (cVDPVs). These cVDPVs showed 97.7%–98.2% nucleotide and 98%–98.7% amino acid homology in VP1 region on comparison with Sabin type 2 reference strain. All these cVDPVs had two signature mutations of neurovirulent phenotypes and 12 additional mutations in P1 capsid region that might also have contributed to increase neurovirulence and replication. Phylogenetic analysis revealed that all these viruses were closely related and originated from previously reported Sabin like 2 virus from Pakistan which did not conform to the standard definition of VDPVs at that time. It was also observed that initial OPV dose was administered approximately 9 months prior to the collection of first stool specimen of index case. Our findings support that suboptimal surveillance and low routine immunization coverage have contributed to the emergence and spread of these viruses in Afghanistan. We therefore recommend high quality immunization campaigns not only in affected district Nad Ali but also in the bordering areas between Pakistan and Afghanistan to prevent the spread of cVDPVs.
Introduction
Poliovirus (PV), the causative agent of acute paralytic disease poliomyelitis, is a member of enterovirus genus of Picornaviridae family and has three distinct serotypes (PV1, PV2 and PV3) [1]. It contains a positive sense 7.5 kb long single stranded RNA genome enclosed by icosahedral capsid which is made of four structural viral proteins VP1, VP2, VP3 and VP4. In addition, its genome also contains non-structural viral proteins (2A, 2B, 2C, 3A, 3B, 3C and 3D), 5′ and 3′ un-translated regions (UTRs) and a poly A tail [1].
For over five decades, poliomyelitis has been efficiently controlled by a live attenuated oral polio vaccine (OPV) which is amongst the best known viral vaccines in practice albeit with two disadvantages. Firstly, it can cause paralysis in extremely rare cases (approximately 1 per 2.7 million first doses of vaccine). Secondly, OPV viruses are genetically unstable [2] and vaccine strains may revert to pathogenic phenotypes during replication in human gut due to high error frequency during RNA synthesis (approximately 10−4 per base pair per replication cycle) [3]. These substitutions accumulate at an approximate rate of 1% per annum in viral protein 1 (VP1) region of genome [4] and can be used for estimation of evolutionary intervals between poliovirus isolates.
According to World Health Organization (WHO) recommendations, these OPV-derived reverent strains with 1% or more nucleotide mutations in the VP1 region are defined as Vaccine-Derived Polioviruses (VDPVs) [5]. In 2011, this criterion was modified down to >0.6% for only type2 VDPVs [6], [7].VDPVs have been classified into two well-defined categories known as Immunodeficiency associated VDPVs (iVDPVs) and Circulating VDPVs (cVDPVs) [7]. iVDPVs have been isolated from immune deficient patients in the United Kingdom (2000), United States (2008) [8], [9], Argentina (2009), Iran (2011), South Africa (2011) and China (2012) [10]. The second type, cVDPVs, arises as a result of sustained person to person transmission within an inadequately immunized population and first outbreak of these VDPVs was reported from Hispaniola (Haiti and the Dominican Republic) in 2001 [11]. Later on, these cVDPVs have been isolated in Egypt, Philippines, China, Madagascar, Nigeria, Myanmar, Indonesia, Cambodia, Somalia, Yemen, Niger, DRC and the United States [10]. Recently, a third category named as ambiguous VDPVs (aVDPVs) has emerged, which includes all those VDPVs whose ultimate source or host remained unidentified [12]. This type of polioviruses have been detected in Peru (1983 and 2011), Israel (1998 and 2006), Pakistan (2000), Romania (2002), Laos (2004), Madagascar (2005), Minnesota (2005), Myanmar (2006), Nigeria (2002, 2006 and 2012), Argentina (2011), DRC (2011), Finland (2011), India(2011), Sudan (2012) and Yemen (2012) [13], [14].
In October 1999, last wild poliovirus type 2 (WPV2) was isolated in Aligarh, Uttar Pradesh, India [15]. Since then, no WPV2 has been reported globally, however the largest outbreak of type 2 cVDPVs was recorded in Nigeria from 2005 to 2009 [16]. This outbreak provided a unique opportunity to analyze the pathogenicity of the virus, its associated disease severity, and the effectiveness of control measures to stop the spread of cVDPVs [17]. In this report, we describe the characterization of six cVDPV2 strains isolated from Acute Flaccid Paralysis (AFP) cases from Nad Ali district of Helmand province in Southern Afghanistan that remained in circulation for at least one year (2010 to 2011).
Materials and Methods
Sample Collection
Two stool samples were collected at 24 hours interval from suspected AFP cases within 14 days of paralysis onset and sent to WHO Regional Reference Laboratory for Polio Eradication Initiative (WHO RRL for PEI) at National institute of Health (NIH) Islamabad, Pakistan through WHO Afghanistan coordinated effort. The study concept and design was approved through the Pakistan's National Institute of Health Internal Review Board. The samples were collected after informed and written consent from the patient's parents/guardians. The samples were received within 72 hours after the collection of second specimen maintaining reverse cold chain.
Virus Isolation and Characterization
The samples were processed according to WHO Polio laboratory protocol and clarified supernatant from each sample was inoculated on RD and L20B cell lines [18]. All L20B-positive isolates were subjected to real time reverse transcriptase polymerase chain reaction (rRT-PCR) for PV serotyping, intratypic differentiation (ITD) and primary screening for suspected VDPVs using WHO protocol [19]. Suspected VDPVs were referred for nucleotide sequencing of VP1 gene encoding structural protein region for final confirmation.
Nucleic Acid sequencing
Viral RNA extraction, reverse transcriptase-PCR amplification and cycle sequencing of P1 capsid and 5′UTR were performed as described previously [20]–[22], using primers listed in Table 1. Bi-directional sequencing was performed using Big Dye Terminator kit v3.1 (Applied Biosystems) and each nucleotide was sequenced at least once from each strand.
Table 1. Sequence and position of Primer pairs used for PCR and Sequencing.
| Primer Name | Primer Sequence | Polarity | Region |
| 5′ UTR | TTAAAACAGCTCTGGGGTTG | Sense | 5′UTR |
| 241c | TACTGGGCTTTTCGAAGTAC | Antisense | 5′UTR |
| UG53 | TGGCTGCTTATGGTGACAAT | Sense | 5′UTR |
| 921c | CGTCCTTAATGGGTTCGGTG | Antisense | 5′UTR |
| 1737 | GTGTWGTGAGTTCAA[Y]GG | Sense | VP4 |
| UC24 | ATCATGGTGTCTATTTCTGC | Antisense | VP3 |
| UG1 | TTTGTGTCAGCGTGTAATGA | Sense | VP1 |
| UC1 | GAATTCCATGTCAAATCTAGA | Antisense | VP1 |
| Y7 | GGGTTTGTGTCAGCCTGTAATGA | Sense | VP3 |
| Q8 | AAGAGGTCTCTRTTCCACAT | Antisense | 2A |
| PV1A | TTIAIIGCRTGICCRTTRTT | Antisense | VP1 |
| PV4S | ACITAYAARGAYACIGTICA | Sense | VP1 |
Phylogenetic analysis
Sequence data was edited and aligned through Sequencher 4.10.1 (Gene Codes Corporation, USA). MEGA 5 software (www.megasoftware.net) was used to calculate the genetic distances and phylogenetic tree was constructed by the neighbor-joining algorithm [23] with Kimura 2-parameter model using 1000 bootstrap replicate values to correct multiple substitutions rate at a site [24].
Estimation of the date of initiating OPV dose
We used presumption that nucleotide substitutions occurred in all three poliovirus serotypes at constant rates of 3.2% synonymous substitutions per synonymous site per year (Ks) and 1.1% total substitutions per site per year (Kt) in the 2637-nt P1/capsid region [25]. The approximate “age” (i.e. the time elapsed after the onset of their independent evolution from vaccine) was then estimated from Ks (corrected proportion of synonymous substitutions), Kt (all substitutions per site) values and the date of specimen collection [25].
Nucleotide sequence accession numbers
5′UTR and P1 coding region sequences of the type 2 polioviruses described in this study were submitted to GenBank library under accession numbers KF322152 (AFG09-1321), KF322153 (AFG10-1094), KF322154 (AFG10-1125), KF322155 (AFG10-1230), KF322156 (AFG10-1924), KF322157 (AFG10-2273), KF322158 (AFG11-066).
Results
Stool samples from 2646 Afghan children collected from June 2009 to February 2011 were processed for virus isolation and characterization. Out of these, 531 (20%) cases were positive for non-polio enteroviruses, 154 (6%) for polioviruses while 1961 (74%) cases were reported as negative. Among PV positive cases, 109 (71%) were positive for vaccine viruses (Sabin-like PVs) and 45 (29%) for wild type polioviruses on intra-typic differentiation. Sabin like type 1 polioviruses were detected in the highest proportion 51.4% (n = 56) followed by type 3 27.5% (n = 30) and type 2 polioviruses 21.1% (n = 23) respectively. All Sabin-like (SL) viruses were screened for VDPVs using rRT-PCR and 12 positive cases were detected which were sequenced for VP1 gene. Comparative analysis of VP1 sequence of these isolates with respective reference Sabin strain revealed that 6 isolates were Sabin like (SL1 = 2, SL2 = 3 and SL3 = 1) and remaining six were confirmed as VDPV type2.
Among SL2 viruses, only one virus (AFG09/1321) isolated during 2009 from a 12 months old male with quadriplegia from district Bust of Helmand province showed 0.9% nucleotide and 1% amino acid divergence in VP1 region respectively when compared with Reference Sabin 2 strain (GenBank accession No. AY184220.1). It was reported as SL2 because it did not fulfill the old definition of VDPV (≥1% VP1 nucleotide divergence when compared to reference Sabin-2 strain) however the new definition (>0.6% VP1 nucleotide divergence when compared to reference Sabin-2 strain) classified this isolate as cVDPV.
All cases with type2 VDPVs isolation were resident of district Nad Ali of Helmand province and showed residual neurological weakness upon 60 days follow up (Table 2). However, one child AFG10/1125 died within 60 days period (Table 2). Based on their close genetic relatedness and geographical location, these six VDPVs were designated as cVDPVs.
Table 2. Demographic description of index case (AFG09/1321) and cVDPVs circulating in Southern Afghanistan.
| Sample I.D | Sex | Age (Months) | Symptoms | OPV Doses | Data of Paralysis | Date of Specimen Collection | 60 days follow up |
| AFG09/1321 | Male | 12 | Weakness of all 4 limbs and neck muscles | Unknown | 24-Jul-09 | 29-Jul-09 | Weakness limited to left lower limb but spastic rather than flaccid |
| AFG10/1094 | Female | 18 | Paralysis of left leg with decreased muscle tone and reflexes | 0 | 10-Jun-10 | 18-Jun-10 | Residual weakness |
| AFG10/1125 | Male | 27 | Paralysis of both leg with decreased muscle tone and reflexes | 1 | 16-Jun-10 | 23-Jun-10 | Died |
| AFG10/1230 | Female | 42 | Paralysis of right leg with decreased muscle tone and reflexes | 15 | 2-Jul-10 | 7-Jul-10 | Residual weakness |
| AFG10/1924 | Male | 11 | Paralysis of both leg with decreased muscle tone and reflexes | 2 | 23-Oct-10 | 29-Oct-10 | Residual weakness |
| AFG10/2273 | Male | 10 | Paralysis of both leg with decreased muscle tone and reflexes | 1 | 18-Dec-10 | 24-Dec-10 | Residual weakness |
| AFG11/066 | Female | 36 | Paralysis of both leg with decreased muscle tone and reflexes | 2 | 20-Jan-11 | 24-Jan-11 | Residual weakness |
These viruses shared 98.2%–97.7% nucleotide and 98.7%–98% amino acid homology in viral capsid protein 1 (VP1) when compared with Sabin type 2 reference strain (Table 3). The overall mean nucleotide and amino acid homologies among these cVDPVs in VP1 region were 99% and 99.6% respectively. Synonymous and non-synonymous mutation detection rates in VP1 region ranged from 4.1% to 6.4% and 0.6% to 1% respectively.
Table 3. Characteristics of cVDPVs and index Sabin like type 2 strain (AFG09/1321).
| Virus | Serotype Identification by rRT-PCR | Intratypic Differentiation By rRT-PCR | VDPV screening by rRT-PCR | Nucleotide Diversity from Sabin 2 in VP1 (%) | Amino acid Diversity from Sabin 2 in VP1 (%) |
| AFG09/1321 | aP2 | bSL | Suspected VDPV | 0.9 | 1 |
| AFG10/1094 | aP2 | bSL | Suspected VDPV | 2.1 | 1.7 |
| AFG10/1230 | aP2 | bSL | Suspected VDPV | 2 | 1.3 |
| AFG10/1125 | aP2 | bSL | Suspected VDPV | 1.8 | 1.3 |
| AFG10/1924 | aP2 | bSL | Suspected VDPV | 2.7 | 2 |
| AFG10/2273 | aP2 | bSL | Suspected VDPV | 1.8 | 1.3 |
| AFG11/066 | aP2 | bSL | Suspected VDPV | 2.3 | 1.7 |
P2, Poliovirus type 2.
SL, Sabin-like.
All cVDPVs showed A→G mutation at nucleotide position 481 in 5′UTR and U→C at nucleotide 2909 in VP1 coding region, leading to amino acid substitution of isoleucine by threonine at codon position 143 (Table 4). Furthermore, five mutations (U63→C, U156→C, U398→C, U570→A, and A736→G) observed in 5′UTR were common across all cVDPVs (Table 4) while two nucleotide insertions were also observed in AFG10/2273 and AFG11/066 at position 89(C) and 91(G) respectively (Table 4).
Table 4. Nucleotide mutations and Amino acid substitutions identified in 5′UTR and P1 Coding region of Index case (1321) and cVDPVs.
| Region | Nucleotide | Amino acid | ||||||||||||||||
| Position | Sabin 2 | 1321 | 1094 | 2273 | 1924 | 1230 | 1125 | 66 | Position | Reference Sabin 2 | 1321 | 1094 | 2273 | 1924 | 1230 | 1125 | 66 | |
| 5′ | 63 | U | C | C | C | C | C | C | ||||||||||
| 78 | C | A | ||||||||||||||||
| *89 | : | G | ||||||||||||||||
| 90 | A | U | C | |||||||||||||||
| *91 | : | C | ||||||||||||||||
| 92 | U | C | C | C | C | C | ||||||||||||
| 97 | U | A | A | A | A | A | A | |||||||||||
| 156 | U | C | C | C | C | C | C | C | ||||||||||
| 259 | U | C | ||||||||||||||||
| 398 | U | C | C | C | C | C | C | C | ||||||||||
| 403 | U | A | ||||||||||||||||
| 425 | U | C | ||||||||||||||||
| 481 | A | G | G | G | G | G | G | G | ||||||||||
| 517 | C | U | ||||||||||||||||
| 565 | G | A | A | A | ||||||||||||||
| 570 | U | A | A | A | A | A | A | |||||||||||
| 575 | U | C | ||||||||||||||||
| 610 | U | C | C | |||||||||||||||
| 645 | U | C | C | C | C | C | ||||||||||||
| 657 | U | C | ||||||||||||||||
| 710 | A | G | G | |||||||||||||||
| 716 | A | U | ||||||||||||||||
| 719 | C | U | U | |||||||||||||||
| 727 | G | A | ||||||||||||||||
| 736 | A | G | G | G | G | G | G | |||||||||||
| 744 | A | C | ||||||||||||||||
| VP4 | 753 | C | U | U | U | U | ||||||||||||
| 756 | C | U | ||||||||||||||||
| 759 | A | G | ||||||||||||||||
| 780 | A | G | ||||||||||||||||
| 786 | C | U | ||||||||||||||||
| 798 | C | U | U | U | U | U | ||||||||||||
| 873 | C | U | U | U | U | U | U | U | ||||||||||
| 879 | A | G | G | G | G | G | ||||||||||||
| 888 | A | U | ||||||||||||||||
| 931 | A | G | 62 | Ille | Val | |||||||||||||
| 945 | C | U | ||||||||||||||||
| 954 | C | U | ||||||||||||||||
| VP2 | 963 | C | U | |||||||||||||||
| 981 | U | C | ||||||||||||||||
| 999 | G | A | ||||||||||||||||
| 1006 | C | U | ||||||||||||||||
| 1014 | U | C | C | |||||||||||||||
| 1071 | U | C | ||||||||||||||||
| 1122 | C | U | U | U | U | U | U | |||||||||||
| 1140 | G | A | ||||||||||||||||
| 1152 | A | G | G | G | G | G | G | |||||||||||
| 1179 | C | U | U | U | ||||||||||||||
| 1290 | C | U | U | U | U | U | ||||||||||||
| 1296 | U | A | ||||||||||||||||
| 1308 | U | C | ||||||||||||||||
| 1322 | G | U | 123 | Gly | Val | |||||||||||||
| 1329 | U | C | A | 125 | Phe | Leu | ||||||||||||
| 1348 | U | C | ||||||||||||||||
| 1356 | U | C | ||||||||||||||||
| 1380 | A | G | G | |||||||||||||||
| 1419 | A | G | ||||||||||||||||
| 1431 | U | C | C | C | C | C | C | |||||||||||
| 1435 | A | G | 161 | Thr | Ala | |||||||||||||
| 1437 | C | U | ||||||||||||||||
| 1440 | U | C | C | C | C | C | C | |||||||||||
| 1443 | U | C | ||||||||||||||||
| 1446 | C | A | ||||||||||||||||
| 1464 | A | G | G | G | G | |||||||||||||
| 1557 | U | C | ||||||||||||||||
| 1638 | C | U | ||||||||||||||||
| 1651 | C | U | ||||||||||||||||
| 1656 | G | A | A | A | A | A | A | A | ||||||||||
| 1659 | A | G | G | |||||||||||||||
| 1674 | U | C | C | |||||||||||||||
| 1686 | U | C | ||||||||||||||||
| 1689 | G | A | A | A | A | A | A | A | ||||||||||
| 1695 | C | U | U | U | U | U | U | U | ||||||||||
| 1749 | C | U | ||||||||||||||||
| 1752 | U | C | C | |||||||||||||||
| VP3 | 1833 | G | A | |||||||||||||||
| 1866 | C | U | U | U | U | U | U | |||||||||||
| 1930 | C | U | 55 | Leu | Phe | |||||||||||||
| 1939 | A | U | U | U | U | U | U | 58 | Thr | Ser | Ser | Ser | Ser | Ser | Ser | |||
| 1953 | G | A | ||||||||||||||||
| 1981 | U | C | C | C | C | C | C | |||||||||||
| 1990 | A | G | G | G | G | G | G | G | 75 | Thr | Ala | Ala | Ala | Ala | Ala | Ala | Ala | |
| 2010 | G | A | A | A | A | A | ||||||||||||
| 2050 | U | C | ||||||||||||||||
| 2085 | C | U | ||||||||||||||||
| 2100 | A | G | G | |||||||||||||||
| 2115 | U | C | ||||||||||||||||
| 2148 | C | U | ||||||||||||||||
| 2151 | A | G | ||||||||||||||||
| 2166 | U | A | ||||||||||||||||
| 2181 | A | G | G | G | G | |||||||||||||
| 2205 | A | G | G | G | G | G | G | |||||||||||
| 2211 | A | G | ||||||||||||||||
| 2273 | G | C | C | C | ||||||||||||||
| 2274 | U | C | ||||||||||||||||
| 2286 | U | C | C | |||||||||||||||
| 2310 | C | U | U | U | U | U | U | U | ||||||||||
| 2316 | U | C | C | |||||||||||||||
| 2322 | A | G | G | G | G | G | G | |||||||||||
| 2331 | C | U | ||||||||||||||||
| 2334 | C | U | ||||||||||||||||
| 2361 | U | C | ||||||||||||||||
| 2397 | C | U | U | U | U | U | ||||||||||||
| 2430 | U | C | C | C | C | C | C | |||||||||||
| 2451 | A | U | ||||||||||||||||
| 2469 | G | A | A | |||||||||||||||
| VP1 | 2499 | U | C | 10 | Val | |||||||||||||
| 2509 | G | A | A | A | A | A | A | Ille | Ille l | Ille | Ille | Ille | Ille | Ille | ||||
| 2537 | U | G | G | G | G | G | G | 19 | Val | Gly | Gly | Gly | Gly | Gly | Gly | |||
| 2543 | C | U | ||||||||||||||||
| 2547 | U | C | ||||||||||||||||
| 2553 | C | U | ||||||||||||||||
| 2555 | A | G | G | G | G | G | G | G | 25 | Asn | Ser | Ser | Ser | Ser | Ser | Ser | Ser | |
| 2558 | G | A | 26 | Ser | Asn | |||||||||||||
| 2568 | C | U | ||||||||||||||||
| 2580 | C | U | U | U | U | U | U | U | ||||||||||
| 2611 | U | C | ||||||||||||||||
| 2622 | G | A | A | A | A | A | ||||||||||||
| 2670 | G | A | ||||||||||||||||
| 2677 | G | A | 66 | Val | Ile | |||||||||||||
| 2694 | G | A | ||||||||||||||||
| 2706 | C | U | ||||||||||||||||
| 2710 | G | A | A | 67 | Val | Ile | Ile | |||||||||||
| 2727 | A | G | G | G | G | G | G | G | ||||||||||
| 2739 | C | U | U | U | U | U | U | U | ||||||||||
| 2766 | U | C | C | C | C | C | ||||||||||||
| 2775 | A | C | ||||||||||||||||
| 2814 | U | A | A | |||||||||||||||
| 2829 | U | A | ||||||||||||||||
| 2832 | A | G | ||||||||||||||||
| 2838 | A | G | G | G | G | G | ||||||||||||
| 2853 | U | C | ||||||||||||||||
| 2883 | C | U | U | U | U | U | ||||||||||||
| 2909 | U | C | C | C | C | C | C | C | 143 | Ile | Thr | Thr | Thr | Thr | Thr | Thr | Thr | |
| 2919 | U | C | ||||||||||||||||
| 2925 | A | G | G | G | G | G | ||||||||||||
| 2928 | U | C | C | C | C | C | ||||||||||||
| 2958 | U | C | C | C | C | C | C | |||||||||||
| 2992 | A | G | 171 | Asn | Asp | |||||||||||||
| 3066 | A | G | ||||||||||||||||
| 3075 | C | U | ||||||||||||||||
| 3150 | U | A | A | A | A | A | ||||||||||||
| 3138 | U | A | ||||||||||||||||
| 3195 | A | G | ||||||||||||||||
| 3219 | U | C | C | C | C | C | C | C | ||||||||||
| 3234 | G | A | ||||||||||||||||
| 3237 | G | A | ||||||||||||||||
| 3261 | C | U | ||||||||||||||||
| 3358 | C | U | ||||||||||||||||
| 3459 | A | G | ||||||||||||||||
Comparison of complete P1 capsid region with reference Sabin 2 strain showed 1.1%–2.3% nucleotide and 0.5% to 1% amino acid variation. The corrected proportion of synonymous and non-synonymous nucleotide substitutions in P1 capsid were 4.2% to 9.3% and 0.2% to 0.4% respectively. Various silent substitutions found common in all isolates were C873→U, G1656→A, G1689→A, C1695→U, C2310→U, U2430→C, C2580→U, A2727→G, C2739→U, A2925→G, U2928→C and U3219→C (Table 4). Multiple synonymous mutations have also been observed in all studied cVDPVs and index case (AFG09/1321) as well (Table 4). AFG10/1230 had two non-synonymous mutations in VP2 resulting two amino acid changes; Gly123→Val and Phe125→Leu. Similarly in one isolate (AFG10/1924) threonine was substituted by alanine at codon position 161 in VP2 (Table 4).
Amino acid comparison of VP3 sequences showed the substitution of Thr75→Ala in all cVDPVs and AFG09/1321, due to A→G replacement at position 1990, located in the immediate vicinity of antigenic site 3B. Substitution of Thr58→Ser in antigenic site 3a (AgS3) was also observed in all studied cVDPV strains; whereas the Leu55→Phe change in 3a (AgS3) was only observed in AFG09/1321 (Table 4). Viral capsid protein 4 (VP4) showed 9 nucleotide changes. The VP4 amino acid sequence of all studied strains remained unchanged and only one amino acid substitution Ille62→Val has been identified in AFG10/2273.
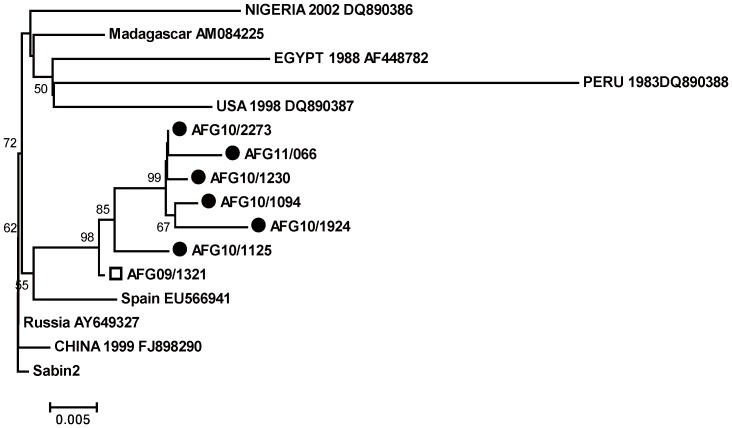
The phylogenetic tree constructed with previously reported cVDPVs from Spain EU566941, Nigeria DQ890386, Russia AY649327, China FJ898290, Madagascar AM084225, USA DQ890387, Peru DQ890388 and Egypt AF448782) revealed that all Afghan cVDPVs belonged to one lineage that originated from AFG09/1321 (Fig. 1). In turn, this isolate appears to have evolved from Sabin 2 vaccine strain and was marked as the index case for the subsequently circulating VDPVs. The approximate time of initiating OPV infection was calculated by Ks and Kt values and date of specimen collection. Analysis showed that index case (AFG09/1321) had 2.5% and 0.8% Ks and Kt value respectively, therefore the estimated time of initial OPV dose administration was determined to be approximately 9 months before the onset of paralysis.
Figure 1. All cVDPVs type2 isolated from Nad Ali district of Helmand province are indicated with round circle filled in black color.
Other globally reported cVDPVs type 2 has retrieved from GenBank to reconstruct phylogenetic tree from VP1 coding sequences using neighbor-joining algorithm with Kimura 2-parameter substitution model.
Discussion
Oral Polio Vaccine has been demonstrated as a powerful tool to stop transmission of PVs for a period spanning over five decades [26]. Although it is considered a safe vaccine and protects individuals through humoral and mucosal immunity, neurovirulent phenotypes known as VDPVs emerge during the course of replication [27], [28]. These VDPVs either emerge during persistent infections in immunodeficient individuals or can evolve during continuous transmission of vaccine viruses in a community where immunization coverage is deficient or patchy [29]. Furthermore, overcrowding, high birth rates, poor sanitation and the absence of wild virus of same serotype as that of VDPVs are major risk factors that facilitate emergence of these viruses and also trigger establishment of numerous independent endemic chains of transmissions [30].
Weak routine immunization and suboptimal campaign quality were the major challenges in southern Afghanistan. Nad Ali is the most populous district of Southern Afghanistan with target population of 99,333 children under 5 years of age. This is one of the districts of Afghanistan that remained endemic for wild polioviruses during 2006 to 2010. Based on AFP surveillance data reports, routine coverage of trivalent oral poliovirus vaccine (tOPV) was 13% during 2008–2009 in South Afghanistan [31]. Therefore during 2008–2009, large scale house to house supplemental immunization campaigns (SIAs) were conducted targeting children <5 years using different formulations (eight immunization rounds with trivalent OPV, eight monovalent type 1 (mOPV1) and four monovalent type 3 OPV (mOPV3), and one round of bivalent OPV containing poliovirus types 1 and 3 (bOPV), however, the vaccination coverage remained less than 50% of the total target population [31], [32]. The vaccination coverage data showed that over 50% of the target children were being missed during the last nine polio vaccination campaigns during 2008–09 [32]. Similarly in February 2010, the entire district could not be covered due to on-going military operation. In later vaccination campaigns during 2010 (March to June) 33–50% targeted children could not be accessed. A number of villages and towns were completely missed during the vaccination campaigns amongst areas where the 6 VDPV2 cases were detected [32]. Therefore suboptimal campaign coverage and inaccessibility to the target population played a major role in the evolution and spread of cVDPVs type 2 in Nad Ali while poor hygienic and sanitation conditions also facilitated viral transmission.
Sequence analysis of VP1 region revealed that the cVDPVs type 2 had evolved from an isolate AFG09/1321, that had been earlier notified as SL2 which did not fulfill the old criterion of VDPVs but in 2011, revised definition of cVDPVs (>0.6% divergent in VP1 region from type2 Sabin reference strain) justified and classified this isolate as cVDPV type 2. This virus carried two signature mutations of virulent phenotype and child also showed cardinal signs of poliomyelitis.
All previously reported mutations responsible for reversion and restoration of neurovirulent properties or elimination of temperature sensitive phenotypes of vaccine derivative were found in the cVDPVs in our study [30], [33]–[36]. However twelve mutations; C873→U, G1656→A, G1689→A, C1695→U, C2310→U, U2430→C, C2580→U, A2727→G, C2739→U, A2925→G, U2928→C and U3219→C were common to all these cVDPVs that have not been previously reported. These mutations may be responsible for increased neurovirulence, enhanced replication capacity and ultimately higher virus titers, prolong period of viral shedding and hence a heightened potential for person to person transmission [37]. Similar observations have previously been reported for revertant viruses [38] and need to be explored further through animal model studies.
The nucleotide data of VP1 gene confirmed the prolonged transmission of OPV derived type2 polioviruses in Nadi Ali district of Afghanistan. The VP1 mutations at aa 143 (Ile143→Thr) for type2 vaccine viruses replicating in humans were observed in all studied isolates. VDPVs screening rRT-PCR assay is also based on the presence of these mutations. Furthermore, the amino acid substitution at codon position VP3-75 (Thr75→Ser) was also found in all analyzed cVDPVs however, this change relates to results in Enzyme linked Immunosorbant (ELISA) ITD assay that was not conducted in this study [39]. None of the Afghan cVDPV except AFG10/2273 has shown amino acid change at codon position 62 (Ill62→Val) that lies within the inner side of the virion and chances for its immune-selection are quite improbable.
In conclusion, our findings provide concrete evidence that circulation of cVDPVs in Southern Afghanistan is result of sub-optimal immunization in the community. The vaccine virus which was progenitor of the reverted strains must have circulated for a long period of time to attain the neurovirulence properties. It is absolutely imperative that more vigorous and determined efforts are required to fill the large immunity gaps through strong routine immunization strategy followed by successive national immunization campaigns. Furthermore enhanced surveillance activities in the border areas of Pakistan and Afghanistan will be instrumental to stop the cross boarder transmission of these viruses and ultimately pave the way towards polio eradication from this region.
Funding Statement
The authors have no support or funding to report.
References
- 1. Agol VI (2006) Molecular mechanisms of poliovirus variation and evolution. Curr Top Microbiol Immunol 299: 211–259. [DOI] [PubMed] [Google Scholar]
- 2. Bellmunt A, May G, Zell R, Pring- Akerblom P, Verhagen W, et al. (1999) Evolution of polio virus type 1 during 5.5 years of prolonged enteral replication in an immune deficient patient. Virology 265: 178–184. [DOI] [PubMed] [Google Scholar]
- 3. Kew OM, Nottay BK (1984) Molecular epidemiology of polioviruses. Rev Infect Dis 6 Suppl 2: S499–504. [DOI] [PubMed] [Google Scholar]
- 4. Centers for Disease C, Prevention (2007) Update on vaccine-derived polioviruses–worldwide, January 2006–August 2007. MMWR Morb Mortal Wkly Rep 56: 996–1001. [PubMed] [Google Scholar]
- 5. Kew OM, Wright PF, Agol VI, Delpeyroux F, Shimizu H, et al. (2004) Circulating vaccine-derived polioviruses: current state of knowledge. Bull World Health Organ 82: 16–23. [PMC free article] [PubMed] [Google Scholar]
- 6. Centers for Disease C, Prevention (2011) Update on vaccine-derived polioviruses–worldwide, July 2009–March 2011. MMWR Morb Mortal Wkly Rep 60: 846–850. [PubMed] [Google Scholar]
- 7. Update on vaccine-derived polioviruses. MMWR Morb Mortal Wkly Rep 55: 1093–1097. [PubMed] [Google Scholar]
- 8. Alexander JP, Ehresmann K, Seward J, Wax G, Harriman K, et al. (2009) Transmission of imported vaccine-derived poliovirus in an under-vaccinated community-Minnesota, USA. J Infect Dis 199: 391–397. [DOI] [PubMed] [Google Scholar]
- 9. Centers for Disease C (2009) Update on Vaccine-Derived Polioviruses — Worldwide, January 2008–June 2009. MMWR Morb Mortal Wkly Rep 58: 1002–1006. [PubMed] [Google Scholar]
- 10. Update on vaccine-derived polioviruses–worldwide, April 2011-June 2012. MMWR Morb Mortal Wkly Rep 61: 741–746. [PubMed] [Google Scholar]
- 11. Kew O, Morris-Glasgow V, Landaverde M, Burns C, Shaw J, et al. (2002) Outbreak of poliomyelitis in Hispaniola associated with circulating type 1 vaccine-derived poliovirus. Science 296: 356–359. [DOI] [PubMed] [Google Scholar]
- 12. Expanding contributions of the global laboratory network for poliomyelitis eradication, 2000–2001. Wkly Epidemiol Rec 77: 133–137. [PubMed] [Google Scholar]
- 13. Centers for Disease C (2012) Update on Vaccine-Derived Polioviruses — Worldwide, April 2011–June 2012. MMWR Morb Mortal Wkly Rep 61: 741–746. [PubMed] [Google Scholar]
- 14. Centers for Disease C (2006) Update on Vaccine-Derived Polioviruses. MMWR Morb Mortal Wkly Rep 55: 1093–1097. [PubMed] [Google Scholar]
- 15.INDIA POLIO FACT SHEET. Available: http://wwwpolioeradicationorg/Portals/0/Document/InfectedCountries/India/PolioIndiaFactSheetpdf. Accessed on June 10, 2013.
- 16. Burns CC, Shaw J, Jorba J, Bukbuk D, Adu F, et al. (2013) Multiple independent emergences of type 2 vaccine-derived polioviruses during a large outbreak in northern Nigeria. J Virol 87: 4907–4922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jenkins HE, Aylward RB, Gasasira A, Donnelly CA, Mwanza M, et al. (2010) Implications of a circulating vaccine-derived poliovirus in Nigeria. N Engl J Med 362: 2360–2369. [DOI] [PubMed] [Google Scholar]
- 18. Polio laboratory manual - World Health Organization. WHO/IVB/0410 4: 2004. [Google Scholar]
- 19. Kilpatrick DR, Yang CF, Ching K, Vincent A, Iber J, et al. (2005) Rapid Group-, Serotype-, and Vaccine Strain-Specific Identification of Poliovirus Isolates by Real-Time Reverse Transcription-PCR Using Degenerate Primers and Probes Containing Deoxyinosine Residues. J Virol 79: 12623–12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Guillot S, Caro V, Cuervo N, Korotkova E, Combiescu M, et al. (2000) Natural Genetic Exchanges between Vaccine and Wild Poliovirus Strains in Humans. J Virol 74: 8434–8443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zurbriggen S, Tobler K, Abril C, Diedrich S, Ackermann M, et al. (2008) Isolation of sabin-like polioviruses from wastewater in a country using inactivated polio vaccine. Appl Environ Microbiol 74: 5608–5614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Karakasiliotis I, Paximadi E, Markoulatos P (2005) Evolution of a rare vaccine-derived multirecombinant poliovirus. J Gen Virol 86: 3137–3142. [DOI] [PubMed] [Google Scholar]
- 23. Saitou N, Nei M (1987) The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol 4: 406–425. [DOI] [PubMed] [Google Scholar]
- 24. Li WH, Ellsworth DL, Krushkal J, Chang BH, Hewett-Emmett D (1996) Rates of nucleotide substitution in primates and rodents and the generation-time effect hypothesis. Mol Phylogenet Evol 5: 182–187. [DOI] [PubMed] [Google Scholar]
- 25. Jorba J, Campagnoli R, De L, Kew O (2008) Calibration of multiple poliovirus molecular clocks covering an extended evolutionary range. J Virol 82: 4429–4440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dowdle WR, De Gourville E, Kew OM, Pallansch MA, Wood DJ (2003) Polio eradication: the OPV paradox. Rev Med Virol 13: 277–291. [DOI] [PubMed] [Google Scholar]
- 27. Domingo E, Martinez-Salas E, Sobrino F, de la Torre JC, Portela A, et al. (1985) The quasispecies (extremely heterogeneous) nature of viral RNA genome populations: biological relevance–a review. Gene 40: 1–8. [DOI] [PubMed] [Google Scholar]
- 28. Kinnunen L, Huovilainen A, Poyry T, Hovi T (1990) Rapid molecular evolution of wild type 3 poliovirus during infection in individual hosts. J Gen Virol 71 Pt 2: 317–324. [DOI] [PubMed] [Google Scholar]
- 29. Kew OM, Sutter RW, de Gourville EM, Dowdle WR, Pallansch MA (2005) Vaccine-derived polioviruses and the endgame strategy for global polio eradication. Annu Rev Microbiol 59: 587–635. [DOI] [PubMed] [Google Scholar]
- 30. Yang CF, Naguib T, Yang SJ, Nasr E, Jorba J, et al. (2003) Circulation of endemic type 2 vaccine-derived poliovirus in Egypt from 1983 to 1993. J Virol 77: 8366–8377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Progress towards poliomyelitis eradication in Afghanistan and Pakistan, 2008. Wkly Epidemiol Rec 84: 77–83. [PubMed] [Google Scholar]
- 32.Afghanistan W (2011) Report on Vaccine Derived polio Virus (VDPV) type 2 cases from Nade Ali/Marja district Helamand province during 2010–11 in Southern region of Afghanistan. Available: http://wwwpolioeradicationorg/Infectedcountries/Afghanistanaspx. Accessed on June 10, 2013.
- 33. Rakoto-Andrianarivelo M, Gumede N, Jegouic S, Balanant J, Andriamamonjy SN, et al. (2008) Reemergence of recombinant vaccine-derived polivirus outbreak in Madagascar. J Infect Dis 197: 1427–1435. [DOI] [PubMed] [Google Scholar]
- 34. Avellón A, Cabrerizo M, de Miguel T, Pérez-Breña P, Tenorio A, et al. (2008) Paralysis case andcontact spread of recombinant vaccine-derived poliovirus, Spain. Emerg Infect Dis 14: 1807–1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rousset D, Rakoto-Andrianarivelo M, Razafindratsimandresy R, Randriamanalina B, Guillot S, et al. (2003) Recombinant vaccine derived polioviruses in Madagascar. Emerging Infectious Diseases 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Razafindratsimandresy R, Joffret ML, Rabemanantsoa S, Andriamamonjy S, Heraud JM, et al. (2013) Reemergence of Recombinant Vaccine–derived Polioviruses in Healthy Children, Madagascar. Emerging Infectious Diseases 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gavrilin GV, Cherkasova EA, Lipskaya GY, Kew OM, Agol VI (2000) Evolution of circulating wild poliovirus and of vaccine-derived poliovirus in an immunodeficient patient: a unifying model. J Virol 74: 7381–7390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Friedrich F (2000) Molecular evolution of oral poliovirus vaccine strains during multiplication in humans and possible implications for global eradication of poliovirus. Acta Virol 44: 109–117. [PubMed] [Google Scholar]
- 39. Shulman LM, Manor Y, Handsher R, Delpeyroux F, McDonough MJ, et al. (2000) Molecular and antigenic characterization of a highly evolved derivative of the type 2 oral poliovaccine strain isolated from sewage in Israel. J Clin Microbiol 38: 3729–3734. [DOI] [PMC free article] [PubMed] [Google Scholar]