Abstract
Ameloblastomas are rare odontogenic epithelial tumors that occur mainly in the mandible. Despite their benign histologic appearance, they are locally aggressive with a high recurrence rate. However, a metastasizing ameloblastoma has been rarely reported. According to the current World Health Organization classification system, the definitive diagnosis of metastasizing ameloblastoma can only be carried out in retrospect, after the event of metastasis. This case report describes a patient with metastatic pulmonary ameloblastoma, 17 years after the surgical excision of an odontogenic tumor, preoperatively misdiagnosed as primary squamous cell carcinoma.
Keywords: Lung neoplasms, Neoplasm metastasis, Ameloblastoma
CASE REPORT
A 50-year-old woman presenting with back pain was referred to our center with a 2.5-cm nodule in the right middle lung field on a chest X-ray. The patient had a past history of surgical excision of an odontogenic tumor at a local dental clinic 17 years previously. A chest computed tomography (CT) scan revealed a 2.6-cm lobulated, heterogeneous enhancing nodule and a 1.5-cm satellite nodule in the anterior segment of the right upper lobe (RUL) (Fig. 1). Therefore, we performed CT-guided percutaneous needle biopsy for the tissue diagnosis of the main nodule. The specimen showed a cohesive tumor island composed of squamoid cells, with central keratin pearl-like material. There was only one event of mitosis in the whole field (Fig. 2A), and the patient was diagnosed with squamous cell carcinoma. Bronchoscopy, brain magnetic resonance imaging, and positron emission tomography scanning were performed for further evaluation and staging, based on the impression of primary lung cancer. Then, we performed a planned RUL lobectomy and mediastinal lymph node dissection through thoracotomy upon the diagnosis of clinical stage IA (T1bN0) or IIB (T3N0) lung cancer. The resected specimen showed two separate nodular lesions that shared the same histopathological features. However, the histopathological diagnosis after the operation was different from that of preoperative biopsy. Postoperative histopathological examination revealed densely packed tumor islands. These tumor islands showed peripheral palisading and loosely arranged central cells, which resembled stellate reticulum. The peripheral palisading cells were columnar and hyperchromatic. Little mitotic activity and cellular pleomorphism were observed (Fig. 2B). The overall features suggested a follicular pattern of ameloblastoma. We contacted the patient's former dentist and requested her medical records, but we could not obtain any information related to the odontogenic tumor. Finally, the diagnosis of metastasizing ameloblastoma was made based on the patient's past history and histopathological studies. The postoperative course was uneventful. Although the patient had no associated symptoms, panoramic radiography and facial CT were performed after consulting a dentist to identify local recurrence at the oral cavity. There was fibrotic scar formation but no evidence of recurrence at previous odontogenic tumor site. No adjuvant therapy was performed. The patient was doing well without any evidence of recurrence or metastasis during regular follow-up.
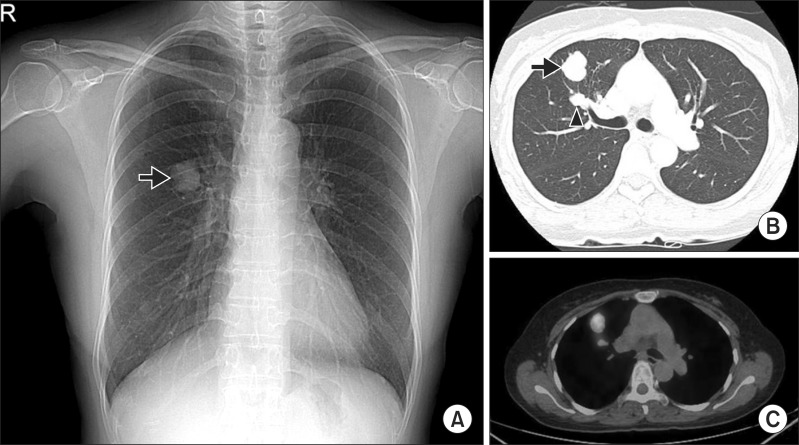
Fig. 1.
A chest X-ray shows a nodule (arrow) in the right middle lung field (A). A preoperative chest computed tomography scan shows main (arrow) and satellite (arrowhead) nodules in the anterior segment of the right upper lobe (B). Further, a positron emission tomography scan shows increased uptake in these nodular lesions (C).
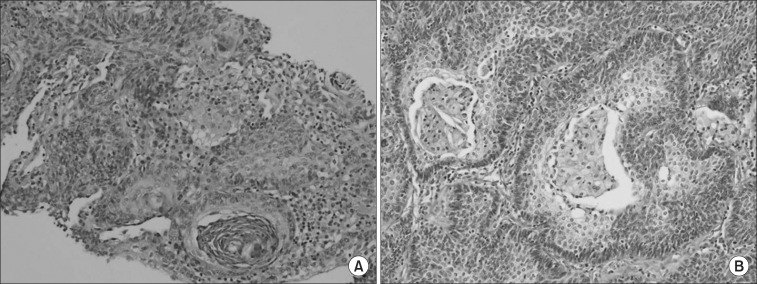
Fig. 2.
Pathological findings. (A) A needle biopsy specimen showing a tumor island composed of squamoid cells (H&E, ×100). (B) A postoperative histologic specimen showing metastasizing ameloblastoma (H&E, ×200).
DISCUSSION
Ameloblastomas are rare odontogenic epithelial tumors and account for 1% of all tumors and cysts of the jaws [1]. Ameloblastomas usually occur in the mandible and less often in the maxilla. They are classified as benign and characterized by slow growth, local invasiveness, and a high rate of recurrence. In contrast with its high recurrence rate (up to 50% to 72%), the metastasizing ameloblastoma (MA) is uncommon [2]. The incidence of malignancy/metastasis in relation to ameloblastoma has been reported to be only 2% [3]. To our knowledge, this is the first report of a patient who was diagnosed with metastasizing pulmonary ameloblastoma in South Korea.
The odontogenic tumors are classified according to the current World Health Organization histological classification published in 2005 [4]. MA is defined as an ameloblastoma that metastasizes despite a benign histological appearance and shows no specific features different from those of ameloblastomas that do not metastasize. Thus, the diagnosis of metastasizing ameloblastoma can only be made in retrospect, after the event of metastasis. Ameloblastic carcinoma is defined as a rare odontogenic malignancy that combines the histological features of ameloblastoma with cytological atypia, even in the absence of metastases.
MAs mostly occur in the lungs, although there are some reports of MA arising in the regional lymph nodes, bones, liver, and brain [5]. Van Dam et al. [6] reported a summary of clinical findings of MAs after reviewing 27 previously published reports and 3 of their cases. The distribution between males and females is nearly equal. There are 74% of primary tumors with purely plexiform, follicular, or mixed patterns. The lungs (78%) are the most common site of metastasis, of which 71% are bilateral. The average interval from the diagnosis of a primary tumor to the diagnosis of metastasis is 18 years, with a range of 3 to 45 years.
Because of the rare occurrence of MAs, the clinical course and the appropriate treatment are not yet well established. In most of the reported cases, MAs seem to have an indolent yet persistent behavior. Close observation, surgical resection, and chemo/radiotherapy can be considered treatment options. Scannell et al. [7] also suggested radiofrequency ablation as a possible treatment option for MAs. However, most authors recommend a complete surgical resection as the treatment of choice, particularly in the cases of operable pulmonary lesions. Chemo/radiotherapy can be reserved to relieve symptoms and to offer palliative care for inoperable lesions [8]. Of course, meticulous follow-up for recurrence after adequate resection of primary tumors should take precedence.
In summary, we have reported the case of a patient with metastatic pulmonary ameloblastoma. The diagnosis was made on the basis of the patient's past history of surgical excision for an odontogenic tumor and the histopathological features of ameloblastoma.
Footnotes
No potential conflict of interest relevant to this article has been reported.
References
- 1.Papaioannou M, Manika K, Tsaoussis B, Cheva A, Sichletidis L, Kioumis J. Ameloblastoma of the mandible with pulmonary metastases 45 years after initial diagnosis. Respirology. 2009;14:1208–1211. doi: 10.1111/j.1440-1843.2009.01613.x. [DOI] [PubMed] [Google Scholar]
- 2.Henderson JM, Sonnet JR, Schlesinger C, Ord RA. Pulmonary metastasis of ameloblastoma: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:170–176. doi: 10.1016/s1079-2104(99)70113-7. [DOI] [PubMed] [Google Scholar]
- 3.Dissanayake RK, Jayasooriya PR, Siriwardena DJ, Tilakaratne WM. Review of metastasizing (malignant) ameloblastoma (METAM): pattern of metastasis and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:734–741. doi: 10.1016/j.tripleo.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 4.Sciubba JJ, Eversole LR, Slootweg PJ. Odontogenic/ameloblastic carcinomas. In: Barnes L, Eveson JW, Reichart P, Sidransky D, editors. Pathology and genetics: head and neck tumors. Lyon: IARC Press; 2005. pp. 289–291. [Google Scholar]
- 5.Eliasson AH, Moser RJ, 3rd, Tenholder MF. Diagnosis and treatment of metastatic ameloblastoma. South Med J. 1989;82:1165–1168. doi: 10.1097/00007611-198909000-00027. [DOI] [PubMed] [Google Scholar]
- 6.Van Dam SD, Unni KK, Keller EE. Metastasizing (malignant) ameloblastoma: review of a unique histopathologic entity and report of Mayo Clinic experience. J Oral Maxillofac Surg. 2010;68:2962–2974. doi: 10.1016/j.joms.2010.05.084. [DOI] [PubMed] [Google Scholar]
- 7.Scannell J, Lees B, Hopper C. Can radiofrequency ablation be used as a treatment modality for the management of pulmonary Metastatic ameloblastoma? Radiol Case Rep. 2009;4:249. doi: 10.2484/rcr.v4i2.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luo DY, Feng CJ, Guo JB. Pulmonary metastases from an Ameloblastoma: case report and review of the literature. J Craniomaxillofac Surg. 2012;40:e470–e474. doi: 10.1016/j.jcms.2012.03.006. [DOI] [PubMed] [Google Scholar]