Abstract
Objective
The purpose of the study was to examine the relationship between self-reported sleep quality and sleep hygiene in Italian and American adolescents and to assess whether sleep-hygiene practices mediate the relationship between culture and sleep quality.
Methods
Two nonprobability samples were collected from public schools in Rome, Italy, and Hattiesburg, Mississippi. Students completed the following self-report measures: Adolescent Sleep-Wake Scale, Adolescent Sleep Hygiene Scale, Pubertal Developmental Scale, and Morningness/Eveningness Scale.
Results
The final sample included 776 Italian and 572 American adolescents 12 to 17 years old. Italian adolescents reported much better sleep hygiene and substantially better sleep quality than American adolescents. A moderate-to-strong linear relationship was found between sleep hygiene and sleep quality in both samples. Separate hierarchical multiple regression analyses were performed on both samples. Demographic and individual characteristics explained a significant proportion of the variance in sleep quality (Italians: 18%; Americans: 25%), and the addition of sleep-hygiene domains explained significantly more variance in sleep quality (Italians: 17%; Americans: 16%). A final hierarchical multiple regression analysis with both samples combined showed that culture (Italy versus United States) only explained 0.8% of the variance in sleep quality after controlling for sleep hygiene and all other variables.
Conclusions
Cross-cultural differences in sleep quality, for the most part, were due to differences in sleep-hygiene practices. Sleep hygiene is an important predictor of sleep quality in Italian and American adolescents, thus supporting the implementation and evaluation of educational programs on good sleep-hygiene practices.
Keywords: Pediatrics, adolescence, sleep quality, sleep hygiene, cultural differences
Adolescence is a period characterized by important changes in cognitive, behavioral, social, and emotional functioning attributable to biological development (ie, puberty) and to new roles and demands in the familial and social milieu (eg, decreased parental involvement, increased academic requirements). There also are dramatic changes in sleep/wake patterns during adolescence, including a decrease in sleep duration,1–3 a delay in the timing of sleep,4,5 and an increasingly large discrepancy between weekday and weekend sleep patterns.6–9 Sleep quality is reduced as well.10 Community- and school-based studies conducted in Europe, Asia, and the United States suggest that between 6% and 37% of adolescents report difficulties on ≥1 of the following behavioral dimensions of sleep quality: going to bed,11,12 falling asleep,3,13–17 maintaining undisturbed sleep,10,16–18 reinitiating sleep after nocturnal awakenings,3,16,17 and returning to wakefulness in the morning.7,9,15,17 Furthermore, up to 16% of adolescents are considered to have clinically significant insomnia.16,19,20
There is ample evidence that inadequate sleep quantity and quality are linked to significant problems in several aspects of teenagers’ lives.5,8 Sleepiness may be a widespread problem in the school setting, where both suboptimal sleep duration and sleep disturbance are associated with reduced academic functioning, including attentional difficulties and increased absences.21,22 Substance use is greater among teenagers with sleep difficulties.13,23 On the highway, >50% of fall-asleep driving accidents are caused by people <25 years old.24 Importantly, disturbed sleep quality is associated with deficits in concurrently measured psychologic, behavioral, and somatic functioning and predicts the emergence of deficits in interpersonal and psychosocial functioning.3,10,23,25 Although causal relationships have not been firmly established, these findings raise the possibility that adolescent academic, emotional, health, and behavioral problems may be prevented or meaningfully improved by interventions that result in increased quantity and quality of sleep.26
Insufficient and irregular teenage sleep have been the focus of a number of investigations, and important biological and social influences have been identified.5,12,15,27,28 Disturbed sleep quality is likely attributable to many of the same factors. Models used in the investigation of sleep quality during early childhood view sleep as occurring within the context of both internal factors (biological, maturational, health related, psychosocial) and external factors (familial, environmental, cultural), which directly or indirectly influence how well children sleep.29,30 These models emphasize the role of caretakers in ensuring that children have a regular sleep/wake schedule, a suitable sleep environment, and a bedtime routine that prepares them physiologically, behaviorally, and emotionally for sleep. These practices, commonly referred to as sleep hygiene, are considered to mediate or moderate the influence of the contextual variables. Models such as these also may be applied to the study of adolescent sleep. During this developmental period, however, there are changes in important contextual variables (eg, pubertal status, school start time, social activities, parental involvement, and employment).12 Because these changes are believed to increase adolescents’ vulnerability to sleep difficulties, good sleep hygiene may be especially important.
This study investigated the relationship between sleep-hygiene practices and reported sleep quality in Italian and American adolescents. Sleep hygiene for adolescents can be defined as behavioral practices that promote good sleep quality, adequate sleep duration, and full daytime alertness.31 These practices include avoiding late-afternoon naps and alcohol, tobacco, and caffeine before bedtime; following a bedtime routine; avoiding bedtime activities that are physiologically, cognitively, and emotionally activating; sleeping alone; not using the bed for activities other than sleep; sleeping in a comfortable, quiet, toxin-free environment; and maintaining a stable sleep schedule.31,32 Although there is a general appreciation of the importance of sleep-hygiene practices for good sleep quality,32 very few studies have examined this relationship in adolescents, and these studies have assessed only selected aspects of sleep hygiene (eg, substance use, cognitive activation).11,13,14,17,25 A better understanding of this relationship would support further development of programs to educate adolescents about good sleep habits.
Sleep hygiene within the context of culture (Italian versus American) was also investigated in the current study. Existing cross-cultural examinations of adolescent sleep are scarce,33 and there is only a modest collection of international studies on sleep quality during this developmental period.3,13–17 Using these reports to make cross-cultural comparisons has been difficult because of differences in operational definitions of sleep-related variables, sample sizes, measures, and administration procedures. Cultural comparisons are of intrinsic value, because they permit evaluation of the benefits and consequences of cultural practices. Furthermore, explaining cultural differences is one way to increase understanding of adolescent sleep quality. In this regard, it is hypothesized that sleep hygiene will be identified as a mediator of sleep-quality differences between Italian and American adolescents.
METHODS
Participants
Data were collected from public school systems in Rome, Italy, and Hattiesburg, Mississippi. In Italy, a nonprobability sample of 5 schools was selected in the urban area of Rome. These school districts were chosen because of the heterogeneous population in terms of socioeconomic status (SES). Italian researchers recruited 932 families at a meeting organized by the public school system and asked caretakers to sign an institutional review board–approved consent form on site (response rate: 83%). A nonprobability sampling strategy was also used in the United States, with the superintendent providing permission to collect data at all 3 public middle and high schools in Hattiesburg, Mississippi, a small city in the southern region of the state. Within each school, specific academic classes were chosen to maximize representation of students in each grade. American researchers informed 979 students about the study in individual classes. These students were asked to take the institutional review board–approved consent form home, have it signed by their caretaker, and return it to their teacher (response rate: 58%).
Measures
Students anonymously completed a set of pencil-and-paper questionnaires (presented in the same order across samples) in the morning (8:00 am to 12:30 pm) during October and November 2002. In both countries, project field staff administered and monitored the completion of questionnaires. Italian researchers used forward-backward translation procedures to create Italian versions of study measures. Because educational categories differ across Europe and America, SES was determined by scoring the head of household's occupation on a scale of 1 (unskilled) to 9 (professional).34
Adolescent Sleep-Wake Scale
The Adolescent Sleep-Wake Scale (ASWS; see Appendix 1) is based on and includes items similar in content to those on the Children’s Sleep-Wake Scale.35,36 The ASWS is a 28-item self-report pencil-and-paper research instrument that assesses sleep quality in 12- to 18-year-old adolescents. Respondents are asked to indicate how often sleep behaviors have occurred during the past month using a 6-point scale (“always,” “frequently-if not always,” “quite often,” “sometimes,” “once in a while,” and “never”). Adolescents’ sleep is measured along 5 behavioral dimensions including going to bed (5 items), falling asleep (6 items), maintaining sleep (6 items), reinitiating sleep (6 items), and returning to wakefulness (5 items). Mean subscale scores for each dimension and a full-scale sleep-quality score (ASWS total; mean of 5 subscales) can be obtained. Scores range from 1 to 6, with higher scores indicating better sleep quality. In this study, internal consistency (Chron-bach's α) for the ASWS subscales was remarkably similar across adolescent samples (Italians: α = .60 to .81; Americans: α = .64 to .82). The full scale (ASWS total) showed good reliability (Italians: α = .80; Americans: α = .86).
Adolescent Sleep Hygiene Scale
The Adolescent Sleep Hygiene Scale (ASHS) (see Appendix 2) was modified from the Children’s Sleep Hygiene Scale.37 The ASHS is a 28-item self-report pencil-and-paper measure that assesses sleep-facilitating and sleep-inhibiting practices in 12- to 18-year-old adolescents along 9 different conceptual domains: physiological (5 items), cognitive (6 items), emotional (3 items), sleep environment (4 items), daytime sleep (1 item), substances (2 items), bedtime routine (1 item), sleep stability (4 items), and bed/bedroom sharing (2 items). Students report how often sleep-related behaviors have occurred during the past months along a 6-point scale (“always,” “frequently-if not always,” “quite often,” “sometimes,” “once in a while,” and “never”). Mean domain scores and an overall sleep-hygiene score (ASHS total; mean of 9 domain scores) are available. All scores range from 1 to 6, and higher scores are indicative of better sleep hygiene. In this study, internal consistency was similar for the American and Italian samples, with the exception of the sleep-environment domain (Italian: α = .37; American: α = .52). Among all adolescents (both samples combined), Chronbach's α ranged from .46 to .74 for the sleep-hygiene domains and was .80 for the full scale (ASHS total).
Pubertal Development Scale
The Pubertal Development Scale (PDS) is an 8-item pencil-and-paper assessment of physical maturation and pubertal status in young humans.38 Measured characteristics include growth in height and body hair, skin changes, voice changes and facial hair growth (boys only), and breast development and menarche (girls only). PDS scores range from 1 (prepubertal) to 4 (full maturation). Previous reports on the self-report version of the PDS have found Chronbach's coefficient α ranging from .67 to .70.38
Morningness/Eveningness Scale
The Morningness/Eveningness (M/E) Scale is a self-report measure of circadian preference in older children and adolescents.4,39 Ten items inquiring about preferred timing of activities (eg, school, taking tests, bedtime, rise time) are scored on a 4- or 5-point scale, with scores ranging from 10 (extreme evening) to 42 (extreme morning). Previous studies have reported reliability for the M/E Scale (Italians: α = .7740; Americans: α = .734,39) and significant associations between M/E Scale scores and bedtimes and rise times (r = 0.25–0.52).4
Data Analysis
All analyses were performed with Statistical Package for the Social Sciences (SPSS Inc, Chicago, IL) version 11.0. Where appropriate, summary measures were presented as means and standard deviations (SDs). Comparisons involving continuous variables were performed by using t tests; however, when distributional assumptions were not met, comparisons were made with a Mann-Whitney U test. Categorical data were analyzed by using a Χ2 test. Pearson correlation for continuous variables and Spearman correlation for ordinal variables were computed to assess the association between ASHS and ASWS variables. Hierarchical multiple regressions were performed to assess the relationships between sleep quality (ASWS total) and ASHS domains, demographic characteristics, pubertal status, circadian preference, and geographic location. The significance level for the described comparisons was set at .05. In the case of multiple comparisons, however, the α level was divided by the number of comparisons (Bonferroni test) to control for an inflated type I error rate.41 Missing values were infrequent (<3% for any variable). Items missing on the ASWS, ASHS, and M/E scales were replaced with means of the remaining cases from respective data-collection locations (Italy and the United States), and PDS missing values were replaced with means from existing participants of the same age, gender, and geographic location (Italy and the United States). Effect size in SD units was computed for ASHS and ASWS mean (M) comparisons (d = M sample 1 – Msample 2/SDpooled).42 As reviewed by Cohen,43 an effect size of .25 is considered small, .50 is considered medium, and ≥.75 is considered large.
RESULTS
Participants
The final sample included 776 Italian and 572 American adolescents (N = 1348; 655 male and 693 female) 12 to 17 years old (mean: 14.6 years; SD: 1.6). At each age, there were at least 170 adolescents. As shown in Table 1, samples did not differ significantly in mean age, pubertal status (PDS scores), or circa-dian preference (M/E Scale scores). The Italian sample included a higher proportion of males. There were significant racial differences across geographic locations: 78.3% of American adolescents but >1% of Italian adolescents were black. SES was significantly lower among Italian than among American adolescents. American participants were more likely to take medications affecting sleep and/or wakefulness (eg, antidepressants, antihistamines, stimulants) and reported a higher prevalence of medical illnesses/disabilities (eg, asthma, attention-deficit/hyperactivity disorder, diabetes) than did Italian adolescents.
TABLE 1.
Sample Characteristics for Italian and American Adolescents (N = 1348)
| Italian (n = 776) | American (n = 572) | Statistics | |
|---|---|---|---|
| Age, mean (SD) | 14.6 (1.6) | 14.6 (1.6) | NS |
| Gender, % male | 55.4 | 41.2 | Χ2 = 29.1, P < .001 |
| Race, % white | 99.6 | 21.7 | Χ2 = 887.2, P < .001 |
| SES*, mean (SD) | 4.5 (1.4) | 5.1 (0.6) | t = 6.3, P < .001 |
| Medications, % | 5.5 | 18.2 | Χ2 = 58.9, P < .001 |
| Illnesses/disabilities, % | 8.6 | 16.8 | Χ2 = 20.5, P < .001 |
| Pubertal status, mean (SD) | 3.1 (.6) | 3.2(.6) | NS |
| Circadian preference, mean (SD) | 26.3 (4.1) | 26.0 (4.4) | NS |
NS indicates not significant.
Occupational scoring for head of household.
Group Differences in Sleep Quality and Sleep Hygiene
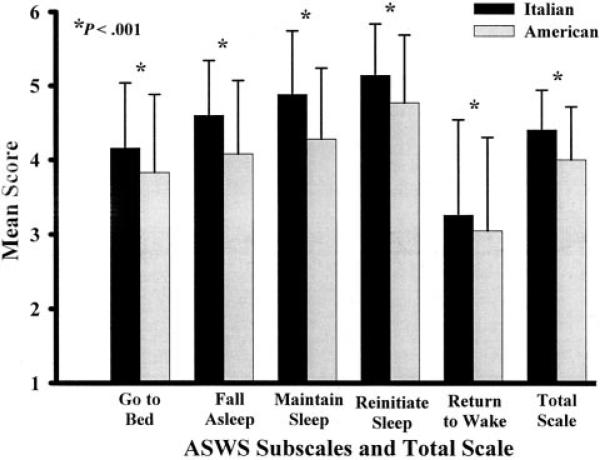
Italian adolescents reported substantially higher scores on every behavioral dimension of the ASWS than did American adolescents (see Fig 1): going to bed (t = −6.16, P < .001; d = 0.37); falling asleep (t = −10.64, P < .001; d = 0.62), maintaining sleep (t = −11.92, P < .001; d = 0.67), reinitiating sleep (t = −8.05, P − .001; d = 0.46), and returning to wakefulness (t = −3.00, P < .001; d = 0.16). Overall sleep quality, as measured by ASWS total, was significantly better among adolescents in the Italian than in the American sample (t = −11.39, P < .001; d = 0.66). Italian/American group differences accounted for 9.5% of the variance in the ASWS total score.
Fig 1.
ASWS subscale and total mean differences with SD bars for Italian (n = 776) and American (n = 572) adolescents.
Examination of mean ASHS domain scores (see Table 2) showed that Italian adolescents reported significantly better sleep hygiene, with higher scores on the physiological, cognitive, emotional, sleep-environment, daytime-sleep, and sleep-stability domains. Mann-Whitney U tests showed that American adolescents had higher scores only on the substance-use and bed/bedroom-sharing domains. No group differences were found on the bedtime-routine domain. The mean ASHS total difference favored the Italian adolescents by close to 0.75 SD.
TABLE 2.
ASHS Domain and Total Scale Scores for Italian (n = 776) and American (n = 572) Samples
| ASHS Domains | Italian | American | Statistics |
|---|---|---|---|
| Physiological | 4.7 (.86) | 3.9 (.92) | t = −17.4, P < .001, d = 0.96 |
| Cognitive | 4.0 (.90) | 3.3 (.96) | t = −13.5, P < .001, d = 0.70 |
| Emotional | 4.7 (.99) | 4.2 (1.10) | t = −8.9, P < .001, d = 0.50 |
| Sleep environment | 5.0 (.79) | 4.5 (1.00) | t = −10.4, P < .001, d = 0.57 |
| Daytime sleep | 5.1 (1.31) | 3.9 (1.75) | t = −14.3, P < .001, d = 0.77 |
| Substances | 5.4 (1.09) | 23.3 (.67) | z = −9.3, P < .001 |
| Bedtime routine | 4.1 (1.85) | 3.9 (1.83) | NS |
| Sleep stability | 3.8 (1.09) | 3.3 (1.10) | t = −8.8, P < .001, d = 0.48 |
| Bed/bedroom sharing | 4.5 (1.88) | 5.1 (1.30) | z = −4.3, P < .001 |
| ASHS total | 4.5 (.57) | 4.0 (.61) | t = −13.03, P < .001, d = 0.70 |
NS indicates not significant.
Relationship Between Sleep Quality and Sleep Hygiene
The data presented in Table 3 illustrate that each of the behavioral dimensions of sleep quality were related to ≥1 of the sleep-hygiene domains for both Italian and American adolescents. It is evident that the consistency and strength of these relationships differed not only across sleep-quality dimensions but also across samples. Among both Italians and Americans, high scores on all ASWS subscales were related to avoidance of cognitively arousing activities (high scores on the cognitive domain). Notably, all the larger correlation coefficients (r > 0.30) involved cognitive or emotional activation (cognitive or emotional domains). Furthermore, the majority of the sleep-hygiene domains (eg, physiologic, emotional, substance use) were selectively related to sleep-quality subscales. Adolescents reporting more frequent daytime napping (daytime-sleep domain), for example, reported more difficulties with waking in the morning (returning-to-wakefulness subscale). Less success in maintaining and reinitiating sleep was associated with sharing a bed or bedroom but only for adolescents in the American sample. None of the sleep-quality subscales were related to the bedtime-routine domain.
TABLE 3.
Correlation Coefficients for ASHS Domains and ASWS Subscales for Italian (n = 776) and American (n = 572) Samples
| ASWS Subscales | ASHS Domains |
|||||||
|---|---|---|---|---|---|---|---|---|
| Physiological* | Cognitive* | Emotional* | Sleep Environment* | Daytime Sleep† | Substances† | Sleep Stability* | Bed/Bedroom Sharing† | |
| Going to bed | ||||||||
| Italian | 0.20 | 0.25 | — | 0.17 | — | 0.17 | 0.18 | — |
| American | 0.16 | 0.23 | — | 0.17 | — | — | 0.24 | — |
| Falling asleep | ||||||||
| Italian | — | 0.20 | 0.25 | — | — | — | — | — |
| American | 0.17 | 0.30 | 0.27 | 0.26 | — | — | 0.18 | — |
| Maintaining sleep | ||||||||
| Italian | 0.25 | 0.31 | 0.40 | 0.17 | — | — | — | — |
| American | 0.21 | 0.31 | 0.35 | 0.24 | — | — | 0.18 | 0.20 |
| Reinitiating sleep | ||||||||
| Italian | 0.16 | 0.17 | 0.28 | — | — | — | — | — |
| American | 0.24 | 0.30 | 0.33 | 0.28 | — | — | — | 0.26 |
| Returning to wake | ||||||||
| Italian | — | 0.17 | 0.19 | — | 0.17 | — | 0.16 | — |
| American | — | 0.23 | 0.29 | — | 0.17 | — | 0.27 | — |
Note: 2-tailed tests of significance (P < .001) for all reported correlation coefficients; — indicates that the correlation coefficient was r < 0.15.
Pearson correlation coefficient.
Spearman correlation coefficient.
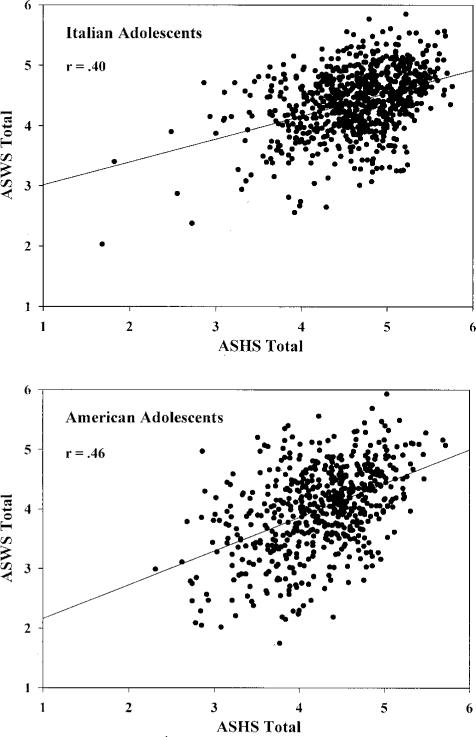
Figure 2 presents scatter plots showing moderate-to-strong linear relationships between sleep hygiene (ASHS total) and sleep quality (ASWS total) across both samples (Italians: r = 0.40, P < .001; Americans: r = 0.46, P < .001).
Fig 2.
Scatter plots of the relationship between the ASHS and ASWS total scores for Italian (n = 776) and American (n = 572) adolescents.
To test whether sleep hygiene accounted for unique variance in overall sleep quality after the removal of the effects of control variables that were potentially related to both measures, separate hierarchical multiple regression analyses were performed on the Italian and American samples. Each regression took the same form, with demographic characteristics (age, gender, SES, race [Americans only]) along with medication/illness status, pubertal status (PDS scores), and circadian preference (M/E Scale scores) entered in the first step and sleep hygiene (individual ASHS domain scores) added in the second step.
The results of these regressions are presented in Table 4. For both samples, control variables entered in step 1 explained a significant proportion of the variance (18% and 25% in the Italian and American samples, respectively) in sleep quality, with circa-dian preference accounting for the highest percentage of unique variance in ASWS total scores. High scores on the M/E scale (morningness) were associated with better overall sleep quality than low scores (eveningness). Addition of ASHS domain scores in the second step explained significantly more variance in ASWS total scores (17% for Italians; 16% for Americans). Among Italian adolescents, inspection of the squared semipartial correlations (sp2) revealed significant unique variance related to the cognitive and emotional sleep-hygiene domains. Among American adolescents, however, the cognitive, emotional, sleep-environment, and bed/bedroom-sharing domains accounted for significant unique variance in ASWS total scores. In all cases, high domain scores (good sleep hygiene) were associated with good sleep quality.
TABLE 4.
Hierarchical Regressions of Control Variables and ASHS Domain Scores on ASWS Total Scores for Italian (n = 776) and American (n = 572) Samples
| Sleep Quality (ASWS
Total) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Italian |
American |
|||||||
| R2 Change | F Value | β | sp2 | R2 Change | F Value | β | sp2 | |
| Step 1 | ||||||||
| Age | .00 | 0.000 | .07 | 0.004 | ||||
| Gender | −.09 | 0.006 | −.10 | 0.006 | ||||
| Race* | — | — | .00 | 0.000 | ||||
| SES | .10 | 0.008 | .06 | 0.003 | ||||
| Medication status | .10 | 0.008 | .00 | 0.000 | ||||
| Illness status | .04 | 0.002 | .05 | 0.003 | ||||
| Pubertal status | .00 | 0.000 | .09 | 0.005 | ||||
| Circadian preference | .39 | 0.144† | .47 | 0.220† | ||||
| R2 change | .18† | 24.09 | .25† | 23.13 | ||||
| Step 2 (ASHS domains) | ||||||||
| Physiological | .08 | 0.005 | -.02 | 0.000 | ||||
| Cognitive | .14 | 0.010† | .21 | 0.026† | ||||
| Emotional | .27 | 0.050† | .17 | 0.020† | ||||
| Sleep environment | .06 | 0.003 | .12 | 0.010† | ||||
| Daytime sleep | .02 | 0.000 | -.05 | 0.003 | ||||
| Substances | .00 | 0.000 | .04 | 0.002 | ||||
| Bedtime routine | .03 | 0.001 | .06 | 0.000 | ||||
| Sleep stability | .06 | 0.004 | .08 | 0.000 | ||||
| Bed/bedroom sharing | -.01 | 0.000 | .11 | 0.010† | ||||
| R2 change | .17† | 21.52 | .16† | 16.12 | ||||
| R2 total (adjusted) | .35† | .41† | ||||||
sp2 indicates squared semipartial correlation coefficient.
Race was not included in step 1 for the Italian sample because of a high proportion of white participants (99.6%).
Two-tailed tests of significance: P < .001.
Variables Mediating the Relationship Between Culture and Sleep Quality
Multiple hierarchical regression analyses were used to assess the extent to which control variables and sleep hygiene mediated the relationship between culture (Italian versus American) and sleep quality (ASWS total). The first analysis assessed mediation by control variables only. In the analysis, characteristics differentiating the Italian and American samples (see Table 1) were entered into step 1, and culture was added in step 2. Race was not included in this grouping of variables, because very few black adolescents were included in the Italian sample (0.4%, see Table 1). Race did not account for a significant amount of variance in the American sample (see Table 2). Examination of the sp2 coefficients in the first step of the hierarchical regression revealed that gender (sp2 = 0.019, with males having better sleep quality), medication status (sp2 = 0.008), and illness/disabilities (sp2 = 0.005) accounted for a significant proportion of the variance in the total sleep quality of both samples combined. Overall, the control variables accounted for 4.5% of the total variance in sleep quality (ASWS total: F[4, 1322] = 15.74, P < .001). In step 2, culture accounted for an additional 7.2% of the variance in sleep quality (F[1, 1321] = 108.00, P < .001).
A second hierarchical regression assessed the mediational role of sleep hygiene. Control variables were again entered in the first step, ASHS domains differentiating samples (see Table 4) were entered in the second step, and culture was added in the third step. In this analysis, the sleep-hygiene domains accounted for an additional 27.3% of the variance in total sleep quality (F[8, 1308] = 65.30, P < .001). The significant sleep-hygiene domains in step 2 were cognitive (sp2 = 0.026), emotional (sp2 = 0.058), environmental (sp2 = 0.012), and sleep stability (sp2 = 0.023). Inclusion of culture in step 3 accounted for only an additional 0.8% of the variance in ASWS total (F[1, 1307] = 15.54, P < .001).
DISCUSSION
Italian adolescents practiced markedly better sleep hygiene and reported substantially better sleep quality than American adolescents. Across cultures, reported practice of sleep hygiene (ASHS total) was moderately to strongly related to sleep quality (ASWS total), and these relationships were not attributable to any of the measured demographic and individual difference variables. Furthermore, differences in overall sleep quality between the Italian and American samples were, for the most part, due to differences in sleep-hygiene practices.
Good sleep quality can be viewed as the seamless integration of sleep into a sleep/wake oscillatory pattern that meets sleep-related needs. In this study, an adolescent with good sleep quality was defined as one who goes to bed easily at bedtime, transitions effortlessly from wakefulness to sleep, maintains undisturbed sleep, reinitiates sleep after nocturnal arousals and awakenings, and transitions easily from sleep to wakefulness in the morning. The sleep-quality measure used in the present analysis, the ASWS, is an early-stage effort to assess different behavioral dimensions of sleep quality based on a model that places sleep within the context of intrinsic and extrinsic variables. The findings of this study support this multidimensional model in that examination of the 5 sleep-quality subscales (ASWS) revealed differing relationships with 8 of the 9 individual domains of sleep hygiene (ASHS). For example, in both samples, less success in going to bed (delaying bedtime) was more common among teens engaging in physiologically, cognitively, and emotionally activating behaviors. In comparison, adolescents with poorer success in returning to wakefulness in the morning were less likely to have stable sleep schedules and more likely to take daytime naps and engage in cognitively and emotionally activating bedtime behaviors. Finding differing patterns of relationships supports the notion that it is important for researchers to assess multiple behavioral dimensions of sleep quality.
This study extends other investigations of adolescent sleep-hygiene practices by providing a comprehensive estimate of the ability of sleep hygiene to predict sleep quality. Whereas previous reports of this relationship have used measures of select elements of sleep hygiene (eg, substance use,13,33,44 cognitive and emotional activation13), our study administered a new measure that more fully assesses the acknowledged sleep-hygiene domain of content.32 Furthermore, although it is difficult to identify and measure all relevant control variables, an effort was made to account for demographic and individual difference variables of known relation to both sleep hygiene and sleep quality.12 Among individual difference variables, circadian preference accounted for the highest percentage of variance in both samples. This finding is consistent with those of other studies showing that evening preference is associated with poor sleep quality as well as with poor sleep-hygiene practices (eg, sleep/wake irregularity, frequent use of psychoactive substances), insufficient sleep duration, and daytime sleepiness.12,17,45–47 After controlling for demographic and individual difference variables, sleep hygiene still accounted for a substantial proportion of the variance in sleep quality (16% among Americans and 17% among Italians).
Among both Italian and American adolescents, the emotional and cognitive domains of the ASHS were the strongest unique predictors of overall sleep quality. Other authors also found increased sleep problems among adolescents who worry, feel sad, or engage in cognitively stimulating activities just before bedtime.13,17,33 This is of particular importance, given existing data that support the role of psychological instability in sleep difficulties during this developmental period.10,13,16,17
These results also suggest culturally related disparities in the prediction of overall sleep quality. Among American but not Italian adolescents, sleeping in a quiet, dark, comfortable environment and not sharing a bed/bedroom were associated with better sleep quality. It is unclear why environmental factors would only be important in the American sample, especially because adolescents in the Italian sample were from a large urban city, which is assumed to produce a noisier sleep environment. Furthermore, the absence of a relationship between sharing a bed/bedroom and sleep quality in the Italian sample may have been due to the heterogeneity of the scale items (see Appendix 2). Although we are not aware of any reports on bed/bedroom sharing during adolescence, 1 recent Italian study found a 3.5% prevalence of cosleeping among 10- to 11-year-old children living in Rome.48 The current sample of Italian adolescents may have been more likely to share bedrooms but not beds with another individual. Furthermore, given that avoidance of sharing a bed but not a bedroom is commonly reported in studies of sleep-hygiene practices for young children,49,50 these items should be revised to specifically tap sleeping with another individual.
In general, Italian adolescents reported much better sleep-hygiene practices than did Americans, with the largest differences occurring in the physiological and daytime-sleep domains. Existing reports show that napping increases during adolescence,51 and this trend may occur in some cultural groups more than in others.52 These differences may also be explained by variability in the sociocultural context, which implies different styles of living. In Italy, better sleep-hygiene practices may be due to maintenance of parental involvement into early adolescence. For example, a previous study on sleep habits and problems with a representative sample of 6632 Italian high school students found that irregular sleep schedules, frequent napping, insufficient sleep duration, and daytime sleepiness were significantly more likely to occur among older (16- to 19-year-old) adolescents than among younger (14- to 15-year-old) ones.40 Although this study did not assess parental involvement across the 2 age groups directly, the results do suggest that incorporating parent-related measures (eg, attitudes about sleep, levels of parental monitoring) may advance our understanding of factors influencing sleep-hygiene practices of adolescents.
Although international differences in sleep patterns and difficulties falling asleep were found in a recent study of 11- to 16-year-olds from 11 European countries,13,33 our study is, to our knowledge, the first cross-cultural investigation of adolescent sleep hygiene and sleep quality conducted during the same period with identical measures and administration procedures. These findings demonstrate remarkable cultural differences in overall sleep quality (ASWS total) as well as in each of the behavioral dimensions of sleep quality (ASWS subscales). Finding group disparities (cultural or otherwise) when studying a behavior is especially important when these differences can be explained. In this regard, sleep-quality differences were related in part to varying sample demographics such as race, gender, and medication use. Of primary importance, however, was that culture accounted for <1% of the variance in adolescent sleep quality after we controlled for both demographic characteristics and sleep-hygiene domains. These findings demonstrate that sleep-hygiene practices may be an important mediating variable when group differences in sleep quality are explored. Thus, researchers may benefit from assessing sleep hygiene comprehensively in future investigations of gender, age, race, or circadian preference differences in sleep quality.
Clinically, our findings highlight the need to understand the sleep-related practices associated with sleep quality first and then to create educational and intervention programs that target modification of these specific behaviors. Recent studies have shown that adolescents have a general lack of knowledge about sleep and healthy sleep habits. For example, Grunstein demonstrated that knowledge of sleep and driving among 1378 Australian adolescents was very poor.47 Cortesi et al,53 in a pilot study of a sleep-education program with 425 Italian high school students, showed that students had low baseline levels of sleep knowledge and that those assigned to an education group, compared with controls, had higher sleep-knowledge scores post-intervention and 3 months after completion of the course. Studies on the effects of the Sleep Smart Program, a prevention-intervention curriculum that teaches healthy sleep-hygiene practices to seventh- and eighth-graders, found that students who received training had improved sleep-pattern regularity and increased school-night sleep duration.54,55 Furthermore, improved sleep hygiene may have other health-related benefits such as decreasing the frequency and duration of migraine attacks in children and adolescents.26
Several limitations of this study deserve mention. First, there is good reason to question the generaliz-ability of the present findings, because they are based on nonprobability samples. It is likely that there are important variations across groups of individuals residing in different regions of Italy and the United States, which supports the need for additional cross-cultural comparisons of sleep from multiple sites across different countries. Second, response rates in this study differed between groups (83% for Italians; 58% for Americans), and it is unknown whether respondents differed from nonrespondents on characteristics related to sleep quality and sleep hygiene (eg, SES, parental involvement). Third, all data were collected with self-report measures. Although it is desirable to use multiple methods of assessing sleep quality (actigraphy, polysomnography, sleep diaries, interviews), self-report questionnaires are the most time- and cost-efficient way to collect data on large samples. Furthermore, measurement of SES presents well-documented problems,56 which are likely compounded in cross-cultural studies as a result of different educational and economic systems. Although the SES measure used in this study included quantitative ratings of American occupations,34 these ratings may not have provided an adequately valid measure of SES for Italians. Finally, translation of measures must be considered when cross-cultural research is conducted. Although we used a common strategy (forward-backward translation), there is a chance that we failed to recognize subtle differences between cultures. Future cross-cultural sleep studies should consider reviewing measures in need of translation in a group of individuals who are fluent in both languages, knowledgeable about both cultures, and have expertise in sleep.57
CONCLUSIONS
Our findings suggest that sleep hygiene is importantly related to sleep quality during adolescence and support the implementation and evaluation of educational programs that emphasize good sleep habits. Investigating similarities and differences in sleep and sleep-related practices within and across countries may facilitate an understanding of factors that underlie sleep/wake regulation during adolescence. Furthermore, these results indicate that culture may influence sleep-hygiene practices and that these sleep-related behaviors may put adolescents from different cultures at risk for poor sleep quality.
ACKNOWLEDGMENTS
We thank the Italian Ministry of Italian Public Education and the Hattiesburg Public School System for allowing us access to students and for facilitating our data-collection efforts. We also acknowledge Sharon Hopkins, Erin Clarke, Teresa Sebastiani, Cristina Vagnoni, and Maurizio Fortunato for data collection, data entry, and statistical contributions.
ABBREVIATIONS
- SES
socioeconomic status
- ASWS
Adolescent Sleep-Wake Scale
- ASHS
Adolescent Sleep Hygiene Scale
- PDS
Pubertal Development Scale
- M/E
Morningness/Eveningness
APPENDIX
APPENDIX 1.
ASWS Subscales and Items
| Going to bed |
| When it's time to go to bed, I want to stay up and do other things (for example: watch television, play video games, talk on the phone). |
| I have trouble making myself go to bed at bedtime. |
| I am ready to go to bed at bedtime. |
| I enjoy bedtime. |
| I try to “put off” or delay going to bed. |
| Falling asleep |
| When it's time to go to sleep (lights-out), I have trouble settling down. |
| When it's time to go to sleep (lights-out), I feel sleepy. |
| When it's time to go to sleep (lights-out), I lie down but then get up and come out of the bedroom. |
| I have trouble going to sleep. |
| I need help getting to sleep (for example: I need to listen to music, watch television, take medication, or have someone else in the bed with me). |
| I fall asleep quickly. |
| Maintaining sleep |
| During the night, I toss and turn in my bed. |
| During the night, I am very restless. |
| During the night, I moan, groan, or talk in my sleep. |
| During the night, my legs kick or jerk. |
| During the night, I wake up more than once. |
| I sleep soundly through the night. |
| Reinitiating sleep |
| After waking up during the night, I have trouble going back to sleep. |
| After waking up during the night, I have trouble getting comfortable. |
| After waking up during the night, I wake up another family member. |
| After waking up during the night, I need help to go back to sleep (for example: I need to watch television, read, or sleep with another person). |
| After waking up during the night, I feel scared. |
| After waking up during the night, I roll over and go right back to sleep. |
| Returning to wakefulness |
| In the morning, I wake up and feel ready to get up for the day. |
| In the morning, I wake up feeling rested and alert. |
| In the morning, I wake up and just can't get going. |
| I need help waking up in the morning (for example: from an alarm clock or another person). |
| I have trouble getting out of the bed in the morning. |
APPENDIX 2.
ASHS Domains and Items
| Physiological |
| After 6:00 pm, I have drinks with caffeine (for example: cola, pop, root beer, iced tea, coffee). |
| During the 1 hour before bedtime, I am very active (for example: playing outside, running, wrestling). |
| During the 1 hour before bedtime, I drink >4 glasses of water (or some other liquid). |
| I go to bed with a stomachache. |
| I go to bed feeling hungry. |
| Cognitive |
| During the 1 hour before bedtime, I do things that make me feel very awake (for example: playing video games, watching television, talking on the telephone). |
| I go to bed and do things in my bed that keep me awake (for example: watching television, reading). |
| I go to bed and think about things I need to do. |
| I go to bed and replay the day's events over and over in my mind. |
| I use my bed for things other than sleep (for example: talking on the telephone, watching television, playing video games, doing homework). |
| I check my clock several times during the night. |
| Emotional |
| During the 1 hour before bedtime, things happen that make me feel strong emotions (sadness, anger, excitement). |
| I go to bed feeling upset. |
| I go to bed and worry about things happening at home or at school. |
| Sleep environment |
| I fall asleep while listening to loud music. |
| I fall asleep while watching television. |
| I fall asleep in a brightly lit room (for example, the overhead light is on). |
| I fall asleep in a room that feels too hot or too cold. |
| Daytime sleep |
| During the day I take a nap that lasts > 1 hour. |
| Substances |
| After 6:00 pm, I smoke or chew tobacco. |
| After 6:00 pm, I drink beer (or other drinks with alcohol). |
| Bedtime routine |
| I use a bedtime routine (for example, bathing, brushing teeth, reading). |
| Sleep stability |
| During the school week, I stay up >1 hour past my usual bedtime. |
| During the school week, I “sleep in” >1 hour past my usual wake time. |
| On weekends, I stay up >1 hour past my usual bedtime. |
| On weekends, I “sleep in” >1 hour past my usual wake time. |
| Bed/bedroom sharing |
| I sleep alone. |
| I sleep all or part of the night with someone else (for example, with your parent[s], sister, or brother). |
Footnotes
A portion of the data from this report was presented at the 17th annual meeting of the Associated Professional Sleep Societies; June 3–8, 2003; Chicago, IL; and the New York Academy of Sciences Conference on Adolescent Brain Development; September 18–20, 2003; New York, NY.
No conflict of interest declared.
REFERENCES
- 1.Klackenberg G. Sleep behaviour studied longitudinally. Data from 4–16 years on duration, night-awakening and bed-sharing. Acta Paediatr Scand. 1982;71:501–506. doi: 10.1111/j.1651-2227.1982.tb09459.x. [DOI] [PubMed] [Google Scholar]
- 2.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–307. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 3.Liu X, Uchiyama M, Okawa M, Kurita H. Prevalence and correlates of self-reported sleep problems among Chinese adolescents. Sleep. 2000;23:27–34. [PubMed] [Google Scholar]
- 4.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16:258–262. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- 5.Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21:871–881. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- 6.Pollak CP, Bright D. Caffeine consumption and weekly sleep patterns in US seventh-, eighth-, and ninth-graders. Pediatrics. 2003;111:42–46. doi: 10.1542/peds.111.1.42. [DOI] [PubMed] [Google Scholar]
- 7.Bearpark HM, Mitchie PT. Prevalence of sleep/wake disturbances in Sidney adolescents [abstract]. Sleep Res. 1987;16:304. [Google Scholar]
- 8.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–887. [PubMed] [Google Scholar]
- 9.Strauch I, Meier B. Sleep need in adolescents: a longitudinal approach. Sleep. 1988;11:378–386. doi: 10.1093/sleep/11.4.378. [DOI] [PubMed] [Google Scholar]
- 10.Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. J Psychosom Res. 2002;53:561–569. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]
- 11.Price VA, Coates TJ, Thoresen CE, Grinstead OA. Prevalence and correlates of poor sleep among adolescents. Am J Dis Child. 1978;132:583–586. doi: 10.1001/archpedi.1978.02120310047009. [DOI] [PubMed] [Google Scholar]
- 12.Carskadon MA. Factors influencing sleep patterns. In: Carskadon MA, editor. Adolescent Sleep Patterns: Biological, Social, and Psychological Influences. Cambridge University Press; Cambridge, MA: 2002. pp. 4–26. [Google Scholar]
- 13.Manni R, Ratti MT, Marchioni E, et al. Poor sleep in adolescents: a study of 869 17-year-old Italian secondary school students. J Sleep Res. 1997;6:44–49. doi: 10.1046/j.1365-2869.1997.00025.x. [DOI] [PubMed] [Google Scholar]
- 14.Tynjala J, Kannas L, Levalahti E, Valimaa R. Perceived sleep quality and its precursors in adolescents. Health Promot Int. 1999;14:155–166. [Google Scholar]
- 15.Gau SF, Soong WT. Sleep problems of junior high school students in Taipei. Sleep. 1995;18:667–673. doi: 10.1093/sleep/18.8.667. [DOI] [PubMed] [Google Scholar]
- 16.Morrison DN, McGee R, Stanton WR. Sleep problems in adolescence. J Am Acad Child Adolesc Psychiatry. 1992;31:94–99. doi: 10.1097/00004583-199201000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Giannotti F, Cortesi F. Sleep patterns and daytime function in adolescence: an epidemiological survey of an Italian high-school student population. In: Carskadon MA, editor. Adolescent Sleep Patterns: Biological, Social, and Psychological Influences. Cambridge University Press; Cambridge, MA: 2002. pp. 132–147. [Google Scholar]
- 18.Ohayon MM, Roberts RE, Zulley J, Smirne S, Priest RG. Prevalence and patterns of problematic sleep among older adolescents. J Am Acad Child Adolesc Psychiatry. 2000;39:1549–1556. doi: 10.1097/00004583-200012000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Roberts RE, Roberts CR, Chen IG. Ethnocultural differences in sleep complaints among adolescents. J Nerv Ment Dis. 2000;188:222–229. doi: 10.1097/00005053-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Ohayon MM, Caulet M, Lemoine P. Comorbidity of mental and insomnia disorders in the general population. Compr Psychiatry. 1998;39:185–197. doi: 10.1016/s0010-440x(98)90059-1. [DOI] [PubMed] [Google Scholar]
- 21.Wolfson AR, Carskadon MA. Understanding adolescents’ sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7:491–506. doi: 10.1016/s1087-0792(03)90003-7. [DOI] [PubMed] [Google Scholar]
- 22.Fallone G, Owens JA, Deane J. Sleepiness in children and adolescents: clinical implications. Sleep Med Rev. 2002;6:287–306. doi: 10.1053/smrv.2001.0192. [DOI] [PubMed] [Google Scholar]
- 23.Patten CA, Choi WS, Gillin JC, Pierce JP. Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics. 2000;106(2) doi: 10.1542/peds.106.2.e23. Available at: www.pediatrics.org/cgi/content/full/106/2/e23. [DOI] [PubMed] [Google Scholar]
- 24.Pack AI, Pack AM, Rodgman E, Cucchiara A, Dinges DF, Schwab CW. Characteristics of crashes attributed to the driver having fallen asleep. Accid Anal Prev. 1995;27:769–775. doi: 10.1016/0001-4575(95)00034-8. [DOI] [PubMed] [Google Scholar]
- 25.Vignau J, Bailly D, Duhamel A, Vervaecke P, Beuscart R, Collinet C. Epidemiologic study of sleep quality and troubles in French secondary school adolescents. J Adolesc Health. 1997;21:343–350. doi: 10.1016/S1054-139X(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 26.Bruni O, Galli F, Guidetti V. Sleep hygiene and migraine in children and adolescents. Cephalalgia. 1999;19(suppl 25):57–59. doi: 10.1177/0333102499019s2516. [DOI] [PubMed] [Google Scholar]
- 27.Andrade MM, Benedito-Silva AA, Domenice S, Arnhold IJ, Menna-Barreto L. Sleep characteristics of adolescents: a longitudinal study. J Adolesc Health. 1993;14:401–406. doi: 10.1016/s1054-139x(08)80016-x. [DOI] [PubMed] [Google Scholar]
- 28.Carskadon MA. Patterns of sleep and sleepiness in adolescents. Pediatrician. 1990;17:5–12. [PubMed] [Google Scholar]
- 29.Sadeh A, Anders TF. Infant sleep problems: origins, assessment, interventions. Infant Ment Health J. 1993;14:17–34. [Google Scholar]
- 30.LeBourgeois MK. An Instrument to Measure the Behavioral Dimensions of Sleep in Children. University of Southern Mississippi; Hattiesburg, MS: 2001. [Google Scholar]
- 31.American Sleep Disorders Association, editor. International Classification of Sleep Disorders. Allen Press, Inc; Lawrence, KS: 1990. [Google Scholar]
- 32.Zarcone V. Sleep hygiene. In: Kryger MH, Dement WC, editors. Principles and Practice of Sleep Medicine. 3rd ed. W. B. Saunders Co; Philadelphia, PA: 2002. pp. 657–661. [Google Scholar]
- 33.Tynjala J, Kannas L, Valimaa R. How young Europeans sleep. Health Educ Res. 1993;8:69–80. doi: 10.1093/her/8.1.69. [DOI] [PubMed] [Google Scholar]
- 34.Hollingshead AB, Redlich FC. Social Class and Mental Illness. John Wiley & Sons; New York, NY: 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.LeBourgeois M, Hancock M, Harsh J. Validation of the Children's Sleep-Wake Scale (CSWS) [abstract]. Sleep. 2001;24:A219. [Google Scholar]
- 36.LeBourgeois M, Harsh J. A new research instrument for measuring children's sleep [abstract]. Sleep. 2001;24:A213. [Google Scholar]
- 37.Harsh JR, Easley A, LeBourgeois MK. An instrument to measure children's sleep hygiene [abstract]. Sleep. 2002;25:A316. [Google Scholar]
- 38.Carskadon MA, Acebo C. A self-administered rating scale for pubertal development. J Adolesc Health. 1993;14:190–195. doi: 10.1016/1054-139x(93)90004-9. [DOI] [PubMed] [Google Scholar]
- 39.Carskadon MA, Acebo C. Relationship of a Morningness/Eveningness Scale to sleep patterns in preadolescents [abstract]. Sleep Res. 1992;21:367. [Google Scholar]
- 40.Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11:191–199. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- 41.Keppel G. Design and Analysis. 3rd ed. Prentice Hall; Englewood Cliffs, NJ: 1991. [Google Scholar]
- 42.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- 43.Cohen J. The statistical power of abnormal-social psychological research: a review. J Abnorm Soc Psychol. 1962;65:145–153. doi: 10.1037/h0045186. [DOI] [PubMed] [Google Scholar]
- 44.Phillips BA, Danner FJ. Cigarette smoking and sleep disturbance. Arch Intern Med. 1995;155:734–737. [PubMed] [Google Scholar]
- 45.Laberge L, Petit D, Simard C, Vitaro F, Tremblay RE, Montplaisir J. Development of sleep patterns in early adolescence. J Sleep Res. 2001;10:59–67. doi: 10.1046/j.1365-2869.2001.00242.x. [DOI] [PubMed] [Google Scholar]
- 46.Andrade MM, Benedito-Silva AA, Menna-Barreto L. Correlations between morningness-eveningness character, sleep habits and temperature rhythm in adolescents. Braz J Med Biol Res. 1992;25:835–859. [PubMed] [Google Scholar]
- 47.Grunstein R, Grunstein RR. Knowledge about sleep and driving in Australian adolescents [abstract]. Sleep. 2001;24:A111. [Google Scholar]
- 48.Cortesi F, Giannotti F, Sebastiani T, Vagnoni C. Cosleeping and sleep behavior in Italian school-aged children. J Dev Behav Pediatr. 2004;25:28–33. doi: 10.1097/00004703-200402000-00005. [DOI] [PubMed] [Google Scholar]
- 49.Mindell JA. Sleeping Through the Night. HarperCollins Publishers; New York, NY: 1997. [Google Scholar]
- 50.Durand VM. Sleep Better. Brooks/Cole Publishing; Pacific Grove, CA: 1998. [Google Scholar]
- 51.Simonds JF, Parraga H. Prevalence of sleep disorders and sleep behaviors in children and adolescents. J Am Acad Child Psychiatry. 1982;21:383–388. doi: 10.1016/s0002-7138(09)60942-0. [DOI] [PubMed] [Google Scholar]
- 52.Webb WE, Dinges DF. Cultural perspectives on napping and the siesta. In: Dinges DF, Broughton RJ, editors. Sleep and Alertness: Chronobiological, Behavioral, and Medical Aspects of Napping. Raven Press; New York, NY: 1989. pp. 247–265. [Google Scholar]
- 53.Cortesi F, Giannotti F, Sebastiani T, Bruni O, Ottaviano S. Knowledge of sleep in Italian high school students: pilot-test of a school-based sleep educational program. J Adolesc Health. 2004;34:344–351. doi: 10.1016/j.jadohealth.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 54.Rossi CM, Campbell AL, Vo OT, Charron T, Marco CA, Wolfson AR. Middle school sleep-smart program: a pilot evaluation [abstract]. Sleep. 2002;25:A279. [Google Scholar]
- 55.Vo OT, LeChasseur K, Wolfson AR, Marco CA. Sleepy pre-teens: second pilot of the sleep-smart program in 7th graders [abstract]. Sleep. 2003;26:A411. [Google Scholar]
- 56.Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med. 2003;56:769–784. doi: 10.1016/s0277-9536(02)00073-4. [DOI] [PubMed] [Google Scholar]
- 57.Geisinger KF. Cross-cultural normative assessment: translation and adaptation issues influencing the normative interpretation of assessment instruments. Psychol Assess. 1994;6:304–312. [Google Scholar]