Abstract
Meckel's diverticulum (MD) is the most common gastrointestinal anomaly with heterotopic mucosa in 60% of cases. 99m technetium-pertechnetate scintigraphy is a sensitive tool for detection of MD containing heterotopic gastric mucosa. It is usually located in the right lower quadrant or umbilical region and less frequently in other quadrants. A mobile or wandering MD is a rare clinical presentation and may pose a diagnostic dilemma. However, presence of temporal correlation with gastric activity and compactness of focus during wandering period could make this riddle easy.
Keywords: Heterotopic gastric mucosa, Meckel's diverticulum, mobile Meckel's, wandering Meckel's
INTRODUCTION
Meckel's diverticulum (MD) is the most common congenital gastrointestinal anomaly with incidence of 2% in general population[1] and reported complication rate of 4-40%.[2] The most common complications are bleeding, intestinal obstruction and diverticulitis.[3] In 60% of cases MD are lined with heterotopic mucosa, in the following manner: Gastric mucosa, 62%; of pancreatic, 6%; both gastric and pancreatic, 5%, jejunal, 2%; Brunner's glands, 2%; and gastric and duodenal, 2%.[4] Based upon these histological facts, 99m technetium-pertechnetate is the most commonly performed functional imaging for localization of MD lined with heterotopic (mucin secreting cells) gastric mucosa. Higher sensitivity (85-90%) in the pediatric population than in adult (60%) patients is reported.[5] It is most commonly visualized in the right lower quadrant and umbilical regions and less commonly in other regions.[6] Wandering or mobile MD during scintigraphy is a rare presentation and may pose a diagnostic challenge for nuclear physicians.
We are presenting a case of wandering MD during scintigraphy, which would help our readers to be cognizant of this atypical presentation in their clinical practice.
CASE REPORT
A 2-year-old male child admitted to the emergency room with 2 days history of 3 episodes of painless per rectal fresh bleeding. On examination, child was irritable, grossly anemic, afebrile with mild abdomen distention, but audible gut sounds. Per-rectal examination revealed only traces of fresh blood. His hemoglobin was 4.9 g/dl (normal 11-14 g/dl) while other biochemical and bleeding parameters were within the normal limits. Ultrasound abdomen was unremarkable and child had blood transfusions with and started on oral ranitidine (2 mg/kg 12 hourly). On the 3rd admission day, MD scintigraphy was performed with 3 mCi of 99m technetium-pertechnetate injected intravenously with 3 h fasting. Dynamic study for 60 min with a frame rate of 20s/frame was acquired in anterior projection under a dual head digital gamma camera (Ecam, Siemens, Germany) fitted with low energy high resolution collimators. Early images showed the appearance of focus of abnormal tracer deposition in hypogastric region concomitant with the appearance of gastric activity in left hypochondrium and better delineation in subsequent frames same as native gastric activity. Sequential images revealed gross shifting of abnormal focus to left iliac region, hypogastrium, right lumbar, umbilical and finally in epigastric region [Figure 1]. As this abnormal focus remained compact during its tortuous path with no sign of change in its morphology during its whole path, an intraluminal source of radiotracer like bleed (which keeps on changing its shape in lumen of small or large bowel) was ruled out and provisional diagnosis of a wandering MD with heterotopic gastric mucosa was made. The child underwent an exploratory laparotomy and MD was resected and histopathology revealed MD with heterotopic gastric and pancreatic mucosa.
Figure 1.
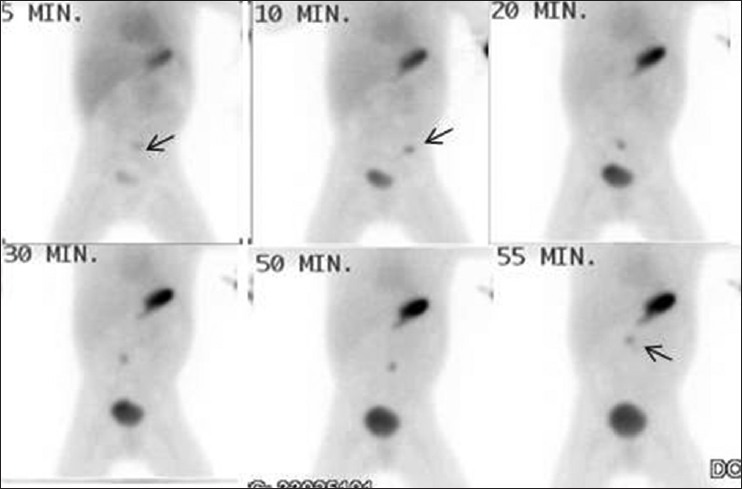
99m technetium-pertechnetate Meckel's diverticulum scintigraphy: Sequential images showing appearance of abnormal focus (arrow) having temporal correlation with gastric activity and wandering in various quadrants maintaining its compactness
DISCUSSION
MD is the most common congenital intestinal anomaly with equal frequency in both genders, but higher incidence of complication in male gender.[2] Presence of adequate heterotopic gastric mucosa (mucin secreting cells) is mandatory for scintigraphic localization of MD with good sensitivity in pediatric group.[5] The characteristic diagnostic criteria are temporal correlation with gastric activity and presence of abnormal focus in umbilical or right lower quadrant. In this case, although there was a good temporal correlation, but abnormal focus was grossly mobile or wandering in various abdominal quadrants. This could easily be confused with ureteric activity or secreted gastric activity entering into duodenum. However, these false positive situations would lack temporal correlation with gastric activity. Furthermore, compactness of mobile focal uptake would be changing with time as it passes through ureter or small bowel lumen. To the best of our knowledge, only three cases of wandering or mobile MD have been reported in the literature.[7,8,9] Primary reason for this feature is mobile and long mesentery[10] and this was the perioperative finding in this child as well. Although diagnosis of MD having heterotopic gastric mucosa on scintigraphy is easy and straightforward but a dynamic or wandering MD may pose a diagnostic challenge. However, temporal correlation with gastric activity and compactness of the focus during wandering period is two sentinel criteria favoring the diagnosis of a MD lined with heterotopic gastric mucosa.
We conclude that wandering MD is a rare scintigraphic presentation, which may pose a diagnostic challenge, but the presence of temporal correlation with gastric activity and compactness of focus during wandering period could make this riddle easy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Satya R, O’Malley JP. Case 86: Meckel diverticulum with massive bleeding. Radiology. 2005;236:836–40. doi: 10.1148/radiol.2363031026. [DOI] [PubMed] [Google Scholar]
- 2.Fink AM, Alexopoulou E, Carty H. Bleeding Meckel's diverticulum in infancy: Unusual scintigraphic and ultrasound appearances. Pediatr Radiol. 1995;25:155–6. doi: 10.1007/BF02010334. [DOI] [PubMed] [Google Scholar]
- 3.Levy AD, Hobbs CM. From the archives of the AFIP. Meckel diverticulum: Radiologic features with pathologic Correlation. Radiographics. 2004;24:565–87. doi: 10.1148/rg.242035187. [DOI] [PubMed] [Google Scholar]
- 4.Matsagas MI, Fatouros M, Koulouras B, Giannoukas AD. Incidence, complications, and management of Meckel's diverticulum. Arch Surg. 1995;130:143–6. doi: 10.1001/archsurg.1995.01430020033003. [DOI] [PubMed] [Google Scholar]
- 5.Poulsen KA, Qvist N. Sodium pertechnetate scintigraphy in detection of Meckel's diverticulum: Is it usable? Eur J Pediatr Surg. 2000;10:228–31. doi: 10.1055/s-2008-1072364. [DOI] [PubMed] [Google Scholar]
- 6.Mittal BR, Kashyap R, Bhattacharya A, Singh B, Radotra BD, Narasimha Rao KL. Meckel's diverticulum in infants and children; technetium-99m pertechnetate scintigraphy and clinical findings. Hell J Nucl Med. 2008;11:26–9. [PubMed] [Google Scholar]
- 7.Wu YC, Kao CH. The ‘wandering’ Meckel diverticulum: An unusual scintigraphic finding. Pediatr Radiol. 2010;40(Suppl 1):S103. doi: 10.1007/s00247-010-1632-8. [DOI] [PubMed] [Google Scholar]
- 8.Hoelzel C, Gillitzer C, Kotzerke J. The floating Meckel. Clin Nucl Med. 2007;32:810–1. doi: 10.1097/RLU.0b013e318148b613. [DOI] [PubMed] [Google Scholar]
- 9.El-Matary W, Roseman D, Lees G, Maguire C. A mobile Meckel! Eur J Pediatr. 2009;168:1525–7. doi: 10.1007/s00431-009-0946-8. [DOI] [PubMed] [Google Scholar]
- 10.Oglevie SB, Smith DC, Gardiner GA. Angiographic demonstration of bleeding in a unusually located Meckel's diverticulum simulating colonic bleeding. Cardiovasc Intervent Radiol. 1989;12:210–2. doi: 10.1007/BF02577156. [DOI] [PubMed] [Google Scholar]


