Abstract
Fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography (F-18 FDG PET/CT) has revealed many unusual presentations and early detection of metastasis in many carcinomas. Epidural involvement in the spine is mostly sequelae of direct infiltration from bony involvement. Direct hematogenous spread to epidural space is very rare. Early diagnosis and treatment before the development of permanent neurologic and functional deficits is essential for a favorable prognosis in such cases. We report here a case of solitary spinal epidural metastasis from lung cancer which was the only systemic metastasis detected on F-18 FDG PET/CT and later confirmed by clinical and regional magnetic resonance imaging findings. This report is, to the best of our knowledge, the first description of such a presentation of systemic metastasis from lung cancer on F-18 FDG PET/CT.
Keywords: Fluorodeoxyglucose positron emission tomography/computed tomography, lung cancer, spinal epidural metastasis
INTRODUCTION
Most of the patients with epidural involvement have associated vertebral metastasis. Most metastatic spinal lesions (70%) are found at the thoracic level, 20% in the lumbar region, and 10% in the cervical region[1] Early diagnosis and appropriate treatment is most important to avoid devastating complication like paraplegia. Magnetic resonance imaging (MRI) is the imaging modality of choice for epidural space assessment,[2] but a symptom-oriented regional MRI is mostly done in these patients. However, spinal epidural metastasis detected in asymptomatic patient with fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography (F-18 FDG PET/CT), followed by targeted MRI before neurological deficits gives the best way to diagnose and treat this condition in early stage.
CASE REPORT
A 78-year-old Indian lady was investigated for cough and weight loss. Initial baseline investigations suggested adenocarcinoma of right lung. Whole body F-18 FDG PET/CT was done for staging workup. The PET/CT scan showed right lung middle lobe mass with few ipsilateral mediastinal lymphnodes. An unusual tracer uptake in D12-L1 right neural foramina region was also noted [Figure 1]. On questioning, she reported lower backache and right hip region pain which was till that time being attributed to old age and degenerative changes. Due to persistent backache, regional MRI was advised after 15 days of PET/CT, which revealed enhancing focal epidural soft tissue thickening on right side at D12-L1 level [Figure 2]. Image-guided biopsy was not amenable and open biopsy was not performed in her clinical context. In view of clinical symptomatology and dual imaging findings, a diagnosis of solitary epidural metastasis was considered. Patient was given for D11-L2 radiotherapy which relieved her symptoms subsequently.
Figure 1.
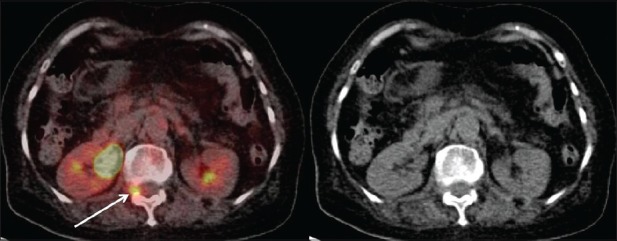
Axial FDG PET CT fused and CT images shows metabolically active lesion in right neural foramina region
Figure 2.
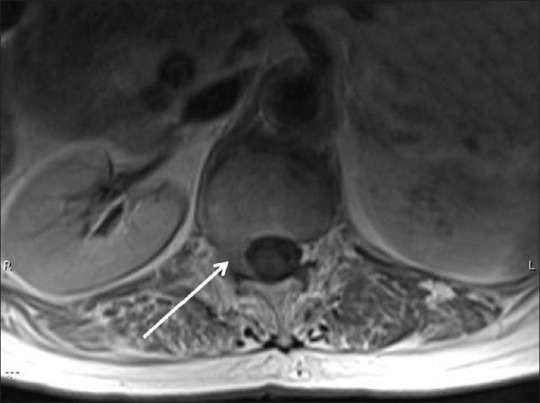
Axial T1W post contrast MRI image shows enhancing soft tissue thickening in right epidural space corresponding to metabolic activity seen on FDG PET CT image
DISCUSSION
Metastatic epidural spinal cord compression (MESCC) is a common neurological complication of cancer that is second only to brain metastasis as the cause of neurological dysfunction caused by metastasis.[3] There are three ways in which metastatic tumors can reach the epidural space. The most common way in approximately 85% of patients, the tumor reaches the spinal cord by the indirect route of an initial hematogenous metastasis to the vertebral body and the metastasis grows in the bone and then spreads into the epidural space, eventually causing secondary compression of the spinal cord.[3] The less common way is invasion of a paravertebral tumor directly into the spinal canal through an intervertebral foramen, which compresses the spinal cord. This process causes about 15% of MESCC and is commonly associated with lymphomas, Ewing's sarcoma, and neuroblastomas. However, least common mode of metastasis described is the direct hematogenous spread to spinal epidural space, dura, or spinal cord.[4]
Back pain is the earliest and most common symptom of spinal epidural metastasis. Back pain is present in more than 95% of patients at diagnosis.[3] The median time from onset of pain to a diagnosis of metastasis is about 2 months.[5] Spinal epidural metastasis associated back pain can takes several forms. Localized pain to the region of the spine affected by the metastases is usually the first symptom; typically, the pain progressively increases in intensity over time. This pain is caused when the bone marrow metastasis extends to stretch the periosteum or invades soft tissues. Radicular pain due to compression or invasion of the nerve roots is commonly present in patients who develop MESCC. The pain is frequently unilateral with cervical or lumbosacral spine involvement or bilateral with thoracic spine involvement. Mechanical back pain is associated with spinal instability caused by vertebral body collapse and is relatively uncommon; it is made worse by movement and partially relieved by rest.[6]
MRI is the method of choice for the diagnosis of spinal epidural metastasis.[2] It provides excellent visualization of soft tissue involvement, bone marrow replacement, ligament involvement, degree of canal compromise, cord edema, and cord compression. The overall accuracy of MRI is 95% (sensitivity 93%, specificity 97%).[7] Normally regional MRI is asked once patient became symptomatic. F-18 FDG PET/CT being a whole body imaging, frequently localized asymptomatic distant metastasis. Most of the spine metastases are associated with extraskeletal metastases. Solitary spinal epidural metastasis has not being reported in the literature so far. In view of no definite distant metastatic sites on FDG PET/CT, tracer uptake in right D12-L1 neural foramina region was kept on follow up. Regional MRI was done later on due to persistent pain which revealed a high probability lesion for epidural metastasis. Biopsy would have been unethical and so not done.
CONCLUSION
Early diagnosis and treatment before the development of neurological and functional deficits is essential for a favorable prognosis in epidural metastasis cases. This case report highlights the role of F-18 FDG PET/CT in early diagnosis of spinal epidural metastasis and with a regional MRI, gives the best opportunity to treat this serious condition in early stage. We suggest keeping this possibility in mind while reporting FDG PET/CT scan.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Aydinli U, Ozturk C, Bayram S, Sarihan S, Evrensel T, Yilmaz HS. Evaluation of lung cancer metastases to the spine. Acta Orthop Belg. 2006;72:592–7. [PubMed] [Google Scholar]
- 2.Jones KM, Schwartz RB, Mantello MT, Ahn SS, Khorasani R, Mukherji S, et al. Fast spin-echo MR in the detection of vertebral metastases: Comparison of three sequences. AJNR Am J Neuroradiol. 1994;15:401–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Cole JS, Patchell RA. Metastatic epidural spinal cord compression. Lancet Neurol. 2008;7:459–66. doi: 10.1016/S1474-4422(08)70089-9. [DOI] [PubMed] [Google Scholar]
- 4.Metser U, Lerman H, Blank A, Lievshitz G, Bokstein F, Even-Sapir E. Malignant involvement of the spine: Assessment by 18F-FDG PET/CT. J Nucl Med. 2004;45:279–84. [PubMed] [Google Scholar]
- 5.Posner JB. Philadelphia: Davis Company; 1995. Spinal metastases. Neurologic complications of cancer; pp. 111–42. [Google Scholar]
- 6.Mavrogenis AF, Pneumaticos S, Sapkas GS, Papagelopoulos PJ. Metastatic epidural spinal cord compression. Orthopedics. 2009;32:431–9. doi: 10.3928/01477447-20090511-20. [DOI] [PubMed] [Google Scholar]
- 7.Li KC, Poon PY. Sensitivity and specificity of MRI in detecting malignant spinal cord compression and in distinguishing malignant from benign compression fractures of vertebrae. Magn Reson Imaging. 1988;6:547–56. doi: 10.1016/0730-725x(88)90129-4. [DOI] [PubMed] [Google Scholar]


