Abstract
The need to develop new dental luting agents in order to improve the success of treatments has greatly motivated research.
Objective
The aim of this study was to evaluate the diametral tensile strength (DTS) and film thickness (FT) of an experimental dental luting agent derived from castor oil (COP) with or without addition of different quantities of filler (calcium carbonate - CaCO3).
Material and Methods
Eighty specimens were manufactured (DTS N=40; FT N=40) and divided into 4 groups: Pure COP; COP 10%; COP 50% and zinc phosphate (control). The cements were mixed according to the manufacturers' recommendations and submitted to the tests. The DTS test was performed in the MTS 810 testing machine (10 KN, 0.5 mm/min). For FT test, the cements were sandwiched between two glass plates (2 cm2) and a load of 15 kg was applied vertically on the top of the specimen for 10 min. The data were analyzed by means of one-way ANOVA and Tukey's test (α=0.05).
Results
The values of DTS (MPa) were: Pure COP- 10.94±1.30; COP 10%- 30.06±0.64; COP 50%- 29.87±0.27; zinc phosphate- 4.88±0.96. The values of FT (µm) were: Pure COP- 31.09±3.16; COP 10%- 17.05±4.83; COP 50%- 13.03±4.83; Zinc Phosphate- 20.00±0.12. One-way ANOVA showed statistically significant differences among the groups (DTS - p=1.01E-40; FT - p=2.4E-10).
Conclusion
The experimental dental luting agent with 50% of filler showed the best diametral tensile strength and film thickness.
Keywords: Dental prosthesis, Biocompatible materials, Ricinus communis, Calcium carbonate, Zinc phosphate cement, Tensile strength
INTRODUCTION
In the past, traditional dental luting agents such as zinc phosphate were commonly used for cementation of crowns21. In spite of disadvantages, such as solubility, lack of retention and low pH7, this luting agent has been successfully used26 and was the most researched cement for over a century. Nowadays, some new adhesive luting agents have been tested in order to reduce microleakage, increase retention, and improve physical properties.
Currently, vegetable polyurethanes, which combine the versatility of polymer formulation with the global concern in producing new biomaterials through resources that preserve the environment, became one of the main studied categories of materials2. In dentistry, membrane material20, sealers17,23,24 and irrigating solution18 were developed from vegetable polyurethane obtained from castor oil. Additionally, since this polyurethane has been described as being biocompatible, osteoconductor, osteoinductor, antimicrobial, osseointegrable and absorbable8,16, it has been used in bone prosthesis, alveolar healing and plastic surgery16. In a study conducted by Camargo, et al.3 (2010), the castor oil bean showed less inflammatory response in subcutaneous tissue of rats when compared with calcium hydroxide cement.
This polyurethane has elasticity, good compatibility, versatility, composition and structure that can be modified in accordance with specific requirements27, characteristics that enable great applicability in the biomedical area and open a new field to the development of dental luting agents. In addition to the innumerable uses of the castor oil, the plant from which it is extracted can be found in many parts of the world. It is greatly exploited in Brazil and India9, and can be produced on a large scale, which makes it interesting from an economic and ecological point of view.
In the oral environment, dental luting agents must withstand masticatory and parafunctional stresses in different clinical situation6,13. They should maintain their integrity while transferring stresses from crowns or fixed partial dentures to tooth structure. Once the retention of crowns is intimately related to mechanical properties of the dental luting agents, the strength of these materials associated to the ability of resisting crack propagation4, which causes ruptures, can predict the clinical success. Resistant dental luting agents provide better stress distribution, less probability of compressive or tensile failures and great probability of clinical success25.
Diametral tensile strength (DTS) is a mechanical property that must be assessed4 because several cements are extremely friable and have a susceptibility to mechanical failure28. This test is widely used due to its relative simplicity and reproducible results. Additionally, it is the most common method for assessing the tensile strength of friable materials because it avoids the difficulties inherent to the flexural tensile strength test1.
In addition to the mechanical properties, physical properties, such as film thickness (FT) of luting agents, can directly affect long-term clinical success. Dental cements should not exhibit a very high FT. Current ISO standards require a FT at the time of seating inferior to 25 µm for water-based luting cements12, and no greater than 50 µm for resin-based cements11. Low FT can improve seating and decrease marginal gaps; whereas improved marginal adaptation can also reduce plaque accumulation, periodontal disease and cement dissolution29. So, the purpose of this study was to compare the DTS and FT of an experimental polyurethane dental luting agent derived from castor oil with traditional zinc phosphate cement.
MATERIAL AND METHODS
The materials with their nomenclature, manufacturers and composition are listed in Figure 1. All materials were proportioned and mixed according to the manufacturers' instructions. Forty specimens were manufactured for DTS test and 40 specimens for FT test.
Figure 1.
Experimental groups, manufacturers and compositions of materials used in this study
| Groups | Manufacturer | Composition |
| Pure COP* | Poliquil Araraquara- Polímeros Químicos Ltda, Araraquara, São Paulo, Brazil | Polyol: tri-functional polyester (castor oil) 370 mgKOH/g Prepolymer: MDI** |
| COP* 10% | Poliquil Araraquara- Polímeros Químicos Ltda, Araraquara, São Paulo, Brazil | Polyol: tri-functional polyester (castor oil) 370 mgKOH/g Prepolymer: MDI** Powder (filler): CaCO3 10% w/w |
| COP* 50% | Poliquil Araraquara- Polímeros Químicos Ltda, Araraquara, São Paulo, Brazil | Polyol: tri-functional polyester (castor oil) 370 mgKOH/g Prepolymer: MDI**Powder (filler): CaCO3 10% w/w |
| Zinc Phosphate | SS White, Rio de Janeiro, Rio de Janeiro, Brazil | Powder: Zinc oxide + Magnesium oxide Liquid: Phosphoric acid + aluminum hydroxide + Zinc oxide + Distilled water |
COP= Castor oil poliurethane;
MDI= methylene diphenyl disocyanato
The castor oil polyurethane (COP) was supplied in sachet. Pure COP contained the prepolymer and polyol separately, while COP 10% and COP 50% included another separation containing 10% or 50% in weight of filler (calcium carbonate - CaCO3), respectively. The quantity of filler, in % weight, was determined by the manufacturer in relation to the sum of the polyol and the prepolymer weights. The mixing method of COP groups includes 2 min of manual mixing into the sachet and other 2 min of mixing with a spatula on a Teflon plate to obtain the final material (Figure 2).
Figure 2.
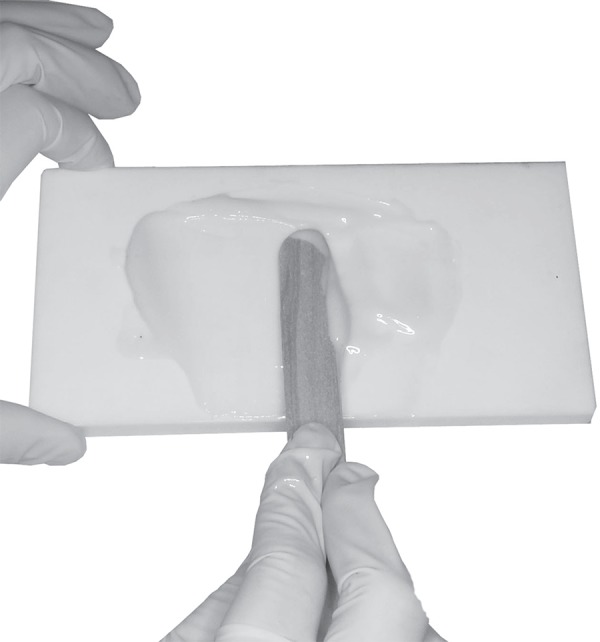
Homogeneous paste of castor oil polyurethane (COP) obtained after manual mixing and mixing with a spatula on a Teflon plate
Zinc phosphate was mixed within 90 s with a spatula following the incremental technique. The proportion of 1.4 g/0.4 mL recommended by the manufacturer was converted to 1.4 g of powder/1.54 g of liquid.
DTS Test: it was conducted with 40 cylindrical specimens (6.0 mm in diameter x 3.0 mm in height) divided into the 4 experimental groups (n=10). Immediately after the mixing, the materials were inserted in a Teflon mold, which was put in a mechanical press under constant load in an atmosphere of 100% relative humidity at 37ºC for 1 h1. Subsequently, all specimens were finished and polished with 400-grit abrasive SiC papers (BuehlerMet Abrasive Papers, Buehler, Lake Bluff, IL, USA) and were stored in distilled water at 37ºC for 24 h before the mechanical test. The specimens were subjected to a compressive load (10 KN) in a universal testing machine (MTS-810 Material Test System, Eden Praire, MN, USA) at a crosshead speed of 0.5 mm/min until fracture. The results were recorded and transformed in tensile values (MPa) by the computer software (Test Star II, International Business Machines Corporation - IBM, Armonk, NY, USA), connected to the system. The results were submitted to one-way ANOVA and Tukey's test (α=0.05) in order to compare the values of DTS among the 4 experimental groups.
FT test: it was conducted with 40 specimens divided into the 4 experimental groups (n=10). The method for determining FT was described in ISO 991719,33. For Pure COP, COP 10% and COP 50%, immediately after the mixing, the dental luting agent was sandwiched between two uniform thickness glass plates (2 cm2) with faces precisely parallels. A load of 15 kg was applied vertically on the top of the glass plate. After 10 min, the thickness of the two plates with cement was determined using a micrometer (Absolute Digimatic Micrometer 227, Mitutoyo Sul America Ltda, Suzano, SP, Brazil). The FT of the cement was calculated by subtracting the thickness of the glasses without the mixed material from the overall thickness. For zinc phosphate group, after 3 min of the beginning of the mixture, the cement was inserted between the two glass plates and submitted to the FT test as cited above.
RESULTS
DTS and FT values of each material are given in Tables 1 and 2.
Table 1.
Diametral tensile strength (MPa) of dental luting agents and standard deviations
| Groups | DTS |
| Pure COP* | 10.94 (1.30)B |
| COP 10% | 30.06 (0.64)A |
| COP 50% | 29.87 (0.27)A |
| Zinc phosphate | 4.88 (0.96)C |
Different uppercase letters indicate significant differences by one-way ANOVA followed by HSD Tukey test One-way ANOVA (p=1.01E-4)
COP = Castor oil polyurethane
DTS= Diametral tensile strenght
Table 2.
Film thicknesses (µm) of dental luting agents and standard deviations
| Groups | Film thickness |
| Pure COP* | 31.09 (3.16)C |
| COP 10% | 17.05 (4.83)AB |
| COP 50% | 13.03 (4.83)A |
| Zinc phosphate | 20.00 (0.12)B |
Different uppercase letters indicate significant differences by one-way ANOVA followed by HSD Tukey test
One-way ANOVA (p=2.4E-10)
COP = Castor oil polyurethane
According to the statistical analysis, all COPs (Pure COP, COP 10% and COP 50%) demonstrated significantly higher (P<0.05) DTS than zinc phosphate. The addition of the filler (CaCO3- 10% and 50% w/w) increased DTS. No significant differences (P>0.05) were found between the DTS values of COP 10% and COP 50%.
As shown in Table 2, FT values of COP 10%, COP 50% and zinc phosphate were inferior to 25 µm; only the Pure COP exceeded this value. There was a positive influence of filler addition in the FT, since the comparisons Pure COP vs. COP 10%, Pure COP vs. COP 50%, COP 10% vs. COP 50% were minor than 0.05 i.e., the mean values of FT diminished as the quantity of filler was incorporated.
DISCUSSION
This research assessed DTS and FT of an experimental polyurethane dental luting agent derived from castor oil, pure or with different quantities of CaCO3, comparing then with zinc phosphate cement.
The zinc phosphate cement and COP differ each other because their viscous and elastic components; zinc phosphate is water-based cement which is more friable after the final setting reaction, while COP is a polymer similar to resinous cements. When submitted to tensile forces, COP shows a curve characteristic of polymers that undergo flow after the linear region of elasticity, with plastic deformation occurring until rupture.
The results showed that the addition of CaCO3 improves the DTS of COP independently of its percentage. Calcium carbonate diminishes the plastic deformation of COP causing an increase in the final resistance since this filler can fill any pores in the matrix, allowing the cement resists to higher loads. The presence of CaCO3 was also proven interesting because it provides radiopacity without affecting biocompatibility14.
Zinc phosphate cement had the lower DTS (4.88 MPa) when compared with COP. DTS of COPs (COP 10% and COP 50%) was higher than values of glass ionomer cement (18 MPa)25 and seems to be more close to the literature results of resin cements which (≈40-45 MPa)6,10,25,26.
With respect to FT, there is no agreement on its minimum value, but values between 50-100 µm seem convenient19. The American Dental Association Specification nº. 8 restricts the zinc phosphate FT ranging from 25 µm to 40 µm5, but literature values of FT of a number of luting materials show that it can range from 10 µm to 152 µm, depending on the nature of the material22.
The results of this study showed that all evaluated dental luting agents, except Pure COP, had FT means inferior to 25 µm, meeting the relevant ISO standard11. The differences found among the FT of the evaluated materials may be explained by the nature and composition of them. While the setting of zinc phosphate cement occurs by means of a water-based reaction with the growth of the crystalline network of the zinc phosphate10, the polymerization of COP includes a moisture curing kinetics which is determined by a reaction between the isocyanate and hydroxyl groups, showing a volumetric expansion and consequently higher FT. The obtained results of zinc phosphate (20.04 µm) are in agreement previous studies21. Pure COP produced FT above the 25 µm recommended by ISO standard.
FT of COP diminished with the addition of CaCO3 making it lesser than that of some resin cements15. Considering that the volumetric expansion is linked to the quantity of organic matrix and that the experimental cement may be composed by only organic matrix (Pure COP) or by an organic matrix with mineral filler (COP+CaCO3), the incorporation of filler diminishes the expansion and consequently provides better FT values.
Despite the clinical importance of the two properties evaluated in this study, the assessment of single properties is not sufficient to identify the best dental luting agent. However, if an experimental dental luting agent does not have appropriate FT and DTS it will not allow the prosthesis serves the functions adequately over a long period. Among the various materials used for cementing indirect restorations and fixed dental prostheses, there is not a single one that fulfills all the characteristics considered ideal. Although one of the experimental materials tested in this study provided better results compared with zinc phosphate cement, further research is required. Comparison with other cements and evaluation of other properties, such as adhesion, hydrolytic degradation and microleakage, can be the focus of future researches. Finally, the introduction of new materials, particularly those not derived from petroleum will enrich the available arsenal of luting materials.
CONCLUSION
Within the limitations of this study, it was conclude that:
1) The polyurethane dental luting agent derived from castor oil (COP) with the addition of CaCO3 filler showed better values of DTS and FT when compared with zinc phosphate cement.
2) For both DTS and FT, the best composition of the experimental polyurethane dental luting agent was the one with the addition of 50% w/w of CaCO3.
Acknowledgments
ACKNOWLEDGEMENTS
The authors of this paper thank to FAPESP for financial support (grants 06/02821-8; 06/00082-3; 07/02441-3)
REFERENCES
- 1.Ban S, Anusavice KJ. Influence of test method on failure stress of brittle dental materials. J Dent Res. 1990;69(12):1791–1799. doi: 10.1177/00220345900690120201. [DOI] [PubMed] [Google Scholar]
- 2.Bao H, Zhang Z, Ying S. Effect of ionic group on the behaviour of polyurethaneurea emulsion. Polymer. 1996;37(13):2751–2754. [Google Scholar]
- 3.Camargo SE, Rode SM, Prado RF, Carvalho YR, Camargo CH. Subcutaneous tissue reaction to castor oil bean and calcium hydroxide in rats. J Appl Oral Sci. 2010;18(3):273–278. doi: 10.1590/S1678-77572010000300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cattani-Lorente MA, Godin C, Meyer JM. Early strength of glass ionomer cements. Dent Mater. 1993;9(1):57–62. doi: 10.1016/0109-5641(93)90107-2. [DOI] [PubMed] [Google Scholar]
- 5.Council on Dental Materials and Devices Council adopts American Dental Association Specification No. 8 (dental zinc phosphate cement) and 11 (agar impression material) . J Am Dent Assoc. 1967;74(7):1565–1573. doi: 10.14219/jada.archive.1967.0412. [DOI] [PubMed] [Google Scholar]
- 6.Della Bona A, Benetti P, Borba M, Cecchetti D. Flexural and diametral tensile strength of composite resins. Braz Oral Res. 2008;22(1):84–89. doi: 10.1590/s1806-83242008000100015. [DOI] [PubMed] [Google Scholar]
- 7.Diaz-Arnold AM, Vargas MA, Haselton DR. Current status of luting agents for fixed prosthodontics. J Prosthet Dent. 1999;81(2):135–141. doi: 10.1016/s0022-3913(99)70240-4. [DOI] [PubMed] [Google Scholar]
- 8.Ferreira CM, Rosa OPS, Torres SA, Ferreira FB, Bernardinelli N. Activity of endodontic antibacterial agents against selected anaerobic bacteria. Braz Dent J. 2002;13(2):118–122. doi: 10.1590/s0103-64402002000200008. [DOI] [PubMed] [Google Scholar]
- 9.Ferreira P, Pereira R, Coelho JF, Silva AF, Gil MH. Modification of the biopolymer castor oil with free isocyanate groups to be applied as bioadhesive. Int J Biol Macromol. 2007;40(2):144–152. doi: 10.1016/j.ijbiomac.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 10.Fonseca RG, Artusi TP, Santos JG, Adabo GL. Diametral tensile strength of dual-curing resin cements submitted exclusively to autopolymerization. Quintessence Int. 2007;38(9):e527–e531. [PubMed] [Google Scholar]
- 11.International Organization for Standardization . ISO 4049: Dentistry - Polymer-based restorative materials. Geneva: The Organization; 2009. [Google Scholar]
- 12.International Organization for Standardization . ISO 9917-1. Dentistry - Water-based cements - part 1: powder/liquid acid based cements. Geneva: The Organization; 2007. [Google Scholar]
- 13.Irie M, Suzuki K, Watts DC. Marginal and flexural integrity of three classes of luting cement, with early finishing and water storage. Dent Mater. 2004;20(1):3–11. doi: 10.1016/s0109-5641(03)00052-6. [DOI] [PubMed] [Google Scholar]
- 14.Jowett AK, Ferguson MW, Combe EC. In vitro biocompatibility testing: a new organ culture model. J Dent. 1988;16(2):55–65. doi: 10.1016/0300-5712(88)90051-6. [DOI] [PubMed] [Google Scholar]
- 15.Kious AR, Roberts HW, Brackett WW. Film thicknesses of recently introduced luting cements. J Prosthet Dent. 2009;101(3):189–192. doi: 10.1016/S0022-3913(09)60026-3. [DOI] [PubMed] [Google Scholar]
- 16.Leite FR, Ramalho LT. Bone regeneration after demineralized bone matrix and castor oil (Ricinus communis) polyurethane implantation. J Appl Oral Sci. 2008;16(2):122–126. doi: 10.1590/S1678-77572008000200008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martins GR, Carvalho CA, Valera MC, Oliveira LD, Buso L, Carvalho AS. Sealing ability of castor oil polymer as a root-end filling material. J Appl Oral Sci. 2009;17(3):220–223. doi: 10.1590/S1678-77572009000300017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meneghin MP, Nomelini SM, Sousa-Neto MD, Marchesan MA, França SC, Santos HS. Morphologic and morphometric analysis of the root canal apical third cleaning after biomechanical preparation using 3.3% Ricinus communis detergent and 1% NaOCl as irrigating solutions. J Appl Oral Sci. 2006;14(3):178–182. doi: 10.1590/S1678-77572006000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Molin MK, Karlsson SL, Kristiansen MS. Influence of film thickness on joint bend strength of a ceramic/resin composite joint. Dent Mater. 1996;12(4):245–249. doi: 10.1016/s0109-5641(96)80030-3. [DOI] [PubMed] [Google Scholar]
- 20.Monteiro AS, Macedo LG, Macedo NL, Balducci I. Polyurethane and PTFE membranes for guided bone regeneration: histopathological and ultrastructural evaluation. Med Oral Patol Oral Cir Bucal. 2010;15(2):e401–e406. doi: 10.4317/medoral.15.e401. [DOI] [PubMed] [Google Scholar]
- 21.Osman SA, McCabe JF, Walls AW. Film thickness and rheological properties of luting agents for crown cementation. Eur J Prosthodont Restor Dent. 2006;14(1):23–27. [PubMed] [Google Scholar]
- 22.Pilo R, Cardash HS. In vivo retrospective study of cement thickness under crowns. J Prosthet Dent. 1998;79(6):621–625. doi: 10.1016/s0022-3913(98)70067-8. [DOI] [PubMed] [Google Scholar]
- 23.Pinheiro CR, Guinesi AS, Pizzolitto AC, Bonetti-Filho I. In vitro antimicrobial activity of Acroseal, Polifil and Epiphany against Enterococcus faecalis. Braz Dent J. 2009;20(2):107–111. doi: 10.1590/s0103-64402009000200003. [DOI] [PubMed] [Google Scholar]
- 24.Rosa PC, Mancini MN, Camargo SE, Garrido AD, Camargo CH, Rode SM. Dimensional alterations and solubility of new endodontic sealers. Braz Dent J. 2010;21(4):301–304. doi: 10.1590/s0103-64402010000400002. [DOI] [PubMed] [Google Scholar]
- 25.White SN, Yu Z. Compressive and diametral tensile strengths of current adhesive luting agents. J Prosthet Dent. 1993;69(6):568–572. doi: 10.1016/0022-3913(93)90283-t. [DOI] [PubMed] [Google Scholar]
- 26.White SN, Yu Z. Physical properties of fixed prosthodontic, resin composite luting agents. Int J Prosthodont. 1993;6(4):384–389. [PubMed] [Google Scholar]
- 27.Yaszemski MJ, Payne RG, Hayes WC, Langer R, Mikos AG. Evolution of bone transplantation: molecular, cellular and tissue strategies to engineer human bone. Biomaterials. 1996;17(2):175–185. doi: 10.1016/0142-9612(96)85762-0. [DOI] [PubMed] [Google Scholar]
- 28.Yettram AL, Wright KW, Pickard HM. Finite element stress analysis of the crowns of normal and restored teeth. J Dent Res. 1976;55(6):1004–1011. doi: 10.1177/00220345760550060201. [DOI] [PubMed] [Google Scholar]
- 29.Yu Z, Strutz JM, Kipnis V, White SN. Effect of dynamic loading methods on cement film thickness in vitro. J Prosthodont. 1995;4(4):251–255. doi: 10.1111/j.1532-849x.1995.tb00351.x. [DOI] [PubMed] [Google Scholar]


