Abstract
Objective
Stimulant medications such as methylphenidate (MPH) improve the academic performance of children with ADHD. However, the mechanism by which MPH exerts an effect on academic performance is unclear. We examined MPH effects on math performance and investigated possible mediation of MPH effects by changes in time on-task, inhibitory control, selective attention, and reaction time variability.
Methods
Children with ADHD ages 7–11 years (n=93) completed a timed math worksheet (with problems tailored to each individual’s level of proficiency) and two neuropsychological tasks (Go/No-Go and Child Attention Network Test) at baseline, then participated in a four week randomized controlled titration trial of MPH. Children were then randomly assigned to their optimal MPH dose or placebo for one week (administered double-blind), and repeated the math and neuropsychological tasks (post-test). Baseline and post-test video-recordings of children performing the math task were coded to assess time on-task.
Results
Children taking MPH completed 23 more math problems at post-test compared to baseline while the placebo group completed 24 fewer problems on post-test versus baseline, but effects on math accuracy (% correct) did not differ. Path analyses revealed that only change in time on-task was a significant mediator of MPH’s improvements in math productivity.
Conclusions
MPH-derived math productivity improvements may be explained in part by increased time spent on-task, rather than improvements in neurocognitive parameters such as inhibitory control, selective attention, or reaction time variability.
INTRODUCTION
Attention-deficit/hyperactivity disorder (ADHD) -- a prevalent neurobehavioral disorder characterized by difficulties with attention, impulsivity, and/or overactivity – is associated with impairments in a variety of domains. Academic functioning is a particular challenge, as children with ADHD have lower academic achievement scores and grades, as well as higher rates of school dropout, compared to typically developing children.1 Individuals with ADHD appear particularly vulnerable to falling behind in math, and have demonstrated a substantial gap in math achievement scores [effect size d=0.67],2 in addition to reduced productivity and accuracy on math computation worksheets,3 compared to their non-ADHD peers.
Although some early studies suggested that stimulant medication treatment may not enhance academic functioning in children with ADHD,4 more recent evidence has documented small but significant improvements in academic achievement scores with psychostimulant treatment.5 In addition to assessing methylphenidate effects on academic achievement, which primarily reflect academic knowledge, researchers have also been interested in investigating the effects of stimulant medications on effortful performance in the classroom (i.e., academic productivity). Math worksheet paradigms have been developed to simulate typical elementary school seatwork, and improvements in math productivity (number of problems attempted and number answered correctly) with psychostimulant treatment have been documented.6
Despite accumulating evidence that psychostimulants may improve math performance, the mechanisms by which they may do so have received relatively little attention,7 and to our knowledge there are no prior studies investigating mediators of stimulant effects on academic outcomes. Improvements in various aspects of executive functioning are a plausible mediator of stimulant effects on math performance, as overall executive function,8 selective attention,9 and inhibitory control10 have been linked to math performance, and stimulant medications have been shown to enhance performance in these neurocognitive domains in some but not all studies.11 Change in reaction time variability is another possible mechanism underlying stimulant effects on math performance, given that children with ADHD are more variable in their reaction times than typically developing children across nearly every type of neuropsychological task,12 and stimulant medication has been shown to attenuate reaction time variability.11 However, little is currently known about the relationship between math performance and reaction time variability. In addition, since psychostimulants affect behaviors such as time spent on-task13 and on-task behavior has been related to math performance ,14 increased time on-task is another possible mediator of the relationship between methylphenidate effects and improved math performance.
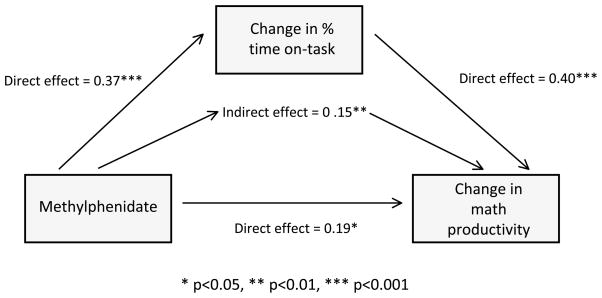
In the context of a randomized clinical trial, the current study sought to examine the effects of methylphenidate on math productivity and accuracy in children with ADHD, and to investigate mediators of methylphenidate’s effects on math performance. We hypothesized that changes in inhibitory control, selective attention, reaction time variability, and time spent on-task may mediate methylphenidate effects on math as these have been shown in prior studies to be either influenced by methylphenidate11 or correlated with math performance.9, 10 See Figure 1, which illustrates this study’s conceptual model.
Figure 1.
Candidate mediators that could potentially explain the beneficial effects of methylphenidate on math productivity
METHODS
Participants
Stimulant-naïve children ages 7–11 were recruited through multiple community and clinical sources (including schools and local practitioners) to participate in a study of neuropsychological performance in children with ADHD. The primary aims of this parent study were to determine ADHD-related neuropsychological performance deficits, particularly those related to reaction time variability12 as well as to determine medication effects on neuropsychological performance.11 All children met diagnostic criteria for ADHD combined type or inattentive type. Diagnostic status was determined using methodology similar to that employed by the Multimodal Treatment Study of ADHD and as per prior studies utilizing this sample.11, 12 The Diagnostic Interview Schedule for Children-Parent Report (DISC-P15) and the Vanderbilt ADHD Teacher Rating Scale16 were used to assess for ADHD. The DISC-P further assessed for a range of comorbid mental health disorders, and those with mania/hypomania were excluded. Children with comorbid anxiety, mood, oppositional defiant, and conduct disorders were included unless these conditions were determined to be the underlying cause of ADHD symptoms or required different treatment.
Children with a Full Scale IQ below 80 (as estimated by the Wechsler Abbreviated Scale of Intelligence [WASI]), and those with standardized achievement scores below 80 on the Wechsler Individual Achievement Test, Second Edition (WIAT-II) Reading or Numerical Operations subtests were excluded from the study in order to rule out children with possible learning disorders.17 Children were also excluded from participation if their medical history suggested organic brain injury (e.g., traumatic brain injury, epilepsy, history of cerebral infarction, etc.).
This study was approved by the Cincinnati Children’s Hospital Institutional Review Board. All participants (n=93) provided written informed consent/assent. An additional 53 children consented for the study but did not participate: 4 lost contact with the study and 49 were excluded. Reasons for exclusion included having an IQ < 80 (N=9), having achievement test standard scores <80 (N=21), not meeting diagnostic criteria for ADHD combined type or inattentive type (N=27), ADHD was not the child’s primary mental health diagnosis (N=3), and undetermined (N=1) [total is > 49 due to some children having more than one reason for exclusion].
Medication titration trial
Participants underwent a four-week within subject, randomized, double-blind crossover trial of long-acting OROS (Osmotic-controlled Release Oral delivery System) methylphenidate (Concerta® [Janssen Pharmaceuticals, Inc., Titusville, New Jersey]), including three active dosage weeks (18mg, 27mg, 36mg for children < 25 kg; 18mg, 36mg or 54mg for children ≥ 25 kg) and one week of placebo, as described in prior publications.11 At the end of each week, parents and teachers filled out Vanderbilt ADHD Rating Scales16, 18 and Pittsburgh Side Effects Rating Scales,19 and the study physician also met with participant families and completed a Clinical Global Impression-Improvement (CGI-I) to assess response to medication. At the end of the medication titration trial, two physicians (WB, TF) blindly reviewed graphs portraying each week’s parent, teacher, and clinician ratings, and each chose an optimal week based on the balance between effectiveness and side effects. Clinician agreement on optimal week (84% agreement) was comparable to that reported in the MTA study.20 Disagreements were resolved through a consensus process. ADHD symptom ratings showed significant improvement during the optimal dose week compared to the placebo week, with effect sizes for these behavioral effects of methylphenidate 0.82 and 0.87 for parent and teacher ratings, respectively.11
Procedures
Participants underwent an initial screening visit during which their caregivers were administered the DISC-P interview and children were administered the WASI and WIAT-II. This was followed by two neuropsychological baseline assessment visits, each lasting approximately two hours, during which children completed the neuropsychological testing and analogue math task described below. Children then participated in the medication titration trial to determine their optimal methylphenidate dosage, and then were randomized to receive placebo or the optimal dosage from the medication titration trial for a week. During that week, children repeated the two day neuropsychological battery and math task assessment (post-testing). For all children randomized to the placebo condition, at least 4 days elapsed between their last MPH dose and post-testing. All post-testing began between one to four hours after medication/placebo ingestion, as reported by parents.
Neuropsychological Battery
Participants completed a battery of 5 computer-based neuropsychological tasks, including the Go/No-Go, Child Attention Network Test (ANT), Choice Discrimination, Stop-signal, and N-back tasks.11 Only the Go/No-Go and Child Attention Network Test (ANT) tasks were selected for these analyses because performance on the other 3 tasks was not significantly improved with MPH in our prior study (MPH effect F statistic ≤4.24 for the Choice Discrimination task, ≤1.30 for the Stop-signal task, and ≤3.51 for the N-back task, all p values >0.05).11 Excluding the practice trials, the GNG task was 21 minutes and the Child ANT task took 15 minutes. A brief description of each task is provided below, with fuller details about each task, task programming, event rates, stimulus presentation duration, interstimulus intervals, and number of trial blocks presented in prior publications.11, 12
Go/No-Go task (GNG).21
Participants were directed to respond by pressing the spacebar to a variety of non-target stimuli (i.e., letters shown on a screen one by one) while inhibiting their response to a specified target stimulus (the letter ‘X’). Correct response was defined as pressing the spacebar when any letter except ‘X’ was shown, and inhibiting depression of the spacebar when an ‘X’ appeared on the screen. The GNG task was used to assess inhibitory control (GNG accuracy, or number of correct responses divided by the number of trials) and inhibitory control reaction time variability (GNG reaction time standard deviation [RTSD]).
Child Attention Network Test (ANT).22
Participants were presented a target stimulus (a fish) either individually or in the center of a horizontal row of 5 distractor stimuli (identical fish), and asked to indicate the direction of the target stimulus by pressing the appropriate arrow button. Correct responses were defined as correctly indicating the direction (right or left) that the target stimulus was facing. The task includes congruent trials (target facing the same direction as distractors), incongruent trials (target facing the opposite direction as distractors), and neutral trials (target presented by itself). Prior to each trial, participants were provided with one of four target cues: 1) a central cue (i.e., an asterisk in the center of the screen), 2) a double cue (i.e., asterisks above and below the center of the screen), 3) a spatial cue (i.e., an asterisk in the location in which the target will appear), or 4) no cue. Each cue was maintained for 150 milliseconds (ms), followed by a 450ms presentation of a fixation cross, followed by a 500ms stimulus presentation. The ANT task was used to measure selective attention (ANT accuracy, or number of correct responses divided by the number of trials) and selective attention reaction time variability (ANT reaction time standard deviation [RTSD]).
Analogue Math Task and Time on-task Assessment
The analogue math task is a naturalistic task modeled after math work undertaken in a typical classroom setting (e.g., self-directed classroom work or homework). Each participant first underwent an assessment to determine his/her math level (i.e., single digit addition, multiple digit addition, single digit multiplication, multiple digit multiplication) using curriculum based measurement methodology,23 then completed math worksheets at his/her own appropriate level for twenty minutes while being video-recorded. Measures of math performance included math productivity (total number of problems completed) and accuracy (number of math problems completed correctly divided by total number completed).
To assess each participant’s time spent on-task, four trained personnel coded math task video recordings, as described in detail elsewhere.24 Briefly, the coders used Noldus Observer XT® software (Noldus Information Technology, 2008) to record the onset and offset of each participant’s attention towards the task. A participant’s behavior was coded as “off-task” when his/her visual gaze left the paper for two or more seconds. However, visual gazes away from the worksheet while counting aloud or counting on one’s fingers was not coded as “off-task.” Percentage of time on-task was calculated by summing the time on-task and dividing by the total length of the recording. Inter-rater reliability, as assessed by intraclass correlation coefficients (ICC), was high for total time on-task (ICC=.89).
Statistical Analyses
Association between Primary Predictor (Assignment to MPH) and Math Outcomes
The association between assignment to MPH and the math outcomes of change in productivity (post-test number of problems completed minus baseline number of problems completed) and change in accuracy (post-test % of problems completed correctly minus baseline % of problems completed correctly) was evaluated using linear regression.
Assessment of Mediation
Potential mediators included change in the time on-task variable and change in any neuropsychological variable that was shown to be sensitive to the effects of MPH in Epstein et al.11 (i.e., GNG accuracy, GNG reaction time standard deviation, ANT accuracy, ANT reaction time standard deviation). For each potential mediator, a pre-post change score was computed by subtracting pre-test scores from post-test scores. A basic assumption of mediation is that the independent variable must correlate with the mediating variable and the mediating variable must correlate with the dependent variable.25 Therefore, regressions were conducted to examine whether MPH status predicted pre-post change in each mediator. Correlations between change in each potential mediator and the math outcomes (change in productivity and change in accuracy) were assessed using Pearson correlations.
Where the basic mediation assumptions were met, we then tested mediation for each candidate mediator in a separate model using path analysis. For each model, pathways from MPH assignment to the mediator and from the mediator to the math outcome were estimated. In addition, a path was modeled from MPH assignment to the math outcome. To determine if the mediated effect was significant, the test for intervening variables as outlined by MacKinnon and colleagues26 was utilized.
Assessment of Potential Confounders
Finally, in order to identify potential confounders of the association between MPH and the math outcomes, we conducted chi-square and t-tests to assess whether a list of potential covariates were related to both MPH and math outcomes. Covariates assessed included baseline math productivity (number of math problems completed at the study entry assessment), baseline math accuracy (% of math problems completed correctly at the study entry assessment), age (in years), WASI verbal IQ standard score, WASI performance IQ standard score, WIAT numerical operations standard score, teacher baseline hyperactive-impulsive symptom score (from Vanderbilt ADHD Teacher Rating Scale completed at study entry), grade (year in school), sex, race (as reported by caregiver), presence of comorbid anxiety (as determined by the DISC-P), presence of comorbid oppositional defiant disorder or conduct disorder (as determined by the DISC-P), and ADHD subtype (children were considered to have met the criteria for a symptom domain [i.e., inattention or hyperactivity/impulsivity] if the parent/caregiver on the DISC-P and the teacher on the Vanderbilt ADHD Teacher Rating Scale reported six non-overlapping symptoms in a symptom domain and both the parent and teacher reported at least four symptoms in that domain). None of the above factors were associated with both assignment to MPH and the math outcomes at p<0.1. Therefore, they were not included in the investigation of mediation effects in our path analysis.
Missing Data
Fifteen of our participants had some missing outcome data (1 did not complete the baseline math task due to having a broken hand, 3 did not return for post-testing, 1 was missing post-test ANT data due to refusal complete the task, and technical computer or video-recording difficulties led to missing data for 10 participants [1 lacked baseline ANT data, 1 lacked post-test ANT and baseline time on-task data, 5 lacked baseline time on-task data, and 3 lacked post-test time on-task data]). Nonetheless, our missing data was a relatively small percentage of our total outcome variables (<5%). In addition, participants with complete data compared to those with any missing data did not differ in sex, race, age, ADHD subtype, parent and teacher inattentive and hyperactive-impulsive symptom scores, assignment to MPH versus placebo, or math problem difficulty level (all p>0.12). For the linear regression and correlational (Pearson’s r) analyses, the missing values were estimated using multiple imputation: we generated ten imputed data sets and combined the parameter estimates obtained from each data set using methods from Rubin27 and implemented via the NORM software.28 For the path analyses, the full information maximum likelihood (FIML) estimation method, which estimates a likelihood function for each missing value based on the variables that are present, was utilized to address missing values.
RESULTS
Study sample characteristics are shown in Table 1. The groups randomized to MPH versus placebo for post-testing did not differ in terms of age, sex, race/ethnicity, ADHD subtype, IQ, math achievement scores, baseline ADHD symptom scores, mental health comorbidity, or math worksheet difficulty level.
Table 1.
Demographic and clinical characteristics of sample (n=93)
| Randomized to MPH1 (n =47) | Randomized to Placebo (n =46) | P-value for Group Comparisons | |
|---|---|---|---|
| Mean (SD2) age in years | 8.2 (1.2) | 8.0 (1.2) | 0.63 |
| Number female (percentage) | 14 (30) | 11 (24) | 0.56 |
| Caucasian, non-Hispanic | 38 (81) | 32 (70) | 0.21 |
| African American, Hispanic, Other | 9 (19) | 14 (30) | |
| ADHD subtype | |||
| Inattentive type | 22 (47) | 26 (56) | 0.35 |
| Combined type | 25 (53) | 20 (44) | |
| WASI3 full scale IQ4 (SD2) | 106 (13) | 105 (13) | 0.57 |
| WIAT-II5 numerical operations score (SD2) | 98 (13) | 96 (13) | 0.52 |
| Baseline Parent Vanderbilt Total Symptom Scores (SD2) | 38 (10) | 37 (9) | 0.71 |
| Baseline Teacher Vanderbilt Total Symptom Scores (SD2) | 35 (10) | 34 (11) | 0.73 |
| Number with specified comorbid psychological disorder from DISC-P6 (percentage) | |||
| Oppositional Defiant, Conduct Disorder | 18 (38) | 26 (35) | 0.72 |
| Any Anxiety Disorder | 15 (32) | 16 (35) | 0.77 |
| Any Mood Disorder | 1 (2) | 1 (2) | 0.99 |
| Number completing each math problem difficulty level | |||
| Single Digit Addition | 26 (55) | 22 (48) | 0.87 |
| Double Digit Addition | 10 (21) | 13 (28) | |
| Single Digit Multiplication | 8 (17) | 8 (17) | |
| Multiple Digit Multiplication | 3 (6) | 3 (7) | |
| Titration trial optimal dosage in mg/kg/day (SD2) | 0.89 (0.64) | 0.81 (0.66) | 0.58 |
MPH = methylphenidate
SD = standard deviation
WASI = Wechsler Abbreviated Scale of Intelligence
IQ = Intelligence Quotient
WIAT-II = Wechsler Individual Achievement Test, Second Edition
DISC-P = Diagnostic Interview Schedule for Children-Parent Report
MPH effects
Those randomized to MPH completed 23 more math problems at post-test compared to baseline while the placebo group completed 24 fewer problems on post-test compared to baseline (β=46.1, p=0.001). The MPH effect size was medium to large (Cohen’s d=0.72). MPH did not affect math accuracy. See Table 2.
Table 2.
Methylphenidate (MPH) and placebo group means and differences for changes in math outcomes and potential mediators
| Outcome or Potential Mediator | MPH [n =47] Mean (SD1) | Placebo [n =46] Mean (SD1) | β | p value |
|---|---|---|---|---|
| Change in math productivity | 23.4 (73.1) | −23.7 (55.5) | 46.1 | 0.001 |
| Change in math accuracy | 0.8 (8.2) | −0.9 (11.5) | 1.7 | 0.44 |
| Change in % time on-task | 5.2 (14.4) | −5.7 (15.6) | 10.9 | 0.001 |
| Change in GNG2 accuracy | 1.3 (12.9) | −7.7 (14.8) | 9.0 | 0.002 |
| Change in GNG2 RTSD3 | −28.4 (260.3) | 136.1 (179.3) | −164.5 | <0.001 |
| Change in ANT4 accuracy | 8.7 (12.9) | 2.0 (12.3) | 6.7 | 0.009 |
| Change in ANT4 RTSD3 | −181.6 (347.1) | 11.0 (184.8) | −192.7 | <0.001 |
SD = standard deviation
GNG = Go/No-Go
RTSD = reaction time standard deviation
ANT = Attention Network Test
Association between MPH and Potential Mediators
As reported elsewhere,11 assignment to MPH was significantly associated with improved GNG accuracy (β=9.0, p=0.002), reduced GNG reaction time variability (β=−164.5, p<0.001), improved ANT accuracy (β=6.7, p=0.009), and reduced ANT reaction time variability (β=−192.7, p<0.001). Assignment to MPH was also significantly associated with increased % time on-task (β=10.9, p=0.001). See Table 2.
Association between Potential Mediators and Math Outcomes
Change in math productivity was significantly and positively associated with change in % time on-task (r=0.47, p<0.0001), GNG accuracy (r=0.24, p=0.03), and GNG reaction time variability (r=0.22, p=0.04). No significant correlations were observed between change in math productivity and change in ANT accuracy or ANT reaction time variability (r=0.12, p=0.25 and r=0.19, p=0.07 respectively). No potential mediators were significantly correlated with change in math accuracy (all r<0.15, p>0.18).
Assessment of Mediation
Among possible mediators, only change in % time on-task, GNG accuracy, and GNG reaction time variability were associated with both MPH and change in math productivity. Thus, each of these three possible mediators was tested for mediation. All three models terminated normally and had acceptable fit indices (Chi-square (3) < 33.70, p values <.001; CFIs >1.00, GFIs >1.00, and RMSEA = 0.00).
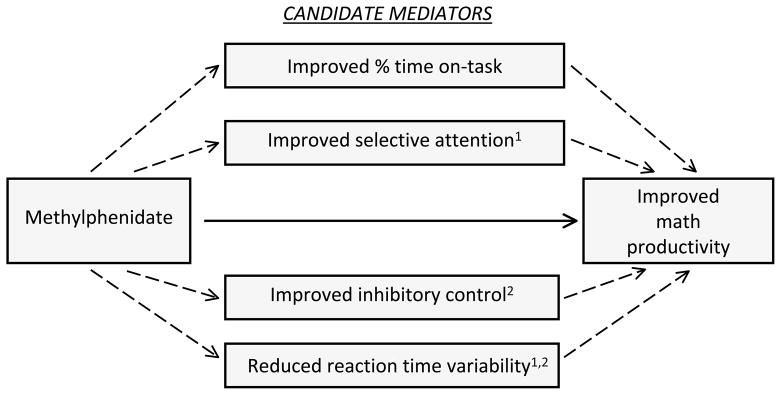
Change in % time on-task mediated the association between MPH and math productivity (See Figure 2). The direct link between assignment to MPH and change in math productivity was significant in the model that included difference in % time on-task. Furthermore, the mediated effect (i.e., the indirect effect) from MPH assignment to change in math productivity through difference in time on-task was significant (indirect effect = 0.15, test of indirect effect = 2.79, p<.01). Differences in GNG accuracy and its reaction time variability did not identify significant mediated effects (test of indirect effects ≤1.38, p values >.16) [See Table 3 and Supplementary Figure].
Figure 2.
Standardized coefficients for direct and indirect effects of assignment to methylphenidate (MPH) and change in time on-task on change in math productivity
Table 3.
Standardized coefficients for direct and indirect effects of assignment to methylphenidate on change in math productivity for each of the three mediator models
| Tested Mediator | Direct Effect | Indirect Effect |
|---|---|---|
| Estimate (test of estimate) | Estimate (test of estimate) | |
| Change in % time on-task | 0.19* (1.97) | 0.15** (2.79) |
| Change in GNG1 accuracy | 0.29** (2.91) | 0.05 (1.38) |
| Change in GNG1 RTSD2 | 0.30** (3.00) | 0.04 (1.03) |
p < .01,
p < .05
GNG = Go/No-Go
RTSD = reaction time standard deviation
DISCUSSION
In a sample of children with ADHD without evidence of learning or cognitive disorders, we found that methylphenidate improved math productivity, with an effect size (Cohen’s d = 0.72) comparable to that of methylphenidate effects on ADHD symptoms (effect sizes of 0.8–1.0).29 Methylphenidate also significantly improved children’s observed ability to remain on-task and improved several areas of neurocognition (i.e., inhibitory control, selective attention and reaction time variability). While improvements in on-task behavior, inhibitory control, and reaction time variability correlated with improvements in math productivity, only improvement in on-task behavior appeared to mediate MPH effects on math productivity. Thus, it appears that MPH exerts its effect on math productivity in part by increasing the proportion of time that children spend attending to the task.
Reasons why children spent more time on-task after receiving methylphenidate are unclear. It may be that MPH enhanced the participants’ perception of the math task’s saliency. Volkow et al have documented that individuals receiving methylphenidate prior to performing a math task rate the task as being “more interesting, motivating, and less tiresome” compared to those receiving placebo, and these MPH-associated ratings of enhanced task saliency are associated with increased extracellular striatal dopamine.7 The important role of motivation and task saliency in academic productivity may also help to explain why the subjects receiving placebo performed worse after repeated math testing compared to baseline in our and other studies.30 While the participants likely had increased interest in the baseline math and neuropsychological testing due to the novelty of the tasks and study participation, it is postulated that the placebo-treated subjects lacked motivation during the post-test repetition of the two day neuropsychological and math task battery, given that individuals with ADHD are particularly susceptible to boredom.31 Alternately, it could be that ongoing MPH treatment may lead to neurophysiologic adaptations that produce a transient neurobehavioral worsening on discontinuation. Although further study is necessary to confirm or refute this hypothesis, some ADHD neuroimaging studies have documented an up-regulation of dopamine transporter availability following sustained MPH treatment that the authors propose may lead to an exacerbation of ADHD symptoms while not under the effects of medication.32
Although MPH improved various aspects of neurocognition in our study, and improvement in inhibitory control and reaction time variability were also correlated with increased math productivity, it is difficult to determine why enhancement in these neurocognitive parameters did not appear to explain or contribute to methylphenidate-associated improvements in math productivity. One possible explanation may be that our participants may not have been challenged to a great enough degree during the math task to allow for changes in executive or neuropsychological functioning to be influential, as we used pre-testing to customize the math task and select a math level for each child in which the child demonstrated proficiency. When working on this less challenging and perhaps less stimulating material, improvement in on-task behavior appeared to be a mechanism by which methylphenidate improved math productivity. However, if our participants had been working at an instructional or frustration level instead, perhaps improvements in executive functioning may have emerged as mediators of methylphenidate effects on math performance. Similarly, our customization of the math task to each participants’ level of proficiency likely limited our ability to document MPH effects on math accuracy due to a ceiling effect, as both the MPH and placebo groups demonstrated >90% accuracy at baseline. In contrast, MPH math studies that administered problems based on each child’s grade rather than his/her actual proficiency level found baseline accuracy of <80% for children with ADHD and did find that MPH improved math accuracy.33
Thus, our study findings are limited to MPH effects on math performance when children are working on a proficiency level, but we cannot draw conclusions regarding MPH effects or its mediators when children are challenged at an instructional or frustration level. Similarly, we cannot comment on MPH effects on outcomes such as math achievement, or on other academic domains such as reading or written expression. In addition, we did not evaluate other executive functions such as working memory as mediators of MPH effects on math because MPH did significantly improve performance on the working memory (N-back) task administered to this sample.11 It is also important to consider that our results may not fully generalize to real world settings. Despite our math task being designed to simulate work undertaken in a typical classroom setting, it was completed in a lab setting where attentional demands unique to an actual classroom may not have been present. Furthermore, children with poor math achievement were excluded from the study and, thus, the pattern of study findings may not apply to those children with learning disabilities. Finally, our findings may not generalize to all children with ADHD, as our stimulant-naïve sample was recruited from both community and clinical sources, and had generally lower rates of mental health comorbidity than samples recruited solely from subspecialty clinics.34
Conclusions
We found that MPH-derived improvements in math productivity may be explained in part by increases in time spent on-task, rather than changes in inhibitory control, selective attention, or reaction time variability. This study is one of the few to date to investigate mechanisms by which psychostimulant treatment may lead to improvements in academics,7 other aspects of academic performance, or even ADHD symptoms.35 Knowledge of the mechanisms by which methylphenidate exerts its therapeutic effects is crucial for the development of additional pharmacological and non-pharmacological therapies to treat ADHD-related impairments, and is regarded as “a necessity if progress regarding ADHD treatments is to proceed with precision, rigor, and clinical and conceptual elucidation.”35
Supplementary Material
Acknowledgments
Source of Funding: The project described was supported by the National Institute of Mental Health (R01MH074770 [Epstein], K23 MH083881 [Froehlich], K23MH083027 [Brinkman], K24 MH064478 [Epstein]). The content is solely the responsibility of the authors and does not represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest or disclosures to report.
Supplementary Figure. Standardized coefficients for direct and indirect effects of methylphenidate and change in inhibitory control accuracy on change in math productivity
References
- 1.Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. J Pediatr Psychol. 2007;32(6):643–654. doi: 10.1093/jpepsy/jsl054. [DOI] [PubMed] [Google Scholar]
- 2.Frazier TW, Youngstrom EA, Glutting JJ, et al. ADHD and achievement: meta-analysis of the child, adolescent, and adult literatures and a concomitant study with college students. J Learn Disabil. 2007;40(1):49–65. doi: 10.1177/00222194070400010401. [DOI] [PubMed] [Google Scholar]
- 3.Benedetto-Nasho E, Tannock R. Math computation, error patterns and stimulant effects in children with Attention Deficit Hyperactivity Disorder. J Attention Disorders. 1999;3(3):121–134. [Google Scholar]
- 4.Swanson JM, Cantwell D, Lerner M, et al. Effects of stimulant medication on learning in children with ADHD. J Learn Disabil. 1991;24(4):219–230. 255. doi: 10.1177/002221949102400406. [DOI] [PubMed] [Google Scholar]
- 5.Langberg JM, Becker SP. Does Long-Term Medication Use Improve the Academic Outcomes of Youth with Attention-Deficit/Hyperactivity Disorder? Clin Child Fam Psychol Rev. 2012 doi: 10.1007/s10567-012-0117-8. [DOI] [PubMed] [Google Scholar]
- 6.Swanson JM, Wigal SB, Wigal T, et al. A comparison of once-daily extended-release methylphenidate formulations in children with attention-deficit/hyperactivity disorder in the laboratory school (the Comacs Study) Pediatrics. 2004;113(3 Pt 1):e206–216. doi: 10.1542/peds.113.3.e206. [DOI] [PubMed] [Google Scholar]
- 7.Volkow ND, Wang GJ, Fowler JS, et al. Evidence that methylphenidate enhances the saliency of a mathematical task by increasing dopamine in the human brain. The American journal of psychiatry. 2004;161(7):1173–1180. doi: 10.1176/appi.ajp.161.7.1173. [DOI] [PubMed] [Google Scholar]
- 8.Biederman J, Monuteaux MC, Doyle AE, et al. Impact of executive function deficits and attention-deficit/hyperactivity disorder (ADHD) on academic outcomes in children. Journal of consulting and clinical psychology. 2004;72(5):757–766. doi: 10.1037/0022-006X.72.5.757. [DOI] [PubMed] [Google Scholar]
- 9.Stevens C, Bavelier D. The role of selective attention on academic foundations: A cognitive neuroscience perspective. Dev Cogn Neurosci. 2012;2 (Suppl 1):S30–48. doi: 10.1016/j.dcn.2011.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.St Clair-Thompson HL, Gathercole SE. Executive functions and achievements in school: Shifting, updating, inhibition, and working memory. Q J Exp Psychol (Hove) 2006;59(4):745–759. doi: 10.1080/17470210500162854. [DOI] [PubMed] [Google Scholar]
- 11.Epstein JN, Brinkman WB, Froehlich T, et al. Effects of Stimulant Medication, Incentives, and Event Rate on Reaction Time Variability in Children With ADHD. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2011;36(5):1060–1072. doi: 10.1038/npp.2010.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Epstein JN, Langberg JM, Rosen PJ, et al. Evidence for higher reaction time variability for children with ADHD on a range of cognitive tasks including reward and event rate manipulations. Neuropsychology. 2011a;25(4):427–441. doi: 10.1037/a0022155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DuPaul GJ, Rapport MD. Does methylphenidate normalize the classroom performance of children with attention deficit disorder? Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32(1):190–198. doi: 10.1097/00004583-199301000-00027. [DOI] [PubMed] [Google Scholar]
- 14.Zentall SS, Smith YN, Lee YB, et al. Mathematical outcomes of attention-deficit hyperactivity disorder. J Learn Disabil. 1994;27(8):510–519. doi: 10.1177/002221949402700806. [DOI] [PubMed] [Google Scholar]
- 15.Shaffer D, Fisher P, Lucas CP, et al. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Wolraich ML, Feurer ID, Hannah JN, et al. Obtaining systematic teacher reports of disruptive behavior disorders utilizing DSM-IV. J Abnorm Child Psychol. 1998;26:141–152. doi: 10.1023/a:1022673906401. [DOI] [PubMed] [Google Scholar]
- 17.Dombrowski SC, Kamphaus RW, Reynolds CR. After the demise of the discrepancy: proposed learning disabilities diagnostic criteria. Prof Psychol Res Pract. 2004;35(4):364–372. [Google Scholar]
- 18.Wolraich ML, Lambert W, Doffing MA, et al. Psychometric properties of the Vanderbilt ADHD diagnostic parent rating scale in a referred population. J Pediatr Psychol. 2003;28(8):559–567. doi: 10.1093/jpepsy/jsg046. [DOI] [PubMed] [Google Scholar]
- 19.Pelham WE. Pharmacotherapy of children With Attention-Deficit Hyperactivity Disorder. School Psychology Review. 1993;22:199–227. [Google Scholar]
- 20.MTA. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Archives of general psychiatry. 1999;56(12):1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- 21.Simmonds DJ, Pekar JJ, Mostofsky SH. Meta-analysis of Go/No-go tasks demonstrating that fMRI activation associated with response inhibition is task-dependent. Neuropsychologia. 2008;46(1):224–232. doi: 10.1016/j.neuropsychologia.2007.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kratz O, Studer P, Malcherek S, et al. Attentional processes in children with ADHD: an event-related potential study using the attention network test. Int J Psychophysiol. 2011;81(2):82–90. doi: 10.1016/j.ijpsycho.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 23.Wright J. [Accessed February 27, 2010];Curriculum-based measurement: A manual for teachers. www.interventioncentral.org/download.php.
- 24.Antonini TN, Narad ME, Langberg J, et al. Behavioral Correlates of Reaction Time Variability in Children With and Without ADHD. Neuropsychology. doi: 10.1037/a0032071. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 26.MacKinnon DP, Lockwood CM, Hoffman JM, et al. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons; 1987. [Google Scholar]
- 28.Schafer JL. Analysis of Incomplete Multivariate Data. London: Chapman & Hall; 1997. [Google Scholar]
- 29.Faraone SV, Biederman J, Spencer TJ, et al. Comparing the efficacy of medications for ADHD using meta-analysis. MedGenMed. 2006;8(4):4. [PMC free article] [PubMed] [Google Scholar]
- 30.Brams M, Muniz R, Childress A, et al. A randomized, double-blind, crossover study of once-daily dexmethylphenidate in children with attention-deficit hyperactivity disorder: rapid onset of effect. CNS drugs. 2008;22(8):693–704. doi: 10.2165/00023210-200822080-00006. [DOI] [PubMed] [Google Scholar]
- 31.Malkovsky E, Merrifield C, Goldberg Y, et al. Exploring the relationship between boredom and sustained attention. Exp Brain Res. 2012;221(1):59–67. doi: 10.1007/s00221-012-3147-z. [DOI] [PubMed] [Google Scholar]
- 32.Wang GJ, Volkow ND, Wigal T, et al. Long-term stimulant treatment affects brain dopamine transporter level in patients with attention deficit hyperactive disorder. PloS one. 2013;8(5):e63023. doi: 10.1371/journal.pone.0063023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barkley RA, DuPaul GJ, McMurray MB. Attention deficit disorder with and without hyperactivity: clinical response to three dose levels of methylphenidate. Pediatrics. 1991;87(4):519–531. [PubMed] [Google Scholar]
- 34.Barkley RA. Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 3. New York, NY: The Guilford Press; 2006. [Google Scholar]
- 35.Hinshaw SP. Moderators and mediators of treatment outcome for youth with ADHD: understanding for whom and how interventions work. Ambulatory pediatrics : the official journal of the Ambulatory Pediatric Association. 2007;7(1 Suppl):91–100. doi: 10.1016/j.ambp.2006.04.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.