Abstract
Vaccines aim to protect against or treat diseases through manipulation of the immune response, promoting either immunity or tolerance. The former generate antibodies and T-cells poised to protect against future pathogen encounter or attack diseased cells such as tumors; the latter, which are far less developed, block pathogenic autoreactive T-cells and autoantibodies that target self tissue. Enormous challenges remain, however, as a consequence of our incomplete understanding of human immunity. A rapidly growing field of research is the design of synthetic materials in vaccines to 1) target organs, tissues, cells, or intracellular compartments; 2) co-deliver immunomodulatory signals that control the quality of the immune response; or 3) directly act as immune regulators, and there exists great potential for well-defined materials to further our understanding of immunity. Here we describe recent advances in the design of synthetic materials to direct immune responses, highlighting successes and challenges in prophylactic, therapeutic, and tolerance-inducing vaccines.
Vaccines can induce the activation of T-cells and B-cells of the adaptive immune system (i.e., cells that recognize and respond to a particular antigen), eliciting the differentiation of these lymphocytes into long-lived memory cells that will rapidly respond if the microbe is encountered in the future. Vaccines were first developed by injecting weakened forms of a live microbe (e.g., a virus or bacterium) that stimulate immune responses without inducing disease, and these “live attenuated” vaccines can induce life-long protective immunity. Often cited as the most effective public health intervention ever developed, successful vaccines have eliminated or dramatically reduced the burden of former epidemics, including smallpox, poliomyelitis, tetanus, diphtheria, and rubella, helping to dramatically increase life expectancy in the developed world over the past century1, 2, 3, 4. However, the future impact of vaccination as a medical intervention extends beyond prophylactic immunization against infectious diseases and the first therapeutic cancer vaccine was recently licensed, in 20105. Parallel advances in cancer immunotherapy treatments that block inhibitory receptors on T-cells, such as the approval of an antibody against cytotoxic T-lymphocyte antigen 4 (CTLA-4) and promising clinical trial results with antibodies against programmed death-1 (PD-1) and PD-L1, are likely to provide additional opportunities to enhance vaccine efficacy in cancer patients5, 6, 7. Vaccines eliciting IgE-blocking, allergen-specific immune responses have shown promise in recent clinical trials for the treatment of allergies8. Intense research is also focused on vaccines that promote tolerance to self-antigens as potential treatments for autoimmune diseases ranging from diabetes to lupus and multiple sclerosis9. Optimism for the potential impact of new vaccine technologies coupled with improved global public health programs led the Bill and Melinda Gates Foundation in 2010 to pledge $10B USD over the next ten years supporting a “Decade of Vaccines” to advance vaccine strategies in the poorest countries of the world.
The enthusiasm over recent successes in vaccine research and development must be tempered by recognizing the significant challenges that remain1, 2. Vaccines against many chronic infections, including human immunodeficiency virus (HIV), malaria, tuberculosis, and hepatitis C, remain major unmet needs. Starting with Jenner’s original demonstration of the concept of vaccination, made before the microbial origin of infectious disease was even established, the majority of licensed vaccines have been developed largely empirically10, and mostly target pathogens with low mutation rates where natural primary infection can drive long-lived immunity in surviving hosts1. These vaccines predominantly drive the generation of neutralizing or opsonizing antibodies, which may not be readily achievable in some diseases. Thus, the translation of advances in cellular and molecular immunology to the design of new vaccines with improved efficacy remains a goal for many vaccinologists.
Rational vaccine design is challenging above all because of our incomplete understanding of the enormously complex human immune system. In most diseases that lack successful vaccines, we often do not know what type of immune response would give the best long-term protection or therapeutic efficacy1, such as the balance of cellular and humoral immunity, the ratio of effector to memory T-cells, the functional properties of activated T-cells (e.g., granzyme or perforin secretion, state of differentiation, and repertoire of cytokines secreted), the breadth vs. strength of specificity, etc. Additionally, even with such knowledge, we lack clear guidelines for how to drive those particular responses. Thus, biomaterials tools should be used more extensively to probe such questions and develop a more quantitative understanding of design principles for vaccinology. Other outstanding challenges include the difficulty of designing antigens that elicit a predefined target antibody or T-cell response, and the substantial limitations of imperfect preclinical animal models4. Indeed, much of our understanding of immunology comes from inbred mouse strains that lack genetic and environmentally-driven diversity and have significant species-related differences in their immune systems compared to humans.
Another major hurdle is eliciting a sufficiently potent immune response while meeting the exceptional safety standards necessary for prophylactic vaccines designed for administration to healthy (often infant) populations. Much of the current effort in vaccine science is focused on developing subunit vaccines composed of molecularly-defined protein, peptide, or polysaccharide antigens that are expected to meet these safety standards. However, purified antigens are typically poorly immunogenic, and must be combined with adjuvants, materials that promote the immune response or directly instruct antigen-presenting cells (APCs) to elicit immunity against the co-administered antigen. It is in the design of adjuvants where materials science and engineering has a second fundamental, and potentially critical, role to play in the future of vaccinology, through the design of new immunostimulatory materials and in the development of delivery systems that can potentiate the immune response for safe and effective subunit vaccines. Until very recently, the only adjuvants approved for use by the US FDA were aluminum salts (collectively termed alum), which were first developed in the 1920’s. However, the explosion in understanding of molecular pathways regulating microbe sensing by the immune system has led to a broad range of new targets for adjuvant design. As we will discuss below, tailored biomaterials offer the prospect of targeted triggering of immune sensors during vaccination combined with control over vaccine exposure kinetics at the tissue and single-cell levels, suggesting the potential for engineering safe and greatly enhanced vaccine responses. These materials also have enormous potential as tools for achieving a better understanding of the complexities of immune regulation. For example, properties such as the precise coupling of antigen or adjuvant; surface features that can promote or prevent protein adsorption or activate complement; sensitivity to endosomal or lysosomal degradation after cell uptake; and size – among others – can all be precisely controlled with engineered materials and their immune outcomes compared.
The advances and challenges described above encompass the four major types of vaccines in preclinical and clinical development (Table 1): Prophylactic vaccines are designed to trigger immunological memory in healthy populations to prevent disease on future exposure, and are often based on the induction of long-lived neutralizing antibody responses. Therapeutic vaccines seek to raise an immune response in the face of ongoing disease (e.g., chronic infections such as HIV or human cytomegalovirus, or cancer). These vaccines must overcome pathogen-mediated evasion of the immune response and will likely require induction of strong cytotoxic T-lymphocyte (CTL; activated CD8+ T-cell) responses to deal with pathogens that have already established intracellular infections. However, the mechanisms for inducing potent effector and memory T-cells while avoiding T-cell depletion, desensitization, or excessive inflammation remain poorly understood1. In the case of cancer, therapeutic vaccines may also need to overcome a variety of suppressive mechanisms employed by tumors, such as immunological ignorance, exhaustion, or tolerance to tumor antigens. The counterparts to vaccines targeting prophylactic or therapeutic immunity are immunizations designed to promote prophylactic or therapeutic tolerance. Tolerizing immunizations aim to induce an immunologic state of unresponsiveness to a foreign antigen (e.g., protein therapeutics or a food allergen) in a naïve individual (prophylactic tolerance), or to induce such tolerance in a patient with ongoing autoimmune disease or allergies (therapeutic tolerance). Each of these settings presents distinct challenges to vaccine development that synthetic materials may be well-suited to help address. In this review, we will describe recent advances in the development of biomaterials that show promise for promoting immunity or tolerance in vaccination; each case is prefaced by a brief discussion of the cellular and molecular mechanisms of the immune system motivating and inspiring the approach.
Table 1.
Challenges in different types of vaccine strategies
| Type | Aim | Example Disease Settings | Challenges | Refs. |
|---|---|---|---|---|
| Immunogenic, prophylactic | Build immune protection against future potential infectious disease to which host is naïve | Successful: smallpox, polio, rubella, human papilloma virus, etc. Not yet successful: malaria, arenaviruses, HIV, hepatitis C virus, filoviruses Evolving: Universal influenza vaccine (multivalents) |
|
Rappuoli, R. et al. (2011)4; Plotkin, S (2005)3; Virgin et al. (2010)122 |
| Immunogenic, therapeutic | Activate potent immunity against pre-existing/chronic diseased cells | Cancer, hepatitis B virus, human papilloma virus |
|
Crow, J. M. et al. (2012)123; Ma, B. et al. (201)124; Klebanoff, C. A. et al. (2011)125 |
| Tolerogenic, prophylactic | Eliminate (or drive immunological ignorance of) lymphocytes specific for a previously unencountered antigen | Cases where early biomarkers of autoimmune disease can be detected before disease onset (e.g., GAD65 antibodies circulating in young children predicts type I diabetes); Therapeutic proteins such as asparaginase, Factor VIII, uricase, or α-glucosidase |
|
Harrison, L. C. (2008)126; Wisniews ki, T. et al. (2010)127 |
| Tolerogenic, therapeutic | Eliminate lymphocytes that are already primed for immunity against a specific antigen | Autoimmune diseases, allergies |
|
Linhart, B. et al. (2012)128; Valenta, R. et al. (2010)8; Harrison, L. C. (2008)126; Sela, M. (2004)129 |
Controlling the context of antigen encounter: Packaging antigen and adjuvant
Synthetic materials have a key role to play in the design of vaccines that exploit evolved pathways by which the immune system recognizes and responds to microbes.
Immunological decision-making: immunity vs. tolerance
The immune system must respond vigorously to dangerous pathogens while avoiding damage to healthy tissue or responses to benign environmental antigens. Therefore, the activation of adaptive immune cells through their surface antigen receptors is tightly controlled, and multiple mechanisms exist to govern their effector, memory, and regulatory functions. B-cells specifically sense antigens via direct binding to B-cell receptors (BCRs), while T-cell receptors (TCRs) recognize peptide fragments bound to self major histocompatibility complex (MHC) molecules displayed on the surface of APCs. T- and B-cells are produced throughout life in the thymus and bone marrow, respectively, and genetic diversity in their antigen receptors is generated by random gene rearrangements to ensure that the host has lymphocytes capable of responding to any pathogen that might be encountered. A process known as negative selection in central tolerance leads to the death of lymphocytes with overt reactivity to self-antigens. However, central tolerance does not eliminate all self-reactive lymphocytes, and thus additional mechanisms (collectively termed peripheral tolerance) control cells in the periphery reactive to self or ‘safe’/abundant foreign environmental antigens. Naïve lymphocytes that receive signaling via their antigen receptor together with a variety of contextual cues develop a fate (e.g., anergy, effector, memory, deletion, etc.) dependent on the integration of these signals. These contextual cues include the cytokines, costimulatory signals, and biophysical cues received by the lymphocyte in tandem with antigen receptor signaling; many of these signals are provided by dendritic cells (DCs), the most potent APC during induction of primary immune responses11, 12 (Fig. 1). DCs distinguish between foreign and self-antigens via a conserved suite of sensor proteins that detect “danger signals,” microbe-associated products with distinct molecular motifs or signatures of cell stress/tissue damage13. This array of sensors is composed of several receptor families, including Toll-like receptors (TLRs), RIG-I-like receptors (RLRs), NOD-like receptors (NLRs), C-type lectin receptors (CLRs) and scavenger receptors (SRs) (Fig. 1). The immune context created by innate immune cells and DCs presenting antigen determines the outcome of prophylactic, therapeutic, or tolerizing immunization; thus a key role for biomaterials as vaccine agents is to help shape this context during vaccination.
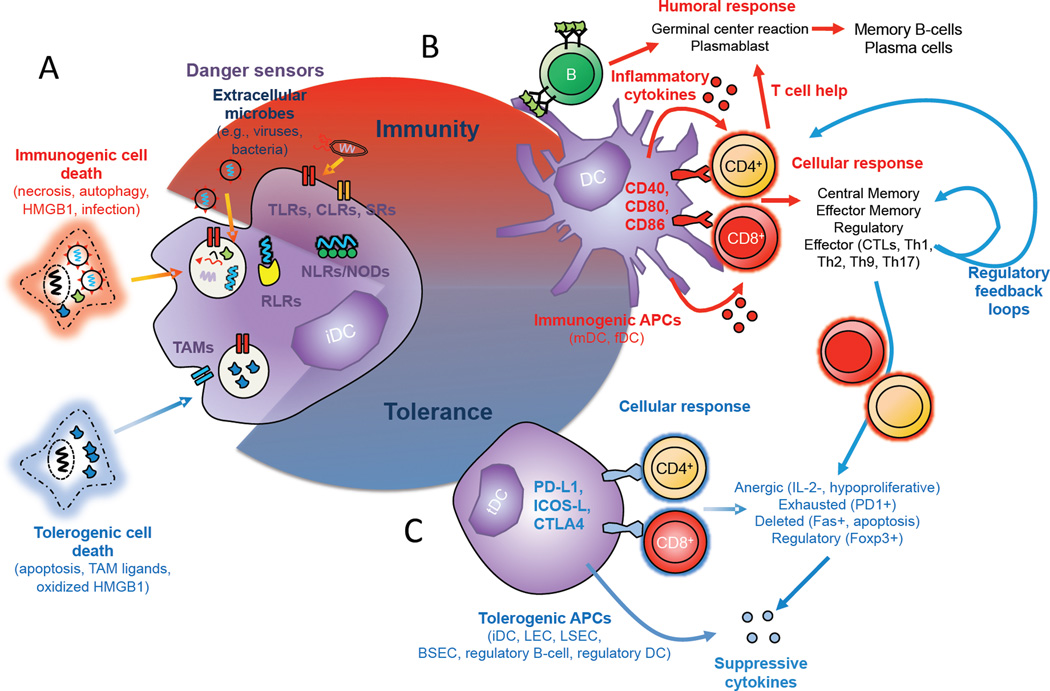
Figure 1. Pathogen sensing by the immune system and immune context during the priming of an adaptive immune response.
DCs are a central interpreter in distinguishing between foreign and self-antigens in the context of microenvironmental cues, and play a major role (along with other innate immune cells) in determining the outcome of antigen recognition by T- and B-cells. A, At steady state, immature DCs (iDCs) throughout the periphery constantly sample their environment and encounter 1) immunogenic signals from infected or immunized, dying cells, accompanied by triggering of danger sensors (TLRs, CLRs, NLRs, RLRs, SRs) or 2) tolerogenic signals from dying self-cells or cellular debris generated by homeostatic turnover; these produce a continuous spectrum of output responses ranging from strong induction of effector phase immunity to strong induction of tolerance, with the exact outcome determined by the integration of inputs by the DC. Pathogen detection occurs via a conserved suite of danger sensors relies on detection of “danger signals,” microbe-associated products with distinct molecular motifs11. Different sensors are present in endosomes (TLRs, SRs), the cytosol (RLRs, NLRs), the ER (SRs) and the plasma membrane (TLRs, CLRs). Each danger sensor recognizes a different motif that is present in a class of microbes but absent from host tissues. In response to these “danger” or tolerizing signals, DCs (and other innate cells) create the immunological context for antigen recognition by secreting cytokines, expressing diverse adhesive, costimulatory or regulatory receptors that provide cues to responding lymphocytes. B, In immunogenic contexts, responding B-cells can subsequently enter germinal centers to undergo somatic hypermutation, become short-lived plasmablasts, or differentiate into long-lived memory B-cells or plasma cells. T-cells can differentiate into effector cells or memory cells with distinct homing and functional capacities; effector cells can have diverse functions (Th1, Th2, Th17, etc.) depending on the context set by DCs. Notably, regulatory feedback loops are engaged even in highly inflammatory contexts, as part of the natural control system regulating immunity, and primed effector cells can be driven to anergic/exhausted states similar to tolerance at later stages of an immune response. C, Peripheral tolerance is maintained by a distinct set of signals, e.g., apoptotic cells that die during homeostatic turnover contain ligands that activate the plasma membrane-expressed Tyro-3, Axl, and Mer (TAM) family receptor tyrosine kinases, inhibiting DC activation and maturation. Many additional APCs also participate in tolerogenic signaling. In tolerogenic contexts, T-cells are driven into several different states of non-responsiveness (anergy, exhaustion, deletion, or regulatory fates) that prevent effector responses against self or harmless environmental antigens.
Microbes: natural micro- and nano-particle targets for the immune system
Interactions of the immune system with pathogens are shaped not only by danger signals, but also the physical nature of microbes, which are biological microparticles and nanoparticles (Fig. 2). The surfaces of many microbes (especially viruses) have dense, multi-copy displays of protein and polysaccharide motifs used to bind to target cells. However, this surface patterning also promotes recognition by B-cells through antigen-specific BCRs. Viruses expressing highly organized, dense arrays of proteins efficiently activate B-cells, while the same proteins expressed at low copy number on the surface of infected cells are ineffective at triggering antibody responses14.
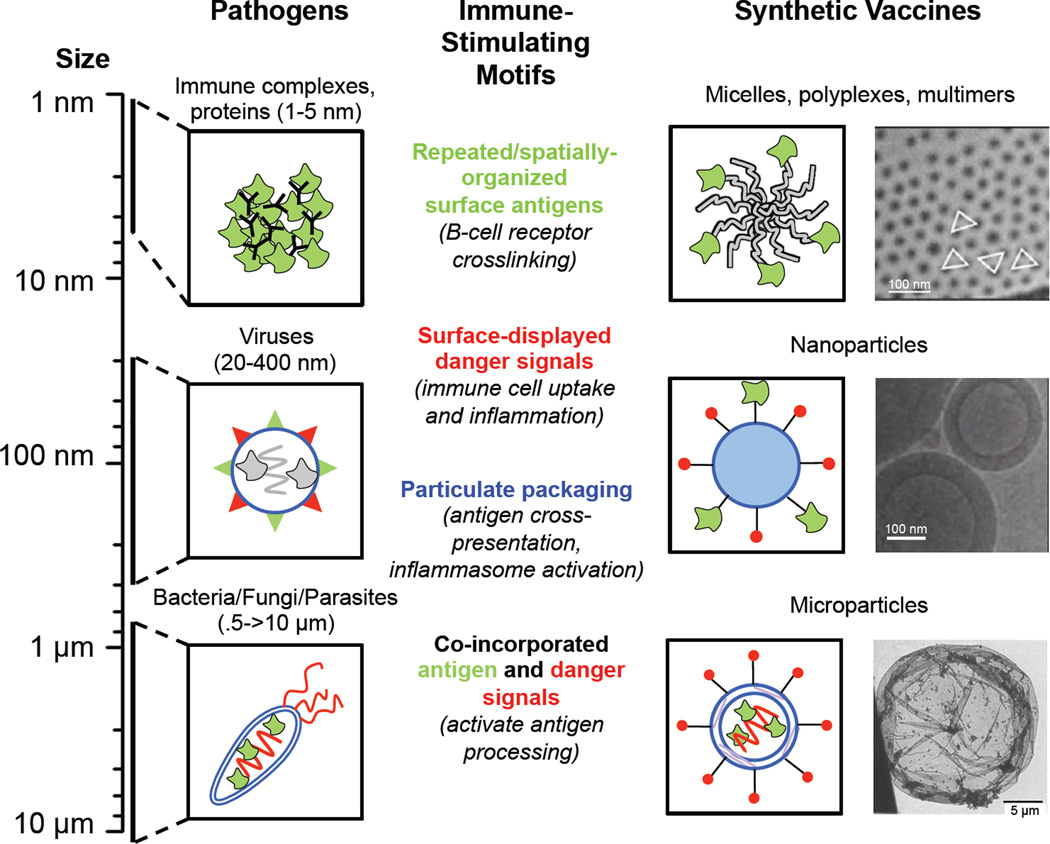
Figure 2. Structural and compositional features of microbes and their mimicry in synthetic biomaterials-based vaccines.
Microbes and microbial products are particulates spanning length scales from tens to thousands of nm in size, with distinct structural and chemical features that are sensed by the immune system. A rich strategy in biomaterials-based vaccines is to design nanoparticles and microparticles that mimic key features of microbes to invoke similar signaling pathways and immune responses elicited by native microbes, without the danger of infection or uncontrolled inflammation.
The particulate nature of microbes is also exploited by the immune system to promote T-cell responses. Soluble antigens endocytosed by DCs from the extracellular environment are typically degraded into short peptides and loaded onto class II MHC molecules that are surveyed by CD4+ helper T-cells. A critical discovery was made by Blander et al. who identified that the decision to present the contents of phagocytosed particulate materials on MHC II molecules depends on the presence of danger signals within the same compartment15. Normally, only proteins in the cytosol of DCs are degraded into peptides that are loaded onto class I MHC molecules. In contrast to soluble antigens, particulate antigens or whole pathogens internalized by DCs can undergo cross-presentation16, where particle-associated antigens are processed and loaded onto class I MHC molecules for CD8+ T-cell activation by a process whose biological mechanisms are still debated. Cross-presentation can be achieved by several cell types, including (most importantly) DCs, as well as (to a lesser extent) neutrophils, macrophages, and blood and lymphatic endothelial cells17, 18. In mice, CD8+ DCs are the most potent subset for cross-priming of T-cells19. However, a recent study of human lymphoid-resident DC populations by Segura et al. demonstrated that, in contrast to blood DCs, all lymphoid-resident human DC subsets (BDCA1+, BDCA3+ and pDCs) had efficient cross-presentation capacity20. Cross-presentation of antigens typically follows their cell uptake by phagocytosis (receptor-mediated uptake for particles ≥500 nm) or macropinocytosis (non-receptor mediated engulfment of particles along with fluid and solute)21. Encapsulation of antigens within synthetic micro- or nano-particles can also promote their capture by APCs and avoid the rapid clearance seen with injected protein antigens22, 23, 24. These findings have motivated the recent focus on development of synthetic nano- and micro-particles as carriers to co-deliver antigen and danger signals to APCs.
New strategies for packaging vaccines in synthetic particles
Synthetic particles surface-conjugated with antigen are especially well suited to triggering B-cells25. On the other hand, encapsulation can lead to much higher quantities of antigen per particle, which is of interest for achieving high intracellular concentrations of antigen in APCs26, 27, 28. Liposomes and particles composed of biodegradable polymers such as poly(lactide-co-glycolide) (PLGA) have been studied for many years as particulate vaccine carriers, but they suffer from multiple limitations, including low levels of entrapped antigen, the potential for damage/denaturation of three-dimensional antigen structures critical for humoral immune responses, and the need for organic solvents in processing.
To address these limitations, several alternative approaches and new materials have been recently explored. Polymer capsules formed via layer-by-layer assembly of polyelectrolytes or disulfide-bonding polymers together with vaccine components onto sacrificial templating microspheres have been shown to promote efficient antigen uptake and presentation by human and mouse DCs in vitro and in vivo29, 30. These particles are multifunctional and allow highly efficient encapsulation of different types of cargo within the core and the layered shell compared to the limited capacity of typical solid polymeric particles. Dierendonck et al. simplified polyelectrolyte capsule fabrication to a cost-efficient, scalable two-step process utilizing spray-drying instead of layer-by-layer deposition, achieving high antigen encapsulation efficiency approaching 85%31. Another major advance in the fabrication of particulate vaccine carriers employs the Particle Replication In Nonwetting Templates (PRINT) process32. This soft lithography approach uses fluoropolymer molds that allow large-scale fabrication of monodisperse nano- and micro-scale particles of diverse morphologies. PRINT is compatible with a wide variety of particulate formulations, including polymeric particles, and a first demonstration of PRINT particles as a delivery system for adsorbed influenza vaccine was recently reported33.
Coordinating antigen and danger signal delivery with synthetic particles
Antigen that is associated with synthetic particles, either via conjugation to particle surfaces or encapsulation in degradable materials, can elicit cross-presentation similar to natural microbial particles (Fig. 2). The first reports of particle-triggered cross-presentation suggested a size dependence to this effect, with optimal cross-presentation triggered by particles ~3 µm in size16, 34, but this is likely system dependent as recent studies of antigen delivery using very small nanoparticles (20–50 nm) have also demonstrated effective CD8+ T-cell priming, with antigen either coupled to the surface27, 28 or encapsulated within35,36.
In addition to facilitating cross-presentation of whole-protein antigens, an important recent advance has been the demonstration in small animal models that synthetic nanoparticles can elicit CD8+ T-cell responses comparable to those induced by strong live microbial vaccine vectors through the co-packaging of antigen and TLR agonists as strong molecular danger signals. Moon et al. developed lipid nanocapsules (interbilayer-crosslinked multilamellar vesicles, or ICMVs) composed of multiple covalently-crosslinked lipid bilayers surrounding an aqueous core37. ICMVs entrapping a protein antigen with the TLR-4 agonist monosphosphoryl lipid A (MPLA) embedded in the capsule walls elicited T-cell responses that could be boosted to levels where nearly 1 in 3 T-cells in the peripheral blood were specific for a single target antigen; this response was dependent on co-delivery of the TLR agonist stably incorporated in the vesicle walls. Nordly et al. also elicited robust CTL responses by developing a colloidally-stable formulation of the TLR-3 agonist poly(I:C) complexed with cationic, gel-state liposomes adsorbed with protein antigen38. CTL responses elicited by this potent lipid nanoparticle vaccine exhibited polyfunctional cytokine secretion and durable memory that could be recalled 10 weeks after immunization. Zaks et al. similarly reported dramatic CD8+ T-cell responses elicited by cationic liposomes complexed with antigen and various TLR agonists39. While it remains to be confirmed whether such vigorous T-cell responses to protein vaccines can be elicited in non-human primates (NHP) or humans, these results demonstrate that appropriate coordination of antigen and inflammatory signals by synthetic particle vectors can dramatically influence the nature of T-cell responses elicited by subunit vaccines.
Notably, vaccines comprised of danger signals co-encapsulated with antigen or loaded in separate particles have both been shown to be effective vaccines. For example, Powell et al. took a direct approach to the incorporation of danger signals by generating a fusion of an immunogenic, designed peptide antigen with the TLR2 agonist Pam3Cys40. The delivery of this fused peptide/danger signal via LbL microparticles formed a synthetic malaria vaccine candidate with enhanced potency and efficacy compared to a traditional vaccine or non-TLR2-containing LbL microparticles. By contrast, Kasturi et al. reported that immunization with antigen and TLR4/7 agonists encapsulated in separate PLGA particles was highly effective at inducing antigen-specific neutralizing antibodies and generated antibody-secreting cells that persisted for 1.5 years post-immunization41. These results are consistent with other prior work demonstrating effective vaccination achieved by adjuvants and antigens delivered in separate particles42. Many other groups have also observed synergistic effects by employing combinations of TLR agonists in particulate vaccines43, 44.
Delivery of molecular adjuvants such as TLR agonists with micro- or nano-particles may enhance their safety, enable the use of more potent adjuvant combinations, or enable small-molecule compounds with poor pharmacokinetics to become useful adjuvants. For example, Tacken et al. demonstrated that the co-delivery of TLR agonists and antigens co-encapsulated in PLGA nanoparticles elicited robust antigen-specific immunity while enabling nearly 100-fold dose sparing of adjuvant, and reduced serum cytokine levels following vaccination relative to an equivalent soluble vaccine45. Alternatively, the enhanced immunologic potency of particle-formulated antigens may allow lower quantities of soluble danger signals to be administered for equivalent immune responses– as illustrated by a study showing that lipid nanocapsule-formulated antigens required 250-fold less MPLA adjuvant to achieve humoral responses equivalent to soluble protein in a malaria vaccine46. Nguyen et al. screened a library of lipid materials for enhanced functional delivery of immunostimulatory RNA (isRNA) adjuvants as lipidoid–RNA nanoparticles (LRNPs)47. Their approach identified materials that formed LRNPs with isRNAs that were distinct from other lipid-based DNA/RNA delivery formulations (e.g., DOTAP, lipofectamine) in their enhanced endosomal retention, tail chemistry-based cell targeting, and robust triggering of cellular and humoral immunity.
Materials-based adjuvancy: self-adjuvanting particles and novel danger signals
The studies cited above have focused on using synthetic materials to deliver molecularly-defined biological danger signals, but an exciting future direction is the design of biomaterials themselves to be direct triggers of danger sensors. Partial motivation for this approach derives from recent advances in understanding the mechanisms of action of the oldest vaccine adjuvant, alum. Alum/antigen complexes have recently been shown to serve as a unique danger signal to DCs, and a receptor-independent, direct interaction has been identified between cell membrane lipids and crystalline compounds such as alum or monosodium urate (MSU, a product released by dying cells following alum injection)48, 49. Alum and MSU interact with membrane lipids, causing receptor aggregation at lipid rafts and recruitment and activation of intracellular kinases. Alum induces abortive phagocytosis and promotes non-phagocytic antigen uptake, leading to endosomal processing and loading onto MHCII molecules. Furthermore, alum-mediated cell death and subsequent host cell DNA release has also been shown to promote Th2 responses and humoral immunity49, 50.
Inflammasome activation is another proposed mechanism of particulate material adjuvancy identified by in vitro studies. Inflammasomes are cytosolic danger sensor complexes51 triggered following endolysosome rupture by these materials52, or indirectly via release of crystalline MSU from stressed/dying cells50, 53. In the case of alum, it has been shown that inflammasomes are dispensable for alum’s adjuvancy in vivo, which instead seems to operate through the direct membrane interactions discussed above. Polymeric particles (e.g., PLGA and polyethylene glycol (PEG)-poly(propylene sulfide)54) have recently been shown to serve as direct activators of the inflammasome in DCs. However, there is little evidence yet that inflammasome activation impacts the humoral response to particulate vaccines, and the role of inflammasome activation in the T-cell response is still unclear55, 56. The inflammasome-triggering ability of materials internalized by innate immune cells may be a general response to internalization of particulates, as it has been observed in vitro with alum, silica, polystyrene particles, polymeric multilayer capsules57, and PEG-poly(propylene sulfide) nanoparticles54. Synthetic particles may also trigger additional processes in antigen presenting cells that impact immune responses: Li et al. recently demonstrated that tumor antigen delivery by α-alumina nanoparticles resulted in immune activation and presentation via induction of autophagy in DCs, a process where cells degrade and recycle their intracellular components within specialized vesicles58. Autophagy resulted in robust cross-presentation and T-cell priming that was able to eradicate established subcutaneous melanoma when delivered as a therapeutic vaccine.
Another strategy to activate danger sensors with biomaterials is via the design of materials that trigger complement or other innate sensing responses in vivo. This approach was first demonstrated with poly(propylene sulfide) nanoparticles stabilized by poly(propylene oxide-b-ethylene oxide) block copolymers. These nanoparticles displayed a PEG corona with hydroxyl chain ends that activated complement, providing an intrinsic danger signal to effectively adjuvant the response to antigen tethered to the particle surfaces27. A follow-up study by Thomas et al. demonstrated the potential to fine-tune complement activation by manipulating particle design parameters including core thiolation, surface charge and surface carboxylation59.
Some materials have been identified with adjuvant properties where the specific mechanism of action remains unknown. Hydrophobicity is a property that has been proposed to dictate the adjuvancy of synthetic polymers and moieties of some microbial danger signals. For example, a systematic series of gold nanoparticles with organic ligand shells of increasing hydrophobicity elicited expression of inflammatory cytokines by splenocytes proportional to particle hydrophobicity60. Petersen et al. recently demonstrated that the activation of innate immune responses by pathogen-mimicking nanoparticles was significantly influenced by polymer hydrophobicity and polar/hydrophobic moiety patterning61. Hydrophobicity has also been shown to affect particulate uptake62. Another example of materials with intrinsic adjuvant properties comes from work by Rudra et al., who recently demonstrated strong class-switched, apparently T-cell-independent antibody responses induced by peptide antigens fused to amino acid sequences that form self-assembling fibrils in vivo. These fibril-forming vaccines might act as depots of antigen, be recognized by known or unknown danger sensors, or act through novel mechanisms to drive the immune response63. Further exploration of such novel routes of adjuvant action may lead to new strategies for adjuvant development that move beyond the well-established classical adjuvants and established danger signal pathways.
Delivering antigens and tolerogenic signals
Using many of the same design principles employed for immunizing vaccines, researchers are also developing prophylactic and therapeutic vaccine strategies that can drive antigenic tolerance. Using danger signal-free synthetic microparticles coupled to immunogenic myelin epitopes, Getts et al. successfully generated protective and therapeutic tolerance in an animal model of multiple sclerosis64. In this study, inert polystyrene and PLGA beads were used to mimic the known tolerogenic properties of apoptotic cells. The authors found that tolerance was dependent on 500-nm particle size, covalent linkage of the peptide antigens, and i.v. administration, which resulted in delivery to splenic marginal zone macrophages. Interestingly, tolerance was induced in a multi-faceted manner that included Treg activation, abortive T-cell activation, and T-cell anergy. Lewis et al. have also shown that antigen-carrying particles can be functionalized with ligands for DC-specific receptors to enable targeting of tolerogenic antigen to DCs with inducing DC activation65.
Many groups are pursuing strategies to induce tolerance by co-delivery of small molecule drugs with antigens. Recently, Yeste et al. utilized a PEGylated gold nanoparticle vehicle for co-delivery of the model autoimmune-inducing antigen MOG and a tolerogenic small molecule drug targeting the aryl hydrocarbon receptor, which is implicated in tolerogenic signaling in DCs66. They demonstrated profound induction of tolerogenic DCs that primed increased numbers of CD4+ regulatory T-cells, and these regulatory cells alleviated antigen-induced autoimmune encephalitis. They also demonstrated that co-delivery of the antigen and small molecule together was necessary to achieve maximum therapeutic efficacy.
In a very different approach, Tsai et al. designed self-peptide-MHC-coated iron oxide nanoparticles (pMHC-NP) with the goal of treating autoimmune type I diabetes (T1D) by tolerizing disease-specific CD8+ T-cells67. These particles can bind to T-cell receptors and provide direct signaling to T-cells independent of APCs. Their results were robust and unexpected, demonstrating that pMHC-NPs were therapeutic in a murine model of T1D by expanding a memory subset of low-avidity regulatory CD8+ T-cells instead of directly tolerizing T1D-specific T-cells. The existence of this pool of regulatory cells and their ability to expand in response to pMHC-NP without co-stimulation were novel immunologic findings. The therapeutic efficacy of pMHC-NP was thus attributed to expansion of regulatory cells that mediated both direct suppression of other T-cells and killing of autoantigen-presenting DCs. This mechanism has promising therapeutic potential because these regulatory T-cells are able to suppress autoimmune responses against multiple potential auto-antigens by acting at the level of the DC.
Kinetics and biodistribution of vaccine exposure in priming immunity
The immune response to vaccination is a function of a given formulation’s spatiotemporal profile, with the timing and localization of antigen and danger signals dictating qualitative and quantitative aspects of vaccine-induced immunity.
Kinetic patterns of antigen availability and inflammation shape the response to infections and vaccination
Antigens and appropriate adjuvant signals provide the context for a developing immune response, but the timing of exposure of the immune system to these signals can be as important as the choice of vaccine components in generating the desired quality and magnitude of response. The role of antigen and inflammation kinetics in shaping the immune response is perhaps best typified by considering natural acute vs. chronic infections: Acute infections are often characterized by brief bursts of antigen production and inflammation induced from infected cells, which may persist initially, but decay over the course of ~1–2 weeks coinciding with the induction of the primary immune response and clearance of the pathogen68. Such brief (albeit potentially strong) exposure to antigen and inflammatory cues can be accompanied by massive clonal expansion of T-cells, robust generation of affinity-matured antibodies, and development of long-lasting memory T-cell and B-cell populations. By contrast, in chronic infections where antigen and inflammation are persistently produced over months or years without effective clearance by the immune response, defective lymphocyte memory, T-cell “exhaustion”, and failure of immune effector functions ensues68, 69. This may reflect the pathogen confusing the immune system by mimicking the continuous antigen exposure of self-antigens, which normally drives tolerance.
Notably, these patterns of natural antigen/inflammation exposure during infection are quite distinct from the relatively brief exposure of lymph node cells to antigen and adjuvant molecules following traditional bolus subunit vaccine injection, where vaccine components carried by lymph are flushed through the lymph nodes within hours, and migrating DCs from the injection site traffic antigen for only 1–2 days70, 71. In vaccination, giving the same immunization with different kinetic patterns (achieved by repeated injections of varying vaccine doses over time) has been shown to dramatically alter the strength of CD8+ T-cell responses to peptide vaccines: administration of exponentially increasing doses of peptide and adjuvant injected daily over the period of one week gave much stronger T-cell responses than a single-timepoint bolus injection, steady low-dose administration, or an exponentially-decaying administration pattern of the same total vaccine dose72. Antigen exposure kinetics are equally crucial at the single-cell level within APCs. Studies of antigen processing have shown that proteins are selected for antigen presentation with APCs during a very narrow window of time following internalization into endolysosomal compartments73, suggesting that antigens that are released from endolysosomally localized particle carriers after a few hours may be too late to contribute productively to antigen presentation.
Importantly, factors such as vaccine particle size, route of administration, and even surface chemistry can affect the exposure kinetics via control of physiological trafficking to various tissues and cells as well as intracellular compartments. While there is growing appreciation that these variables significantly affect the quality and magnitude of the immune response, there remains little understanding of the underlying mechanisms at play. These issues are discussed below.
Delivering vaccines into target tissues
The first step in immunization is the deposition of a vaccine into a target tissue; synthetic materials are being developed to enable vaccine delivery through noninvasive routes (skin, oral administration) and to promote vaccine uptake through mucosal surfaces (airways, gastrointestinal and reproductive tracts). Materials that are capable of protecting antigens in transit through the stomach and gut for oral vaccination have long been sought74, but poor uptake efficiency75 and the potential for antigens encapsulated in solid degradable polymers to be degraded76 have remained substantial hurdles to oral vaccine development. Recently, promising results with a two-stage oral delivery system based on antigen and adjuvant-loaded PLGA nanoparticles encapsulated within microspheres composed of a pH-responsive Eudragit poly(methacrylic acid) copolymer were reported77. The Eudragit microspheres served as a protective carrier that selectively dissolved only within the above-neutral pH conditions of the terminal ileum, releasing the antigen-carrying nanoparticles where they could be taken up across the intestinal epithelium. This two-stage system promoted T-cell and humoral responses that were protective against mucosal challenge with recombinant vaccinia virus in mice. Targeting of particles to antigen-transcytosing M cells overlying Peyer’s patches in the gut via antibodies or M cell-specific ligands may provide additional avenues to further enhance vaccines delivered to the GI tract78.
Materials are also being developed to promote vaccine delivery through the skin, and here many exciting advances have come in the area of microneedle skin patches designed to perforate the outer layers of the stratum corneum and painlessly deposit vaccines in the epidermis and/or upper dermis. Microneedles composed of polyvinylpyrrolidone polymerized in situ in molds in the presence of an inactivated influenza vaccine allowed the formation of dissolving vaccine-loaded skin patch arrays that promoted enhanced protection of mice from influenza challenge when compared to a traditional intramuscular syringe vaccination79. Because the micro-needles quickly dissolve upon application to the skin, these patches are strong candidates for self-administrable vaccines that would have no associated biohazard waste. Dissolving microneedles have also been demonstrated to potently deliver synthetic nano/micro-particle vaccines into skin80. A second recent advance has been in the development of silicon microneedle arrays that are geometrically designed to optimally penetrate to precise depths to release coated vaccines within the epidermal layer, where Langerhans cells (the key DCs of the skin) reside81. Finally, the ability of microneedles to carry and release complex vaccine formulations may enable currently ineffective vaccine strategies to achieve potency. DeMuth et al. recently described an approach for “polymer multilayer tattooing,” where microneedles coated with a quick-releasing polyelectrolyte multilayer coating deposit these vaccine-loaded films into skin, where they release DNA and adjuvants over a tunable time period, thereby greatly enhancing immunogenicity and achieving immune responses comparable to the current gold-standard process known as in vivo electroporation82.
Vaccination through mucosal surfaces is of great interest to promote protection at key portals of pathogen entry, but the mucus barrier that lines the airway, gastrointestinal, and reproductive tract mucosa is a formidable barrier to vaccine absorption. Mucus is composed of fibrous bundles of mucins, large, highly glycosylated proteoglycans comprising hydrophobic protein backbones decorated by a dense brush of short anionic polysaccharides; mucus gels range from very thin layers up to 800 µm thick in portions of the gut83, and are designed to entrap and remove particulates and microbes. Aqueous pores in the physical gels formed by mucin fibers have been estimated to be ~340 nm in diameter, but particles much smaller than this mean size can be efficiently captured by the mucin strands84. The high negative charge of the gel traps any positively-charged particle, while providing an electrostatic barrier to partitioning of negatively-charged particles. Finally, particles with exposed hydrophobic patches are efficiently captured by the hydrophobic domains of the protein backbones of mucin chains. However, recent studies have revealed that synthetic particles as large as 500 nm in size are capable of rapid diffusion through mucus by employing dense PEG coatings to simultaneously mask hydrophobic surface patches and provide near-neutral net surface charge85, 86–thus mimicking the charge-neutral surface chemistry of mucus-penetrating viral particles. These mucus-penetrating surface chemistries enable vaccine- and drug-loaded polymer particles to penetrate to the epithelial surfaces in the lungs26 and the reproductive tract87, 88. Mucus-penetrating particles may enable vaccines to be delivered to mucosal DCs prior to elimination by mucociliary clearance mechanisms. For delivery to nasal mucosa, Nochi et al. demonstrated an alternative approach based on amphiphilic pullulan polymers that self-assembled with protein antigens into cationic nanogels. These cationic nanoparticles adhered tightly to the nasal mucus/apical epithelial membranes for up to 2 days (compared to soluble antigen that was cleared from the nasal passages within hours), enabling antigen to be more effectively captured by nasal DCs and promoting robust Clostridium botulinum or tetanus-neutralizing antibodies89. Because vaccination at mucosal sites often promotes mucosa-localized memory/plasma cells much more efficiently than does parenteral immunization, these approaches have great promise for enhancing protection against a variety of respiratory, reproductive tract, and gastrointestinal pathogens.
Size of subunit vaccines
The size of an injected particulate affects its physiological tissue distribution and kinetics, cellular distribution (e.g., within the draining lymph node), cellular uptake by APCs, and intracellular processing pathways (Fig. 3), thereby strongly influencing the quality and quantity of the immune response it elicits. Within the interstitial (or extravascular) space, where particulate material is introduced either by injection or by extravasation (e.g., in tumors with leaky blood vessels), particles can both diffuse and convect. The Peclet number (Pe) represents a ratio of convective transport to diffusion for a given situation; when Pe > 1, fluid convection – which is driven in the interstitium by lymphatic drainage caused by a pressure gradient between the blood and lymphatic vessels – and its associated convective forces dominate particle transport. However, both interstitial diffusion and convection are hindered by the architecture of the extracellular matrix. For moderately sized proteins (e.g., 69 kDa albumin with a hydrodynamic radius of ~3.5 nm and diffusion coefficients measured in the range of 40–110 µm2/s depending on the tissue), convection begins to become more important compared to diffusion in average interstitial flows of ~0.1–1 µm/s90. For typical 20–50 nm nanoparticles, convection likely dominates interstitial transport in most tissues; larger particles are sterically hindered by the extracellular matrix and mostly convect along heterogeneous fluid channels.
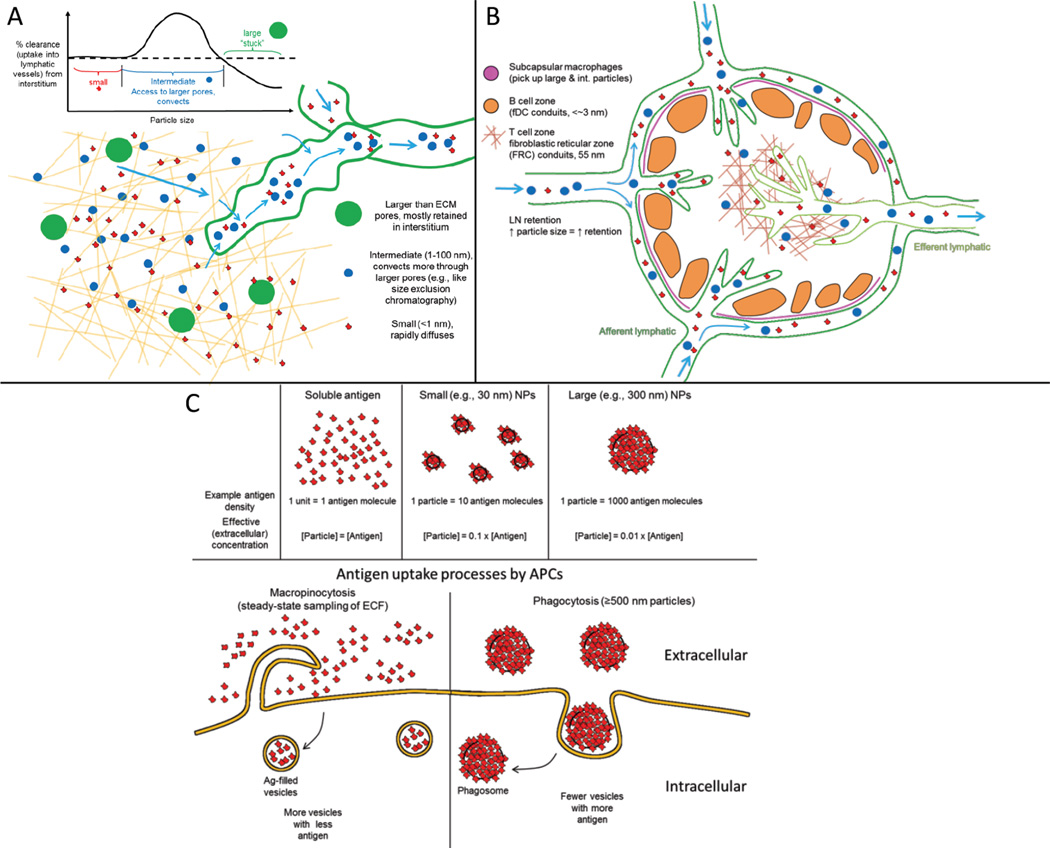
Figure 3. Effects of particulate size on tissue, cell, and intracellular targets after entry into interstitial tissue.
A, After injection into the interstitium (i.e., intramuscular, intradermal, subcutaneous, etc), particles (whose definition here includes molecules) will disperse and convect with interstitial flow, driven by transient pressure gradients that arise from the injection as well as the natural small pressure gradient between blood and lymphatic capillaries. Very small particles (red), whose diffusion velocity is greater than convective velocity, can readily diffuse and will rapidly dilute in local concentration, which limits the effective lymphatic concentration. Larger, intermediate-sized (blue) particles have smaller diffusion speeds and furthermore are transported within the more permeable regions of the ECM (as in size-exclusion chromatography), and thus their transport is governed more by convection and they are more efficiently directed into the lymphatic vessels. However, as size increases, steric hindrance becomes limiting, and particles that are too large (~ >500 nm although this depends on tissue, level of hydration, and experimental conditions) remain mostly trapped in the interstitial space. B, Once inside the lymphatic vessel, lymph node retention positively correlates with particle size. Larger (or opsonized) particles are readily taken up by subcapcular macrophages, while intermediate-sized particles can directly access the T cell zone and associated DCs. The B-cell zone conduits, however, which are formed by follicular dendritic cells, restrict access to particles <~3 nm. C, Size also affects antigen concentration and dose upon intracellular uptake by the APC. If the antigen is a free protein, then the effective “particle concentration” is equal to the antigen concentration, and this is also equal to the concentration within macropinocytotic vesicles after uptake. However, if antigen is adsorbed or incorporated into a nanoparticle, then the concentration of antigen “units”, or particles, is less than the antigen concentration by the number of antigen molecules adsorbed per particle. Larger particles of e.g., 250 nm can contain 1000 antigen molecules per particle, and thus reduce the effective antigen concentration 1000-fold. On the other hand, upon uptake, antigen should be 10-fold or 1000-fold more concentrated inside the phagosome when taken up in nanoparticulate form vs. free antigen form. It is unknown how such differences in antigen delivery (i.e., more vesicles with fewer antigens each vs. fewer vesicles with more antigens each) affect cross-presentation efficiency.
Convective flows sweep macromolecules and particles from the interstitium into lymphatic vessels that carry them to the lymph node. Lymphatic targeting has been shown to be optimal for particles in the size range of 10–50 nm27, 91; particles above this size can still enter lymphatic vessels, but do so at a rate that decreases with increasing particle size due to interstitial hindrance. Small molecules (<2 nm) may also access blood vessels, although their solute permeability is lower than that of the interstitium. Thus, nearly all injected macromolecules and nanoparticles in the 10–~50 nm size range will leave the interstitial space of healthy tissues via lymphatic drainage.
Once inside lymphatic vessels, particles are transported to the lymph node where the larger particles are taken up by subcapsular macrophages and smaller particles or molecules can enter the B- or T-cell zones via conduits (formed by follicular DCs or fibroblastic reticular cells, respectively) or the lymphatic sinuses. Some particles will not enter the lymph node, instead remaining in the subcapsular sinus and leaving via the efferent lymphatic vessel. The term “lymph node retention” refers to the relative fraction of entering solute that remains in the lymph node (presumably taken up by resident cells), although this is a kinetic phenomenon. In general, particles of increasing size show increasing lymph node retention once inside the lymphatics, but target subcapsular macrophages more readily, while smaller particles can rapidly enter B- and T-cell zones for uptake by B-cells and DCs24.
Within a few hours after injection, nanoparticles can be seen in the systemic circulation (to which they eventually drain), peaking in concentration at ~12 h post-injection23. There, they may concentrate in the spleen as well as liver, kidneys, and lungs. A recent biodistribution study demonstrated that after intradermal injection of 25 nm polymeric nanoparticles, total accumulation of particles in leukocytes within the draining lymph nodes peaked after 1 h, while peak accumulation in DCs, monocytes, and B cells occurred between 6–24 h. In contrast, splenic accumulation in all cell types peaked at 24 hours with a striking affinity for Ly6c+ monocytic cells, particularly in tumor-bearing mice23.
As discussed above, cellular uptake and processing pathways are also size-dependent. Antigens that are in particulate form (including micro- and nano-sized carriers, exosomes, and proteins complexed with heat-shock proteins) are more likely to be processed through cross-presentation pathways than those that are in free protein form. In terms of dose, however, it should be considered that attaching antigens to particles leads to localized antigen concentration with a smaller effective concentration relative to soluble antigens, considering “concentration” as the number of antigenic particles (or molecules) per volume (Fig. 3C). This factor should be considered when comparing immune responses to equivalent antigen dose of free vs. particle-bound antigen since the effective “concentration” (i.e., outside the cell) of particle-bound antigen is equal to the antigen concentration divided by the number of antigen molecules per particle. Overall, however, the improved targeting and processing pathways of antigens in particulate forms permits lower antigen doses with particle-bound antigen. Numerous studies have demonstrated that particulate forms of antigen drive stronger immune responses than free antigens when co-delivered with the same adjuvants, thus reducing the required antigen dose22, 27, 37, 46, 63, 92, 93.
Vaccine targeting at the single-cell level
At the single-cell level, synthetic materials can also regulate vaccine delivery by controlling the intracellular timing and location of antigen/danger signal release following vaccine uptake by APCs. Murthy and Frechet first demonstrated engineering of the timing of intracellular antigen release from synthetic particles by designing antigen-loaded hydrogel particles crosslinked by acetal linkages that were stable at neutral pH but acid-labile, providing rapid degradation and antigen release within the acidic endolysosomal compartments of DCs93. Rapid breakdown of these gel particles into soluble polymer fragments simultaneously provided an osmotic driving force for rupture of the endosomes and release of the freed antigen into the cytosol, promoting cross-presentation of antigen to CD8+ T-cells. More recently, a variety of examples of endosome-disrupting polymer particles and vesicles that release antigen into the cytosol have been reported, which are triggered by the acidic conditions of the endolysosomal pathway94, 95, 96, 97. the reducing conditions of the endosomes36, or external light cues98. It has also been shown that antigen-releasing PLGA nanoparticles internalized by DCs can continuously release antigen within cells, thus providing an intracellular store that prolongs antigen presentation over several days, enhancing CD8+ T-cell priming99. Confocal microscopy suggested that some particles are not localized in acidic endolysosomal compartments and antigen was detected directly in the cytosol, explaining these enhanced T-cell responses. In the realm of nucleic acid-based vaccines, Geall et al. recently reported a cationic PEGylated liposome system for intracellular delivery of self-replicating mRNA-based vaccines, which achieved dramatically enhanced potency relative to naked mRNA or DNA injections100. As cytosolic delivery is a key objective broadly in drug delivery, other novel materials developed for nucleic acid delivery (reviewed elsewhere in this issue) and additional cytosolic access strategies (e.g., cell-penetrating nanoparticles101) may be of future interest for regulating the entry of antigen into cells. In addition, controlling the kinetics of molecular adjuvant delivery into the cytosol could open up many recently discovered intracellular danger sensors (e.g., NLRs and RLRs13, 51) as viable targets for vaccine immunomodulation.
Regulating antigen exposure kinetics with synthetic vaccine materials
The application of synthetic materials as controlled release vehicles to regulate the kinetics of vaccine exposure was appreciated in the earliest studies of vaccines, and the first synthetic vaccine adjuvant alum was long believed to act mainly as a slow-release source of antigen, though more recent studies suggest that alum is not an effective “depot” for many antigens and that sustained antigen release over time is not important for the immune response to this adjuvant102, 103. However, the development of controlled-release polymer matrices and particles that definitively provide continuous release of antigen over periods of weeks to months demonstrated the ability of slow-release formulations to robustly promote the humoral immune response104, 105, 106. Gupta et al. in particular showed that antibody responses against tetanus toxoid released from large (~50 µm) PLGA microspheres over more than 1 month in vivo elicited robust toxin-neutralizing antibodies, while the same “empty” microspheres mixed with soluble antigen (controlling for possible inflammatory/APC-activating actions of the microspheres themselves) elicited no response104. Three points of note about these early studies are that (1) they generally focused on designing materials to achieve sustained release of antigen over a period of many weeks with the objective of obtaining single-shot vaccines that do not require boosting, though this pattern of antigen exposure may better mimic the setting of chronic infection that tends to ablate T-cell responses; (2) early slow-release vaccines were generally developed without the explicit addition of inflammatory molecules, and thus the type and kinetic pattern of inflammation induced by these vaccines is poorly understood; and (3) often only humoral immunity was analyzed in response to these sustained-antigen release vaccines (and typically only antibody titers). In regard to the second point, Hailemichael et al. showed that long-lived antigen depots formed by mixing peptide vaccines with incomplete Freund’s adjuvant lead to T-cell deletion rather than expansion in the absence of an added inflammatory signal (e.g., TLR agonists)107.
Recently, the impact of regulating the kinetics of inflammatory adjuvant exposure rather than antigen were explored through intranodal injections of PLGA microspheres releasing the TLR-3 agonist polyI:C108. These experiments showed that both T-cell and antibody responses were substantially amplified by persistently exposing lymph node cells to adjuvant over the course of 5–7 days, as opposed to bolus injections where the adjuvant was cleared within hours; this effect was mediated by sustained levels of DC activation in the LNs over time. Cytokines have also been explored as adjuvants in vaccines, and these molecules also typically have very short half-lives (~minutes) following parenteral injection. St. John et al. demonstrated a biomimetic approach to controlling cytokine delivery in vaccination, by packaging tumor necrosis factor-α (TNF-α, a prototypical inflammatory cytokine) in zwitterionic heparin/chitosan polyelectrolyte complexes, ~400 nm diam. nanoparticles mimicking the inflammatory granules released by mast cells within minutes of stimulation in inflamed tissues109. These mast-cell mimics deposited in lymph nodes and exhibited a ~24-hour release of cytokine in vitro, presumably promoting sustained exposure in vivo. Nanoparticle-TNF delivery promoted a “Th1”-like immune response (associated with better protection in many disease models such as cancer110 and Leishmania infection111) and protection by a model influenza vaccine. Increased exposure of draining lymph nodes to vaccines is also likely achieved by other particulate vaccine carriers that are transported through lymph to deposit in the subcapsular sinus or diffuse into the lymph-filled conduits of the node, where they may deposit and act as local depots of antigen and/or inflammatory signals for days to weeks27, 46.
In an approach designed to regulate the kinetics of multiple steps in the immune response, Ali et al. employed biodegradable polymer scaffolds that released the cytokine granulocyte/macrophage colony stimulating factor (GM-CSF) to attract and differentiate DCs, CpG DNA to activate the resulting DCs, and tumor antigen to load the activated DCs and drive an anti-tumor immune response112, 113. Greatly enhanced anti-tumor immunity was generated by this strategy when compared to bolus injection of the same vaccine components112. In a related approach, Singh et al. demonstrated the ability of in situ-crosslinking hydrogels carrying chemokines, plasmid DNA, and siRNA-loaded microparticles, to attract DCs, modulate their cytokine signaling, and drive a Th1-biased immune response to plasmid-encoded antigens114. Altogether, these data suggest that the kinetics of antigen and inflammatory signal exposure may be equally important in controlling the immune response during vaccination, and that sustained exposure to inflammatory signals over at least ~1 week enhances both T- and B-cell responses to subunit vaccines.
Outlook
Although great successes have been achieved over the last two centuries in vaccinology, enormous challenges remain, both in our understanding of what type of immune response is needed for fighting many diseases as well as how to generate those specific responses. Most of the diseases that have no available vaccine present challenging immunological problems, such as in chronic infections or cancer where natural immunity fails or in autoimmune diseases where natural tolerance mechanisms fail. The studies summarized here illustrate how synthetic materials can be used as adjuvants or delivery systems to amplify, regulate, or qualitatively alter vaccine immune responses. Additionally, these materials provide tools for further understanding the basic mechanisms controlling immunity. What are the key challenges ahead? One important issue is the evaluation of more materials-based vaccine concepts in non-human primate (NHP) models and humans. Small animal models are important tools for proof-of-concept studies, but often fail to predict the efficacy of vaccine concepts in NHPs and humans115, 116. For example, no vaccine strategy to date has demonstrated the ability to robustly induce CD8+ T-cell responses to protein vaccines in large animal models. If the promising cross-priming of CD8 responses triggered by nanoparticle vaccines in small animals is replicated in NHPs, this would represent a major advance for vector-free vaccine development. Currently, few nanoparticle/microparticle or materials-adjuvant-based vaccines have been tested in NHPs or clinical trials, though the data generated from initial studies are encouraging41, 117, 118, 119. The next few years will see many additional concepts undergo advanced preclinical and early clinical testing through the numerous startup and early-stage biotechnology companies pursuing commercialization of these technologies (Table 2).
Table 2.
Biomaterials-based vaccine technologies in commercial development
| Company | Materials/Technology platform |
Disease indications | Development phase |
|---|---|---|---|
| Vedantra Pharmaceuticals | Crosslink-stabilized lipid nanocapsules | Malaria, HPV | Preclinical |
| CSL Limited | ISCOMATRIX saponin derivative/cholesterol/lipid nanoparticles | HPV, HCV, influenza | Phase 1 |
| Isconova | ISCOM-based Matrix platform, saponin derivative/ cholesterol/lipid nanoparticles | Influenza, malaria, rabies, HSV-2 | Phase 1 |
| Liquidia Technologies | PRINT process for monodisperse particles | Influenza, pneumonia | Phase 1 (influenza, elderly) |
| NanoBio Corporation | Nanoemulsion of bacterial spores | Influenza, trivalent influenza RSV, hepatitis B virus, anthrax, Smallpox | Phase 1 (influenza) |
| NanoTherapeutics, Inc. | GelVac self-gelling polymer plant polysaccharide powders | Influenza, typhoid, norovirus, HIV | Phase 1 (H5N1 influenza) |
| Selecta Biosciences | Targeted polymer nanoparticles | nicotine, malaria, type 1 diabetes, food allergy | Phase 1 (nicotine) |
| Novavax, Inc. | RSV-F micelles | Respiratory syncytial virus (RSV), influenza, rabies | Phase 2 (RSV, influenza) |
| Pevion Biotech AG | Virosome (cell-free lipid/protein self-assembling influenza-like liposomes) | Recurrent vulvovaginal candidiasis, RSV, malaria, HIV, hepatitis C virus | Phase 1 (RVVC, HIV, hepatitis C virus), Phase 2 (malaria) |
| Vical, Inc. | Cationic liposomes, Lipid/DNA poloxamer | HSV2, HIV, dengue | Phase I (Dengue), Phase 2 (HIV) |
| Crucell (Johnson & Johnson) | Virosomes | Aluminum-free hepatitis A virus, rabies, influenza | Approved (aluminum-free hepatitis A virus, Epaxal; influenza, Inflexal V) |
| GSK | “Adjuvant System” family of vaccine adjuvants, including liposomal monophosphoryl lipid A/saponin derivative QS21 (AS01B), oil-in-water emulsion with MPLA/QS21 (AS02A), MPLA adsorbed on alum (AS04) | Tuberculosis, malaria, HIV, HSV, HPV | Phase 1 (tuberculosis, HIV), Phase 3 (malaria), Approved (HPV) |
| Novartis | MF59 oil-in-water nanoemulsion; mRNA replicons in cationic liposomes | MF59, many infectious diseases; liposomal replicons initial focus on RSV | Approved (influenza, Europe); Preclinical (liposomal replicons) |
A second challenge for the growing field of immuno-biomaterials engineering is to begin analyzing in deeper detail the qualitative features of immune responses triggered by advanced materials that modulate cellular/tissue targeting, innate immune stimulation, and vaccine kinetics. Moving beyond simply aiming for greater expansion of antigen-specific T-cells and higher antibody titers to the critical questions of immune functionality (e.g., what functions do these T-cells have? What is their avidity? What epitopes are recognized by elicited antibodies? What degree of somatic hypermutation have they undergone?) will be an important step in determining the ultimate impact of synthetic materials in vaccine design. It is becoming increasingly clear that qualitative features of the immune response, such as the polyfunctionality and avidity of T-cells, glycosylation and subclass of antibodies, and the degree of affinity maturation of antibodies, can have a major impact on the effectiveness of vaccines120, 121. There exists little understanding of how vaccines can be designed to impact these qualitative features of immune responses, and biomaterials can play a key role in providing controlled systems to stimulate the immune system and determine what molecular levers must be pulled, how hard, and when, in order to direct the immune system to the desired state of memory. Answering these questions will be an exciting challenge at the interface of materials science and immunology in the coming years.
ACKNOWLEDGMENTS
This work was supported in part by the Ragon Institute of MGH, MIT, and Harvard, the Gates Foundation, the Dept. of Defense (contracts W911NF-13-D-0001 and W911NF-07-D-0004, T.O. 8), and the NIH (AI095109 and AI091693). D.J.I. is an investigator of the Howard Hughes Medical Institute. Funding was provided by the Bill and Melinda Gates Foundation and Carigest SA (to M.A.S.).
Footnotes
AUTHOR CONTRIBUTIONS
D.J.I., M.A.S., and G.L.S. wrote the paper.
COMPETING INTERESTS
D.J.I. is an inventor on patents licensed to Vedantra Pharmaceuticals, Inc., in which D.J.I. holds equity and is a co-founder.
References
- 1.Germain RN. Vaccines and the future of human immunology. Immunity. 2010;33:441–450. doi: 10.1016/j.immuni.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 2.Pulendran B, Li S, Nakaya HI. Systems vaccinology. Immunity. 2010;33:516–529. doi: 10.1016/j.immuni.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Plotkin SA. Vaccines: past, present and future. Nature medicine. 2005;11:S5–S11. doi: 10.1038/nm1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rappuoli R, Aderem A. A 2020 vision for vaccines against HIV, tuberculosis and malaria. Nature. 2011;473:463–469. doi: 10.1038/nature10124. [DOI] [PubMed] [Google Scholar]
- 5.Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature. 2011;480:480–489. doi: 10.1038/nature10673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Topalian SL, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. The New England journal of medicine. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brahmer JR, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. The New England journal of medicine. 2012;366:2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valenta R, et al. From allergen genes to allergy vaccines. Annual Review of Immunology. 2010;28:211–241. doi: 10.1146/annurev-immunol-030409-101218. [DOI] [PubMed] [Google Scholar]
- 9.Dolgin E. The inverse of immunity. Nature medicine. 2010;16:740–743. doi: 10.1038/nm0710-740. [DOI] [PubMed] [Google Scholar]
- 10.D'Argenio DA, Wilson CB. A decade of vaccines: Integrating immunology and vaccinology for rational vaccine design. Immunity. 2010;33:437–440. doi: 10.1016/j.immuni.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 11.Steinman RM, Banchereau J. Taking dendritic cells into medicine. Nature. 2007;449:419–426. doi: 10.1038/nature06175. [DOI] [PubMed] [Google Scholar]
- 12.Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392:245–252. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 13.Kawai T, Akira S. The roles of TLRs, RLRs and NLRs in pathogen recognition. International Immunology. 2009;21:317–337. doi: 10.1093/intimm/dxp017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bachmann MF, et al. The influence of antigen organization on B cell responsiveness. Science. 1993;262:1448–1451. doi: 10.1126/science.8248784. [DOI] [PubMed] [Google Scholar]
- 15.Blander JM, Medzhitov R. Toll-dependent selection of microbial antigens for presentation by dendritic cells. Nature. 2006;440:808–812. doi: 10.1038/nature04596. [DOI] [PubMed] [Google Scholar]
- 16.Kovacsovics-Bankowski M, Rock KL. A phagosome-to-cytosol pathway for exogenous antigens presented on MHC class I molecules. Science. 1995;267:243–246. doi: 10.1126/science.7809629. [DOI] [PubMed] [Google Scholar]
- 17.Lund AW, et al. VEGF-C promotes immune tolerance in B16 melanomas and cross-presentation of tumor antigen by lymph node lymphatics. Cell reports. 2012;1:191–199. doi: 10.1016/j.celrep.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 18.Lin ML, Zhan Y, Villadangos JA, Lew AM. The cell biology of cross-presentation and the role of dendritic cell subsets. Immunology and cell biology. 2008;86:353–362. doi: 10.1038/icb.2008.3. [DOI] [PubMed] [Google Scholar]
- 19.den Haan JM, Bevan MJ. Constitutive versus activation-dependent cross-presentation of immune complexes by CD8(+) and CD8(−) dendritic cells in vivo. The Journal of experimental medicine. 2002;196:817–827. doi: 10.1084/jem.20020295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Segura E, Durand M, Amigorena S. Similar antigen cross-presentation capacity and phagocytic functions in all freshly isolated human lymphoid organ-resident dendritic cells. The Journal of experimental medicine. 2013;210:1035–1047. doi: 10.1084/jem.20121103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foged C, Hansen J, Agger EM. License to kill: Formulation requirements for optimal priming of CD8(+) CTL responses with particulate vaccine delivery systems. European journal of pharmaceutical sciences : official journal of the European Federation for Pharmaceutical Sciences. 2012;45:482–491. doi: 10.1016/j.ejps.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 22.Bachmann MF, Jennings GT. Vaccine delivery: a matter of size, geometry, kinetics and molecular patterns. Nature reviews. Immunology. 2010;10:787–796. doi: 10.1038/nri2868. [DOI] [PubMed] [Google Scholar]
- 23.Kourtis IC, et al. Peripherally administered nanoparticles target monocytic myeloid cells, secondary lymphoid organs and tumors in mice. PloS one. 2013;8:e61646. doi: 10.1371/journal.pone.0061646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Swartz MA, Hirosue S, Hubbell JA. Engineering approaches to immunotherapy. Science translational medicine. 2012;4:148rv149. doi: 10.1126/scitranslmed.3003763. [DOI] [PubMed] [Google Scholar]
- 25.Villa CH, et al. Single-walled carbon nanotubes deliver peptide antigen into dendritic cells and enhance IgG responses to tumor-associated antigens. ACS nano. 2011;5:5300–5311. doi: 10.1021/nn200182x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nembrini C, et al. Nanoparticle conjugation of antigen enhances cytotoxic T-cell responses in pulmonary vaccination. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:E989–E997. doi: 10.1073/pnas.1104264108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reddy S, et al. Exploiting lymphatic transport and complement activation in nanoparticle vaccines. Nature Biotechnology. 2007;25:1159–1164. doi: 10.1038/nbt1332. [DOI] [PubMed] [Google Scholar]
- 28.Fifis T, et al. Size-dependent immunogenicity: therapeutic and protective properties of nano-vaccines against tumors. Journal of immunology. 2004;173:3148–3154. doi: 10.4049/jimmunol.173.5.3148. [DOI] [PubMed] [Google Scholar]
- 29.De Rose R, et al. Binding, Internalization, and Antigen Presentation of Vaccine-Loaded Nanoengineered Capsules in Blood. Advanced Materials. 2008;20:4698–4703. [Google Scholar]
- 30.De Geest BG, et al. Surface-engineered polyelectrolyte multilayer capsules: synthetic vaccines mimicking microbial structure and function. Angewandte Chemie. International Edition in English. 2012;51:3862–3866. doi: 10.1002/anie.201200048. [DOI] [PubMed] [Google Scholar]
- 31.Dierendonck M, et al. Facile Two-Step Synthesis of Porous Antigen-Loaded Degradable Polyelectrolyte Microspheres. Angewandte Chemie International Edition. 2010;49:8620–8624. doi: 10.1002/anie.201001046. [DOI] [PubMed] [Google Scholar]
- 32.Perry JL, Herlihy KP, Napier ME, DeSimone JM. PRINT: A Novel Platform Toward Shape and Size Specific Nanoparticle Theranostics. Accounts of Chemical Research. 2011;44:990–998. doi: 10.1021/ar2000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galloway AL, et al. Development of a nanoparticle-based influenza vaccine using the PRINT technology. Nanomedicine : nanotechnology, biology, and medicine. 2013;9:523–531. doi: 10.1016/j.nano.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 34.Reis e Sousa C, Germain RN. Major histocompatibility complex class I presentation of peptides derived from soluble exogenous antigen by a subset of cells engaged in phagocytosis. The Journal of experimental medicine. 1995;182:841–851. doi: 10.1084/jem.182.3.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scott EA, et al. Dendritic cell activation and T cell priming with adjuvant- and antigen-loaded oxidation-sensitive polymersomes. Biomaterials. 2012;33:6211–6219. doi: 10.1016/j.biomaterials.2012.04.060. [DOI] [PubMed] [Google Scholar]
- 36.Hirosue S, Kourtis IC, van der Vlies AJ, Hubbell JA, Swartz MA. Antigen delivery to dendritic cells by poly(propylene sulfide) nanoparticles with disulfide conjugated peptides: Cross-presentation and T cell activation. Vaccine. 2010;28:7897–7906. doi: 10.1016/j.vaccine.2010.09.077. [DOI] [PubMed] [Google Scholar]
- 37.Moon JJ, et al. Interbilayer-crosslinked multilamellar vesicles as synthetic vaccines for potent humoral and cellular immune responses. Nature materials. 2011;10:243–251. doi: 10.1038/nmat2960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nordly P, et al. Immunity by formulation design: induction of high CD8+ T-cell responses by poly(I:C) incorporated into the CAF01 adjuvant via a double emulsion method. Journal of controlled release : official journal of the Controlled Release Society. 2011;150:307–317. doi: 10.1016/j.jconrel.2010.11.021. [DOI] [PubMed] [Google Scholar]
- 39.Zaks K, et al. Efficient immunization and cross-priming by vaccine adjuvants containing TLR3 or TLR9 agonists complexed to cationic liposomes. Journal of immunology. 2006;176:7335–7345. doi: 10.4049/jimmunol.176.12.7335. [DOI] [PubMed] [Google Scholar]
- 40.Powell TJ, et al. Plasmodium falciparum synthetic LbL microparticle vaccine elicits protective neutralizing antibody and parasite-specific cellular immune responses. Vaccine. 2013;31:1898–1904. doi: 10.1016/j.vaccine.2013.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kasturi SP, et al. Programming the magnitude and persistence of antibody responses with innate immunity. Nature. 2011;470:543–547. doi: 10.1038/nature09737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kazzaz J, et al. Encapsulation of the immune potentiators MPL and RC529 in PLG microparticles enhances their potency. Journal of controlled release : official journal of the Controlled Release Society. 2006;110:566–573. doi: 10.1016/j.jconrel.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 43.Zhu Q, et al. Using 3 TLR ligands as a combination adjuvant induces qualitative changes in T cell responses needed for antiviral protection in mice. The Journal of clinical investigation. 2010;120:607–616. doi: 10.1172/JCI39293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garaude J, Kent A, van Rooijen N, Blander JM. Simultaneous targeting of toll- and nod-like receptors induces effective tumor-specific immune responses. Science translational medicine. 2012;4:120ra116. doi: 10.1126/scitranslmed.3002868. [DOI] [PubMed] [Google Scholar]
- 45.Tacken PJ, et al. Targeted delivery of TLR ligands to human and mouse dendritic cells strongly enhances adjuvanticity. Blood. 2011;118:6836–6844. doi: 10.1182/blood-2011-07-367615. [DOI] [PubMed] [Google Scholar]
- 46.Moon JJ, et al. Enhancing humoral responses to a malaria antigen with nanoparticle vaccines that expand Tfh cells and promote germinal center induction. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:1080–1085. doi: 10.1073/pnas.1112648109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nguyen DN, et al. Lipid-derived nanoparticles for immunostimulatory RNA adjuvant delivery. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:E797–E803. doi: 10.1073/pnas.1121423109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ng G, et al. Receptor-independent, direct membrane binding leads to cell-surface lipid sorting and Syk kinase activation in dendritic cells. Immunity. 2008;29:807–818. doi: 10.1016/j.immuni.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Flach TL, et al. Alum interaction with dendritic cell membrane lipids is essential for its adjuvanticity. Nature medicine. 2011;17:479–487. doi: 10.1038/nm.2306. [DOI] [PubMed] [Google Scholar]
- 50.Marichal T, et al. DNA released from dying host cells mediates aluminum adjuvant activity. Nature medicine. 2011;17:996–1002. doi: 10.1038/nm.2403. [DOI] [PubMed] [Google Scholar]
- 51.Harris J, Sharp FA, Lavelle EC. The role of inflammasomes in the immunostimulatory effects of particulate vaccine adjuvants. European journal of immunology. 2010;40:634–638. doi: 10.1002/eji.200940172. [DOI] [PubMed] [Google Scholar]
- 52.Hornung V, et al. Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Nature immunology. 2008;9:847–856. doi: 10.1038/ni.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shi Y, Evans JE, Rock KL. Molecular identification of a danger signal that alerts the immune system to dying cells. Nature. 2003;425:516–521. doi: 10.1038/nature01991. [DOI] [PubMed] [Google Scholar]
- 54.Ballester M, et al. Nanoparticle conjugation and pulmonary delivery enhance the protective efficacy of Ag85B and CpG against tuberculosis. Vaccine. 2011;29:6959–6966. doi: 10.1016/j.vaccine.2011.07.039. [DOI] [PubMed] [Google Scholar]
- 55.Sharp FA, et al. Uptake of particulate vaccine adjuvants by dendritic cells activates the NALP3 inflammasome. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:870–875. doi: 10.1073/pnas.0804897106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Demento SL, et al. Inflammasome-activating nanoparticles as modular systems for optimizing vaccine efficacy. Vaccine. 2009;27:3013–3021. doi: 10.1016/j.vaccine.2009.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.De Geest BG, et al. Polymeric multilayer capsule-mediated vaccination induces protective immunity against cancer and viral infection. ACS nano. 2012;6:2136–2149. doi: 10.1021/nn205099c. [DOI] [PubMed] [Google Scholar]
- 58.Li H, Li Y, Jiao J, Hu HM. Alpha-alumina nanoparticles induce efficient autophagy-dependent cross-presentation and potent antitumour response. Nature nanotechnology. 2011;6:645–650. doi: 10.1038/nnano.2011.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thomas SN, et al. Engineering complement activation on polypropylene sulfide vaccine nanoparticles. Biomaterials. 2011;32:2194–2203. doi: 10.1016/j.biomaterials.2010.11.037. [DOI] [PubMed] [Google Scholar]
- 60.Moyano DF, et al. Nanoparticle hydrophobicity dictates immune response. Journal of the American Chemical Society. 2012;134:3965–3967. doi: 10.1021/ja2108905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Petersen LK, et al. Activation of innate immune responses in a pathogen-mimicking manner by amphiphilic polyanhydride nanoparticle adjuvants. Biomaterials. 2011;32:6815–6822. doi: 10.1016/j.biomaterials.2011.05.063. [DOI] [PubMed] [Google Scholar]
- 62.Seong SY, Matzinger P. Hydrophobicity: an ancient damage-associated molecular pattern that initiates innate immune responses. Nature reviews. Immunology. 2004;4:469–478. doi: 10.1038/nri1372. [DOI] [PubMed] [Google Scholar]
- 63.Rudra JS, Tian YF, Jung JP, Collier JH. A self-assembling peptide acting as an immune adjuvant. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:622–627. doi: 10.1073/pnas.0912124107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Getts DR, et al. Microparticles bearing encephalitogenic peptides induce T-cell tolerance and ameliorate experimental autoimmune encephalomyelitis. Nature Biotechnology. 2012;30:1217–1224. doi: 10.1038/nbt.2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lewis JS, Zaveri TD, Crooks CP, 2nd, Keselowsky BG. Microparticle surface modifications targeting dendritic cells for non-activating applications. Biomaterials. 2012;33:7221–7232. doi: 10.1016/j.biomaterials.2012.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yeste A, Nadeau M, Burns EJ, Weiner HL, Quintana FJ. Nanoparticle-mediated codelivery of myelin antigen and a tolerogenic small molecule suppresses experimental autoimmune encephalomyelitis. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:11270–11275. doi: 10.1073/pnas.1120611109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tsai S, et al. Reversal of autoimmunity by boosting memory-like autoregulatory T cells. Immunity. 2010;32:568–580. doi: 10.1016/j.immuni.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 68.Wherry EJ, Blattman JN, Murali-Krishna K, van der Most R, Ahmed R. Viral persistence alters CD8 T-cell immunodominance and tissue distribution and results in distinct stages of functional impairment. Journal of virology. 2003;77:4911–4927. doi: 10.1128/JVI.77.8.4911-4927.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mueller SN, Ahmed R. High antigen levels are the cause of T cell exhaustion during chronic viral infection. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:8623–8628. doi: 10.1073/pnas.0809818106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pape KA, Catron DM, Itano AA, Jenkins MK. The humoral immune response is initiated in lymph nodes by B cells that acquire soluble antigen directly in the follicles. Immunity. 2007;26:491–502. doi: 10.1016/j.immuni.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 71.Itano AA, et al. Distinct dendritic cell populations sequentially present antigen to CD4 T cells and stimulate different aspects of cell-mediated immunity. Immunity. 2003;19:47–57. doi: 10.1016/s1074-7613(03)00175-4. [DOI] [PubMed] [Google Scholar]
- 72.Johansen P, et al. Antigen kinetics determines immune reactivity. Proceedings of the National Academy of Sciences of the United States of America. 2008;105:5189–5194. doi: 10.1073/pnas.0706296105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Howland SW, Wittrup KD. Antigen release kinetics in the phagosome are critical to cross-presentation efficiency. Journal of immunology. 2008;180:1576–1583. doi: 10.4049/jimmunol.180.3.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Marx PA, et al. Protection against vaginal SIV transmission with microencapsulated vaccine. Science. 1993;260:1323–1327. doi: 10.1126/science.8493576. [DOI] [PubMed] [Google Scholar]
- 75.Neutra MR, Kozlowski PA. Mucosal vaccines: the promise and the challenge. Nature reviews. Immunology. 2006;6:148–158. doi: 10.1038/nri1777. [DOI] [PubMed] [Google Scholar]
- 76.Zhu G, Mallery S, Schwendeman S. Stabilization of proteins encapsulated in injectable poly (lactide-co-glycolide) Nature Biotechnology. 2000;18:52–57. doi: 10.1038/71916. [DOI] [PubMed] [Google Scholar]
- 77.Zhu Q, et al. Large intestine-targeted, nanoparticle-releasing oral vaccine to control genitorectal viral infection. Nature medicine. 2012 doi: 10.1038/nm.2866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fujkuyama Y, et al. Novel vaccine development strategies for inducing mucosal immunity. Expert review of vaccines. 2012;11:367–379. doi: 10.1586/erv.11.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sullivan SP, et al. Dissolving polymer microneedle patches for influenza vaccination. Nature medicine. 2010;16:915–920. doi: 10.1038/nm.2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zaric M, et al. Skin dendritic cell targeting via microneedle arrays laden with antigen-encapsulated poly-D,L-lactide-co-glycolide nanoparticles induces efficient antitumor and antiviral immune responses. ACS nano. 2013;7:2042–2055. doi: 10.1021/nn304235j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Prow TW, et al. Nanopatch-targeted skin vaccination against West Nile Virus and Chikungunya virus in mice. Small. 2010;6:1776–1784. doi: 10.1002/smll.201000331. [DOI] [PubMed] [Google Scholar]
- 82.DeMuth PC, et al. Polymer multilayer tattooing for enhanced DNA vaccination. Nature materials. 2013;12:367–376. doi: 10.1038/nmat3550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Atuma C, Strugala V, Allen A, Holm L. The adherent gastrointestinal mucus gel layer: thickness and physical state in vivo. American journal of physiology. Gastrointestinal and liver physiology. 2001;280:G922–G929. doi: 10.1152/ajpgi.2001.280.5.G922. [DOI] [PubMed] [Google Scholar]
- 84.Lai SK, Wang YY, Hida K, Cone R, Hanes J. Nanoparticles reveal that human cervicovaginal mucus is riddled with pores larger than viruses. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:598–603. doi: 10.1073/pnas.0911748107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tang BC, et al. Biodegradable polymer nanoparticles that rapidly penetrate the human mucus barrier. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:19268–19273. doi: 10.1073/pnas.0905998106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lai SK, et al. Rapid transport of large polymeric nanoparticles in fresh undiluted human mucus. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:1482–1487. doi: 10.1073/pnas.0608611104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cu Y, Booth CJ, Saltzman WM. In vivo distribution of surface-modified PLGA nanoparticles following intravaginal delivery. Journal of controlled release : official journal of the Controlled Release Society. 2011;156:258–264. doi: 10.1016/j.jconrel.2011.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ensign LM, et al. Mucus-penetrating nanoparticles for vaginal drug delivery protect against herpes simplex virus. Science translational medicine. 2012;4:138ra179. doi: 10.1126/scitranslmed.3003453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nochi T, et al. Nanogel antigenic protein-delivery system for adjuvant-free intranasal vaccines. Nature materials. 2010;9:572. doi: 10.1038/nmat2784. [DOI] [PubMed] [Google Scholar]
- 90.Fleury ME, Boardman KC, Swartz MA. Autologous morphogen gradients by subtle interstitial flow and matrix interactions. Biophysical journal. 2006;91:113–121. doi: 10.1529/biophysj.105.080192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tang L, Fan TM, Borst LB, Cheng J. Synthesis and biological response of size-specific, monodisperse drug-silica nanoconjugates. ACS nano. 2012;6:3954–3966. doi: 10.1021/nn300149c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bershteyn A, et al. Robust IgG responses to nanograms of antigen using a biomimetic lipid-coated particle vaccine. Journal of controlled release : official journal of the Controlled Release Society. 2012;157:354–365. doi: 10.1016/j.jconrel.2011.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Murthy N, et al. A macromolecular delivery vehicle for protein-based vaccines: acid-degradable protein-loaded microgels. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:4995–5000. doi: 10.1073/pnas.0930644100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hu Y, et al. Cytosolic delivery of membrane-impermeable molecules in dendritic cells using pH-responsive core-shell nanoparticles. Nano Letters. 2007;7:3056–3064. doi: 10.1021/nl071542i. [DOI] [PubMed] [Google Scholar]
- 95.Su X, Fricke J, Kavanagh DG, Irvine DJ. In vitro and in vivo mRNA delivery using lipid-enveloped pH-responsive polymer nanoparticles. Molecular pharmaceutics. 2011;8:774–787. doi: 10.1021/mp100390w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Haining WN, et al. pH-triggered microparticles for peptide vaccination. Journal of immunology. 2004;173:2578–2585. doi: 10.4049/jimmunol.173.4.2578. [DOI] [PubMed] [Google Scholar]
- 97.Heffernan MJ, Kasturi SP, Yang SC, Pulendran B, Murthy N. The stimulation of CD8+ T cells by dendritic cells pulsed with polyketal microparticles containing ion-paired protein antigen and poly(inosinic acid)-poly(cytidylic acid) Biomaterials. 2009;30:910–918. doi: 10.1016/j.biomaterials.2008.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vasdekis AE, Scott EA, O'Neil CP, Psaltis D, Hubbell JA. Precision intracellular delivery based on optofluidic polymersome rupture. ACS nano. 2012;6:7850–7857. doi: 10.1021/nn302122h. [DOI] [PubMed] [Google Scholar]
- 99.Shen H, et al. Enhanced and prolonged cross-presentation following endosomal escape of exogenous antigens encapsulated in biodegradable nanoparticles. Immunology. 2006;117:78–88. doi: 10.1111/j.1365-2567.2005.02268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Geall AJ, et al. Nonviral delivery of self-amplifying RNA vaccines. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:14604–14609. doi: 10.1073/pnas.1209367109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Verma A, et al. Surface-structure-regulated cell-membrane penetration by monolayer-protected nanoparticles. Nature materials. 2008;7:588–595. doi: 10.1038/nmat2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Marrack P, McKee A, Munks M. Towards an understanding of the adjuvant action of aluminium. Nature reviews. Immunology. 2009;9:287–293. doi: 10.1038/nri2510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hutchison S, et al. Antigen depot is not required for alum adjuvanticity. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2012;26:1272–1279. doi: 10.1096/fj.11-184556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gupta RK, Chang AC, Griffin P, Rivera R, Siber GR. In vivo distribution of radioactivity in mice after injection of biodegradable polymer microspheres containing 14C-labeled tetanus toxoid. Vaccine. 1996;14:1412–1416. doi: 10.1016/s0264-410x(96)00073-4. [DOI] [PubMed] [Google Scholar]
- 105.Preis I, Langer RS. A single-step immunization by sustained antigen release. Journal of Immunological Methods. 1979;28:193–197. doi: 10.1016/0022-1759(79)90341-7. [DOI] [PubMed] [Google Scholar]
- 106.Thomasin C, Corradin G, Men Y, Merkle HP, Gander B. Tetanus toxoid and synthetic malaria antigen containing poly(lactide)/poly(lactide-co-glycolide) microspheres: Importance of polymer degradation and antigen release for immune response. Journal of controlled release : official journal of the Controlled Release Society. 1996;41:131–145. [Google Scholar]
- 107.Hailemichael Y, et al. Persistent antigen at vaccination sites induces tumor-specific CD8(+) T cell sequestration, dysfunction and deletion. Nature medicine. 2013;19:465–472. doi: 10.1038/nm.3105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jewell CM, Lopez SC, Irvine DJ. In situ engineering of the lymph node microenvironment via intranodal injection of adjuvant-releasing polymer particles. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:15745–15750. doi: 10.1073/pnas.1105200108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.St John AL, Chan CY, Staats HF, Leong KW, Abraham SN. Synthetic mast-cell granules as adjuvants to promote and polarize immunity in lymph nodes. Nature materials. 2012;11:250–257. doi: 10.1038/nmat3222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Braumuller H, et al. T-helper-1-cell cytokines drive cancer into senescence. Nature. 2013;494:361–365. doi: 10.1038/nature11824. [DOI] [PubMed] [Google Scholar]
- 111.Reiner SL, Locksley RM. The regulation of immunity to Leishmania major. Annual Review of Immunology. 1995;13:151–177. doi: 10.1146/annurev.iy.13.040195.001055. [DOI] [PubMed] [Google Scholar]
- 112.Ali OA, Emerich D, Dranoff G, Mooney DJ. In situ regulation of DC subsets and T cells mediates tumor regression in mice. Science translational medicine. 2009;1:8ra19. doi: 10.1126/scitranslmed.3000359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ali OA, Huebsch N, Cao L, Dranoff G, Mooney DJ. Infection-mimicking materials to program dendritic cells in situ. Nature materials. 2009;8:151–158. doi: 10.1038/nmat2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Singh A, et al. An injectable synthetic immune-priming center mediates efficient T-cell class switching and T-helper 1 response against B cell lymphoma. Journal of controlled release : official journal of the Controlled Release Society. 2011;155:184–192. doi: 10.1016/j.jconrel.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 115.Langhorne J, et al. The relevance of non-human primate and rodent malaria models for humans. Malaria Journal. 2011;10:23. doi: 10.1186/1475-2875-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Morgan C, et al. The Use of Nonhuman Primate Models in HIV Vaccine Development. PLoS Medicine. 2008;5:e173. doi: 10.1371/journal.pmed.0050173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Tsuji K, et al. Induction of immune response against NY-ESO-1 by CHP-NY-ESO-1 vaccination and immune regulation in a melanoma patient. Cancer immunology, immunotherapy : CII. 2008;57:1429–1437. doi: 10.1007/s00262-008-0478-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ataman-Onal Y, et al. Surfactant-free anionic PLA nanoparticles coated with HIV-1 p24 protein induced enhanced cellular and humoral immune responses in various animal models. Journal of controlled release : official journal of the Controlled Release Society. 2006;112:175–185. doi: 10.1016/j.jconrel.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 119.Otten G, et al. Induction of broad and potent anti-human immunodeficiency virus immune responses in rhesus macaques by priming with a DNA vaccine and boosting with protein-adsorbed polylactide coglycolide microparticles. Journal of virology. 2003;77:6087–6092. doi: 10.1128/JVI.77.10.6087-6092.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Appay V, Douek DC, Price DA. CD8+ T cell efficacy in vaccination and disease. Nature medicine. 2008;14:623–628. doi: 10.1038/nm.f.1774. [DOI] [PubMed] [Google Scholar]
- 121.Nimmerjahn F, Ravetch JV. Antibody-mediated modulation of immune responses. Immunological reviews. 2010;236:265–275. doi: 10.1111/j.1600-065X.2010.00910.x. [DOI] [PubMed] [Google Scholar]
- 122.Virgin HW, Walker BD. Immunology and the elusive AIDS vaccine. Nature. 2010;464:224–231. doi: 10.1038/nature08898. [DOI] [PubMed] [Google Scholar]
- 123.Crow JM. HPV: The global burden. Nature. 2012;488:S2–S3. doi: 10.1038/488S2a. [DOI] [PubMed] [Google Scholar]
- 124.Ma B, Xu Y, Hung C-F, Wu T-C. HPV and therapeutic vaccines: where are we in 2010? Curr Cancer Ther Rev. 2010;6:81–103. [Google Scholar]
- 125.Klebanoff CA, Acquavella N, Yu Z, Restifo NP. Therapeutic cancer vaccines: are we there yet? Immunological reviews. 2011;239:27–44. doi: 10.1111/j.1600-065X.2010.00979.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Harrison LC. Vaccination against self to prevent autoimmune disease: the type 1 diabetes model. Immunology and cell biology. 2008;86:139–145. doi: 10.1038/sj.icb.7100151. [DOI] [PubMed] [Google Scholar]
- 127.Wisniewski T, Goni F. Immunomodulation for prion and prion-related diseases. Expert review of vaccines. 2010;9:1441–1452. doi: 10.1586/erv.10.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Linhart B, Valenta R. Vaccines for allergy. Current opinion in immunology. 2012;24:354–360. doi: 10.1016/j.coi.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sela M, Mozes E. Therapeutic vaccines in autoimmunity. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(Suppl 2):14586–14592. doi: 10.1073/pnas.0404826101. [DOI] [PMC free article] [PubMed] [Google Scholar]