Abstract
Significance: Delayed healing of skin wounds is a serious problem for the patients, clinicians, and society. The application of interventions with proven effectiveness to increase wound healing is relevant.
Recent Advances: This article summarizes the results of effect studies with the application of electrostimulation (ES) as additional treatment to standard wound care (SWC). Therefore, five published narrative reviews are discussed. In addition, 15 studies with a clear randomized controlled trial design are analyzed systematically and the results are presented in four forest plots. The healing rate is expressed in the outcome measure percentage area reduction in 4 weeks of treatment (PAR4). This leads to a continuous measure with mean differences between the percentage healing in the experimental group (SWC plus ES) and in the control group (SWC alone or SWC plus placebo ES). Adding ES to SWC in all wound types increases PAR4 by an extra 26.7% (95% confidence interval [CI] 15.6, 37.8); adding unidirectional ES to SWC increases PAR4 by 30.8% (95% CI 20.9, 40.6) and adding unidirectional ES to the treatment of pressure ulcers increases PAR4 by 42.7% (95% CI 32.0, 53.3).
Critical Issues: There is a discrepancy between the proven effectiveness of ES as additional treatment to SWC and the application of ES in real practice. Possible drawbacks are the lack of clinical expertise concerning the proper application of ES and the extra time effort and necessary equipment that are needed.
Future Directions: Clinicians concerned about the optimal treatment of patients with delayed wound healing should improve their practical competency to be able to apply ES.

Gerard Koel, PT, MSc
Scope and Significance
Chronic wounds are a serious problem for patients, clinicians, and society. This review focuses on the clinical effectiveness and practicality of the application of electrostimulation (ES) as an additional treatment in wound care.
Electrotherapy (ET) is sometimes defined in a broad way gathering all modalities developed with an electrical apparatus that is applied to a patient with therapeutic objectives (like ultrasound, laser, shortwave, or shockwave therapy); however, in this review, ET is defined in a smaller way meaning those therapies that apply an electrical stimulus to the patient. ET can be classified in three categories: low frequency (<1,000 Hz), medium frequency (1,000–300,000 Hz), and high frequency (>300,000 Hz). Stimulation of neuromuscular tissues is just possible with low- and medium-frequency ET and that is why these forms are also indicated as ES. In this review, the effectiveness of low-frequency ES on wound healing is evaluated. In low-frequency ES, at least two electrodes are attached to the body to realize an electric circuit leading to an internal electric field (EF) with physiological responses of the body. The placement of the electrodes is often one in the wound and the other one opposite to it or with both electrodes just around the wound. Two forms of low-frequency ES should be distinguished; unidirectional ES with a fixed cathode (negative pole) and anode (positive pole) leading to an EF in the same direction, or bidirectional ES with biphasic pulses and with alternating cathode and anode and an also alternating EF.
The effectiveness of different types of ES (unidirectional and bidirectional ES) on different wound types as pressure ulcers (PU), venous leg ulcers (VLU), and diabetic foot ulcers (DFU) will be described by summarizing the results presented in effect studies with high methodological quality.
Translational Relevance
Basic science research has shown that in living organisms, endogenous EFs play a vital role in the regulation of several physiological processes, including wound healing. Well-known measurable electrical phenomena include action potentials in the neuromuscular system, positioning of proteins in connective tissue, electroencephalogram, electrocardiogram, and electroretinogram. Mammalian skin layers have voltage gradients, which in the case of a skin wound lead to the development of the transepithelial potential (TEP) that plays a leading role in the generation of the endogenous integumentary EF.1,2 The EF has a stimulating effect on epidermal stem cells relevant for wound healing.3,4
Clinical Relevance
Chronic wounds of the skin and subcutaneous tissues are often a significant problem for patients in that, they often contribute to decreased mobility, wound-related pain, and infection. The costs for caring of chronic wounds in many societies have reached almost insurmountable levels.5 In the industrialized world, the high prevalence of chronic wounds is significantly related to aging and to the higher occurrence of comorbidities like diabetes mellitus and stroke. Unfortunately, it appears that the number of people with chronic wounds will continue to increase. The application of interventions with proven effectiveness and efficacy is relevant.
Discussion of Findings and Relevant Literature
Current status
Levels of evidence
In 2011, the Oxford Center of Evidence Based Medicine (EBM) published the new version of the GRADE system for classifying the levels of external evidence.6 For interventions like ES used in the treatment of chronic wounds, five levels of evidence are distinguished; the highest level 1 means that a systematic review (SR) of several effect studies with a proper randomized controlled trial (RCT) design is available. Level 2 evidence is based on studies with the RCT design, level 3 on controlled, but nonrandomized studies, level 4 on case series or case–control studies, and level 5 on mechanism or theory-based therapy.
An SR is based on a thorough literature search, applies clear criteria to include studies, weighs the studies for methodological quality and for possible risk of bias, and performs the analysis and statistical pooling with transparent and valid methods. An SR ends with a recommendation for clinical practice; sometimes a clear recommendation can be formulated; but very often it is, due to inconsistent results described in the effect studies, not possible to come up with a clear overall result. At the Cochrane website (www.cochrane.org [the main source for SRs]), about 25 SRs on topical treatments for wound healing can be assessed. Evaluating reviews concerning several topical wound treatments leads to the conclusion that at best, no clear evidence is available for most of the treatments like dressings,7,8 silver,9,10 honey,11 negative pressure treatment,12 or ultrasound therapy.13 In fact, only two clear conclusions are made; in VLU, compression improves healing14 and cleaning a wound with tap water does not increase the chance for contamination.15
Quality of effect studies regarding bioelectric fields and wound healing
Searching the scientific literature leads to the positive conclusion that, in this field, a sufficient number of studies are performed. That counts for fundamental research on the rationale of ES for wound healing, for uncontrolled case studies as well for effect studies with the RCT design. In the next paragraph, the published reviews will be discussed; at the moment, there is no SR available.
Availability and quality of reviews
Recently, a number of narrative reviews have been published concerning the topic, “Does ES stimulate wound healing?”16–20 Four of the five review authors evaluated the effects of ES to be positive and consider ES as a “potentially useful, accessible, and cheap intervention,”18 but “further research is desired.”16,19 Only the judgment of Collins et al.20 is less positive. Including 13 studies with the RCT design, the authors conclude that they “…failed to find statistically significant differences in wound healing between patients treated with ES and controls in the majority of reports.”20 All five reviews have a narrative design, which means (1) they are written by experts, (2) studies are included without clear selection criteria, (3) studies are evaluated without transparency in the research methodology, and (4) conclusions are still based on authority and have nonoptimal generalizability. Narrative reviewing is a reason why different reviews reviewing the same topic, sometimes even based on the same effect studies, can arrive at different interpretations and conclusions. In the next paragraph, a SR on the effects of ES on the acceleration of wound healing is described.
Translation to guidelines
Despite the fact that many good quality studies are available in most clinical guidelines, ES is not mentioned as one of the options for proper treatment. An exception has to be made for the guideline for PU, the type of wound that is most frequently studied. The combined European Pressure Ulcer Advisory Panel (EPUAP)/National Pressure Ulcer Advisory Panel (NPUAP) reference guideline is clearly positive about the application of ES to improve the healing of PU.21 In that guideline for clinicians, the strength of evidence is classified from A (strong) to B (moderate) and C (weak), and on page 35, the application of ES is described as follows: “…. consider the use of direct contact ES in the management of recalcitrant stage II, as well as stage III and IV PU to facilitate wound healing (strength of evidence=A).”
New systematic analysis of studies on healing rate
Selection of high-quality effect studies
A literature search in the available databases like Medline, Embase, and Cinahl was performed with appropriate search/MESH terms. All chronic wound types were included, the intervention had to be low-frequency ES, the design was RCT, and the primary outcome measure was the healing rate. The authors were very strict to categorize a study as an RCT study only if the study states that the allocation was random. The precise method of randomization need not be specified. Procedures such as coin-tossing and dice-rolling should be considered as random. Quasi-randomization allocation procedures such as allocation by hospital record number, birth date, participating institute (in a multicenter study), or alternation, do not satisfy this criterion.
To be sure to select only high-quality RCTs, we further applied the inclusion and exclusion criteria listed in Table 1.
Table 1.
The inclusion and exclusion criteria for effect studies with randomized controlled trial design to enter the systematic review
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Good RCT design, experimental group with SWC plus ES and control group of the same SWC without ES or with sham ES | No selection bias (random sequence generation and concealed allocation) No reporting bias, so methods paragraph and results paragraph are consistent |
| Appropriate blinding of observers who perform the measurement | Loss to follow-up larger than 20% |
| Clear description of the form of ES | Involvement of ES manufacturers |
| Number of wounds, at least 20 |
ES, electrostimulation; RCT, randomized controlled trial; SWC, standard wound care.
This very strict selection, independently performed by two authors, led to the inclusion of 15 high-quality studies.22–36 The analysis is described in the next section.
Expression of healing rates in percentage area reduction in 4 weeks
The 15 RCTs have treatment times ranging from 3 weeks to 16 weeks (average treatment time is 6.5 weeks; most of the time with five treatments per week) and the studies describe the wound surface in cm2 at the start of the study (A0) and at the end of the study (A1). In this review, the percentage area reduction (PAR) will be used to express the healing rate. The PAR is a sensitive measure that corrects for possible differences in the initial wound surface area.37 PAR is calculated as [(A0 − A1)/A0] ×100%, where in A0 is the initial wound area and A1 the wound area at the end of the treatment period.
Clinicians are advised to use the PAR at 4 weeks as a relevant predictor for wound closure, so in this review, the percentage area reduction in 4 weeks (PAR4) is used as a continuous outcome measure.38–40 Expressing healing rates in PAR4 values makes it possible to compare the effects of different studies with different treatment periods. The information in the 15 RCTs was good enough allowing the authors of this review to calculate the PAR4 values from the original data.
Analysis of PAR4 leads to a weighted mean difference between ES groups (standard wound care [SWC] plus ES) and control groups (SWC with placebo ES or SWC alone). Wounds with poor healing progress at 4 weeks were highly likely to remain unhealed after 8 weeks of additional treatment. Cardinal et al.40 analyzed retrospectively the effects of topical wound care in 306 VLU and 241 DFU and found the following characteristics of PAR4 as a predictor of complete ulcer healing at 12 weeks. Selecting a cutoff point of PAR4=37.7%, the positive predictive value for complete healing was 70.6% and the likelihood ratio was 6.15; meaning that patients (wounds) who reach at least PAR4 37.7% have a 6.15 greater chance of total healing in 12 weeks than wounds that do not reach a PAR4 of 37.7%.
In the Supplementary Data (available online at www.liebertpub.com/wound), the calculations for the PAR4 in the 15 studies and the standard deviations for those new PAR4 samples are presented. The method of calculation is described. Table 2 presents the PAR4 values of the 15 included studies.
Table 2.
Details of the 15 included randomized controlled trial studies
| Characteristics of RCT Studies | Exp (SWC+ES) | Control (SWC – ES) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Ref. | Study, Year of Publication | N total | Type of Ulcer | Type of ES | Weeks | N Exp. | PAR4 (%) | N Ctr. | PAR4 (%) |
| 22 | Ahmad, 2008 | 60 | PU | Uni | 5 | 45 | 62.35 | 15 | 20.76 |
| 23 | Baker/Rubayi, 1996 | 192 | DFU | Bi | 4 | 125 | 38.49 | 67 | 51.00 |
| 24 | Baker/Chambers, 1997 | 114 | PU | Bi | 4 | 61 | 64.77 | 53 | 41.78 |
| 25 | Barczak, 2001 | 33 | PU | Uni | 4 | 16 | 69.21 | 17 | 44.04 |
| 26 | Carley, 1985 | 30 | Mixed | Uni | 5 | 15 | 83.46 | 15 | 37.92 |
| 27 | Feedar, Kloth, 1991 | 50 | Mixed | Uni | 4 | 26 | 56.18 | 24 | 32.82 |
| 28 | Franek, 2006 | 55 | VLU | Uni | 7 | 28 | 42.05 | 27 | 28.27 |
| 29 | Franek, 2012 | 50 | PU | Uni | 6 | 26 | 68.83 | 24 | 23.24 |
| 30 | Houghton, 2003 | 42 | VLU | Uni | 4 | 22 | 44.30 | 20 | 16.00 |
| 31 | Houghton, 2010 | 34 | PU | Uni | 12 | 16 | 37.02 | 18 | 13.83 |
| 32 | Jankovic, 2008 | 43 | VLU | Bi | 3 | 24 | 89.62 | 19 | 56.42 |
| 33 | Junger, 2008 | 39 | VLU | Uni | 16 | 20 | 15.11 | 19 | 3.04 |
| 34 | Peters, 2001 | 40 | DFU | Uni | 12 | 20 | 56.09 | 20 | 34.17 |
| 35 | Petrofsky, 2010 | 20 | DFU | Bi | 4 | 10 | 68.40 | 10 | 30.10 |
| 36 | Wood, 1993 | 74 | PU | Uni | 8 | 43 | 60.37 | 31 | 6.77 |
| Total/average | 876 | PU: 6 | Uni: 11 | 6.53 | 497 | 57.08 | 379 | 29.34 | |
| VLU: 4 | Bi: 4 | ||||||||
| DFU: 3 | |||||||||
| Mixed: 2 | |||||||||
Ctr, control group; DFU, diabetic foot ulcers; Exp, experimental group; PAR4, percentage area reduction in 4 weeks; PU, pressure ulcers; VLU, venous leg ulcers.
Results of the meta-analysis
The descriptive statistics in Table 2 shows that the 379 wounds treated with SWC (SWC alone or SWC combined with placebo ES) reduced their surface area in 4 weeks of treatment by 29.3%. Needless to say, many variables have an influence on wound healing, for example, ulcer duration, initial surface area, and comorbidities are prognostic factors related to treatment results; so different studies include different patients with different wounds and different results. PAR4 values vary from 3.0%33 to 56.4%32; both studies concern VLU, but Junger et al.33 included wounds with a mean duration of 42 months, whereas Jankovic et al.32 included wounds with a mean duration of 10 weeks. The mean PAR4 in the 15 studies that applied ES was 57.0%; so the application of additional ES increases wound reduction by an extra 27.7%. The forest plot of these comparisons, all wounds with all types of ES with SWC+ES and SWC alone is presented in Fig. 1.
Figure 1.
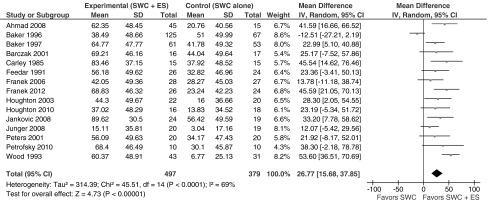
Forest plot with the results of all 15 studies (left column)22–36 on all wound types comparing the mean differences between the experimental group (SWC plus ES) and the control group (SWC alone or SWC plus placebo ES). ES, electrostimulation; SWC, standard wound care; CI, confidence interval.
Fig. 1 shows that 14 of 15 studies have a positive mean difference (mean wound reduction of SWC with additional ES—mean wound reduction of SWC alone). In seven studies, the 95% confidence interval is completely positive (above 0), meaning that the probability that the increased healing is based on coincidence is smaller than 5% (p<0.05). The sum of the mean differences divided by the number of studies is +26.7% with a 95% confidence interval of +15.6 to +37.8%, meaning that this difference in favor of ES is both clinically relevant (it almost doubles the healing rate) and statistically significant (p<0.05). Many factors like wound prognosis, type of skin wound, duration at the start, type of ES, ES stimulus characteristics, possible comorbidities, and method of measurement have an influence on the results, so heterogeneous results can be predicted. This clinical heterogeneity caused by the above-mentioned differences in clinical trials can also lead to statistical heterogeneity. Statistical heterogeneity quantifies if the amount of differences between the results of effect studies is larger than one would expect is based on coincidence (random error). To determine the statistical heterogeneity, the Chi2 test is included to assess whether differences are based on coincidence or not; in case of a low p-value (p<0.1), the differences are not based on coincidence, but statistical heterogeneity is present.41 Another way to quantify inconsistency is to determine the I2 test by relating the Chi2 to the number of included effect studies (I2=[Chi2 − n/Chi2]×100%); if I2 is higher than 50%, substantial heterogeneity is present.42 So, in fact, analyzing different clinical studies in a context of healing wounds with many variables, a certain amount of heterogeneity is inevitable. Strategies to address heterogeneity are the application of a more conservative random effects meta analysis.41 In addition, the challenge is rising to evaluate if heterogeneity disappears in stratified subgroup analyses. The type of ES waveform (unidirectional or bidirectional) is one of the key factors that influences the results and the fact that the rationale for ES is more related to unidirectional ES, stratified analyses were performed with the 11 RCT studies that applied unidirectional ES and the 4 studies that applied bidirectional ES (Table 2, 5th column). The forest plots for both ES waveform types are presented in Figs. 2 and 3 and show that the results of unidirectional ES (extra PAR4=30.8%; 95% confidence interval [CI] 20.9, 40.6) are clearly better than for bidirectional ES (extra PAR4=18.3%; 95% CI −7.1, 43.7). In the analysis of unidirectional ES in all wound types (Fig. 2), heterogeneity is decreased (p=0.07; I2=41%), but the analysis is still performed randomly.
Figure 2.
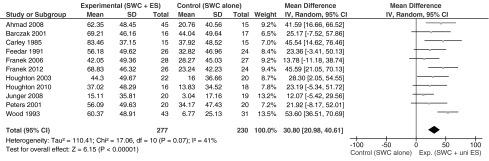
Forest plot with the results of the 11 studies (left column)22,25–31,33,34,36 that applied unidirectional ES on all wound types comparing the mean differences between the experimental group (SWC plus ES) and the control group (SWC alone or SWC plus placebo ES).
Figure 3.
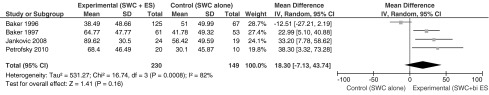
Forest plot with the results of the four studies (left column)23,24,32,35 that applied bidirectional ES on all wound types comparing the mean differences between the experimental group (SWC plus ES) and the control group (SWC alone or SWC plus placebo ES).
The most evaluated wound type is PU. Table 2 (4th column) shows six RCTs, where ES was used in the treatment of PU, five studies applied unidirectional ES (Ahmad 2008, Barczak 2001, Franek 2012, Houghton 2008, Wood 1993), and one study applied bidirectional ES (Baker 1997). The forest plot of that compared SWC plus additional unidirectional ES with SWC without unidirectional ES is presented in Fig. 4 and shows homogeneous results (p=0.34, I2=12%; fixed analysis performed) of an extra wound-healing effect of 42.7% after 4 weeks treatment with unidirectional ES (95% CI 32.0, 53.3).
Figure 4.
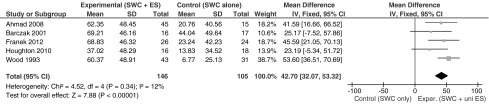
Forest plot with the results of the five studies (left column)22,25,29,31,36 that applied unidirectional ES on pressure ulcers comparing the mean differences between the experimental group (SWC plus ES) and the control group (SWC alone or SWC plus placebo ES).
The mean PAR4 in the SWC group was 21.6%, whereas the mean PAR4 in the SWC+unidirectional ES was 59.5%. In the forest plot with corrections for the weight of the studies, the mean difference was more than 40%. In all five studies, the unidirectional ES was applied with the active electrode directly in the wound.
Discrepancy between current status/evidence and practical use
Based on a large number of RCTs, five reviews and the analysis described in paragraph 3, ES is an intervention with satisfying external evidence. Nonetheless, in wound-healing practice settings, ES is not generally used in a systematic way and also appears not to be an important topic described in guidelines or presented at plenary sessions at wound-healing congresses. In EBM, there are, beside external evidence, two other factors described: clinical expertise and expectations and preferences of practitioners and patients.43 If a practitioner is uncertain as to how to apply an intervention, and is not familiar with the theory and practice of that intervention and if patients and practitioners have no experience, there also are no positive expectations. These two last mentioned factors of EBM can hinder an intervention with just convincing external evidence as the main characteristic. In daily practice, other factors have a significant influence on the choice of interventions included in the treatment plan. Factors like having the proper equipment plus accessories, is the treatment time sufficient to use the intervention, can the patient or partner of the patient apply the intervention, and is the patient's insurance plan willing to pay for the intervention, are all important issues in the clinical reasoning process.
Many of these accompanying factors negatively effect whether ES will be utilized for wound-healing treatment. In most countries, the health care professionals who receive formal education about ES are physical therapists who often are not intensively involved in wound treatment, whereas the professionals most frequently involved in the treatment of patients with wounds are specialized wound nurses or medical specialists who are not familiar with the application of ES. So translating the external research findings to clinical practice is imperative in moving the use of ES forward in wound-healing practice. Clinicians should improve practical competences to be able to apply ES appropriately.
SWC or extra interventions needed
SWC should be well known in theory and practice, easy to apply, and clearly described in guidelines. SWC should be the first choice treatment in the majority of patients. Wounds tend to become a chronic problem and because the treatment time is very often long, patients and therapists should estimate early in the treatment process if SWC alone is expected to be effective. If in 4 weeks a wound area decreases more than 40%, there is a good chance that wound closure will occur with an additional 8 weeks of treatment.40 That is our motivation to describe the PAR4 as a simultaneous outcome measure and a prognostic factor. If the clinician has measurement tools with satisfying agreement, the evaluation of PAR4 is a helpful strategy to determine if SWC alone is satisfying or if an extra intervention with ES to increase wound healing is indicated.44–46
Conclusions
Summary of results
Applying additional unidirectional ES to a program of SWC increases the reduction in the wound surface area in 4 weeks of treatment by an extra 30% (95% CI 20.9, 40.6). In the best studied wound type (PU), these results increase to an extra wound reduction in 4 weeks of treatment by 42.7% (95% CI 32.0, 53.3). In PU care, there is clear motivation to apply unidirectional ES; in other wound types like VLU and DFU, also bidirectional ES can realize positive results.
Pros and cons of clinical application of ES
The main motivation for the application of ES is its proven effectiveness for wound healing expressed in increased healing rates. Further, ES is a safe treatment with minimal if any adverse effects. If appropriate equipment is available, patients, with the help of partners, can apply part of the treatment self. Besides the improved wound healing, many patients also have reported a decrease of wound-related pain.32,33
Drawbacks for ES are the time needed to set up treatment and the fact that aside from physical therapists, not many clinicians are competent or have the appropriate equipment to apply the intervention correctly. Education and training will be necessary to apply ES in wound healing in a systematic way.
Take-Home Messages.
A clear and positive recommendation is available regarding the effectiveness of ES to increase wound healing. The application of unidirectional ES directly in the wound in the treatment of PU is most effective by increasing wound area reduction with an extra 40% in 4 weeks of treatment.
If SWC has disappointing effects that can be quantified as an initial wound healing in 4 weeks of less than 40%, the clinician should choose additional treatment and among the options, ES is an evidence-based application with proven effectiveness.
Supplementary Material
Abbreviations and Acronyms
- DFU
diabetic foot ulcers
- EBM
evidence-based medicine
- EF
electric field
- EPUAP
European Pressure Ulcer Advisory Panel
- ES
electrical stimulation
- ET
electrotherapy
- NPUAP
National Pressure Ulcer Advisory Panel
- PAR4
percentage area reduction in 4 weeks
- PU
pressure ulcers
- RCT
randomized controlled trial
- SR
systematic review
- SWC
standard wound care
- TEP
transepithelial potential
- VLU
venous leg ulcers
Author Disclosure And Ghostwriting
For both authors, there are no conflicts of interest and no financial interests exist. The text was expressly written by the two authors. No ghost-writers were used to write this article.
About the Authors
Gerard Koel is a physical therapist and manual therapist. He works part time as a teacher and researcher at the Saxion University of Applied Sciences. He is strongly involved in the three Master educations of the Faculty. In addition, he has developed several postacademic courses about shoulder pain and lower back pain. He works part time in the Wooldersteen physical therapy practice in Hengelo. Pamela E. Houghton is a physical therapist and PhD. She is an associate professor at the School of Physical Therapy, University of Western Ontario, London, Ontario, Canada. She coordinates several Master's students, has written a number of RCT effect studies on the field of wound healing, and presents regularly at international congresses on wound healing.
References
- 1.Foulds IS. and Barker AT: Human skin battery potentials and their possible role in wound healing. Br J Dermatol 1983; 109:515. [DOI] [PubMed] [Google Scholar]
- 2.McCaig CD, Rajinec AM, Song B, and Zhao M: Controlling cell behavior electrically: current views and future potential. Physiol Rev 2005; 85:943. [DOI] [PubMed] [Google Scholar]
- 3.Nishimura KY, Isseroff RR, and Nuccitelli R: Human keratinocytes migrate to the negative pole in direct current electrical field comparable to those measured in mammalian wounds. J Cell Sci 1996; 109:199. [DOI] [PubMed] [Google Scholar]
- 4.Li L, Gu W, Du J, Reid B, Deng X, Liu Z, Zong Z, Wang H, Yao B, Yang C, Yan J, Zeng L, Chalmers L, Zhao M, and Jiang J: Electric fields guide migration of epidermal stem cells and promote skin wound healing. Wound Repair Regen 2012; 20:840. [DOI] [PubMed] [Google Scholar]
- 5.Posnett J, Gottrup F, Lundgren H, and Saal G: The resource impact of wounds on health-care providers in Europe. J Wound Care 2009; 18:154. [DOI] [PubMed] [Google Scholar]
- 6.Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, and Thornton H: “The 2011 Oxford CEBM Levels of Evidence (Introductory Document)”. Oxford Centre for Evidence-Based Medicine. www.cebm.net/index.aspx?o=5653
- 7.Nelson EA. and Bradley MD: Dressings and topical agents for arterial leg ulcers. Cochrane Database Syst Rev 2007: CD001836. [DOI] [PubMed] [Google Scholar]
- 8.Vermeulen H, van Hattem JM, Storm-Versloot MN, and Ubbink DT: Topical silver for treating infected wounds. Cochrane Database Syst Rev 2007: CD005486. [DOI] [PubMed] [Google Scholar]
- 9.Ubbink DT, Westerbos SJ, Evans D, Land L, and Vermeulen H: Topical negative pressure for treating chronic wounds. Cochrane Database Syst Rev 2008: CD001898. [DOI] [PubMed] [Google Scholar]
- 10.Al-Kurdi D, Bell-Syer SEM, and Flemming K: Therapeutic ultrasound for venous leg ulcers. Cochrane Database Syst Rev 2010: CD001180. [DOI] [PubMed] [Google Scholar]
- 11.Jull AB, Rodgers A, and Walker N: Honey as a topical treatment for wounds. Cochrane Database Syst Rev 2008: CD005083. [DOI] [PubMed] [Google Scholar]
- 12.Palfreyman SSJ, Nelson EA, Lochiel R, and Michaels JA: Dressings for healing venous leg ulcers. Cochrane Database Syst Rev 2006: CD001103. [DOI] [PubMed] [Google Scholar]
- 13.Bergin S. and Wraight P: Silver based wound dressings and topical agents for treating diabetic foot ulcers. Cochrane Database Syst Rev 2006: CD005082. [DOI] [PubMed] [Google Scholar]
- 14.O'Meara S, Cullum NA, and Nelson EA: Compression for venous leg ulcers. Cochrane Database Syst Rev 2009: CD000265. [DOI] [PubMed] [Google Scholar]
- 15.Selim P, Bashford C, and Grossman C: Evidence-based practice: tap water cleansing of leg ulcers in the community. Cochrane Database Syst Rev J Clin Nurs 2001; 10:372. [DOI] [PubMed] [Google Scholar]
- 16.Kloth LC: Electrical stimulation for wound healing: a review of evidence from in vitro studies, animal experiments, and clinical trails. Lower Extremity Wounds 2005; 4:23. [DOI] [PubMed] [Google Scholar]
- 17.Sussman C: Electrical stimulation for wound healing. In: Wound Care, a Colaborative Practice Manual for Health Professionals, 3rd edition, edited by Sussman C. and Bates-Jensen BM. Philadelphia: Wolters Kluwer, Chapter 22, 2006, p. 505 [Google Scholar]
- 18.Balakatounis KC. and Angoules AG: Low-intensity electrical stimulation in wound healing: review of the efficacy of externally applied currents resembling the current of injury. J Plast Surg 2008: 283. [PMC free article] [PubMed] [Google Scholar]
- 19.Ramadan A, Elsaidy M, and Zyada R: Effect of low-intensity direct current on the healing of chronic wounds: a literature review. J Wound Care 2008; 17:292. [DOI] [PubMed] [Google Scholar]
- 20.Collins C, Roberts G, Zhao M, and Mani R: The use of electrical stimulation of chronic wounds: a review of the evidence. J Wound Technol 2009; 6:10 [Google Scholar]
- 21.EPUAP/NPUAP: Treatment of Pressure Ulcers: Quick Reference Guide; Washington DC, www.npuap.org, 2009 [Google Scholar]
- 22.Ahmad ET: High voltage pulsed galvanic stimulation: effect of treatment durations on healing of chronic pressure ulcers. Indian J Physiother Occup Ther 2008; 2:1. [PMC free article] [PubMed] [Google Scholar]
- 23.Baker LL, Rubayi S, Villar F, and DeMuth SK: Effect of electrical stimulation waveform on healing of ulcers in human beings with spinal cord injury. Wound Repair Regen 1996; 4:21. [DOI] [PubMed] [Google Scholar]
- 24.Baker LL, Chambers R, DeMuth SK, and Villar F: Effects of electrical stimulation on wound healing in patients with diabetic ulcers. Diabetes Care 1997; 20:405. [DOI] [PubMed] [Google Scholar]
- 25.Barczak M, Kluger P, Kluger J, Bauerle J, and Puhl W: Therapeutic Effectiveness of Electric Stimulation in Paraplegic Patients with Pressure Sores. PhD thesis of M. Barczak submitted to Prof. Dr. W. Puhl at the Medical School of the University of Ulm, Germany 12January2001 [Google Scholar]
- 26.Carley P. and Wainapel S: Electrotherapy for acceleration of wound healing; low intensity direct current. Arch Phys Med Rehabil 1985; 66:443. [PubMed] [Google Scholar]
- 27.Feedar JA, Kloth LC, and Gentzkow GD: Chronic dermal ulcer healing with monophasic pulsed electrical stimulation. Phys Ther 1991; 71:639. [DOI] [PubMed] [Google Scholar]
- 28.Franek A, Taradaj J, Polak A, Cierpka L, and Blasczak E: Efficacy of high voltage stimulation for healing of venous leg ulcers in surgically and conservatively treated patients. Phlebologie 2006; 35:127 [Google Scholar]
- 29.Franek A, Kostur R, Polak A, Taradaj J, Szlachta Z, Blasczak E, Dolibog P, Dolibpg P, Koczy B, and Kucio C: Using high voltage electrical stimulation in the treatment of recalcitrant pressure ulcers, results of a randomized, controlled clinical study. Ostomy Wound Manage 2012; 58:30. [PubMed] [Google Scholar]
- 30.Houghton PE, Kincaid CB, Lovell M, Campbell KE, Keast DH, Woodbury G, and Harris KA: Effect of electrical stimulation on chronic leg ulcer size and appearance. Phys Ther 2003; 83:17. [PubMed] [Google Scholar]
- 31.Houghton PE, Campbell KE, Fraser C, Harris C, and Woodbury MG: Electrical stimulation therapy increases healing of pressure ulcers in community dwelling people with spinal cord injury. Arch Phys Med Rehabil 2010; 91:669. [DOI] [PubMed] [Google Scholar]
- 32.Jankovic A. and Blinic I: Frequency rhythmic electrical modulation system in the treatment of chronic painful leg ulcers. Arch Dermatol Res 2008; 300:377. [DOI] [PubMed] [Google Scholar]
- 33.Junger M, Arnold A, Zuder D, Stahl HW, and Heising S: Local therapy and treatment costs of chronic, venous leg ulcers with electrical stimulation (Dermapulse): a prospective, placebo controlled double blind trial. Wound Repair Regen 2008; 16:480. [DOI] [PubMed] [Google Scholar]
- 34.Peters EJ, Lavery LA, Armstrong DG, and Fleischli JG: Electric stimulation as an adjunct to heal diabetic foot ulcers: a randomized clinical trial. Arch Phys Med Rehabil 2001; 82:721. [DOI] [PubMed] [Google Scholar]
- 35.Petrofsky JS, Lawson D, Berk L, and Suh H: Enhanced healing of diabetic foot ulcers using local heat and electrical stimulation for 30 minutes three times a week. J Diabetes 2010; 2:41. [DOI] [PubMed] [Google Scholar]
- 36.Wood JM, Evans PE, Schallreuter KU, Jacobson WE, Sufit R, Newman J, White C, and Jacobson M: A multicenter study on the use of pulsed low-intensity direct current for healing chronic stage II and stage III decubitus ulcers. Arch Dermatol 1993; 129:999. [PubMed] [Google Scholar]
- 37.Kantor J. and Margolis DJ: A multi-centre study of percentage change in venous leg ulcer area as a prognostic index of healing at 24 weeks. Br J Dermatol 2000; 142:960. [DOI] [PubMed] [Google Scholar]
- 38.Tallman P, Muscare E, Carson P, Eaglstein WH, and Falanga V: Initial rate of healing predicts complete healing of venous ulcers. Arch Dermatol 1997; 133:1231. [PubMed] [Google Scholar]
- 39.Sheehan P, Jones P, Caselli A, Giurini JM, and Veves A: Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a 12-week prospective trial. Diabetes Care 2003; 26:1879. [DOI] [PubMed] [Google Scholar]
- 40.Cardinal M, Eisenbud DE, Philips T, and Harding H: Early healing rates and wound area measurements are reliable predictors of later complete wound closure. Wound Repair Regen 2008; 16:19. [DOI] [PubMed] [Google Scholar]
- 41.Higgins JPT. and Green S: Cochrane Handbook for Systematic Reviews of Interventions. Chichester: Wiley-Blackwell, Cochrane book series, 2008 [Google Scholar]
- 42.Higgins JPT, Thompson SG, Deeks JJ, and Altman DG: Measuring inconsistency in meta analysis. BMJ 2003; 327:557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sackett DL, Richardson WS, Rosenberg W, and Haynes BR: Evidence-Based Medicine: How to Practice and to Teach EBM. Edinburgh: Churchill-Livingstone, 1997 [Google Scholar]
- 44.Cutler NR, George R, Seifert RD, Brunelle R, Sramek JJ, McNeill K, and Boyd WM. Comparison of quantitative methodologies to define chronic pressure ulcer measurement. Decubitus 119; 6:22. [PubMed] [Google Scholar]
- 45.De Vet HCW, Terwee CB, Knol DL, and Bouter LM: When to use agreement versus reliability measures. J Clin Epidemiol 2006; 59:1033. [DOI] [PubMed] [Google Scholar]
- 46.O'Meara SM, Bland JM, Dumville JC, and Cullum NA. A systematic review of the performance of instruments designed to measure the dimensions of pressure ulcers. Wound Repair Regen 2012; 20:263. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


