Abstract
Personality disorders have been defined as “stable over time”. However, research now supports marked change in the symptoms of these disorders and significant individual variability in the trajectories across time. Using the Longitudinal Study of Personality Disorders, we explore the ability of the Revised Interpersonal Adjective Scales – Big Five (IASR-B5; Trapnell & Wiggins, 1990) to predict individual variation in initial value and rate of change in borderline personality disorder symptoms. The dimensions of the IASR-B5 predict variability in initial symptoms and rates of change. Interaction effects emerged between Dominance and Conscientiousness, Love and Neuroticism, and Conscientiousness and Neuroticism in predicting initial symptoms, and between Dominance and Love, and Love and Neuroticism in predicting rates of change suggesting that the effects of broad domains of personality are not merely additive but conditional on each other.
Keywords: Borderline Personality Disorder, Longitudinal Study of Personality Disorders, Interpersonal Adjective Scales, Interpersonal Circumplex
“There is nothing wrong with change, if it is in the right direction” - Winston Churchill
One of the cardinal features of the personality disorders (PD) as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM; American Psychiatric Association [APA], 2000) is that they are “enduring” and “stable over time” (p. 685). However, the data from a number of large prospective longitudinal studies converge in the finding that PDs are not as stable as once thought (Cohen, Crawford, Johnson, & Kasen, 2005; Johnson et al., 2000; Lenzenweger, 1999; Skodol et al., 2005; Zanarini, Frankenburg, Hennen, & Silk, 2003). Evidence has accumulating that this group of disorders does, in fact, demonstrate marked change over time (Skodol, 2008). These results point towards a hope filled reconceptualization of PD as a diagnosis that can and does change. This is good news, as these disorders have been shown to be highly prevalent (Lenzenweger, Lane, Loranger, & Kessler, 2008; Lenzenweger, Loranger, Korfine, & Neff, 1997) and very costly at both personal (Yen et al., 2005) and societal levels (Bender et al., 2001). On the other hand, this places the burden on researchers and clinicians to develop etiological, descriptive, diagnostic, and treatment models that accommodate this emerging view that now argues against PD as a rigid and inflexible form of psychopathology. As part of these new efforts, personality assessment can no longer treat the assessment of PD as the assessment of a static entity. The implication for personality assessment is that it must also move beyond capturing static “snapshots” of functioning in PD, and move towards measuring the dynamic elements of stability and change in functioning and disorders. Therefore, it is important to establish what the individual risk and protective factors are that augment or mitigate an individual’s trajectory of change. The current study joins this new call in assessment science (e.g., Baird, Le, & Lucas, 2006; Hertzog & Nesselroade, 2003; Ram & Gerstorf, 2009) by examining the basic personality predictors of long-term stability and change in borderline personality disorder (BPD). This study uses the Revised Interpersonal Adjective Scales – Big Five (IASR-B5; Trapnell & Wiggins, 1990) and data from the Longitudinal Study of Personality Disorder (LSPD; Lenzenweger, 2006) to accomplish this.
A number of large-scale naturalistic studies of PD have assessed the longitudinal stability of PD diagnoses and symptom criteria. The Collaborative Longitudinal Study of Personality Disorder has focused on the diagnoses of Avoidant, Borderline, Obsessive-Compulsive, and Schyzotypal PD (Skodol et al., 2005). Results of this study show that there are significant declines in the number of individuals meeting diagnostic threshold, and accordingly significant declines in symptoms when treated as dimensions (Shea et al., 2002). Similar results have emerged from the McLean Study of Adult Development, which is limited to BPD patients, with 75% of the initially diagnosed sample not meeting diagnostic threshold at six year follow up (Zanarini et al., 2003). That number increased to 88% at 10 year follow up, with relatively low incidence of recurrence (6%; Zanarini et al., 2006). These studies used clinic/hospital samples and were limited to one or a subset of the PDs.
In contrast, the Children in the Community study (CIC; Cohen et al., 2005) and the LSPD (Lenzenweger, 2006) have both studied PD longitudinally in non-clinical samples. The CIC study reported a 28% to 48% reduction in PD symptom counts going from adolescence to young adulthood (Johnson et al., 2000). The LSPD, which has also tracked all of the DSM defined personality disorders, mirrors the other studies in demonstrating generally significant decline in PD symptoms over time (Lenzenweger, 1999). Antisocial and Paranoid PD are exceptions which demonstrate symptom increase and stability, respectively, over the four-year course of the study. The LSPD has taken these results further by examining the interindividual variability in trajectories of change within an individual growth curve analytic framework. Results indicate that the mean decline in the whole sample masks significant interindividual heterogeneity in symptom change over time (Lenzenweger, Johnson, & Willett, 2004). Although on the average individuals decline in the number of criteria they meet, some show stability over time, and others increase in criteria over time. Therefore, it is important to elucidate the influential aspects of individuals and their environment that act as risk and protective factors in augmenting or mitigating an individual’s trajectory of change.
Undoubtedly, the influences on individual trajectories in psychopathology generally, and PD more specifically, are multiple. Notwithstanding, contemporary models of personality disorder argue for the direct links between basic personality/temperament and disordered personality functioning (e.g., Clark, 2007; Depue & Lenzenweger, 2001, 2005, 2006; Pincus, 2005; Pincus, Lukowitsky, & Wright, 2010; Widiger & Simonsen, 2005). Therefore the immediate avenue of research leads towards elucidating the underlying basic personality and temperament factors that predict stability and change in PD (Lenzenweger & Willet, 2007). Indeed, Lenzenweger and colleagues (Lenzenweger & Castro, 2005; Lenzenweger & Willet, 2007) have already commenced this work using the Depue and Lenzenweger Model (DLM; Depue & Lenzenweger, 2001, 2005, 2006) as an organizing and predictive framework for the dynamic waning and surging of PD over time. The DLM posits a model of interactive neurobehavioral systems that impact both normal and abnormal personality functioning. Within this system, underlying neurobehavioral systems are linked with higher-order personality processes. These systems are manifested in the following personality traits: (a) agentic extraversion, (b) affiliation, (c) negative emotion, (d) fear or harm avoidance, and (e) nonaffective constraint (i.e., control).
The DLM has been used as a predictor of variability and change in PD in two studies using the LSPD. In the more recent of these studies, the DLM served as a predictor for the symptom counts from each of the three DSM clusters of PD within a multivariate latent growth curve framework (Lenzenweger & Willet, 2007). Although the specific results are beyond the scope of this review, in general the DLM’s conceptualizations of personality dimensions were successful in predicting the variability in initial value and rate of change in PD symptoms. More relevant to the current study, Lenzenweger & Castro (2005) used the DLM as assessed at the first wave of the LSPD data collection as a predictor of BPD criteria—both symptom counts at the outset of the study and change over time. Results of this study indicated that when it came to predicting interviewer assessed BPD symptoms, fear and nonaffective constraint were associated with lower initial BPD symptoms, whereas negative emotion and agentic extraversion were positively associated with BPD symptom counts. These dimensions were also significant predictors of change; however, the directions of the associations were opposite. Thus, the DLM has proved quite useful in predicting the interindividual variability in PD criteria, both concurrently and as they change over time.
We propose that two additional interrelated models of personality are fruitful avenues of inquiry—the interpersonal circumplex (IPC) and the five-factor model (FFM). The IPC maps two of the neural systems and neurobehavioral processes used in the DLM (Depue & Collins, 1999; Depue & Lenzenweger, 2001, 2005, 2006; Depue & Marone-Strupinsky, 2005), whereas the FFM differs in critical ways (Lenzenweger & Willett, 2007). The Interpersonal paradigm (e.g., Leary, 1957; Pincus et al., 2010; Wiggins, 2003) has conceptualized personality as “the relatively enduring pattern of recurrent interpersonal situations that characterize a human life” (Sullivan, 1953, pp. 110-111). The interpersonal approach to personality utilizes a two-dimensional circumplex model based on the metaconcepts of Agency and Communion (Bakan, 1966; Wiggins, 1991, 2003). Agency refers to the notion of individuation, autonomy, and directedness, whereas Communion refers to associating, involvement, and sharing with others. Alternatively, Agency has been referred to as Power or Dominance, and Communion as Love or Warmth. These dimensions serve as the axes of the IPC (Wiggins, 1996) and are presumed to underlie functioning at the motivational (Horowitz, 2004; Horowitz et al., 2006; Locke, 2000), trait (Wiggins, 1979), cognitive (Locke & Sadler, 2007; Tracey & Rohlfing, 2010), behavioral (Moskowitz, 1994, 2005), and problematic (Alden, Wiggins, & Pincus, 1990) levels of interpersonal functioning. The IPC is rooted in both theoretical (Sullivan, 1953; Leary, 1957) and empirical (Wiggins, 1982) foundations and therefore serves as a powerful nomological net for the study of behavior, personality, and psychopathology (Pincus & Gurtman, 2006; Pincus et al., 2010; Pincus, Lukowitsky, Wright, & Eichler, 2009; Pincus & Wright, in press).
Furthermore, the dyadic-interactional perspective of the popular FFM (Wiggins & Trapnell, 1996) places Agency and Communion as the first two of the five factors, joined by Neuroticism, Conscientiousness, and Openness. And indeed, more conventional articulations of the first two dimensions of the FFM, Extraversion and Agreeableness, have found them to be rotational variants of Agency and Communion (McCrae & Costa, 1989; Pincus, 2002). The dyadic-interactional perspective of the FFM further argues that the remaining three factors each contain Agentic and Communal aspects (e.g., Ansell & Pincus, 2004), and that each influences interpersonal motivations and striving. For example, an Agentic expression of Conscientiousness might be “decisiveness”, whereas a Communal expression might be “dependability”. Expressions of Neuroticism that are associated with low Agency or low Communion may be respectively found in “depression” and “angry hostility”. Finally, Agentic and Communal expressions of Openness can be found in “intelligence” and “feelings” respectively (see Wiggins & Trapnell, 1996 for a complete discussion).
Both the IPC and the FFM have a strong history of being used to articulate differences between the PDs (Widiger & Simonsen, 2005). Given the ubiquitous nature of interpersonal dysfunction in PD (Livesley, 2001), the IPC has often been proposed as a model that can serve as a basis for characterizing PD (APA, 2000; Haslam, 2003; Horowitz, 2004; Pincus, 2005; Widiger & Simonsen, 2005) and many empirical studies confirm this (e.g., Gurtman, 1996; Morey, 1985; Pincus & Wiggins, 1990; Soldz, 1997; Soldz, Budman, Demby, & Merry, 1993; Wiggins & Pincus, 1989). Paralleling PD research in general, a significant amount of recent empirical work relating the IPC to PD has focused on Borderline PD (Hilsenroth, Menaker, Peters, & Pincus, 2007; Ryan & Shean, 2007; Leichsenring, Kunst, & Hoyer, 2003; Leihener et al., 2003). Notably, although BPD (and borderline pathology more generally) is clearly a disorder with strong interpersonal features, it evades a clear association with any specific location on the IPC when assessed cross-sectionally. Soldz et al. (1993) found borderline pathology to be associated with extraverted-intrusive interpersonal problems, whereas Hilsenroth et al. (2007), Morey (1985), and Sim and Romney (1990) have found it to be associated with dependent-exploitable interpersonal problems. Moreover, Ryan and Shean (2007) and Leihener and colleagues (2003) found two clusters of BPD based on interpersonal problems associated contrastingly with dependant-exploitable and hostile-vindictive expressions. Wright, Pincus, Conroy, and Hilsenroth (2009) found two clusters of BPD associated with exploitable and nonassertive interpersonal problems. Leichsenring et al. (2003) found that different symptoms of borderline pathology loaded in different locations of interpersonal circumplex space. These accumulating results support early assertions that BPD does not map onto a specific location in interpersonal circumplex space (Pincus & Wiggins, 1990; Wiggins & Pincus, 1989, 1994). What is undoubtedly the case is that BPD does not load uniformly in interpersonal space at a single time-point, as the interpersonal features of BPD, although prominent, are characterized by instability and oscillation. In contrast, the FFM profile of BPD is more consistent, with the metanalytical result that BPD is strongly positively associated with Neuroticism, and moderately negatively associated with Agreeableness and Conscientiousness, with no consistent association with Extraversion or Openness (Saulsman & Page, 2004).
The current study aims to build on prior work that has mapped BPD onto the IPC and FFM cross-sectionally, by examining the ability for these models to predict the stability of BPD criteria longitudinally within the LSPD. The interpretive framework here is the dyadic-interactional perspective of the FFM, therefore we adopt the view that the dimensions of normal personality, although presumed to be orthogonal in the population, are not orthogonal within individuals—especially in the context of an individual’s life trajectory. Quite the contrary, it is expected that the basic dimensions of personality will mutually influence each other, interacting synergistically to predict the features of BPD across a developmental epoch. This approach is rarely taken in the broader FFM literature, with very few exceptions (viz. Morey, 2002). Furthermore, these analyses were performed on cross-sectional data. By looking longitudinally and interactionally within an individual growth curve framework, this study adopts a more person centered approach in the study of the relationship between personality and its pathology. Longitudinal data captures the very important dynamic interplay between an individual’s personality and their environment in the maintenance of personality pathology. Additionally, the exploration of interaction effects examines the within individual personality dynamics that might elucidate trajectory types. This study is meant to serve as an early step in an approach towards quantitative personality assessment that more approximates studying individuals within the context of their lives.
The focus of the current study is on the predictive power of these normal personality dimensions as assessed at the outset of the study, in much the same way as they might be assessed in the context of a referral, consultation, or beginning of treatment. The measure employed is the IASR-B5, which is an augmented version of the popular Interpersonal Adjective Scales (IAS; Wiggins, 1995). Added to the two IAS dimensions of Dominance (Agency) and Love (Communion), this measure includes three additional bipolar scales that measure Neuroticism, Conscientiousness, and Openness (Trapnell & Wiggins, 1990). The IASR-B5, like its parent measure the IAS, assesses personality based on ratings of trait-adjectives. In keeping with the goal of placing this study within the larger clinical personality assessment literature, the outcome measure will be clinician assessed BPD criteria, as is generally the case in clinical practice. It is important to note here that the burden of predicting the change in clinician assessed BPD symptoms up to four years out is a taxing one for any measure. Thus this study features not only a longitudinal design, but a heteromethod design, where self-ratings on trait descriptive adjectives are used to predict clinician judgment of disordered functioning (Meyer et al., 2001).
Methods
Participants
The 258 participants in the LSPD (Lenzenweger, 1999; Lenzenweger et al., 1997, 2004) were drawn from a population consisting of 2,000 first-year undergraduate students. Extensive detail concerning the initial participant selection procedure and sampling is given elsewhere (Lenzenweger, 2006; Lenzenweger et al., 1997). The 258 participants consisted of 121 males (47%) and 137 females (53%). The mean age of the participants at entry into the study was 18.88 years (SD = 0.51). All participants gave voluntary written informed consent and received an honorarium of $50.00 at each wave. Of the initial 258 participants, 250 completed all three assessment waves and are included in this analysis. Sample characteristics are summarized in Table 1.
Table 1. Demographic characteristics of the LSPD sample (N = 250).
| Father (%) | Mother (%) | ||
|---|---|---|---|
| Parents Education | |||
| 1-8 yrs | 1.6 | 0.8 | |
| 9-11 yrs | 2.4 | 2.8 | |
| 12 yrs | 8.4 | 15.2 | |
| 13-15 yrs | 16.0 | 20.4 | |
| 16+ yrs | 68.8 | 58.8 | |
| Not available | 2.8 | 2.0 | |
| Parents Occupation | |||
| Laborer/Service | 2.0 | 2.4 | |
| Operatives (Machine) | 2.8 | 1.2 | |
| Craftsman/Foreman | 3.2 | 1.6 | |
| Clerical/Sales | 4.0 | 16.8 | |
| Management/Official | 26.8 | 12.8 | |
| Professional/Technical | 52.4 | 42.0 | |
| Not available or Homemaker | 8.8 | 23.2 | |
| Race | (%) | ||
| African-American | 3.6 | ||
| Latino-Hispanic | 4.8 | ||
| Caucasian-Anglo | 72.0 | ||
| Asian-Pacific Islander | 17.2 | ||
| Native American | 0.8 | ||
| Other | 1.6 |
Procedure
PD assessments
As noted above, the LSPD has a prospective multiwave longitudinal design with participants initially evaluated at three points in time (i.e., first, second, and forth years in college). Although not required for application of individual growth modeling (Singer & Willett, 2003), the LSPD data are balanced, in that all participants have three waves of data, and are time structured such that each participant was assessed repeatedly on the same three wave schedule, although the time between assessments varies from case to case. Interview assessments were conducted by experienced Ph.D. or advanced M.S.W. clinicians. Finally, because the LSPD is a naturalistic prospective study, participants were free to seek psychological treatment of their own accord. The PD features of each of the 250 study participants were assessed three times over the 4-year period. The average age of study participants at the assessment waves were 18.88 years (SD = 0.51) for Wave I, 19.83 years (SD = 0.54) for Wave II, and 21.70 years (SD = 0.56) for Wave III. The mean time between entry into the study (Wave I) and Waves II and III was 0.95 years (SD = 0.14) and 2.82 years (SD = 0.23), respectively.
IPDE DSM-III-R screen (IPDE-S)
This is a 250-item self-administered true-false PD screening inventory developed by A. W. Loranger. The diagnostic efficiency and psychometric properties of the IPDE-S in a two-stage screen application were described previously (Lenzenweger, 2006; Lenzenweger et al., 1997). Participants were assigned to either a “possible PD” (PPD) or “no PD” (NPD) group according to the IPDE-S (response rate = 84.2%) at the outset of the study. PPD participants were those who met the diagnostic threshold for at least one specific DSM-III-R PD, whereas NPD were those participants who (a) did not meet the DSM-III-R defined threshold for diagnosis and (b) had fewer than 10 PD features across all disorders. One-hundred thirty-four participants (66 female) were in the PPD group and 124 (71 female) were in the NPD group. This methodological feature of the study ensured a sufficient sampling of PD criteria within a nonclinical sample, while also retaining what is in essence a control group of individuals who were not immediately presenting with the features of the disorder but who may develop them over the course of the study and thereby also allow for the study of emerging psychopathology.
International Personality Disorder Examination (IPDE)
The IPDE (Loranger, 1988; 1999) was used as the PD measure in this study. It assessed the DSM-III-R criteria for the Axis II disorders. Clinically experienced interviewers received training in IPDE administration and scoring by Dr. A. W. Loranger and were supervised throughout the project by the third author (M.F.L.), who was blind to the participants’ identity, putative PD status, and all prior assessment information. The interrater reliability intraclass correlation coefficients for IPDE assessments were excellent at all three waves, ranging between .84 and .92 for the total score across all the 3-point PD items. The interviewers were (a) blind to the putative PD group status of the participants and (b) blind to all prior LSPD PD assessment data, and (c) the same interviewer did not assess the same participant more than once. The BPD dimensional score from the IPDE was used in this analysis, though reliability data is not available for this specific score. The sample distribution of BPD feature counts was heavily positively skewed as is common for psychopathology variables that are formed from counts, particularly when studied in nonclinical community populations. Thus, we followed standard statistical practices for counted variables, taking a square-root transformation of the raw count as the outcome in our analyses. This reduces the skewness in the raw counts of PD features, linearizes individual growth in PD features over time, and renders the distribution of the residuals in our analysis more hospitable to the required normal theory assumptions.
Revised Interpersonal Adjective Scales – Big Five (IASR-B5)
The IASR-B5 (Trapnell & Wiggins, 1990) is an extended version of the IAS (IAS; Wiggins, Trapnell, & Phillips, 1988). The 64-item IAS consists of eight scales assessing the eight octants of the Wiggins (1979) circumplex. In turn, these can be converted into scores for the two primary dimensions of the IPC: Agency/Dominance/Control and Communion/Love/Warmth. The IASR-B5 augments this measure by including 20-item markers for each of the three FFM factors of Conscientiousness, Neuroticism, and Openness. The three FFM scales of the IASR-B5 correlate highly with the corresponding scales on the NEO Personality Inventory (r’s = .76, .74, and .67, respectively; Trapnell & Wiggins, 1990). Participants responded to each of 124 adjectives (e.g., dominant, coldhearted) on an 8-point scale of self-description. For the current analyses, the five dimensional scores from the IASR-B5 administration at Wave 1 were used as individual level predictors in the individual growth curve models described below.
Structured clinical interview for DSM-III-R— Nonpatient version (SCID-NP)
This is the well-known semistructured DSM-III-R Axis I clinical interview for use with nonpatients (Spitzer, Williams, Gibbon, & First, 1990). The SCID interview was performed first and followed by the IPDE. All interviewers achieved high reliability with criterion cases (all intraclass correlation coefficients > .80 for symptom assessments), though reliability data for this sample is not available. The SCID interview was done first, followed by the IPDE as is customary practice for thorough Axis II assessments. The Axis I diagnostic information generated by the SCID is not a primary focus of this report, although we report the results of these assessments as part of the clinical description of the sample.
Analyses
The analytical approach taken in this study was the individual growth curve (IGC) analysis, sometimes referred to as Hierarchical Linear Modeling, Multilevel Modeling, or Random Coefficients Regression. IGC analyses allow for the investigation of within person change over time (Raudenbush & Bryk, 2002; Singer & Willet, 2003). The dependant variable in this study was the transformed version (i.e., square root) of the IPDE BPD dimensional score. In this analytical framework, measurement occasions (Level 1) are treated as nested within individuals (Level 2). Therefore, each individual has a trajectory of change over time. This trajectory is most often treated as a linear function of time, plus error. This Level 1 model contains two important unknown growth parameters—the intercept and slope—which determine the shape of change over time. The individual intercept parameter represents the mean level of the BPD features for the individual at the onset of the study (or, alternatively, whenever the origin of the time scale has been defined). The individual slope parameter represents the rate of change over time and is the within-person rate of change in BPD features over time in the present study. The advantage of IGC modeling is that the coefficients for these two parameters can be allowed to vary randomly if there is significant interindividual variation in intercept and slope in the sample. That is to say, each individual is allowed to take on their own values for intercept and slope, which in turn can be explained by introducing between-person predictors (e.g., gender, interpersonal and FFM dimensions, age) at Level 2 in the model.
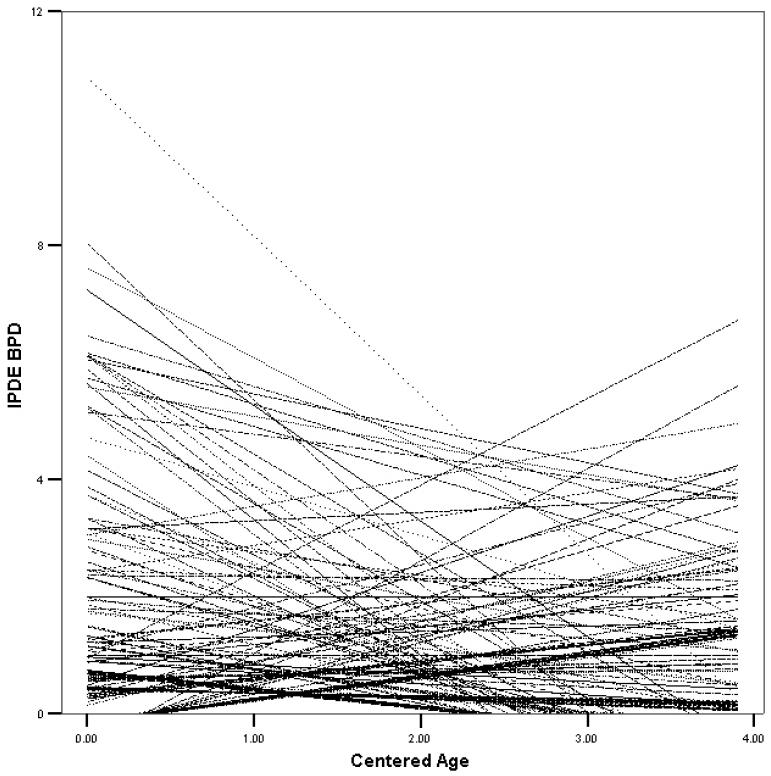
To illustrate, we have included Figure 1 which is a plot of the 250 participants’ individual ordinary least squares fitted regression lines for the outcome measure of IPDE BPD features. The IPDE dimensional score is on the ordinate and time in years centered on participants’ age at enrolment is on the abscissa. Visually the heterogeneity in the number of features at the beginning of the study and rates of change across these individuals is striking. This plot demonstrates the importance of using IGC approaches that allow each individual to retain their own trajectory while also allowing for an investigation of the determinants of these trajectories. The Level 2 model uses between-individual variables to explain this rich individual heterogeneity in growth trajectories. Of importance for interpreting the results of IGC models are the fixed and random (i.e., variance) coefficients. The fixed coefficients can be interpreted straightforwardly in much the same way as basic multiple regression coefficients. These test whether the average effect of the predictor variable is significantly different from zero. In contrast, the random effects test whether significant variability remains unexplained in the outcome variable. In this study, of most interest are the random coefficients associated with the Level 1 intercept and slope parameters. These are and respectively, and indicate whether random variability remains to be explained in the intercept and slope parameters. Additionally, the covariance (σ01) between the intercept and slope is reported, but it is not a focus in this study.
Figure 1.
Ordinary least squares individual growth trajectories for IPDE diagnosed BPD features in 250 participants over the study period. The time is reported in years since the beginning of the study, and it is centered for each participant using the participant’s age at entry into the study. Adapted from Lenzenweger & Castro (2005) with permission from the Cambridge University Press.
In our analyses, the hypothesized Levels 1 and 2 statistical models were fitted simultaneously to the LSPD data using full maximum likelihood estimation and the HLM-6 computer program (Raudenbush, Bryk, Cheong, Congdon, & Du Toit, 2004). Adopting a maximum likelihood approach was supported due to the lack of missing data, the transformation reduced the high degree of skew and kurtosis in the raw data going from 3.03 to 1.35 and 11.16 to .94 respectively, and a post hoc analysis of the residuals indicated they conformed to a normal distribution. We conducted our analyses sequentially. First, we conducted a set of unconditional growth analyses (Singer & Willett, 2003) in which we posited a linear individual change trajectory at Level 1, but did not attempt to predict interindividual variation in the growth parameters by between-participant factors. Such unconditional analyses are useful for partitioning the outcome variation into variance components that describe the net variation in slope and intercept across individuals. Second, we conducted a set of conditional analyses in which we examined systematic interindividual differences in intercept and slope as a function of between-participant predictors, namely study group (PPD vs. NPD), participant gender, and age in years at entry into the study were included as control variables, and the dimensions of IASR-B5 as substantive predictors. These predictors yield fixed effects in the prediction of the slope and intercept values retained from the Level 1 analysis. The fitting of the Level 2 model also yields estimates of residual variance that describe remaining interindividual variability in the individual slopes and intercepts (as well as their covariance) after accounting for the hypothesized fixed effects, giving rise to the variance components (i.e., , , and σ01). Improvement in model fit was assessed by comparison of deviance statistics. Fixed-effects and variance components were tested for statistical significance using the provided t (2-tailed) and χ2 statistics.
Results
Clinical Characteristics of the Sample
The lifetime DSM-III-R Axis I diagnoses for the study participants have been reported previously (Lenzenweger, 1999; Lenzenweger et al., 2004). However, Table 2 summarizes the Axis I diagnoses (definite and probable) in the sample by putative PD status. Additionally, 41 (31.8%) PPD participants versus 21 (17.4%) NPD participants reported a prior history of treatment by Wave 3 (χ2 = 6.97, df = 1, p = .008). Finally, at Wave 1, 11% of the participants qualified for an Axis II diagnosis of some sort. This percentage rose to 16% by Wave 3. The raw rates of diagnosed PDs in the LSPD sample as of Wave 1 were as follows: paranoid = 1.2%, schizoid = 1.2%, schizotypal = 1.6%, antisocial = 0.8%, borderline = 1.6%, histrionic = 3.5%, narcissistic = 3.1%, obsessive-compulsive = 1.6%, passive-aggressive = 0.8%, avoidant = 1.2%, dependent = 0.8%, and not otherwise specified = 4.3%.
Table 2. Lifetime DSM-III-R Axis ISCID-NP diagnoses (definite and probable) for a sample of250 participants.
| Number of Subjects (%) |
|||||
|---|---|---|---|---|---|
| Disorder | NPD (n = 121) |
PPD (n = 129) |
χ 2 | p | ES (r) |
| Major depression | 16 (13.2) | 47 (36.4) | 17.84 | <0.001 | 0.27 |
| Bipolar/bipolar NOS | 1 (0.8) | 6 (4.7) | 3.36 | 0.07 | 0.12 |
| Dysthymia (current only) | 3 (2.5) | 13 (10.1) | 6.02 | 0.014 | 0.16 |
| Other affective disorder | 10 (8.3) | 32 (24.8) | 12.22 | <0.001 | 0.22 |
| Alcohol abuse | 2 (1.7) | 7 (5.4) | 2.56 | 0.11 | 0.10 |
| Alcohol dependence | 2 (1.7) | 13 (10.1) | 7.86 | 0.005 | 0.18 |
| Drug abuse | 3 (2.5) | 3 (2.3) | 0.006 | 0.94 | 0.00 |
| Drug dependence | 0 (0.0) | 4 (3.1) | 3.81 | 0.05 | 0.12 |
| Social phobia | 6 (5.0) | 22 (17.1) | 9.18 | 0.002 | 0.19 |
| Simple phobia | 8 (6.6) | 15 (11.6) | 1.88 | 0.17 | 0.09 |
| Panic | 3 (2.5) | 1 (0.8) | 1.15 | 0.28 | 0.07 |
| Obsessive–compul sive | 4 (3.3) | 8 (6.2) | 1.14 | 0.28 | 0.07 |
| Anorexia | 4 (3.3) | 4 (3.1) | 0.01 | 0.93 | 0.01 |
| Bulimia | 2 (1.7) | 11 (8.5) | 5.99 | 0.014 | 0.15 |
| Eating disorder NOS | 0 (0.0) | 1 (0.8) | 0.94 | 0.33 | 0.06 |
| Any Axis I diagnosis | 32 (26.4) | 81 (62.8) | 33.3 | <0.001 | 0.36 |
Note. SCID-NP, Structured Clinical Interview for DSM-III-R—Non-patient version; NPD, non-personality disorder controls; PPD, possible personality disorder; NOS, not otherwise specified. The values are the number of cases and percentages per diagnostic category observed in the two participant groups. Cases consist of both definite and probable lifetime Axis I diagnoses combined for the entire study period; some participants have more than one Axis I diagnosis. Significance is based on the Pearson χ2 test (two tailed. df = 1). ES r = effect size r calculated from χ2 using the following formula .
Individual Growth Curve Analyses
As a first step, we fit an unconditional growth curve model to both the standard and transformed IPDE BPD scores. These initial models are termed unconditional because the growth in the dependent variable is specified only as a function of time and error, with no between-person explanatory variables included. The intercept and slope were allowed to vary randomly. The parameters of the untransformed model, presented here as Model 1 in Table 3, have previously been presented elsewhere (Lenzenweger & Castro, 2005; Lenzenweger et al., 2004). The transformed (i.e., square root) version of the model has not previously been presented, and is listed as Model 2 in Table 3 for comparison to the conditional models that were subsequently fitted to these data. Aside from the resultant values of the fixed and random effects coefficients, the models remain highly similar. The fixed effect coefficient for the intercept in both models is significantly different from zero (p < .001) with a large effect size (ES r = .48 and .57 respectively; where ; Rosenthal & Rosnow, 1991). The fixed effect coefficient for the slope in both the untransformed and transformed models is significant (p < .001 and < .01 respectively), with medium (ES r = .24) and small (ES r = .17) effect sizes, respectively. The untransformed model shows that the average number of BPD features present in the sample was about one at the start of the study, with an average annual decline of .14 criteria. In addition, each model demonstrates significant variability in intercept ( i.e., initial value) and slope (; i.e., rate of change) of the Level 1 models remaining to be explained at Level 2. Therefore, the between person variables will be included at Level 2 as predictors of this variability in initial value and overall rate of decline in BPD features over the course of the study. A comparison of the deviance statistics between the two models demonstrates that the use of the transformed variables provides a much better fit to the data.
Table 3. Conditional and unconditional individual growth models predicting borderline personality disorder symptoms.
| Elevation (Intercept) of Individual Trajectory |
Rate of Change (Slope) of Individual Trajectory |
Variance Components |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fixed Effect Coeff. |
p | ES r | Fixed Effect Coeff. |
p | ES r | p | p | p | σ 01 | p | Deviance (-2LL) |
||||
| Model 1 | |||||||||||||||
| BPD | 0.970 | 0.001 | 0.48 | −0.143 | 0.001 | 0.24 | 1.024 | 0.001 | 2.505 | <0.001 | 0.131 | <0.001 | −0.572 | 0.001 | 2561.679 |
| Model 2 | |||||||||||||||
| BPD Transform | 0.544 | 0.001 | 0.57 | −0.047 | 0.007 | 0.17 | 0.240 | 0.001 | 0.438 | <0.001 | 0.014 | 0.003 | −0.066 | 0.001 | 1471.801 |
| Model 3 | |||||||||||||||
| Gender (Male) | 0.115 | 0.277 | 0.07 | −0.028 | 0.452 | 0.05 | 0.240 | 0.001 | 0.292 | 0.001 | 0.007 | 0.025 | −0.037 | 0.009 | 1393.828 |
| Group (PPD) | 0.354 | <0.001 | 0.24 | −0.089 | 0.010 | 0.16 | |||||||||
| Age of Entry | 0.154 | 0.056 | 0.12 | −0.081 | 0.005 | 0.18 | |||||||||
| DOM | 0.078 | 0.058 | 0.12 | −0.019 | 0.202 | 0.08 | |||||||||
| LOV | −0.048 | 0.318 | 0.06 | 0.008 | 0.356 | 0.03 | |||||||||
| CONSC | −0.098 | 0.032 | 0.14 | −0.004 | 0.806 | 0.02 | |||||||||
| NEUR | 0.150 | 0.001 | 0.23 | −0.029 | 0.047 | 0.13 | |||||||||
| Model 4 | |||||||||||||||
| Gender (Male) | 0.145 | 0.125 | 0.10 | −0.042 | 0.234 | 0.08 | 0.238 | 0.001 | 0.239 | 0.001 | 0.004 | 0.046 | −0.027 | 0.045 | 1355.903 |
| Group (PPD) | 0.360 | <0.001 | 0.25 | −0.081 | 0.016 | 0.16 | |||||||||
| Age of Entry | 0.173 | 0.033 | 0.14 | −0.085 | 0.006 | 0.18 | |||||||||
| DOM | 0.062 | 0.132 | 0.10 | −0.012 | 0.424 | 0.05 | |||||||||
| LOV | −0.062 | 0.151 | 0.09 | 0.010 | 0.481 | 0.05 | |||||||||
| CONSC | −0.066 | 0.088 | 0.11 | −0.007 | 0.614 | 0.03 | |||||||||
| NEUR | 0.160 | <0.001 | 0.27 | −0.033 | 0.023 | 0.15 | |||||||||
| DOMxLOV | −0.066 | 0.064 | 0.12 | 0.036 | 0.022 | 0.15 | |||||||||
| DOMxCONSC | −0.097 | 0.010 | 0.17 | 0.015 | 0.274 | 0.01 | |||||||||
| DOMxNEUR | 0.033 | 0.275 | 0.07 | 0.002 | 0.878 | 0.07 | |||||||||
| LOVxCONSC | −0.042 | 0.201 | 0.08 | 0.010 | 0.397 | 0.06 | |||||||||
| LOVxNEUR | −0.085 | 0.002 | 0.20 | 0.017 | 0.033 | 0.14 | |||||||||
| CONSCxNEUR | −0.072 | 0.021 | 0.15 | 0.010 | 0.306 | 0.07 | |||||||||
Note: Model 1 is the unconditional model using the untransformed dependant variable. Model 2 is also unconditional, but uses the square root transformed dependant variable. Model 3 is the conditional model without interactions. Model 4 is the conditional model with interaction terms included. All components of the Level-1 and Level-2 models were estimated simultaneously. Gender is coded male = 1 and female = 0; group status is coded possible personality disorder (PPD) = 1 and no personality disorder (NPD) = 0. Tabled values represent the final estimates of the fixed effects with robust standard errors. The fixed effects and variance component parameters were tested to determine if they differ from zero. ES r, effect size r, with benchmarks for dichotomous/dimensional predictors of .10/.10 = small effect, .24/.30 = medium effect, .37/.50 = large effect (Rosenthal & Rosnow, 1991). For Models 1 and 2 deviance statistics are based on six estimated parameters. Model 3 deviance is based on 20 estimated parameters. Model 4 deviance is based on 32 estimated parameters. Model estimation was done with full maximum likelihood with the HLM-6 program. Variance components and the deviance statistic reported in the rightmost columns are for the entire model. Significant values (p < .05) bolded.
We then fit two conditional models. In the first model, Model 3 in Table 3, the control variables and four dimensions (i.e., consensus big four; Widiger, 1998; Widiger, Livesley, & Clark, 2009) of the IASR-B5 were included as predictors. The second model, Model 4 in Table 3, expands on these analyses by testing the interaction between the four personality dimensions. These dimensions are the IPC axes of Dominance (DOM) and Love (LOV), and the FFM dimensions of Conscientiousness (CONSC) and Neuroticism (NEUR).1 The control variables were biological sex, sample selection group (i.e., PPD vs. NPD), and age at entry in to the study. The time between assessments for each participant was calculated in years, using each participant’s date of birth and exact assessment date, and then centered on age at entry into the study for each study participant. Centering the assessment intervals on age at entry and including age at entry as a predictor at Level 2 accounts for each participant’s unique chronological age when he/she began the study and causes the individual Level 1 intercepts to represent the value of the Wave I assessments as the participants’ “initial status.” Taking age at entry to the study into account is theoretically important because it helps to account for differences in the developmental level of the study participants. By including selection group, we account for the methodological approach of the LSPD’s selection process.
The first conditional model included the control variables and IASR-B5 dimensions of DOM, LOV, NEUR, and CONSC as predictors of interindividual variation in initial BPD features and interindividual change in these features over the course of the study. Overall model fit improved significantly by including these predictors (; p < .001). The resulting fixed effects and random components from this model are detailed in Table 4. First, we report the predictors of initial status (i.e., intercept). For the control variables, group status is a significant predictor of initial elevation (p < .001; ES r = .24) with those in the PPD group possessing a higher number of BPD features at the outset of the study. Additionally, age at entry to the study, although not significant at p = .05 (p = .056; ES r = .07), suggested that those who are older at the outset of the study had more features of the disorder. In terms of the assessed personality variables, consistent with past research, NEUR is a significant positive predictor of BPD features (p < .001; ES r = .23) and CONSC is a significant negative predictor (p = .032; ES r = .14). DOM, although also not significant at p = .05 (p = .058; ES r = .12), tended to be associated with greater BPD feature counts.
When it came to predicting the interindividual differences in change over time, a slightly different picture emerged. The coefficients for Group and NEUR were again significantly different from zero (p’s = .010 and .047 respectively; ES r’s = .16 and .13 respectively), and predicted a steeper decline in features over time. CONSC was no longer a significant predictor (p = .806) when it came to change in BPD over time, whereas age of entry to the study now achieved significance (p =.005; ES r = .18) with those who are older showing a more rapid decline in features over time. The variance components for both the intercept and slope of the Level 1 model continued to evidence significant variability that remained to be explained.
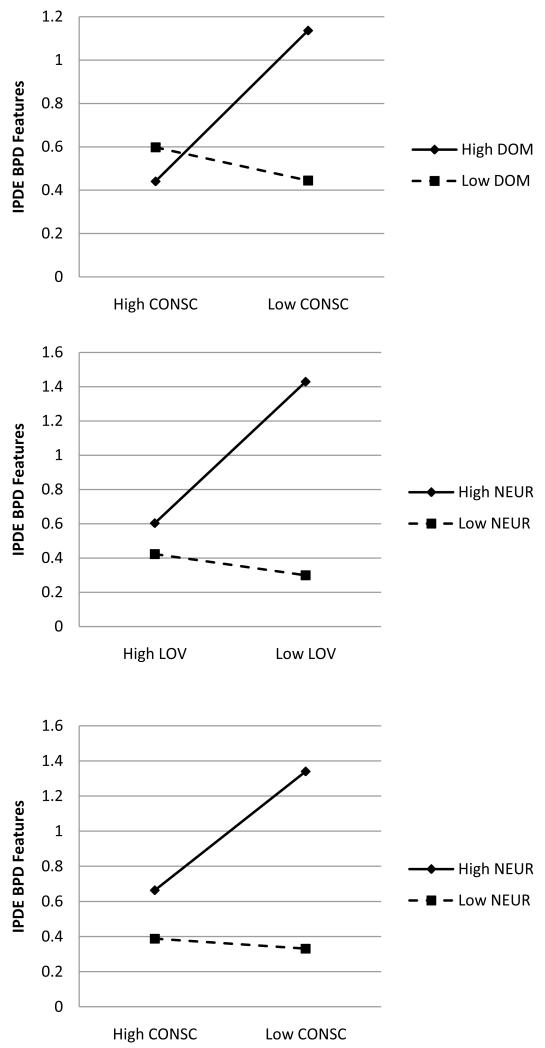
Based on the theory that the IPC dimensions would not be simple predictors of BPD features, we estimated a second conditional model that included interaction terms for the four included IASR-B5 dimensions. Overall model fit was significantly improved by including the interaction terms (; p < .001). Interaction effects were plotted to visually interpret the results and are presented in Figures 2 and 3. In predicting the variability in initial status of BPD symptoms, Group (p < .001; ES r = .25) and NEUR (p < .001; ES r = .27) remained as significant predictors of increased BPD features. In contrast, CONSC no longer was a significant predictor by itself and age of entry emerged as a significant predictor (p = .033; ES r = .14). Three interaction terms were significant. The DOM × CONSC (p < .010, ES r = .17) interaction revealed that high DOM and low CONSC only led to increased BPD features when in the presence of each other, otherwise neither had a significant effect. The LOV × NEUR interaction term was significant (p = .002, ES r = .20) such that the positive association between NEUR and BPD features is much stronger in the presence of low LOV. Finally, CONSC × NEUR significantly predicted (p = .015, ES r = .15) BPD features with low CONSC and high NEUR each augmenting the effects of the other. Significant variability remains to be explained in the intercepts (; p = .001) despite the inclusion of these predictors.
Figure 2.
Plots of the fitted Level 2 interaction effects for the final model intercept. DOM = Dominance score; LOV = Love score, NEUR = Neuroticism score; CONSC = Conscientiousness score. High = 1SD above the mean score, Low = 1SD below mean score.
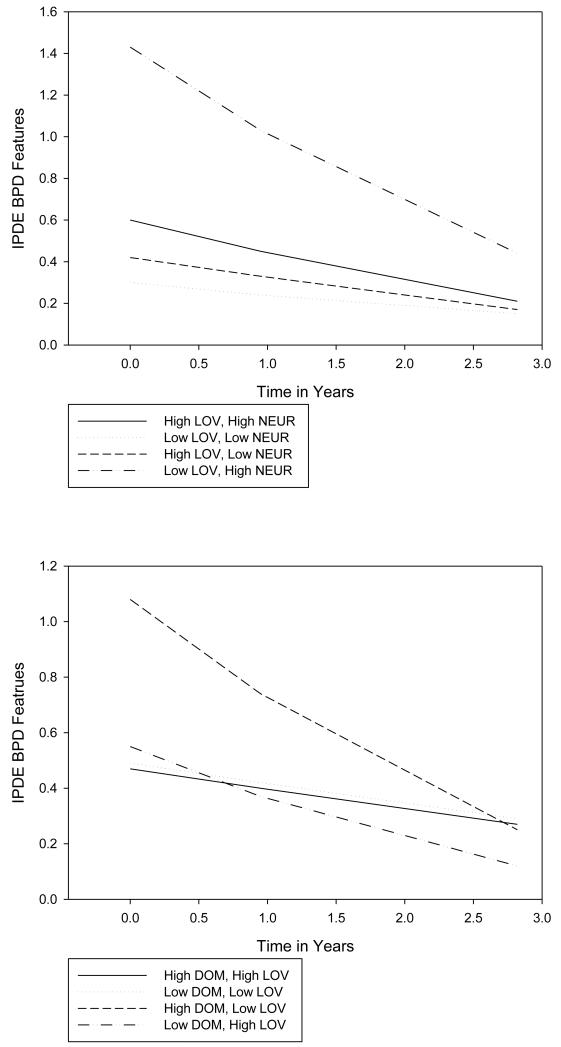
Figure 3.
Plots of the interaction effects of the fitted borderline personality disorder (BPD) feature growth curves. DOM = Dominance score; LOV = Love score, NEUR = Neuroticism score; High = 1SD above the mean score, Low = 1SD below mean score.
In predicting the slope, the same set of variables was significantly associated with change as in the previous model. The interaction terms that achieved significance in predicting change were not identical to those that predicted initial value. In predicting the slope DOM × CONSC and CONSC × NEUR were no longer significant predictors. The LOV × NEUR significantly predicted change (p = .033, ES r = .14), with those who were high in NEUR and low in LOV beginning the study with the highest number of BPD criteria, and then showing the fastest decline. Additionally, DOM × LOV was a significant predictor (p = .022, ES r = .15) of rate of change across the study. The results indicated that those who were higher in DOM and lower in LOV started at the highest value, and showed a steeper decline in BPD features across the study. Of note, high LOV and low DOM was associated with lower starting values, but a similarly steep slope. In contrast, when the signs of DOM and LOV were the same, the change was characterized by more modest initial values and shallow rates of change. All three-way interaction terms were non-significant for intercept or slope. Significant variability remains to be explained in the slopes (; p = .046).
Discussion
The accumulating data from a number of large longitudinal studies of PD suggests that these disorders are more plastic and characterized by change than had previously been asserted (Johnson et al., 2000; Lenzenweger, 1999; Lenzenweger et al., 2004; Shea et al., 2002; Zanarini et al., 2003). These new findings have important implications for conceptualization and classification of these disorders. In turn, these findings also have implications for assessment and treatment of personality pathology. The emerging challenge for the field of personality assessment is how to capture and predict the dynamic aspects of PD. The results of the current study pertain to the prediction of lack of stability over a large time scale (e.g., four years). We used individual growth curve modeling to predict variability in the initial value and rate of change in BPD symptoms using the IASR-B5 in the LSPD sample. Our focus was on the four dimensions of DOM, LOV, CONSC, and NEUR based on their theoretical importance and past empirical results (e.g., Saulsman & Page, 2004; Wiggins & Pincus, 1994).
The results of the first model, which does not include the interaction terms, are consistent with prior research on the IPC, FFM, and BPD. Higher levels of NEUR and lower levels of CONSC were associated with higher levels of BPD features at the start of the LSPD. Neither DOM nor LOV show significant relationships to BPD features at the outset, although this was perhaps to be expected given previous variable results with the IPC (e.g., Ryan & Shean, 2007; Wiggins & Pincus, 1989). Additionally, participant group (i.e., PPD vs. NPD) was a significant predictor of initial number of BPD features, capturing a major study design feature. In terms of predicting the variability in change, the results differ with those who are older showing a more rapid rate of decline in BPD features, likely capturing a developmental feature of the maturational process. Interestingly, CONSC, although a significant predictor of initial value, had no bearing on change in BPD features. This remains true through all of the tested models, suggesting that a low level of conscientiousness may not play much of a role in the maintenance process of BPD. Those in the PPD group show a more rapid rate of decline. Higher initial values of NEUR were also predictive of more rapid rates of decline. While at first glance a somewhat puzzling result, it is important to remember that the predictor is a baseline level of NEUR, and not NEUR over time. Therefore it is capturing the strong downward mean trend in BPD features of the study sample, as those who were higher in initial NEUR on average declined more throughout the study. These results are interesting in that they demonstrate the ability of a lexically based personality measure to capture the variability in change in clinician diagnosed symptoms across a 4-year time span. However, based on the dyadic-interactional view of the FFM (Wiggins & Trapnell, 1996), even more interesting are the analyses that capture the interplay between these personality variables.
The second conditional model demonstrated the effect we anticipated, namely that these personality dimensions modify the expression of each other to produce distinct conditional results. In predicting the initial values of BPD criteria, there were three significant interactions. Starting with the interaction between CONSC and NEUR, this suggests that while NEUR has a main effect, low CONSC is only problematic when there are high levels of NEUR. In that regard, low constraint is most problematic when one has a tendency to be emotionally reactive and distress-prone—generating a common clinical portrait of negative affectivity and impulsivity seen in BPD (Scott, Levy, & Pincus, 2009). Both of the interpersonal dimensions emerged in interactions with separate variables. DOM interacted with CONSC such that low CONSC was only problematic in the presence of high DOM. In the context of BPD features, a lack of control and planfulness is most problematic when one is also highly assertive and domineering. LOV interacted with NEUR such that high levels of LOV mitigated the usually detrimental effects of high NEUR associated with BPD, suggesting that those who seek out connections with others may receive support to better manage their affective reactivity. Alternatively, when individuals are interpersonally cold and high in neuroticism, they are at significantly greater risk for BPD symptoms.
Two interactions involving LOV were predictive of rate of change in BPD features. Although these two variables did not interact in the prediction of initial level of BPD symptoms, DOM and LOV significantly interacted in predicting the rate of change. The effect was such that those who were rated themselves as being arrogant-calculating (i.e., high DOM, low LOV) started with the highest values and showed more rapid rates of decline, whereas those who characterized themselves as unassuming-ingenuous (i.e., low DOM, high LOV) started the study with more modest BPD symptomatology with similarly steep rates of decline. In contrast, those who characterized themselves as either gregarious-extraverted (i.e., high DOM, high LOV) and aloof (i.e., low DOM, low LOV) started with modest levels of BPD symptomatology and showed no appreciable decline in BPD symptoms. These results might appear confusing at first, but what is occurring is the effect of the dimension that runs between arrogant-calculating and unassuming-ingenuous on the IPC. For those who are familiar with IPC terminology, this is the BC-JK axis. It is this axis that Agreeableness from the conventional conceptualization of the FFM most closely maps onto (McCrae & Costa, 1989, Pincus, 2002). Thinking about it in terms of this dimension, these results indicate that for those whose interpersonal style lies somewhere along this dimension there are stark differences in BPD trajectories over time. Those who are arrogant-calculating show the natural decline in BPD symptoms most drastically. This is understandable as they began with the highest number BPD symptoms, and the known trend is a decline in features over time, thus they evidence the greatest mean change. In contrast, those who are unassuming-ingenuous in their interpersonal approach start with lower values of BPD symptoms, but show a similar rate of decline, not because they are demonstrating the known decline in symptoms over time, but because their cooperative interpersonal style is protective. They are neither domineering nor hostile, and are more likely able to effectively work with and enlist the help and care of others. For those who are not characterized by either of these interpersonal styles, there is negligible change over time.
Finally, LOV interacted with NEUR such that those individuals who were low in LOV and high in NEUR began the study with the most BPD symptoms, and also showed the steepest rates of decline on average. Those individuals who did not describe themselves as high NEUR and low LOV did not show such steep declines. It is important to note that significant variance remains to be explained in the intercept and slope of these models, indicating that personality traits do not account for all of the variability in initial values and rates of change in BPD symptoms.
While the dimensions of the FFM model are hypothesized to be orthogonal in the population (Costa & McCrae, 1992), within an individual they can interact to produce qualitatively distinct expressions of personality. This point is emphasized, for example, in the Depue and Lenzenweger (2005) model, which views PDs as emergent phenomena reflective of rich interactions among underlying neurobehavioral systems. This is not a common approach in FFM research, which most typically focuses on profiles, even when the analytical approach is correlational (e.g., Miller, Gauhgan, Pryor, Kamen, & Campbell, 2009). Based on the current results, we believe that examining the interactions between the five-factors of the FFM within the same model would be an advantageous avenue for future investigation building on the vast literature that has related the FFM and PDs (e.g., Samuel & Widiger, 2008; Saulsman & Page, 2004). From a diagnostic standpoint, these interactions suggest that perhaps PDs cannot be fully captured by mere profiles of normal personality traits, but that the emergent phenomenon of personality pathology can be found in the complex interaction of these dimensions that are conditional on each other. Stated otherwise, individuals with BPD may be characterized by high neuroticism, low agreeableness, and low conscientiousness, but every person who is high in neuroticism, low in agreeableness, and low in conscientiousness will not have BPD (some will be schizotypal, for example, and others will show no pathology). Not every individual with the same basic personality profile will evidence the same psychiatric disorder. Perhaps it is only for those individuals within which these dimensions interact in specific ways that begin to evidence the types of personality pathology captured by a BPD diagnosis. This study further attests to the importance of investigating personality and psychopathology longitudinally and interactionally. By considering the influence and interaction of each of these dimensions with each other on the trajectory of psychopathology across time, we are better able to understand the conditions that support the perpetuation and decline of PD.
This is also the first study of which we are aware that has used the IPC dimensions of Agency and Communion as predictors of longitudinal change in PD criteria counts. As noted in the introduction, BPD has been a difficult diagnosis for the IPC to statically capture (Wiggins & Pincus, 1989). It is not that the disorder is not interpersonal in nature—exactly the opposite (APA, 2000). Instead, it is that BPD is not tethered to one location in interpersonal space, being characterized by labile behavioral oscillations (Russell, Moskowitz, Zuroff, Sookman, & Paris, 2007) which would likely give rise to the type of heterogeneity in results reviewed in the introduction of this study. Moreover, BPD as a disorder is more than its characteristic interpersonal expressions of the pathology. It is also characterized by strong negative emotions and disconstraint (Saulsman & Page, 2004). Relatedly, recent results from a finite mixture modeling study found 3 BPD types; a) non-paranoid/non-aggressive; b) paranoid/non-aggressive; c) antisocial/aggressive, non-paranoid which undoubtedly differ in their interpersonal styles (Lenzenweger, Clarkin, Yeomans, Kernberg, & Levy, 2008). Consistent with the dyadic-interactional perspective of the FFM, results reported here suggest that these additional features of the disorder interact with one’s interpersonal style in the expression and maintenance of the disorder (Wiggins & Trapnell, 1996).
Although the specific results for BPD are exciting indeed, we present them here in the spirit of exploration and hypothesis generation, not as the final word on the disorder. These trajectories are still at a very coarse level of analysis, representing years of individual interactions, relationships, and the push and pull of the individual and the environment. What is occurring as an individual navigates their interpersonal field that results in their specific trajectory across time? What accounts for the remaining variability in change over time? Are there significant relationship variables to account for (e.g., volatile or stable significant others)? Are their life events that also interact with an individual’s personality (e.g., trauma, suicide attempts, marriage; financial hardship)? The answers to these last two questions are undoubtedly yes and yes (see, e.g., Paris, 2001). In the context of lives, an individual both acts and is acted upon by the environment in complex ways which are better captured, but still only approximated, by using the individual trajectory as the unit of analysis.
From a clinician’s point of view, one potential limitation of this study is that it did not assess change due to treatment response. Therefore, these results should not be taken as indicative of the type of person who will respond well to treatment. The LSPD was designed to capture the natural change in criteria over time. Instead, what these results point to clinically is the prognosis associated with individual’s interpersonal style. Or, perhaps these results point to the type of interpersonal stance that a BPD patient might be encouraged to adopt thereby engendering the naturalistic change pattern of a decline in symptoms. Moreover, these results point towards a new direction in assessment research. As assessment science moves forward, it must build upon the wealth of knowledge that has been accumulated around predicting psychopathology at a single time-point, and move towards predicting the dynamic aspects of disorders (e.g., Odgers et al., 2009). In this context, a personality assessment is not the taking of a still photograph or portrait of an individual, but rather the production of a movie trailer. It is a brief summary that foreshadows what is to come throughout the feature length version. Fortunately, unlike the movie trailer that previews a completed work, an individual’s script can be revised and rewritten as it plays along. These results also show that even lexically based self-report assessments of personality are capable of predicting the types of dynamic instability that we now know is characteristic of personality disorders. Therefore, we are hopeful that the field is well equipped to begin focusing on the patterns of change, fluctuation, plasticity, variability, and flexibility that is so characteristic of emerging conceptions of personality and its pathology.
Acknowledgments
This research was supported in part by grant MH-45448 from the National Institute of Mental Health, Washington, DC (Dr. Lenzenweger).
We thank Armand W. Loranger, PhD for providing training and consultation on the use of the International Personality Disorder Examination (IPDE) and Jerry S. Wiggins, PhD for providing consultation on the initial use of the Revised Interpersonal Adjectives Scale - Big 5 (IASR-B5). We are grateful to Lauren Korfine, PhD for project coordination in the early phase of the study.
Footnotes
Openness was not included in any of the presented models because the FFM and PD literature has consistently failed to find significant relationship between Openness and BPD (Saulsman & Page, 2004). Furthermore, our own analyses with this data set have been consistent with this finding.
Contributor Information
Aidan G. C. Wright, The Pennsylvania State University
Aaron L. Pincus, The Pennsylvania State University
Mark F. Lenzenweger, State University of New York at Binghamton
References
- Alden LE, Wiggins JS, Pincus AL. Construction of circumplex scales for the Inventory of Interpersonal Problems. Journal of Personality Assessment. 1990;55:521–536. doi: 10.1080/00223891.1990.9674088. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. Text Revision. [Google Scholar]
- Ansell EB, Pincus AL. Interpersonal perceptions of the five-factor model of personality: An examination using the structural summary method for circumplex data. Multivariate Behavioral Research. 2004;39:167–201. doi: 10.1207/s15327906mbr3902_3. [DOI] [PubMed] [Google Scholar]
- Baird BM, Le K, Lucas RE. On the nature of intraindividual personality variability: Reliability, validity, and associations with well-being. Journal of Personality and Social Psychology. 2006;90:512–527. doi: 10.1037/0022-3514.90.3.512. [DOI] [PubMed] [Google Scholar]
- Bakan D. The duality of human existence: An essay on psychology and religion. Rand McNally; Oxford, England: 1966. [Google Scholar]
- Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. American Journal of Psychiatry. 2001;158:295–302. doi: 10.1176/appi.ajp.158.2.295. [DOI] [PubMed] [Google Scholar]
- Clark LA. Assessment and diagnosis of personality disorder: Perennial issues and an emerging reconceptualization. Annual Review of Psychology. 2007;58:227–257. doi: 10.1146/annurev.psych.57.102904.190200. [DOI] [PubMed] [Google Scholar]
- Cohen P, Crawford TN, Johnson JG, Kasen S. The children in the community study of developmental course of personality disorder. Journal of Personality Disorders.Special Issue: Longitudinal Studies. 2005;19(5):466–486. doi: 10.1521/pedi.2005.19.5.466. doi:10.1521/pedi.2005.19.5.466. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr., McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Psychological Assessment Resources; Odessa, FL: 1992. [Google Scholar]
- Depue RA, Collins PF. Neurobiology of the structure of personality: Dopamine, facilitation of incentive motivation, and extraversion. Behavioral and Brain Sciences. 1999;22:491–569. doi: 10.1017/s0140525x99002046. [DOI] [PubMed] [Google Scholar]
- Depue RA, Lenzenweger MF. A neurobehavioral dimensional model. In: Livesley WJ, editor. Handbook of personality disorders: Theory, research, and treatment. Guilford; New York, NY: 2001. pp. 136–176. [Google Scholar]
- Depue RA, Lenzenweger MF. A neurobehavioral dimensional model of personality disturbance. In: Clarkin JF, Lenzenweger MF, editors. Major theories of personality disorder. 2nd ed. Guilford; New York, NY: 2005. pp. 391–453. [Google Scholar]
- Depue RA, Lenzenweger MF. Toward a developmental psychopathology of personality disturbance: A neurobehavioral dimensional model. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology, Vol. 2: Developmental neuroscience. 2nd ed. John Wiley & Sons, Inc.; Hoboken, NJ: 2006. pp. 762–796. [Google Scholar]
- Depue RA, Morrone-Strupinsky JV. A neurobehavioral model of affiliative bonding: Implications for conceptualizing a human trait of affiliation. Behavioral and Brain Sciences. 2005;28:313–395. doi: 10.1017/S0140525X05000063. [DOI] [PubMed] [Google Scholar]
- Gurtman MB. Interpersonal problems and the psychotherapy context: The construct validity of the inventory of interpersonal problems. Psychological Assessment. 1996;8:241–255. [Google Scholar]
- Haslam N. The dimensional view of personality disorders: A review of the taxometric evidence. Clinical Psychology Review. 2003;23:75–93. doi: 10.1016/s0272-7358(02)00208-8. [DOI] [PubMed] [Google Scholar]
- Hertzog C, Nesselroade JR. Assessing psychological change in adulthood: An overview of methodological issues. Psychology and Aging. 2003;18:639–657. doi: 10.1037/0882-7974.18.4.639. [DOI] [PubMed] [Google Scholar]
- Hilsenroth MJ, Menaker J, Peters EJ, Pincus AL. Assessment of borderline pathology using the Inventory of Interpersonal Problems Circumplex Scales (IIP-C): A comparison of clinical samples. Clinical Psychology and Psychotherapy. 2007;14:365–376. [Google Scholar]
- Horowitz LM. Interpersonal foundations of psychopathology. American Psychological Association; Washington, DC: 2004. [Google Scholar]
- Horowitz LM, Wilson KR, Turan B, Zolotsev P, Constantino MJ, Henderson L. How interpersonal motives clarify the meaning of interpersonal behavior: A revised circumplex model. Personality and Social Psychology Review. 2006;10:67–86. doi: 10.1207/s15327957pspr1001_4. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F, Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: A community-based longitudinal investigation. Acta Psychiatrica Scandinavica. 2000;102:265–275. doi: 10.1034/j.1600-0447.2000.102004265.x. [DOI] [PubMed] [Google Scholar]
- Leary T. Interpersonal diagnosis of personality. Ronald Press; New York: 1957. [Google Scholar]
- Leichsering F, Kunst H, Hoyer J. Borderline personality organization in violent offenders: Correlations of identity diffusion and primitive defense mechanisms with antisocial features, neuroticism, and interpersonal problems. Bulletin of the Menninger Clinic. 2003;67:314–327. doi: 10.1521/bumc.67.4.314.26983. [DOI] [PubMed] [Google Scholar]
- Leihener F, Wagner A, Haaf B, Schmidt C, Lieb K, Stieglitz R, Bohus M. Subtype differentiation of patients with borderline personality disorder using a circumplex model of interpersonal behavior. Journal of Nervous and Mental Disease. 2003;191:248–254. doi: 10.1097/01.NMD.0000061150.38924.2A. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF. Epidemiology of personality disorders. Psychiatric Clinics of North America. 2008;31:395–403. doi: 10.1016/j.psc.2008.03.003. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF. Stability and change of personality disorder features: The Longitudinal Study of Personality Disorders. Archives of General Psychiatry. 1999;59:1009–1015. doi: 10.1001/archpsyc.56.11.1009. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF. The longitudinal study of personality disorders: history, design, and initial findings [special essay] Journal of Personality Disorders. 2006;20:645–670. doi: 10.1521/pedi.2006.20.6.645. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Castro DD. Predicting change in borderline personality: Using neurobehavioral systems indicators within an individual growth curve framework. Development and Psychopathology. 2005;17:1207–1237. doi: 10.1017/s0954579405050571. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Clarkin JF, Yeomans FE, Kernberg OF, Levy KN. Refining the borderline personality disorder phenotype through finite mixture modeling: Implications for classification. Journal of Personality Disorders. 2008;22:313–331. doi: 10.1521/pedi.2008.22.4.313. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Johnson MD, Willet JB. Individual growth curve analysis illuminates stability and change in personality disorder features: The Longitudinal Study of Personality Disorders. Archives of General Psychiatry. 2004;61:1015–1024. doi: 10.1001/archpsyc.61.10.1015. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the national comorbidity survey replication. Biological Psychiatry. 2007;62:553–564. doi: 10.1016/j.biopsych.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzenweger MF, Loranger AW, Korfine L, Neff C. Detecting personality disorders in a non-clinical sample: Application of a 2-stage procedure for case identification. Archives of General Psychiatry. 1997;54:345–351. doi: 10.1001/archpsyc.1997.01830160073010. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Willet JB. Predicting individual change in personality disorder features by simultaneous individual change in personality dimensions linked to neurobehavioral systems: The longitudinal study of personality disorders. Journal of Abnormal Psychology. 2007;116:684–700. doi: 10.1037/0021-843X.116.4.684. [DOI] [PubMed] [Google Scholar]
- Livesley WJ. Commentary on reconceptualizing personality disorder categories using trait dimensions. Journal of Personality. 2001;69(2):277–286. doi: 10.1111/1467-6494.00145. [DOI] [PubMed] [Google Scholar]
- Locke KD. Circumplex scales of interpersonal values: Reliability, validity, and applicability to interpersonal problems and personality disorders. Journal of Personality Assessment. 2000;75:249–267. doi: 10.1207/S15327752JPA7502_6. [DOI] [PubMed] [Google Scholar]
- Locke KD, Sadler P. Self-efficacy, values, and complementarity in dyadic interactions: Integrating interpersonal and social-cognitive theory. Personality and Social Psychology Bulletin. 2007;33:94–109. doi: 10.1177/0146167206293375. [DOI] [PubMed] [Google Scholar]
- Loranger A. The Personality Disorder Examination (PDE) manual. DV Communications; Yonkers, NY: 1988. [Google Scholar]
- Loranger AW. International Personality Disorder Examination: DSM-IV and ICD-10 Interviews. Psychological Assessment Resources Inc.; Odessa, Fla: 1999. [Google Scholar]
- McCrae RR, Costa PT. The structure of interpersonal traits: Wiggins’s circumplex and the five-factor model. Journal of Personality and Social Psychology. 1989;56:586–595. doi: 10.1037//0022-3514.56.4.586. [DOI] [PubMed] [Google Scholar]
- Moskowitz DS. Cross situational generality and the interpersonal circumplex. Journal of Personality and Social Psychology. 1994;66:921–933. doi: 10.1037//0022-3514.66.4.753. [DOI] [PubMed] [Google Scholar]
- Meyer GJ, Finn SE, Eyde LD, Kay GG, Moreland KL, Dies RR, Eisman EJ, Kubiszyn TW, Read GM. Psychological testing and psychological assessment: A review of evidence and issues. American Psychologist. 2001;56:128–165. [PubMed] [Google Scholar]
- Miller JD, Gaughan ET, Pryor LR, Kamen C, Campbell WK. Is research using the narcissistic personality inventory relevant for understanding narcissistic personality disorder. Journal of Research in Personality. 2009;43:482–488. [Google Scholar]
- Morey LC. An empirical comparison of interpersonal and DSM-III approaches to classification of personality disorders. Psychiatry: Journal for the Study of Interpersonal Processes. 1985;48:358–364. doi: 10.1080/00332747.1985.11024296. [DOI] [PubMed] [Google Scholar]
- Morey LC, Gunderson J, Quigley BD, Shea MT, Skodol AE, McGlashan TH, Stout RL, Zanarini MC. The representation of borderline, avoidant, obsessive-compulsive, and schizotypal personality disorders by the five-factor model. Journal of Personality Disorders. 2002;16:215–234. doi: 10.1521/pedi.16.3.215.22541. [DOI] [PubMed] [Google Scholar]
- Moskowitz DS. Unfolding interpersonal behavior. Journal of Personality.Special Issue: Advances in Personality and Daily Experience. 2005;73:1607–1632. doi: 10.1111/j.1467-6494.2005.00360.x. [DOI] [PubMed] [Google Scholar]
- Odgers CL, Mulvey EP, Skeem JL, Gardner W, Lidz CW, Schubert C. Capturing the ebb and flow of psychiatric symptoms with dynamical systems models. American Journal of Psychiatry. 2009;166:575–582. doi: 10.1176/appi.ajp.2008.08091398. [DOI] [PubMed] [Google Scholar]
- Paris J. Psychosocial adversity. In: Livesley WJ, editor. Handbook of personality disorders: Theory, research, and treatment. Guilford; New York: 2001. pp. 231–241. [Google Scholar]
- Pincus AL. Constellations of dependency within the five-factor model of personality. In: Costa PT Jr., Widiger TA, editors. Personality disorders and the five-factor model of personality. 2nd ed. American Psychological Association; Washington, DC, US: 2002. pp. 203–214. [Google Scholar]
- Pincus AL. A contemporary integrative interpersonal theory of personality disorders. In: Clarkin J, Lenzenweger M, editors. Major theories of personality disorder. 2nd Ed. Guilford; New York: 2005. pp. 282–331. [Google Scholar]
- Pincus AL, Gurtman MB. Interpersonal theory and the interpersonal circumplex: Evolving perspectives on normal and abnormal personality. In: Strack S, editor. Differentiating normal and abnormal personality. 2nd ed. Springer Publishing Co.; New York, NY, US: 2006. pp. 83–111. [Google Scholar]
- Pincus AL, Lukowitsky MR, Wright AGC. The interpersonal nexus of personality and psychopathology. In: Millon T, Kruger RF, Simonsen E, editors. Contemporary directions in psychopathology: Scientific Foundations for the DSM-V and ICD-11. Guilford Press; New York: 2010. pp. 523–552. [Google Scholar]
- Pincus AL, Lukowitsky MR, Wright AGC, Eichler WC. The interpersonal nexus of persons, situations, and psychopathology. Journal of Research in Personality. 2009;43:264–265. [Google Scholar]
- Pincus AL, Wiggins JS. Interpersonal Problems and conceptions of personality disorders. Journal of Personality Disorders. 1990;4:342–352. [Google Scholar]
- Pincus AL, Wright AGC. The interpersonal diagnosis of psychopathology. In: Horowitz LM, Strack SN, editors. Handbook of interpersonal psychology: Theory, research, assessment, and therapeutic interventions. Wiley; New York, NY: In press. [Google Scholar]
- Scott LN, Levy KN, Pincus AL. Adult attachment, personality traits, and borderline personality disorder features in young adults. Journal of Personality Disorders. 2009;23:258–280. doi: 10.1521/pedi.2009.23.3.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram N, Gerstorf D. Time-structured and net intraindividual variability: Tools for examining the aging of dynamic characteristics and processes. Psychology and Aging. 2009;24:778–791. doi: 10.1037/a0017915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon R. HLM-6: Hierarchical Linear and Nonlinear Modeling. Scientific Software International; Lincolnwood, IL: 2004. [Google Scholar]
- Russell JJ, Moskowitz DS, Zuroff DC, Sookman D, Paris J. Stability and variability of affective experience and interpersonal behavior in borderline personality disorder. Journal of Abnormal Psychology. 2007;116:578–588. doi: 10.1037/0021-843X.116.3.578. [DOI] [PubMed] [Google Scholar]
- Ryan K, Shean G. Patterns of interpersonal behaviors and borderline personality characteristics. Personality and Individual Differences. 2007;42:193–200. [Google Scholar]
- Samuel DB, Widiger TA. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: A facet level analysis. Clinical Psychology Review. 2008;28:1326–1342. doi: 10.1016/j.cpr.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saulsman LM, Page AC. The five-factor model and personality disorder empirical literature: A meta-analytic review. Clinical Psychology Review. 2004;23(8):1055–1085. doi: 10.1016/j.cpr.2002.09.001. [DOI] [PubMed] [Google Scholar]
- Shea MT, Stout R, Gunderson J, Morey LC, Grilo CM, McGlashan T, et al. Short term diagnostic stability of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. American Journal of Psychiatry. 2002;159:2036–2041. doi: 10.1176/appi.ajp.159.12.2036. [DOI] [PubMed] [Google Scholar]
- Sim JP, Romney DM. The relationship between a circumplex model of interpersonal behaviors and personality disorders. Journal of Personality Disorders. 1990;4:329–341. [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press Inc.; New York, NY: 2003. [Google Scholar]
- Skodol AE. Longitudinal course and outcome of personality disorders. Psychiatric Clinics of North America. 2008;31:495–503. doi: 10.1016/j.psc.2008.03.010. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Shea MT, McGlashan TH, Morey LC, Sanislow CA, et al. The Collaborative Longitudinal Personality Disorder Study (CLPS): Overview and Implications. Journal of Personality Disorders. 2005;19:487–504. doi: 10.1521/pedi.2005.19.5.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldz S. The interpersonal circumplex as a structural model in clinical research: Examples from group psychotherapy, interpersonal problems, and personality disorders. In: Plutchick R, Conte H, editors. Circumplex models of personality and emotions. American Psychological Association; Washington, DC: 1997. pp. 411–430. [Google Scholar]
- Soldz S, Budman S, Demby A, Merry J. Representation of personality disorders in circumplex and five-factor space: Explorations with a clinical sample. Psychological Assessment. 1993;5:41–52. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First M. Users guide for the structured clinical interview for DSM-III-R. American Psychiatric Press; Washington, DC: 1990. [Google Scholar]
- Sullivan HS. The interpersonal theory of psychiatry. Newton; New York: 1953. [Google Scholar]
- Tracey TJG, Rohlfing JE. Variations in the understanding of interpersonal behavior: Adherence to the interpersonal circle as a moderator of the rigidity-psychological well being relation. Journal of Personality. 2010;78:711–745. doi: 10.1111/j.1467-6494.2010.00631.x. [DOI] [PubMed] [Google Scholar]
- Trapnell PD, Wiggins JS. Extension of the Interpersonal Adjective Scales to include the Big Five dimensions of personality. Journal of Personality and Social Psychology. 1990;59:781–790. [Google Scholar]
- Widiger TA. Four out of five ain’t bad. Archives of General Psychiatry. 1998;55:865–866. doi: 10.1001/archpsyc.55.10.865. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Hagemoser S. Personality disorders and the interpersonal circumplex. In: Plutchick R, Conte H, editors. Circumplex models of personality and emotions. American Psychological Association; Washington, DC: 1997. pp. 299–326. [Google Scholar]
- Widiger TA, Livesley WJ, Clark LA. An integrative dimensional classification of personality disorder. Psychological Assessment. 2009;21:243–255. doi: 10.1037/a0016606. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Simonsen E. Alternative dimensional models of personality disorder: Finding a common ground. Journal of Personality Disorders. 2005;19:110–130. doi: 10.1521/pedi.19.2.110.62628. [DOI] [PubMed] [Google Scholar]
- Wiggins JS. A psychological taxonomy of trait-descriptive terms: The interpersonal domain. Journal of Personality and Social Psychology. 1979;37:395–412. [Google Scholar]
- Wiggins JS. Circumplex models of interpersonal behavior in clinical psychology. In: Kendall PC, Butcher JN, editors. Handbook of research methods in clinical psychology. Wiley; New York: 1982. pp. 183–221. [Google Scholar]
- Wiggins JS. Agency and communion as conceptual coordinates for the understanding and measurement of interpersonal behavior. In: Cicchetti D, Grove WM, editors. Thinking clearly about psychology: Essays in honor of Paul Meehl, Vol. 2: Personality and Psychopathology. University of Minnesota Press; Minneapolis, MN: 1991. pp. 89–113. [Google Scholar]
- Wiggins JS. The Interpersonal Adjective Scales: Professional manual. Psychological Assessment Resources; Odessa, FL: 1995. [Google Scholar]
- Wiggins JS. An informal history of the interpersonal circumplex tradition. Journal of Personality Assessment. 1996;66:217–233. doi: 10.1207/s15327752jpa6602_2. [DOI] [PubMed] [Google Scholar]
- Wiggins JS. Paradigms of personality assessment. Guilford; New York: 2003. [DOI] [PubMed] [Google Scholar]
- Wiggins JS, Pincus AL. Conceptions of personality disorders and dimensions of personality. Psychological Assessment. 1989;1:305–316. [Google Scholar]
- Wiggins JS, Pincus AL. Personality structure and the structure of personality disorders. In: Costa PT Jr., Widiger TA, editors. Personality Disorders and the Five-Factor Model of Personality. American Psychological Association; Washington, D.C.: 1994. pp. 73–93. [Google Scholar]
- Wiggins JS, Trapnell PD. A dyadic-interactional perspective on the five-factor model. In: Wiggins JS, editor. The five-factor model of personality: Theoretical perspectives. Guilford Press; New York, NY, US: 1996. pp. 88–162. [Google Scholar]
- Wiggins JS, Trapnell P, Phillips N. Psychometric and geometric characteristics of the revised interpersonal adjective scales (IAS—R) Multivariate Behavioral Research. 1988;23:517–530. doi: 10.1207/s15327906mbr2304_8. [DOI] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Conroy DE, Hilsenroth MJ. Integrating methods to optimize circumplex description and comparison of groups. Journal of Personality Assessment. 2009;91:311–322. doi: 10.1080/00223890902935696. [DOI] [PubMed] [Google Scholar]
- Yen S, Pagano ME, Shea MT, et al. Recent life events preceding suicide attempts in a personality disorder sample: Findings from the Collaborative Longitudinal Personality Disorders Study. Journal of Consulting and Clinical Psychology. 2005;73:99–105. doi: 10.1037/0022-006X.73.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR,, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. American Journal of Psychiatry. 2003;160:274–283. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Prediction of the 10-year course of borderline personality disorder. American Journal of Psychiatry. 2006;163:827–32. doi: 10.1176/ajp.2006.163.5.827. [DOI] [PubMed] [Google Scholar]