Abstract
Background
The use of cannabis for medical purposes is proliferating in the U.S., and PTSD is an explicitly approved condition for accessing medical cannabis in 5 states. Prior research suggests that people with PTSD often use cannabis to help cope with their condition, and that doing so results in more frequent and problematic cannabis use patterns. Specific coping motivations, such as sleep improvement, among medical cannabis users, have not been examined.
Methods
The present study evaluated specific coping use motivations, frequency of cannabis and alcohol use, and mental health among a convenience sample of patients (N=170) at a medical cannabis dispensary in California.
Results
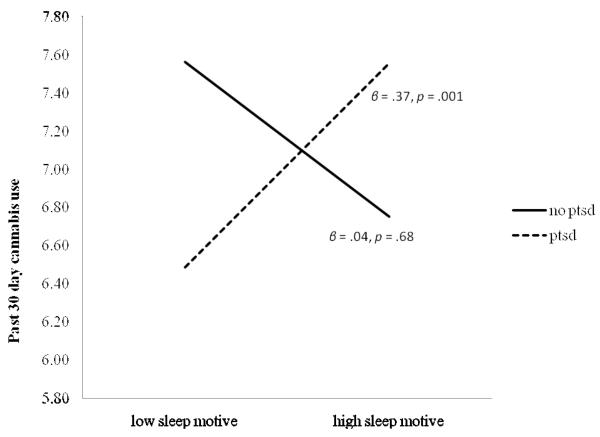
Those with high PTSD scores were more likely to use cannabis to improve sleep, and for coping reasons more generally, compared with those with low PTSD scores. Cannabis use frequency was greater among those with high PTSD scores who used for sleep promoting purposes compared with those with low PTSD scores or those who did not use for sleep promoting purposes.
Conclusions
Consistent with prior research, this study found increased rates of coping-oriented use of cannabis and greater frequency of cannabis use among medical users with high PTSD scores compared with low PTSD scores. In addition, sleep improvement appears to be a primary motivator for coping-oriented use. Additional research is needed to examine the health consequences of this pattern of cannabis use and whether alternative sleep promoting interventions (e.g. CBT-I) could reduce the reliance on cannabis for adequate sleep among those with PTSD.
Keywords: cannabis, coping, medical marijuana, PTSD, sleep
1. INTRODUCTION
Cannabis is the most widely used illicit substance in the United States (SAMHSA, 2012) and the legalization of cannabis for medicinal purposes has become a growing trend. The approved conditions for which cannabis may be doctor-recommended varies at the state level, but most states allow medical use of cannabis for certain medical disorders/problems (e.g., cancer, severe and chronic pain, HIV/AIDS). The use of medical cannabis for psychological disorders, however, is not as common. Currently, only 5 of 20 states with medical cannabis laws explicitly allow the medical use of cannabis as a treatment for those with posttraumatic stress disorder (PTSD).
Though there has been a general dearth of empirical research speaking to the use and effects of cannabis among those with PTSD, existing evidence suggests that individuals with PTSD, particularly those with heightened hyperarousal symptoms, use cannabis primarily for coping reasons (e.g., Boden et al., 2013; Bonn-Miller et al., 2007a; Passie et al., 2012), and that such coping-oriented use may be associated with heavier and more problematic cannabis use patterns (e.g., dependence), as documented in the general population (Bonn-Miller and Zvolensky, 2009). Following, there has been increasing interest in understanding, among those with PTSD, the specific motives for which cannabis is used. In a study among 20 adult females with PTSD, Bonn-Miller and colleagues (2010) found poor sleep quality to interact with PTSD symptom severity in the prediction of coping-oriented cannabis use. Here, individuals with elevated PTSD symptoms and sleep problems were particularly likely to use cannabis to cope.
Though Bonn-Miller and colleagues (2010) documented the importance of sleep problems in terms of understanding the association between PTSD and coping-oriented cannabis use, little research has been conducted to examine whether specific symptoms of PTSD are being “treated” with cannabis use, and, in particular, whether individuals with PTSD use cannabis specifically to improve sleep, or instead to cope with negative affect more broadly. Here, recent work has demonstrated that specific psychoactive components of cannabis may initially facilitate sleep onset (Russo et al., 2007; Schierenbeck et al., 2008), though long-term and problematic use has been associated with sleep disturbances, including altered sleep architecture (Bolla et al., 2008; Vandrey et al., 2011). Additionally, there has yet to be an investigation of how specific coping motivations are associated with use frequency within this context.
The present study sought to examine (1) the specific cannabis motives that distinguish a medicinal cannabis-using individual with PTSD from an individual without PTSD, and (2) whether the interaction of PTSD and PTSD-specific use motives are associated with more severe use frequency. We hypothesized that medical cannabis users with PTSD would be more likely to report cannabis use specifically to improve sleep, compared to those without PTSD. Further, due to the development of tolerance to the sleep-inducing effects of cannabis (Schierenbeck et al., 2008), as well as prior documented associations between coping-oriented use and heavy cannabis use patterns (Bonn-Miller and Zvolensky, 2009), we hypothesized that those with PTSD who also used for sleep motives would evidence greater cannabis use frequency. As research has demonstrated that depression and alcohol use are both associated with PTSD (McFarlane, 1998; Shalev et al., 1998) and cannabis use (Bovasso, 2001; Griffin et al., 2002), depressive symptoms and alcohol use were included as covariates.
2. METHOD
2.1 Participants
Study participants (N=217) were adult (18 and over) patients using cannabis obtained from a licensed medical cannabis dispensary in San Francisco, California. Of the participants enrolled in the study, 170 completed the requisite questionnaires and were included in data analyses. The mean age of the sample was 41 years (SD=15) and 22% were female. Participants were excluded based on inability to provide written informed consent to participate, and being under 18 years of age. The majority of participants self-identified as Caucasian (67.1%), followed by Black/Non-Hispanic (7.8%), Hispanic (7.8%), Black/Hispanic (3.0%), Asian (3.0%), and “Other” (11.4%). The most common self-reported conditions for which participants sought medical cannabis included anxiety (62.7%), chronic pain (55.6%), stress (47.9%), insomnia (47.9%), and depression (41.4%; see Bonn-Miller et al., 2013 for more complete description).
2.2 Procedure
Patients presenting to the medical cannabis dispensary were provided with the opportunity to participate in the study by research staff. After obtaining written informed consent to participate, interested individuals completed a battery of questionnaires. Research staff debriefed participants upon completion, and participants were entered into 1 of 4 drawings to receive a $100 prize. Data describing self-reported cannabis use characteristics of this sample have been reported previously (Bonn-Miller et al., 2013). Study procedures were approved by the Stanford University IRB and conducted in accordance with the ethical principles of the Declaration of Helsinki.
2.3 Measures
2.3.1 Posttraumatic Stress
The PTSD Checklist-Civilian Version (PCL-C; Weathers et al., 1993) is a 17-item questionnaire in which respondents indicate presence and severity of symptoms of PTSD, derived from the DSM-IV symptoms for PTSD (APA, 2000). A total score was calculated. Consistent with recommendations among community samples (NCPTSD, 2013), a total score of 30 was used as a cut-off to generate two groups: those without PTSD (PCL score < 30) and those with probable PTSD (PCL score > 30). The PCL-C has excellent psychometric properties (Weathers et al., 1993). Cronbach’s α = .95 in the current sample.
2.3.2 Cannabis Use Motives
The Comprehensive Marijuana Motives Questionnaire (CMMQ; Lee et al., 2009) was used to index motives for cannabis use. Participants rate how often they use cannabis for each of 36 reasons on a 5-point Likert-type scale (1 = “Almost Never/Never” to 5 = “Almost Always/Always”). These 36 items comprise 12 different domains (3 reasons/domain) of motives for use including: Enjoyment, Conformity, Coping (e.g., “To forget your problems”), Experimentation, Boredom, Alcohol, Celebration, Altered Perception, Social Anxiety, Low Risk, Sleep (e.g., “To help you sleep”), and Availability. Cronbach’s α = .74 for CMMQ subscales in the current sample.
2.3.3 Cannabis Use Frequency
A single item from the Marijuana Smoking History Questionnaire (MSHQ; Bonn-Miller and Zvolensky, 2009) was used to determine past 30-day cannabis use, regardless of use motive (e.g., medicinal). Participants were asked to rate the frequency of their cannabis use in the past 30 days on a scale of 0 “no use” to 8 “more than once a day.” The MSHQ has performed well in previous research, with convergent validity for the employed frequency item (Bonn-Miller and Zvolensky, 2009; Bonn-Miller et al., 2007b). In the present sample, scores ranged from 2-8 (M = 7.09, SD = 1.37).
2.3.4 Alcohol Use
The Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993) is a 10-item self-report measure of hazardous and harmful alcohol consumption. A total score is calculated to produce a global measure of problematic alcohol use. Cronbach’s α = .84 in the current sample.
2.3.5 Depressive Symptoms
The Inventory of Depression and Anxiety Scale (IDAS; Watson et al., 2007) is a 64-item questionnaire measuring depression and anxiety. The General Depression subscale was employed as a measure of depressive symptoms and used as a covariate. Cronbach’s α = .84 in the current sample.
2.4 Data Analysis
First, a series of t-tests were conducted to examine group (no PTSD versus probable PTSD) differences in terms of cannabis use motives. T-tests were adjusted (p = .01) for multiple comparisons. Next, we examined the interaction of motive for use (sleep and coping) and group on past 30-day cannabis use. Two separate hierarchical multiple regressions (HMRs) were conducted (one for sleep, one for coping motives) in which past 30-day cannabis use served as the outcome variable. Sleep and coping motives were selected, as these were the only two motives that were found to vary as a function of PTSD symptom levels. All continuous variables were standardized prior to entry. In Step 1, main effects for motive (sleep or coping) and PTSD group were simultaneously entered. In step 2, the interaction between motive (sleep or coping) and PTSD group was entered. In step 3, alcohol use (AUDIT total score) and depressive symptoms (IDAS General Depression sub-score) were entered as covariates. Variables were entered in this fashion to test whether the obtained results remained after adjusting for relevant covariates, while ensuring that interaction effects were not significant merely due to suppression effects of covariates (Simmons et al., 2011).
3. RESULTS
Results of t-tests indicated that individuals with probable PTSD reported greater motivation to use cannabis for sleep and coping reasons compared to those without PTSD. No associations were found between PTSD and any other motives (see Table 1). In the hierarchical regressions (see Table 1), a significant main effect for sleep motives, but not PTSD group, was observed in predicting past 30-day cannabis use. Furthermore, as predicted, the interaction between sleep motives and group was associated with past 30-day cannabis use, accounting for 3% of unique variance. After adjusting for covariates in Step 3, the interaction remained significant with the entire model accounting for 25.2% of variance in past 30-day cannabis use. In terms of coping motives, there was a main effect for coping, but not PTSD group. In addition, the interaction of PTSD group and coping was non-significant.
Table 1.
Mean scores for each motive for cannabis use based on group and regression analyses
| Group | Regression Analyses: DV = Past 30-day Cannabis Use | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| Motive for Use |
PTSD N = 75 |
No PTSD N = 95 |
Step 1 | Step 2 | Step 3 | ||||||||||
|
| |||||||||||||||
| Motive | Group | Motive | Group | Int | Motive | Group | Int | Dep | Alc | ||||||
|
| |||||||||||||||
| M | SD | M | SD | t | β | β | β | β | β | β | β | β | β | β | |
|
| |||||||||||||||
| Sleep | 10.84 | 3.97 | 9.32 | 4.11 | −2.42* | .18* | −.01 | .04 | −.02 | .21* | .03 | −.01 | .21* | −.05 | .08 |
| Enjoy | 10.35 | 2.97 | 10.42 | 3.59 | 0.15 | ||||||||||
| Conform | 3.57 | 1.47 | 3.59 | 1.72 | 0.10 | ||||||||||
| Coping | 6.63 | 2.96 | 5.45 | 2.62 | −2.72† | .19* | −.02 | .25* | −.02 | −.08 | .25* | .02 | −.07 | −.10 | .08 |
| Experiment | 5.28 | 3.43 | 4.97 | 2.67 | −0.65 | ||||||||||
| Boredom | 5.15 | 2.61 | 5.34 | 2.97 | 0.44 | ||||||||||
| Alcohol | 3.83 | 1.54 | 3.56 | 1.19 | −1.02 | ||||||||||
| Celebration | 6.56 | 3.48 | 7.30 | 3.69 | 1.33 | ||||||||||
| Perception | 8.80 | 3.92 | 8.46 | 3.95 | −0.55 | ||||||||||
| Social Anxiety | 7.77 | 3.78 | 6.71 | 3.46 | −1.98 | ||||||||||
| Low Risk | 9.40 | 3.61 | 9.16 | 3.88 | −0.42 | ||||||||||
| Available | 5.74 | 2.87 | 5.22 | 2.43 | −1.28 | ||||||||||
| Total Score | 79.56 | 23.17 | 76.64 | 21.55 | −0.73 | ||||||||||
Note: n = 170.
p < .05;
p < .01;
p < .001.
Motive = Motive for use; Group = Probable PTSD/No PTSD; Int = Interaction term (motive * group); Dep = Depressive symptoms; Alc = Alcohol use. In relation to the regression analyses: Step 1 represents the entry of the main effects; Step 2 is comprised of main effects and the interaction term; Step 3 represents the inclusion of the main effects, interaction, and covariates.
Consistent with recommendations for examining interactions (Aiken and West, 1991), post-hoc probing of the significant interaction indicated that sleep motives was positively associated with past 30-day cannabis use among individuals with probable PTSD, but not among individuals without PTSD (see Figure 1).
Figure 1.
Level of past 30-day cannabis use as a function of the interaction between PTSD group (no PTSD versus Probable PTSD) and sleep motives. Frequency of past 30-day cannabis use was ranked on a scale of 0 “no use” to 8 “more than once a day.
Analyses were also run using a continuous index of PTSD symptoms (total PCL score). Results remained consistent. A significant interaction of sleep motive and PTSD symptoms emerged both before, β = .70, p = .008, and after, β = .69, p = .009, accounting for covariates. In addition, analyses related to coping motives still yielded a non-significant interaction, β = −.07, p = .80.
4. DISCUSSION
The present study sought to extend prior work by determining motivation for cannabis use among individuals who report elevated PTSD symptoms and use medical cannabis. First, the present study replicated prior work (e.g., Bonn-Miller et al., 2007a; 2013) by documenting that individuals with probable PTSD used cannabis for negative affect reduction (i.e., coping motives). Consistent with hypotheses, the present study also provided the first empirical evidence for cannabis use for sleep reasons among those with probable PTSD, with these two motives (i.e., coping, sleep) being the only motives observed to differ between those with probable PTSD and those without.
Also consistent with expectation, PTSD group was found to interact with sleep motives in terms of cannabis use frequency. These findings extend prior work that documented an interactive relation between PTSD symptoms and sleep problems in terms of coping motives (Bonn-Miller et al., 2010) by showing that those with probable PTSD (and those with greater PTSD symptom severity) who used cannabis to improve sleep reported more frequent cannabis use. Indeed, no association was observed between sleep motives and use frequency among the non-PTSD group. Though coping-oriented use was elevated among those with probable PTSD, no interaction was observed for frequency of cannabis use, providing strong evidence for the uniqueness of the association between PTSD symptoms and sleep motives in terms of cannabis use frequency. Finally, all of the aforementioned associations were observed above and beyond co-occurring alcohol problems and depressive symptoms, and among a sample of medicinal cannabis users, a group heretofore unexamined in terms of PTSD and associated use motivation.
Though the present study provides strong empirical evidence for the unique role of sleep-motivated cannabis use among medicinal cannabis users with probable PTSD, it is not without limitation. First, the present study was cross-sectional in nature. Additionally, it was conducted within one cannabis dispensary in San Francisco, and the sample was primarily male. So as to improve our understanding of the observed associations and generalizability of findings, future work should employ prospective assessment among samples more representative of the medicinal cannabis using population. Another limitation of the present study was that no interview-based or objective measures were employed (all data were self-report). Though the employed measures were well validated and have been used extensively in prior literature, future work would benefit from including biochemical verification of cannabis use status as well as behavioral (e.g., cue exposure) and/or interview-based (e.g., Clinician Administered PTSD Scale; Blake et al., 1995) measures of PTSD status and symptomatology.
Limitations notwithstanding, the present study provides empirical evidence to suggest that individuals with high levels of PTSD symptoms use medicinal cannabis for coping and sleep motives, and that sleep-motivated use, specifically, is associated with more frequent cannabis use. Interventions shown to improve sleep quality (e.g., Cognitive Behavioral Therapy for Insomnia; Morin et al., 2006) may be useful in terms of providing an alternative to cannabis for individuals with PTSD who are reporting significant difficulties with sleep. It is unknown whether the high rate of cannabis use among this sub-population is associated with adverse health outcomes relative to those with PTSD who do not use cannabis.
Acknowledgments
Role of Funding Source. Funding for this study was provided by A VA Clinical Science Research and Development (CSR&D) Career Development Award-2 (Bonn-Miller), a donation from the San Francisco Patient and Resource Center (Bonn-Miller), Health Services Research and Development Service funds (Babson), and a grant from the National Institute on Drug Abuse (U01-DA031784; Vandrey). The funding sources had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors Dr. Bonn-Miller designed the study and wrote the protocol. Drs. Bonn-Miller and Vandrey managed the literature searches and summaries of previous related work. Dr. Babson undertook the statistical analysis, method, and results. Dr. Bonn-Miller wrote the first draft of the manuscript. Dr. Vandrey provided editing and revisions to drafts. All authors contributed to and have approved the final manuscript.
Conflict of Interest All authors declare that they have no conflicts of interest.
Contributor Information
Marcel O. Bonn-Miller, Center for Innovation to Implementation and National Center for PTSD, VA Palo Alto Health Care System 795 Willow Road, Menlo Park, California 94025-USA; Center of Excellence in Substance Abuse Treatment and Education, Philadelphia VAMC Department of Psychiatry, University of Pennsylvania
Kimberly A. Babson, Center for Innovation to Implementation, VA Palo Alto Health Care System Department of Psychiatry and Behavioral Sciences, Stanford School of Medicine 795 Willow Road, Menlo Park, California 94025-USA
Ryan Vandrey, Department of Psychiatry and Behavioral Sciences, Johns Hopkins University 5510 Nathan Shock Drive, Baltimore, Maryland 21224-USA.
REFERENCES
- Aiken L, West S. Multiple Regression: Testing and Interpreting Interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th Edition – Text Revision American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Blake D, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. J. Trauma Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Boden MT, Babson KA, Vujanovic AA, Short NA, Bonn-Miller MO. Posttraumatic stress disorder and cannabis use characteristics among military veterans with cannabis dependence. Am. J. Addict. 2013;22:277–284. doi: 10.1111/j.1521-0391.2012.12018.x. [DOI] [PubMed] [Google Scholar]
- Bolla K, Lesage S, Gamaldo C, Neubauer D, Funderbuck F, Lud Cadet J, David PM, Verdejo-Garcia A, Benbrook AR. Sleep disturbance in heavy marijuana users. Sleep. 2008;31:901–908. doi: 10.1093/sleep/31.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Babson KA, Vujanovic AA, Feldner MT. Sleep problems and PTSD symptoms interact to predict marijuana use coping motives: a preliminary investigation. J. Dual Diagnosis. 2010;6:111–122. [Google Scholar]
- Bonn-Miller MO, Boden MT, Bucossi MM, Babson KA. Self-reported cannabis use characteristics, patterns, and helpfulness among medical cannabis users. Am. J. Drug Alcohol Abuse. 2013 doi: 10.3109/00952990.2013.821477. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Feldner MT, Bernstein A, Zvolensky MJ. Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event-exposed marijuana users. J. Trauma Stress. 2007a;20:577–586. doi: 10.1002/jts.20243. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ. An evaluation of the nature of marijuana use and its motives among young adult active users. Am. J. Addict. 2009;18:409–416. doi: 10.3109/10550490903077705. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Marshall E. Incremental validity of anxiety sensitivity in relation to marijuana withdrawal symptoms. Addict. Behav. 2007b;32:1843–1851. doi: 10.1016/j.addbeh.2006.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovasso G. Cannabis abuse as a risk factor for depressive symptoms. Am. J. Psychiatry. 2001;158:2033–2037. doi: 10.1176/appi.ajp.158.12.2033. [DOI] [PubMed] [Google Scholar]
- Griffin K, Botvin G, Scheier L, Nichols T. Factors associated with regular marijuana use among high school students: a long-term follow-up study. Subst. Use Misuse. 2002;37:225–238. doi: 10.1081/ja-120001979. [DOI] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, Grossbard JR. Development and preliminary validation of a comprehensive marijuana motives questionnaire. J. Stud. Alcohol Drugs. 2009;70:279–287. doi: 10.15288/jsad.2009.70.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane A. Epidemiological evidence about the relationship between PTSD and alcohol abuse: the nature of the association. Addict. Behav. 1998;23:813–825. doi: 10.1016/s0306-4603(98)00098-7. [DOI] [PubMed] [Google Scholar]
- Morin C, Bootzin R, Buysse D, Edinger J, Espie C, Lichstein K. Psychological and behavioral treatment of insomnia: update of the recent evidence (1998-2004) Sleep. 2006;29:1398–1414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- National Center for PTSD [Retrieved on 9/15/2013];Using the PTSD Checklist (PCL) http://www.ptsd.va.gov/professional/pages/assessments/assessment-pdf/pcl-handout.pdf.
- Passie T, Emrich HM, Karst M, Brandt SD, Halpern JH. Mitigation of post-traumatic stress symptoms by cannabis resin: a review of the clinical and neurobiological evidence. Drug Test Anal. 2012;4:649–659. doi: 10.1002/dta.1377. [DOI] [PubMed] [Google Scholar]
- Russo EB, Guy GW, Robson PJ. Cannabis, pain, and sleep: lessons from therapeutic clinical trials of Sativex, a cannabis-based medicine. Chem. Biodivers. 2007;4:1729–1743. doi: 10.1002/cbdv.200790150. [DOI] [PubMed] [Google Scholar]
- Saunders J, Aasland O, Babor T, de la Fuente J, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schierenbeck T, Riemann D, Berger M, Homyak M. Effect of illicit recreational drugs upon sleep: cocaine, ecstasy and marijuana. Sleep Med. Rev. 2008;12:381–389. doi: 10.1016/j.smrv.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Shalev A, Freedman S, Peri T, Brandes D, Sahar T, Orr S, Pitman R. Prospective study of posttraumatic stress disorder and depression following trauma. Am. J. Psychiatry. 1998;155:630–637. doi: 10.1176/ajp.155.5.630. [DOI] [PubMed] [Google Scholar]
- Simmons J, Nelson L, Simonsohn U. False-positive psychology: undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychol. Sci. 2011;22:1359–1366. doi: 10.1177/0956797611417632. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2012. [Google Scholar]
- Vandrey R, Smith MT, McCann UD, Budney AJ, Curran EM. Sleep disturbance and the effects of extended release zolpidem during cannabis withdrawal. Drug Alcohol Depend. 2011;117:38–44. doi: 10.1016/j.drugalcdep.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, O’Hara M, Simms L, Kotov R, Chmielewski M, McDade-Montez E, Gamez W, Stuart S. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psychol. Assess. 2007;19:253–268. doi: 10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]