Abstract
Objective
To evaluate whether clinical characteristics alter the accuracy of clinical estimation of fetal weight (EFW) in term pregnancies in a teaching hospital.
Methods
Secondary analysis of a retrospective cohort study of patients presenting for labor at term. Clinical EFW was performed using Leopold maneuvers. A Spearman’s rank correlation coefficient (r) was used to evaluate the linear relationship between clinical EFW and actual birth weight (BW). Body mass index (BMI), gestational age, fetal station and admission diagnosis were evaluated with respect to their impact on clinical EFW. The primary outcome was an absolute error between clinical EFW and actual BW >500 grams.
Results
Of 3,797 patients, 941 (24.8%) had an absolute error in clinical EFW exceeding 500 grams. The overall correlation between clinical EFW and actual BW was weak (r=0.4). There was a significant trend of improved accuracy of clinical EFW with increasing gestational age; however, BMI, fetal station, and admission diagnosis did not have significant effects. 181 of 221 cases (81.9%) of fetal macrosomia (>4000 grams) were undetected by clinical EFW.
Conclusion
The correlation between clinical EFW and actual birth weight is overall weak, particularly in patients with macrosomic fetuses; however, BMI, admission diagnosis, and fetal station do not have a significant impact.
Keywords: body mass index, clinical estimation of fetal weight, Leopold maneuvers, macrosomia, obesity
Introduction
Clinical estimation of fetal weight (EFW) at term using Leopold maneuvers is a routine obstetric practice; however, the inherent subjective element of this measurement weakens it as a clinical tool. Factors such as maternal obesity, discomfort during labor, and progressive descent of the fetal head with advancing gestational age may further differentially impact the accuracy of clinical EFW. An accurate EFW is critical in determining mode of delivery, as cesarean delivery is recommended at pre-defined fetal weight thresholds in order to prevent shoulder dystocia and its associated morbidities.1 Inaccurate estimation of fetal weight may lead to an increased risk of shoulder dystocia in patients whose fetal weight is underestimated or, alternatively, to the increased surgical risk of a cesarean delivery in patients whose fetal weight may be overestimated.
Despite the high frequency with which Leopold maneuvers are performed to estimate fetal weight and the potential implications of these estimates, there is a relative paucity of literature evaluating clinical factors which may modify their accuracy. The majority of literature on this topic has focused on the effect of maternal obesity and has demonstrated conflicting results.2-5 Field et al. observed no difference in the accuracy of fetal weight prediction across all body mass index (BMI) categories; whereas, Fox et al. recently demonstrated that increased maternal BMI was associated with decreased accuracy of clinical EFW.2,3 With the growing obesity epidemic in the United States, this aspect of clinical estimation of fetal weight draws increasing concern.
The majority of high-risk pregnancies in the United States are delivered at academic tertiary care centers which are mainly staffed by resident physicians under the supervision of an attending physician. Arguably, this patient population is at highest risk for fetal growth disorders based on multiple maternal and fetal co-morbidities. A prior study has demonstrated that provider experience does not significantly impact the accuracy of clinical EFW; therefore, although labor admissions are performed mostly by residents at these centers, it is still reasonable to study this high risk population of patients in order to evaluate other potential modifiers of clinical EFW in this teaching setting.6 The objective of this study was 1) to determine whether clinical estimates of fetal weight at the time of labor admission correlate with actual birth weight and 2) to evaluate whether clinical characteristics, including maternal obesity, alter the accuracy of these clinical estimates in term pregnancies in a teaching hospital.
Methods
This was a secondary analysis of a retrospective cohort study of consecutive patients with vertex, singleton gestations who presented for labor at ≥ 37 weeks from 2004-2008. Only patients who reached the second stage of labor were included in the original cohort. Cases of both spontaneous labor as well as inductions of labor were included. Pregnancies with known fetal anomalies were excluded. Approval from the institutional review board at the Washington University School of Medicine was obtained.
Standard of care at our institution is for a clinical EFW to be performed using Leopold maneuvers at the time of admission for labor. Clinical estimation of fetal weight is provided as a point estimate rounded off to the nearest 100 grams. Leopold maneuvers are generally performed by the admitting physician, typically a junior level resident. Patients without prior ultrasound dating and those with a high clinical suspicion for macrosomia routinely have an ultrasound performed to assess fetal weight. For the purposes of this analysis, all patients with an ultrasound EFW at the time of admission were excluded. Maternal demographics as well as extensive pregnancy and neonatal outcome information were extracted from electronic medical records.
The primary outcome was defined as an absolute error between clinical EFW and actual birth weight >500 grams. This outcome was chosen as a clinically relevant outcome, as errors of this magnitude could have a potential impact on delivery mode planning. Secondary outcomes included overall absolute error, overall absolute percent error [(EFW-BW)/BW x 100%], absolute percent error >10%, absolute percent error >20%, and the percentage of macrosomic infants not detected on clinical exam. Macrosomia was defined as birth weight >4000 grams. Clinical characteristics including maternal BMI, gestational age at admission, fetal station of <0 versus ≥0 at the time of presentation, and admission diagnosis of spontaneous labor versus induction of labor were evaluated with respect to their impact on clinical estimation of fetal weight. Maternal BMI was obtained by self-report at the time of admission and was divided into categories of <25 kg/m2, 25-29.9 kg/m2, 30.0-34.9 kg/m2, and ≥35 kg/m2. Gestational age at admission was evaluated in intervals of <39 weeks, 39 to 396/7 weeks, 40 to 406/7 weeks, and ≥ 41 weeks. In order to evaluate resident provider experience over time, we divided the academic year in half (July-December and January-June) and compared outcomes between these groups. We hypothesized that clinical accuracy would improve throughout the academic year if resident provider experience had a significant impact on clinical estimation of fetal weight.
Baseline characteristics of the study cohort were reported using descriptive statistics. A Spearman’s rank correlation coefficient (rho) was used to evaluate the linear relationship between clinical estimates of fetal weight and actual birth weights. The primary and secondary study outcomes were then evaluated with respect to each clinical characteristic of interest. A one-way analysis of variance was used to compare continuous outcomes across BMI categories, gestational age categories, and time of year categories. The Cochran-Armitage test for trend was used to compare categorical outcomes across categories. To evaluate the effect of fetal station and admission diagnosis on clinical EFW, continuous outcomes were compared between groups using Student’s t-tests and dichotomous outcomes were compared using chi-square tests. Normality of distribution was evaluated using the Kolmogorov-Smirnov test. P-values <0.05 were considered statistically significant. All statistical analysis was performed using STATA 10, Special Edition (College Station, TX).
Results
Of 5,345 patients, EFW on admission was recorded for 4,261 (79.7%). After excluding patients with an ultrasound EFW (n=335) and those without complete height and weight data for the calculation of maternal BMI (n=129), 3,797 patients remained for analysis, comprising our final cohort. The mean gestational age at the time of admission for labor was 38.9 ± 1.2 weeks, and the mean birth weight was 3279 ± 439 grams. 5.8% of the cohort delivered a macrosomic infant weighing >4000 grams, and 3.1% delivered an infant weighing <2500 grams. Characteristics of the study cohort are shown in Table I.
Table I.
Characteristics of the Study Cohort
| N=3,797 | % | |
|---|---|---|
|
| ||
| Mean Maternal Age (years) * | 24.9 ± 5.8 | - |
|
| ||
| Primiparous | 1,414 | 37% |
|
| ||
| Multiparous | 2,383 | 63% |
|
| ||
| Race | ||
| Caucasian Race | 621 | 16.4% |
| African American Race | 2,826 | 74.4% |
| Hispanic Race | 218 | 5.7% |
| Asian Race | 74 | 2.0% |
| Other | 58 | 1.5% |
|
| ||
|
Mean Gestational Age at the
Time of Delivery (weeks) * |
38.9 ± 1.2 | - |
|
| ||
| Mean Birth Weight (grams) * | 3279 ± 439 | - |
|
| ||
| Birth Weight >4000 grams | 221 | 5.8% |
|
| ||
| Birth Weight <2500 grams | 116 | 3.1% |
|
| ||
| Mode of Delivery | ||
| Spontaneous Vaginal Delivery | 3,253 | 85.7% |
| Operative Vaginal Delivery | 487 | 12.8% |
| Cesarean Delivery | 57 | 1.5% |
|
| ||
| Mean Maternal BMI (kg/m 2 ) * | 31.7 ± 6.8 | - |
|
| ||
| Spontaneous Labor | 2,613 | 68.8% |
|
| ||
| Induction of Labor | 1,184 | 31.2% |
|
| ||
| Gestational Diabetes | 96 | 2.5% |
|
| ||
| Pre-Existing Diabetes | 116 | 3.1% |
|
| ||
| Chronic Hypertension | 454 | 12.0% |
|
| ||
| Pre-Eclampsia | 366 | 9.6% |
Data expressed as mean ± standard deviation
BMI=body mass index
The overall correlation between clinical EFW and actual birth weight was weak. (rho=0.4) 181 of 221 cases (81.9%) of macrosomia were undetected by clinical EFW. The mean absolute error between clinical EFW and actual BW was 347 ± 273 grams, with a total of 941 fetuses (24.8%) found to have an absolute error exceeding 500 grams. The clinical EFW was found to be an over-estimate of actual birth weight in 58.2% of patients and an under-estimate of actual birth weight in 41.2% of patients.
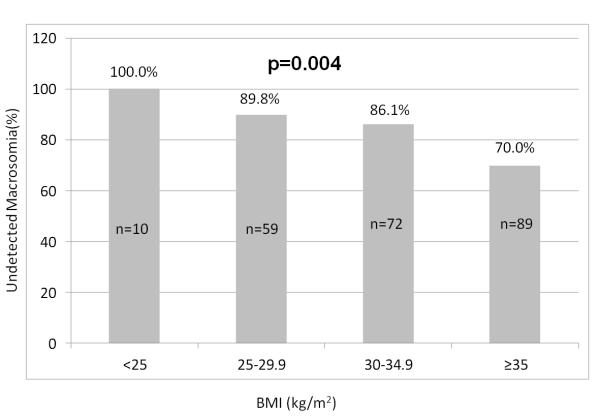
Maternal BMI did not have a significant influence on the accuracy of clinical EFW, with Leopold maneuvers being equally inaccurate across BMI strata. There was no statistically significant difference in absolute error >500 grams nor in any of the other secondary outcomes of accuracy across BMI categories. (Table II) Providers were more likely to under-estimate fetal weight in patients with a BMI <30 kg/m2 compared to patients with BMI ≥30 kg/m2 (p=0.006). In contrast, providers were more likely to over-estimate fetal weight in patients with a BMI ≥30 kg/m2 compared to patients with a BMI <30 kg/m2 (p=0.007). In a subgroup analysis evaluating only patients who delivered macrosomic infants (n=221), there was a significant inverse relationship between increasing BMI and the proportion of undetected cases of macrosomia (p=0.004). (Figure I)
Table 2.
Effect of Maternal BMI on the Accuracy of Clinical EFW
| BMI | <25 kg/m2 (n=517) |
25.0-29.9 kg/m2 (n=1,234) |
30.0-34.9 kg/m2 (n=1,066) |
≥35 kg/m2 (n=980) |
p-value |
|---|---|---|---|---|---|
|
Absolute Error
(grams) * |
331g ± 257 | 336g ± 268 | 352g ± 281 | 365g ± 277 | 0.90 |
|
Absolute Error
>500 grams |
24.9% | 22.9% | 25.1% | 26.6% | 0.25 |
|
Absolute Percent
Error * |
11.2 ± 9.3 | 10.7 ± 9.3 | 11.0 ± 9.8 | 11.5 ± 9.8 | 0.57 |
|
Absolute Percent
Error >10% |
44.1% | 44.4% | 43.3% | 47.4% | 0.27 |
|
Absolute Percent
Error >20% |
17.2% | 14.3% | 14.8% | 15.8% | 0.45 |
Data expressed as mean ± standard deviation
BMI=body mass index; EFW=estimated fetal weight
Figure 1.
Proportion of macrosomia cases undetected by clinically estimated fetal weight across maternal body mass index (BMI) categories.
Neither admission diagnosis nor fetal station had a significant impact on the accuracy of clinical EFW. Comparing 2,613 (68.8%) patients who were admitted with spontaneous labor to 1,184 (31.2%) patients who were admitted for an induction of labor, no statistically significant difference in the accuracy of clinical EFW was found. Similarly, when comparing 3,362 (88.5%) patients with a fetal station <0 at the time of admission to 419 (11.0%) patients with a fetal station ≥0 at the time of admission, no statistically significant difference in any of the outcomes of accuracy was found. (Table III)
Table III.
Effect of Admission Diagnosis and Fetal Station on the Accuracy of Clinical EFW
| Admission Diagnosis | |||
|---|---|---|---|
| Outcome | Spontaneous Labor (n=2,613) |
Induction of Labor (n=1,184) |
p-value |
|
Absolute Error
(grams) * |
344 ± 266 | 354 ± 287 | 0.64 |
|
Absolute Error >500
grams * |
24.1% | 26.3% | 0.15 |
|
Absolute Percent
Error |
11.0 ± 9.2 | 11.2 ± 10.3 | 0.98 |
|
Absolute Percent
Error >10% |
45.1% | 42.1% | 0.52 |
|
Absolute Percent
Error >20% |
15.5% | 14.7% | 0.52 |
| Fetal Station | |||
| Outcome |
Fetal Station <0
(n=3,362) |
Fetal Station ≥0
(n=419) |
p-value |
|
Absolute Error
(grams) * |
348 ± 273 | 342 ± 273 | 0.57 |
|
Absolute Error >500
grams |
24.8% | 24.3% | 0.84 |
|
Absolute Percent
Error * |
11.0 ± 10.7 | 11.2 ± 9.8 | 0.90 |
|
Absolute Percent
Error >10% |
44.6% | 46.1% | 0.57 |
|
Absolute Percent
Error >20% |
15.0% | 16.9% | 0.30 |
Data expressed as mean ± standard deviation
EFW=estimated fetal weight
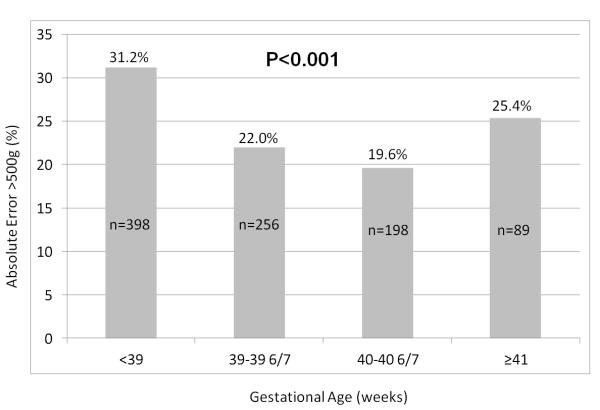
When comparing the accuracy of clinical EFW by gestational age, there was a significant J-shaped relationship between of the proportion of fetal weight estimates with an absolute error >500 grams and increasing gestational age, reaching a nadir at 40 weeks’ gestation and then rising again in following weeks (p<0.001). (Figure II) Similar trends were observed in absolute error, absolute percent error, absolute percent error >10%, and absolute percent error >20%. (Table IV) Although statistically significant, the overall difference in absolute error across gestational age categories was small (<100 grams) and, therefore, may not have strong clinical significance.
Figure II.
Proportion of clinical estimates of fetal weight with an absolute error >500rams across gestational age categories.
Table IV.
Effect of Gestational Age on the Accuracy of Clinical EFW
| Outcome | <39 wks (n=1,275) |
39-39 6/7 wks (n=1,161) |
40-40 6/7 wks (n=1,011) |
≥41 wks (n=350) |
p-value |
|---|---|---|---|---|---|
|
Absolute Error
(grams) * |
396 ± 285 | 326 ± 266 | 312 ± 252 | 342 ± 286 | <0.001 |
|
Absolute Error
>500 grams |
31.2% | 22.0% | 19.6% | 25.4% | <0.001 |
|
Absolute
Percent Error * |
13.7 ± 11.1 | 10.2 ± 8.9 | 9.2 ± 7.8 | 9.6 ± 8.0 | <0.001 |
|
Absolute
Percent Error >10% |
55.9% | 41.2% | 37.1% | 39.4% | <0.001 |
|
Absolute
Percent Error >20% |
23.8% | 13.5% | 8.3% | 9.7% | <0.001 |
Data expressed as mean ± standard deviation
EFW=estimated fetal weight; wks=weeks
Finally, when evaluating admission time of year as a surrogate marker of resident provider experience, there was also no statistically significant difference in any of the outcomes of accuracy. Resident providers were equally as likely to make a clinical estimation error of >500 grams during the first six months of the academic year compared to the latter six months. (p=0.42).
Discussion
Our study demonstrates that the accuracy of clinical EFW at term using Leopold maneuvers in a teaching hospital is overall poor; however, these estimates are not further adversely impacted by clinical factors such as maternal obesity, maternal discomfort in labor, or fetal station at the time of admission. While we did observe a significant trend of increasing accuracy of clinical EFW with advancing gestational age up to 40 weeks, the overall small difference in absolute error across gestational age categories likely would not be enough to impact mode of delivery planning, making this finding clinically insignificant.
Similar to our findings, Field et al. previously demonstrated that maternal obesity did not alter the accuracy of clinical EFW; however, that study included both term and preterm patients and used an atypical definition of obesity (>29 kg/m2).2 Alternatively, Fox et al. evaluated the impact of maternal BMI on the accuracy of clinical EFW in a retrospective cohort study of 400 term patients. That study demonstrated a significant decrease in the proportion of clinical estimations within 10% and 20% of actual birth weight with increasing maternal BMI. However, consistent with our results, that study failed to demonstrate a significant difference in absolute error or absolute percent error across BMI categories.3 In contrast to prior studies, we chose to evaluate the primary outcome of clinical EFW and actual birth weight discordance exceeding 500 grams. This outcome captures a level of discordance that could have significant impact on determining mode of delivery, while still allowing for the natural variability in estimation that is expected from a subjective measurement such as that obtained from a Leopold maneuver.
One striking finding from our study is that the majority of cases of macrosomia (81.9%) went undetected by clinical exam. In a prospective cohort study of 192 patients, Noumi et al. observed a low sensitivity of 50% and positive predictive value of 43% in the detection of fetal macrosomia >4000 grams by clinical exam.5 Levin et al. also demonstrated an increased error in clinical estimation of birth weight in the subgroups of birth weight <2500 grams and >4000 grams.6 Surprisingly, in our study, a significantly higher proportion of cases of macrosomia actually were identified in obese patients than in those patients with normal BMI. It is possible that the increased thickness of the abdominal wall in cases of obesity contributes to a higher clinical EFW and, therefore, a decreased chance of missing a case of macrosomia. Additionally, it is also possible that provider biases regarding maternal obesity as a risk factor for macrosomia may lead to higher clinical estimates in obese patients.7,8
Apart from maternal obesity, there is limited data regarding other clinical factors that may impact the accuracy of clinical EFW. Blann and Prien performed both clinical and sonographic estimation of fetal weight before and after amniotomy in 162 laboring patients. That study found that post-amniotomy clinical EFW had the strongest correlation with actual birth weight.9 Noumi et al. evaluated the clinical variables of maternal age, parity, Bishop score, gestational age, birth weight, and post-graduate year of the examiner and found that none of these variables significantly influenced the accuracy of clinical EFW.5 Although it may seem intuitive that increased maternal discomfort during an admission for spontaneous labor or advanced descent of the fetal head would decrease the accuracy of clinical EFW, the current data, including the findings from this study, argues against this notion and suggests that the accuracy of clinical EFW is independent from the influence of these clinical variables.
Strengths of our study include our large sample size from which detailed maternal demographic and labor admission data were extracted. This allowed to us to thoroughly evaluate multiple clinical variables which could potentially influence the accuracy of clinical EFW. Our large sample size also allowed us to stratify maternal obesity in two levels (BMI 30.0-34.9 and BMI ≥35) as well as evaluate the differential impact of maternal BMI on a subgroup of patients who delivered macrosomic fetuses. Another strength of our study includes our clinically relevant outcome of absolute error between clinical EFW and actual birth weight >500 grams. Additionally, the consistency of our findings across all of the various outcomes of accuracy provides support to the reliability of our findings. Finally, we excluded all patients with an ultrasound estimate of fetal weight, thereby eliminating any potential bias of the sonographic EFW on the clinical EFW.
Our study is not without limitations, including the fact that all patients must have progressed to the second stage of labor in order to be included in the original study cohort by design. While this is unlikely to have an effect on our primary analysis of accuracy across predefined clinical variables, it may introduce a selection bias into our subgroup analysis of macrosomia. Given that fetal macrosomia is associated with a higher rate of cesarean delivery for failure to progress, it is likely that our study population from the second stage of labor is actually under-representative of the true incidence of macrosomia in the population. Additionally, while the incidence of macrosomia in our cohort was large enough to evaluate its clinical detection rate, it was not large enough to allow us to evaluate the outcomes of shoulder dystocia or elective cesarean delivery, the true clinical consequences of under- or overestimation of fetal macrosomia. Finally, we were unable to capture individual provider level of experience; however, a recent study demonstrated that provider experience and type of obstetrical training had no significant influence on the accuracy of clinical EFW. 6 We were, however, able to capture time of year of admission and demonstrated that increasing experience during residency training throughout the academic year did not have a significant impact on the accuracy of clinical EFW.
In conclusion, our study demonstrates that the accuracy of clinical EFW at term is not significantly impacted by maternal BMI, diagnosis of active labor, or fetal station when performed by resident physicians in a teaching hospital. Our study also shows that the correlation between clinical EFW and actual birth weight is overall weak, particularly in the subgroup of patients who went on to deliver macrosomic infants. While the majority of literature has demonstrated an equivalent accuracy between sonographic and clinical EFW, there has been recent suggestion that sonographic estimation of fetal weight actually may be more accurate at predicting birth weight in term patients with fetuses weighing >4000 grams.10-13 Further studies might support clinical EFW thresholds at which the addition of ultrasound estimation of fetal weight may aid in the identification of fetal macrosomia; however, our study suggests that clinical EFW at the time of admission for labor at term has little accuracy and limited value in modern obstetrics.
Acknowledgements
Declarations of Interest
1. Dr. Goetzinger is supported by a training grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (5 T32 HD055172) and from a NIH/NCRR Washington University CTSA grant (UL1RR024992). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official view of the NCRR or NIH.
2. Dr. Cahill is a Robert Wood Johnson Foundation Physician Faculty Scholar, which partially supports this work.
Footnotes
1. This paper was presented, in part, as a poster presentation at the 32nd Annual Meeting of the Society for Maternal-Fetal Medicine on February 9, 2012 in Dallas, TX.
References
- 1.American College of Obstetricians and Gynecologists . ACOG Practice Bulletin #22. American College of Obstetricians and Gynecologists; Washington DC: 2000. Fetal macrosomia. [Google Scholar]
- 2.Field NT, Piper JM, Langer O. The effect of maternal obesity on the accuracy of fetal weight estimation. Obstet Gynecol. 1995;86(1):102–107. doi: 10.1016/0029-7844(95)00096-A. [DOI] [PubMed] [Google Scholar]
- 3.Fox NS, Bhavsar V, Saltzman DH, Rebarber A, Chasen ST. Influence of maternal body mass index on the clinical estimation of fetal weight in term pregnancies. Obstet Gynecol. 2009;113(3):641–645. doi: 10.1097/AOG.0b013e3181998eef. [DOI] [PubMed] [Google Scholar]
- 4.Farrell T, Holmes R, Stone P. The effect of body mass index on three methods of fetal weight estimation. BJOG. 2002;109:651–657. doi: 10.1111/j.1471-0528.2002.01249.x. [DOI] [PubMed] [Google Scholar]
- 5.Noumi G, Collado-Khoury F, Bombard A, Julliard K, Weiner Z. Clinical and sonographic estimation of fetal weight performed in labor by residents. Am J Obstet Gynecol. 2005;192:1407–1409. doi: 10.1016/j.ajog.2004.12.043. [DOI] [PubMed] [Google Scholar]
- 6.Levin I, Gamzu R, Buchman V, et al. Clinical estimation of fetal weight: Is accuracy acquired with professional experience? Fetal Diagn Ther. 2011;29:321–324. doi: 10.1159/000323149. [DOI] [PubMed] [Google Scholar]
- 7.Weiss JL, Malone FD, Emig D, et al. Obesity, obstetric complications and cesarean delivery rate – a population-based screening study. FASTER Research Consortium. Am J Obstet Gynecol. 2004;190:1091–1097. doi: 10.1016/j.ajog.2003.09.058. [DOI] [PubMed] [Google Scholar]
- 8.Cedergren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004;103:219–224. doi: 10.1097/01.AOG.0000107291.46159.00. [DOI] [PubMed] [Google Scholar]
- 9.Blann DW, Prien SD. Estimation of fetal weight before and after amniotomy in the laboring gravid woman. Am J Obstet Gynecol. 2000;182:1117–1120. doi: 10.1067/mob.2000.105390. [DOI] [PubMed] [Google Scholar]
- 10.Sherman DJ, Arieli S, Tovbin J, Siegel G, Caspi E, Bukovsky I. A comparison of clinical and ultrasonic estimation of fetal weight. Obstet Gynecol. 1998;91:212–217. doi: 10.1016/s0029-7844(97)00654-6. [DOI] [PubMed] [Google Scholar]
- 11.Baum JD, Gussman D, Wirth JC., 3rd Clinical and patient estimation of fetal weight vs. ultrasound estimation. J Reprod Med. 2002;47:194–198. [PubMed] [Google Scholar]
- 12.Ashrafganjooei T, Naderi T, Eshrati B, Babapoor N. Accuracy of ultrasound, clinical and maternal estimates of birth weight in term women. East Mediterr Health J. 2010;16:313–317. [PubMed] [Google Scholar]
- 13.Peregrine E, O’Brien P, Jauniaux E. Clinical and ultrasound estimation of birth weight prior to induction of labor at term. Ultrasound Obstet Gynecol. 2007;29:304–309. doi: 10.1002/uog.3949. [DOI] [PubMed] [Google Scholar]