Abstract
The effectiveness of rheological blends of high molecular weight hyaluronic acid (HA) and low molecular weight hydroxypropyl methylcellulose (HPMC) in the prevention of peritoneal adhesions post-surgery is demonstrated. The physical mixture of the two carbohydrates increased the dwell time in the peritoneum while significantly improving the injectability of the polymer compared to hyaluronic acid alone. HA-HPMC treatment decreased the total adhesion area by ~70% relative to a saline control or no treatment in a repeated cecal injury model in the rabbit. No significant cytotoxicity and minimal inflammation was associated with the blend, and no chemical or physical processing was required prior to their use beyond simple mixing.
Keywords: peritoneal adhesions, hyaluronic acid, hydroxypropyl methylcellulose, rheological blends
1. Introduction
The prevention of post-operative peritoneal adhesions remains a significant challenge. Without intervention, adhesions occur in up to 93% of patients following abdominal surgery [1]. While some of these adhesions do not pose problems, others cause significant post-operative complications including chronic pain, infertility, and potentially lethal intestinal obstruction [2]. Furthermore, even non-symptomatic adhesions from previous surgeries can result in an additional risk of complications [3] and longer operation times [4] if subsequent surgeries are required.
To address this challenge, a variety of drugs, physical barrier materials, and combinations thereof have been evaluated. Steroidal [1, 5, 6] and non-steroidal [7, 8] anti-inflammatory drugs, anti-angiogenesis drugs [9, 10], tissue plasminogen activator [11], mitomycin C [12], and vitamin E [13] have all shown at least some efficacy at reducing adhesions. However, drug therapies alone have resulted in inconsistent efficacy in both animal models [14] and clinical trials [15], perhaps in part due to the rapid clearance of drugs from the peritoneal cavity. As an alternative, the development of barrier materials whose primary role is to maintain physical separation between the peritoneal wall and the viscera has become an area of intense research focus. A variety of barrier materials has been developed based primarily on hydrophilic polymers that may be injected as solutions, fabricated into membranes, or cross-linked to form hydrogels. Several hydrophilic polymers, including oxidized regenerated cellulose [16], dextran [17] and dextran derivatives [18], chitosan [19] and derivatives [20, 21], carboxymethyl cellulose [22], polyethylene glycol [23] or copolymers thereof [24–26], alginate [27], and hyaluronic acid [28–31], have been investigated and shown to have at least some benefit in adhesion prevention, both alone and in combination with drugs [7, 32]. In cases where hydrogels are used, the hydrogels are typically prepared in situ via UV photopolymerization [33] or via the use of in situ-gelling materials that gel thermally [21, 26, 34, 35] or via mixing of two reactive precursors via injection [36–39]. Hyaluronic acid has attracted particular interest for use as a solution [40], film [28], and hydrogel [41]-based adhesion prevention material given its demonstrated biocompatibility in the peritoneum, highly hygroscopic behavior, and high viscosity when a high molecular weight polymer is used. We have previously shown the efficacy of in situ cross-linking hyaluronic acid-based hydrogels consisting of hyaluronic acid alone [36] as well as hyaluronic acid mixed with other carbohydrates [42, 43] in preventing peritoneal adhesions. Such cross-linked hydrogels can function as a physical barrier [36, 42, 43] and/or as a drug delivery vehicle for dexamethasone [44], budesonide [37] and tissue-type plasminogen activator [38]. However, while these hydrogel-based vehicles are more effective than polymer solutions comprised of similar polymers (perhaps because of the increased residence time at the interface between the peritoneal wall and the viscera [42]), these approaches require chemical modification of the polymer precursors in order to facilitate gelation, increasing material costs, and introducing reactive functional groups that may affect biocompatibility adversely, and may create regulatory hurdles.
Rheological blends - solutions of two or more polymers that exhibit more gel-like properties when mixed relative to the constituent polymers formulated alone at the same concentrations - offer an alternative to chemical modification. Intermolecular interactions between the two constituent polymers, typically hydrogen bonding interactions between one high molecular weight polymer and one lower molecular weight polymer in the case of carbohydrates, can increase the effective cross-link density and thus the hydrogel-like properties of the mixture without compromising (or indeed improving) the injectability of the material [45]. The benefits of rheological blends have previously been applied in ocular surgery [46] and spinal repair [47], applying the blends as easily injectable rheological and/or structural materials as well as delivery vehicles for drugs [48, 49] and cells [50].
We have previously reported the development of rheological blends based on high molecular weight hyaluronic acid (HA) and low molecular weight hydroxypropyl methylcellulose (HPMC) [51] and their use as drug delivery vehicles for facilitating prolonged duration local anesthesia [52]. The incorporation of HPMC both facilitates the formation of (shear-reversible) hydrogen bonding interactions with HA to increase the mechanical strength of the blend without sacrificing injectability [46] and significantly reduces the hygroscopicity of HA to facilitate slower hydration and re-dissolution of the blend relative to HA solutions alone [51], thus potentially prolonging the residence time of the blend in the peritoneum. Here, we investigate the efficacy of these HA-HPMC rheological blends as physical barriers to prevent peritoneal adhesions, using a rabbit sidewall defect-cecum abrasion model [42]. We show that HA-HPMC blends significantly reduce the occurrence of peritoneal adhesions, on par with the chemically-crosslinkable HA-based hydrogels previously reported [42], without requiring any chemical modification whatsoever of the precursor polymers.
2. Materials and Methods
2.1 Materials
Hyaluronic acid (HA, Mw = 1.4MDa) was obtained from Genzyme Inc. (Cambridge, MA) and hydroxypropyl methylcellulose (HPMC, Mw = 86kDa) was obtained from Sigma-Aldrich (St. Louis, MO). Physical blends were prepared by dissolving both polymers in a defined volume of 0.9% sodium chloride to achieve the target mass percentages in the blend inside a 20 mL scintillation vial. Blends are abbreviated as HAxHPMCy, where x and y are the concentrations in wt% of HA and HPMC respectively.
2.2 In Vitro Cytotoxicity Evaluation
A MTT assay was used to evaluate the biocompatibility of the HA/HPMC blends with MeT-5A human mesothelial cells cultured in ATCC-recommended media (Medium199 with Earle’s balanced salt solution, 0.75 mM L-glutamine, 1.25 g/L sodium bicarbonate, 3.3 nM epidermal growth factor (EGF), 400 nM hydrocortisone, 870 nM insulin, 20 mM HEPES, and 10% fetal bovine serum). Cells were plated in 1mL aliquots in a 24-well plate at 50000 cells/well and permitted to adhere over 24 hours. Passages 3–25 of the cells were used for cytotoxicity studies. HA and HPMC were sterilized in their dry state under a UV lamp over a period of three hours, after which 0.9% saline solution was added aseptically. Syringes were loaded with material by transferring the blends into a 5 mL syringe using a spatula and then extruding the blends into a 1 mL syringe through a 16 gauge needle, all aseptically. Materials were applied to the plated cells using a 20G syringe in 0.1 mL aliquots, with four replicate wells tested for each material. Media-only and cell-only controls (also performed in quadruplicate) were included on each 24-well plate tested. At time points of 24 hours and 4 days after material addition, both the media and the test material were removed and replaced with 1 mL of fresh media and 150 μL MTT reagent (Promega, Madison, WI). Solubilization solution was added following four hours of incubation, and the plates were mixed on an orbital stirrer for 24 hours. Absorbances in each well were measured in duplicate in a 96-well plate using a multi-well plate reader (Molecular Devices, Sunnyvale, CA) at 570 nm.
2.3 Mouse Intraperitoneal Injections
Animals were cared for in compliance with protocols approved by the Massachusetts Institute of Technology Committee on Animal Care, in conformity with the NIH guidelines for the care and use of laboratory animals (NIH publication #85-23, revised 2011). Male SV129 mice weighing 25 g were purchased from Taconic (Hudson, NY) and housed in groups in a 6 AM–6 PM light-dark cycle. Mice were specific pathogen-free (SPF) for all common adventitial murine pathogens. Blends comprised of 3:2 HA:HPMC mass ratios were chosen for evaluation given the relatively slow hydration kinetics and the optimized secondary interactions between HA and HPMC observed at this mass ratio in previous work [51]. Polymer blends of concentrations HA3HPMC2 (5 wt% total concentration), HA4.5HPMC3 (7.5 wt% total concentration), and HA6HPMC4 (10 wt % total concentration) were sterilized by UV radiation for 3 hours, after which the dry polymer was dissolved in saline and loaded into 1 mL syringes. Mice were anesthetized with isoflurane and injected with 1 mL of the polymer blend into the peritoneal cavity using a 25G needle, representing polymer loadings of 2000–4000 mg/kg depending on the formulation used. Three mice were sacrificed at each of 1 day, 2 days, 4 days, 6 days, 8 days, 10 days, 12 days, 16 days, and 21 days post-injection and residual material including fluid (if present) was recovered for analysis and the volume recorded (n = 3). In each group, animal sacrifice ceased once there was no recoverable fluid in the peritoneum. Note that recovery of the fluid was likely incomplete, due to the difficulty of scraping it from between the viscera. However, this difficulty was common to all groups. The dissector was blinded as to which treatment individual mice had received. Abdominal contents were sampled as needed, fixed in Accustain fixative (Sigma-Aldrich, St. Louis, MO), and processed for histology (hematoxylin-eosin) using standard techniques.
2.4 Rheology
Rheology data was collected with an ARG-2 controlled stress oscillatory rheometer (TA Instruments, New Castle, DE) using a 40mm parallel plate geometry and a 0.8mm gap. Both the sample platform and the oscillating plate were masked using adhesive-backed 600 grit silicon carbide sandpaper to maximize the contact between the polymer blends and the test geometry. Stress sweeps were conducted at an angular frequency of 3 rad/s followed by frequency sweeps within the angular frequency (ω) range 0.1 < ω < 500 rad/s, controlled using a constant applied stress confirmed to lie within the linear viscoelastic range of the materials. Shear rate sweeps were then conducted using shear rates (γ) in the range 0.05 < γ < 200 s−1 to measure the shear thinning behavior of the materials. At least ten minutes were left between experiments to ensure the recovery of any secondary structure interactions between the different experiments.
2.5 Rabbit Repeated Injury Model
Animals were cared for in compliance with protocols approved by the Massachusetts Institute of Technology Committee on Animal Care, in conformity with the NIH guidelines for the care and use of laboratory animals (NIH publication #85-23, revised 2011). Peritoneal adhesions were induced in female albino rabbits (Oryctolagus cuniculus; New Zealand White, Covance, Hazelton, PA) (3 ± 0.2 kg) through repeated laparotomies as described previously [38]. In brief, de novo adhesions were induced by introducing a 3 × 4 cm defect (including the parietal peritoneum and approximately 1 mm of muscle) on the right lateral abdominal wall and by abrading seven cecal haustra with 80–160 strokes with a surgical brush. A second laparotomy was performed after one week to cut the adhesions and introduce additional injuries to the same locations as those injured in the first laparotomy. Bleeding was more extensive in the second laparotomy and excessive blood from the injury was removed. 10 mL of HA6HPMC4 were applied to the injured abdominal wall and cecum by extrusion directly from a 10 mL syringe (n = 4). Post-operative care of the animals is described elsewhere [36]. The animals were sacrificed 1 week after the second laparotomy by intravenous injection of sodium pentobarbital. Adhesions were scored using a modification of a reported method [53]: Score 0 = no adhesion; score 1 = tissue adhesions separable by gravity; score 2 = tissue adhesions separable by blunt dissection; and score 3 = tissue adhesions separable only by sharp dissection. Overall scores represent the highest adhesion score in the animal if multiple adhesions were present. The areas associated with score 2 and 3 adhesions were measured and are reported in terms of total adhesion area per animal. Tissues recovered from the necropsy were fixed in Accustain, embedded in paraffin, sectioned, and stained with hematoxylin and eosin for histological examination.
3. Results
3.1 Cytotoxicity of Rheological Blends
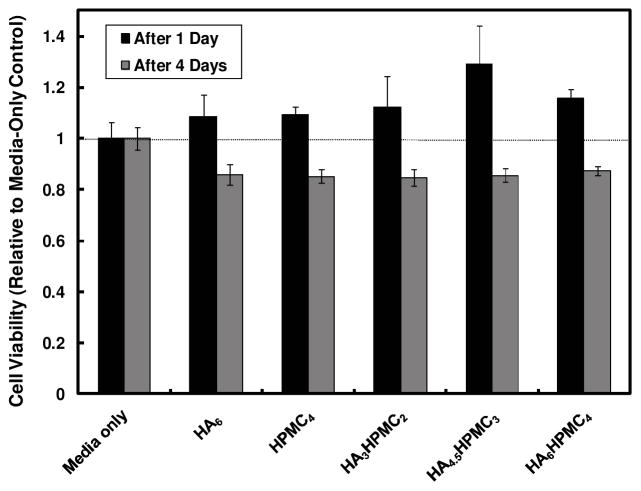
The cytotoxicity of hyaluronic acid (HA), hydroxypropyl methylcellulose (HPMC), and blends thereof (abbreviated as per Methods) at the concentrations tested in vivo were assayed in MeT-5A human mesothelial cells using an MTT assay (Figure 1).
Figure 1.
Cell viability (relative to media-only control) of MeT-5A mesothelial cells in the presence of HA only, HPMC only, and HA-HPMC blends at all tested concentrations
Cell viability increased slightly after 1 day of materials exposure and decreased slightly after 4 days of materials exposure, with at least 85–90% of MTT activity preserved in the presence of all tested materials combinations even after four days. These results suggests that mesothelial cells characteristic of the peritoneal wall were highly tolerant of HA, HPMC, and HA-HPMC blends, even at very high concentrations (10 mg/mL overall polymer concentration in the test well in the HA6HPMC4 blend tested).
3.2 Intraperitoneal injections in mice
As a screening test prior to using the materials in a rabbit model of peritoneal injury, the in vivo biocompatibility and persistence of various concentrations of HA-HPMC blends was assayed via percutaneous intraperitoneal injections in mice. Animals were injected with 1 mL of test solution, and the effects on the peritoneum were assessed upon necropsy 1, 2, 4, 6, 8, 10, 12, 16, and 21 days post-injection, as long as material was present in each group (n = 3 at each time point; please see section 2.3 for details). 3:2 weight ratio HA:HPMC blends were selected for testing based on their maximum rheological synergism (i.e. enhancement in viscosity as a result of mixing) relative to other compositions, as identified in our previous work [51]. Results are shown in Figure 2. Injection of blends resulted in distribution of fluid throughout the peritoneum, as can be seen in the separation of the viscera viewed through the anterior abdominal wall at the time of necropsy (Fig. 2a), where the loops of bowel are normally closely apposed. No mortality was observed as a result of any injection except for one mouse in which the colon was ruptured by the injection, even at the very high polymer concentrations tested (up to 4000 mg/kg).
Figure 2.
Intraperitoneal HA-HPMC blends in mice (a) Frontal view of translucent abdominal wall musculature and peritoneum (after reflection of the skin), 6 days after injection of HA6HPMC4. Viscera separated by fluid can be seen through the abdominal wall. (b) Effect of polymer concentration on the volume of fluid recovered from the peritoneal cavity as a function of time (n = 3 at each time point). (c) “Foamy” macrophages in peritoneal fluid 2 days after injection of HA6HPMC4. The lucent intracellular areas are ingested material. (d) Parietal peritoneal surface 2 days after injection of HA6HPMC4. The basophilic material in the upper part of the panel is the gel, with scattered macrophages). Histological findings were similar in all blends tested.
Significant differences in tissue reaction and the quantity and dwell time of residual fluid were observed as a function of the polymer blend concentration (Fig. 2b). After injection of HA3HPMC2, the viscera remained separated and did not develop adhesions in the first six days post-injection. A maximum of ~2 mL of clear fluid (blend plus absorbed water) were recovered. At eight days post-injection, no fluid could be recovered from the peritoneal cavity, and score 2 or 3 adhesions were observed in all animals between the peritoneal wall and the bowel and/or the corpus adiposum, a location corresponding to the site of the injection and hence most likely due to injection injury. When the polymer concentration of the blend was increased to HA4.5HPMC3, more fluid was recovered from the peritoneum at time points greater than two days post-injection relative to HA3HPMC2, (p < 0.03 for any pair-wise comparison) and the fluid was not completely resorbed until 6 days after injection (double the time it took with HA3HPMC2). Only one animal developed an adhesion (at 6 days post-injection), at the site of injection. The viscera appeared normal after the fluid had been resorbed. Further increasing the blend concentration to HA6HPMC4, extended the time that the blend remained in the peritoneum, with 1.5 mL of fluid still recoverable after 16 days and complete resorption not occurring until 3 weeks post-injection. Again, significantly more peritoneal fluid was recovered at time points greater than two days post-injection relative to the lower concentration blends tested (p < 0.02, ~4 mL maximum recovered 12 days post-injection), owing primarily to the high water binding capacity of HA present in its highest concentration in the HA6HPMC4 blend. No adhesions were observed at any time point in any animal. Therefore, the higher the total polymer concentration used and the longer the blend was present in the peritoneum, the lower the frequency of observed adhesions.
Hematoxylin-eosin stained slides of peritoneal fluid revealed scattered macrophages, many of them laden with ingested gel material (“foamy” macrophages, Fig. 2c). In samples where there was still macroscopic gel residue, stained sections of the peritoneum showed basophilic material in contact with the mesothelial surface, which was generally intact (Fig. 2d), except in samples where there were adhesions. In those, there was localized inflammation consisting of neutrophils, macrophages, and blood vessels penetrating the abdominal musculature. It is possible that pyrogens in the test compounds contributed to the relatively minimal inflammation seen. Histological appearances were similar between groups.
The injections of blends of HA and HPMC were compared to those of the separate polymers. Injection of 6 wt% HA resulted in significant abdominal distension; 4–5 mL of peritoneal fluid were recovered four days post-injection and 6–7 mL of peritoneal fluid were recovered six days post-injection (Fig. 2b), approximately twice the volume that accumulated with HA6HPMC4. Residual fluid from the HA-only injection remained in the peritoneum for 9 days (versus 16 days with HA6HPMC4, Fig. 2b). No adhesions were observed in any animals treated with HA6. With 4 wt% HPMC, the recovered peritoneal fluid volumes were less than the initial injection volume of 1 mL at all tested time points (Fig. 2b), and the material persisted only for ~5 days post-injection. One animal treated with HPMC4 was however observed to form an adhesion (score 3), associated with the site of injection.
In summary, the higher concentration blends were present in the peritoneum for much longer than either polymer alone and also caused less peritoneal distension than HA alone at a comparable concentration (although more than with HPMC) while still being effective at avoiding adhesion formation in all animals tested, unlike administration of HPMC alone. It should also be noted that neither HA10 nor HPMC10 can be injected through a standard 25G needle [51], the former because of very high yield stress, the latter because of high viscosity. The use of a HA-HPMC blend permits the application of significantly higher overall polymer concentrations (and thus longer retention times in the peritoneum) than would be achievable using either polymer alone.
3.3 Rheology of Recovered Blends
The time course of the rheological properties was studied in order to provide information regarding the relative importance of dilution and degradation on the blend lifetimes in vivo. HA6HPMC4 recovered at each tested time point was subjected to rheological characterization to probe both the dilution and degradation of the polymer blends as a function of time within the peritoneum. Figure 3a plots viscosity as a function of shear rate and Figure 3b shows the elastic modulus (G′) of the blends as a function of the applied oscillation stress (ω = 3 rad/s).
Figure 3.
Rheological response of recovered HA6HPMC4 after varying retention times in the peritoneum: (a) viscosity versus shear rate; (b) elastic modulus versus oscillation stress. Elastic modulus data for HA6 and HPMC4 (open points) are also shown for comparison.
Continuous reductions in viscosity (Fig. 3a), elastic modulus (Fig. 3b), and yield stress (Fig. 3b) were observed over time, consistent with continuous dilution and degradation of the blends. A large decrease in both viscosity and yield stress was observed for HA6HPMC4 after one day in vivo, but both the yield stress (i.e. the critical stress at which flow is observed) and the shear thinning ratio (i.e. the ratio between the high shear and low shear steady state viscosities in Fig. 3a) remained high, particularly in comparison to HPMC4. This result suggests that the HA component of the blend, which primarily determines both the yield stress and shear thinning ratio of the blend due to its significantly higher molecular weight relative to HPMC, remains largely un-degraded on day 1, and the viscosity loss occurs primarily via dilution. Further decreases in viscosity (Fig. 3a), shear thinning ratio (Fig. 3a), yield stress (Fig. 3b) and elastic modulus (Fig. 3b) were observed between two and four days of implantation over the entire stress range sampled, likely attributable to ongoing blend dilution, polymer resorption, and degradation of the enzymatically-cleavable HA component of the blend [54]. In the week following day 4, however, relatively little change was observed in the rheological response of the recovered peritoneal fluid, with yield stresses stabilizing at ~20 Pa and low-shear viscosities reducing only by a factor of ~4 between 4 days and 12 days following injection. These results suggest that the HA component of the blend was largely eliminated from the peritoneal fluid after four days, leaving predominantly HPMC - which degrades more slowly, is less hygroscopic, and has significantly lower yield stress - in the peritoneum. These findings are consistent with previous observations of HA residence times in vivo that reported a half life of ~1 day following injection of 1 wt% HA solution [55]; extrapolating this clearance rate over the full time scale of our study, only ~6% of the total mass of HA injected would still be present in the blend after 4 days, which would account for the significant drop-off in mechanical properties observed at that time point.
The same trends were noted with HA4.5HPMC3 only with lower initial values for viscosity, yield stress, and elastic modulus owing to the lower initial polymer concentration of the blends (see Supporting Information, Figure S1). As with the HA6HPMC4 blends, the results suggest that the blend changes from HA-rich to HPMC-rich over the first four days of implantation, a time period over which almost all of the observed decreases in viscosity and yield stress associated with the blends are observed (Figure S1). This change in net blend composition versus time due to the different stabilities of the constituent polymers in vivo may have important implications for predicting the biological responses to these materials (HA is involved in wound healing pathways, for example [56]) in addition to providing a better understanding of the mechanism of prolonged adhesion prevention.
3.4 Rabbit Repeated Injury Model
We tested the ability of HA6HPMC4 to prevent adhesions in a rabbit model of repeated injury that creates adhesions that are very difficult to prevent [38]. HA6HPMC4 was chosen among the blends based on its long demonstrated persistence time, higher viscosity one week post-injection, and the lack of observed adhesions in the mouse model at all time points tested. At laparotomy under general anesthesia, the cecum was abraded and a layer of abdominal wall muscle (along with the overlying peritoneum) was excised to induce adhesions. One week later, a second laparotomy was performed and the formed adhesions were cut, the injured surfaces re-abraded, and the injuries treated with HA6HPMC4 (n = 4, Fig. 4a); as controls, animals were either treated with saline or untreated after injury [38]. One week after this second injury, the animals were euthanized.
Figure 4.

In vivo assessment of adhesion prevention by HA6HPMC4 in a rabbit double injury model (a) application of the HA6HPMC4 blend immediately following the second injury (b) adhesion formation seven days after repeated injury following treatment with HA6HPMC4 (c) adhesion formation seven days after repeated injury following treatment with saline only.
No significant weight change (−0.5 ± 2.3 %) was observed between the second surgery when HA6HPMC4 was applied and necropsy one week later. This observed weight change following HA6HPMC4 application was not significantly different from the weight change observed in animals whose injuries were not treated (−3.5 ± 7.4 %, n = 6, p = 0.19 in a pair-wise comparison) but was less than that observed for saline-treated animals (−4.8 ± 1.8 %, n = 6, p = 0.01 in a pair-wise comparison) [38]. Little to no material residue was observed in any of the treated rabbits after the seven day treatment period, suggesting resorption of the blends largely occurs over the week following administration. No qualitative difference in healed tissue mechanics was observed between treated and control rabbits. Adhesions were observed in all rabbits, with at least some score 3 adhesions present in all animals. However, the area of those adhesions following HA6HPMC4 treatment (Fig. 4b, 4.1 ± 4.3 cm2) was ~70% less than that observed in untreated animals subjected to repeated injury (13.1 ± 6.0 cm2, n = 6, p = 0.01) or animals treated with only saline (Fig. 4c, 15.1 ± 5.2 cm2, n = 6, p = 0.004). Indeed, the HA6HPMC4 polymer blends performed as well as the injectable in situ cross-linking (hydrazide-aldehyde) hyaluronic acid hydrogels previously reported by Yeo et al. [38] at reducing adhesion area (p = 0.40 in a pair-wise comparison) without the need to modify the polymers in any way, albeit requiring a significantly higher weight fraction of polymer (10 wt% with the blend compared to 2 wt% with the in situ gel).
4. Discussion
Rheological blends based on high molecular weight hyaluronic acid and low molecular weight hydroxypropyl methylcellulose offer significant advantages over both polymer solutions and thermal or chemically cross-linked hydrogel formulations. These polymers, that interact via hydrogen bonding, clear much more slowly from the peritoneum than does hyaluronic acid alone (half life ~1 day in rabbits [55]). As a result, the material and the resulting protective effect versus adhesions can be maintained for more than the one week period that some have identified as required for complete healing of the peritoneal wall following trauma [58].
It should be emphasized that the double injury rabbit model used in this work is significantly more challenging than models used in other studies to evaluate compounds that show good efficacy in animal studies but relatively poorer performance in the clinic [59]. In this light, the observed ~70% reduction in adhesion area is of potential clinical significance for adhesion prevention.
The HA-HPMC blends have advantages over other materials previously reported for the prevention of peritoneal adhesions. First, both HA and HPMC are widely studied biomedical polymers that are already approved for use in a variety of in vivo environments (including in humans) and were not chemically modified prior to use relative to their approved forms. HA-HPMC blends could therefore be relatively easily translated into the clinic. Second, the HA-HPMC blends have properties that simplify administration, due to the weak hydrogen-bonding mechanism of viscosity building in which the cross-links can be reversibly broken by shear upon injection. Application of the hydrogels can be stopped and re-started as desired without fear of cross-linking within the syringe or needle, as is the case with many chemically cross-linked formulations. A single syringe can be used to apply the material instead of the double-barreled syringes required with in situ cross-linking systems. Third, the HA-HPMC blends exhibit linear viscoelastic behavior in that the material behaves as an elastic hydrogel at high shear rates but a viscous liquid at low shear rates [51]. Consequently, although the blend assumes a tubular shape templated by the needle as it is extruded out of the syringe, the blends can flow once applied in vivo, enabling the gel to more completely cover the contact area between the peritoneal wall and the peritoneal cavity.
Given the demonstrated potential of HA-HPMC blends for prolonging the release of drug in a local anesthetic model [52], we anticipate that the blends will also be effective matrices for the delivery of anti-adhesion drugs loaded in solution [38] (in which the blend directly regulates release via diffusion) and/or drug precipitates [60] or microscale or nanoscale drug delivery vehicles [61].
5. Conclusions
Rheological blends of high molecular weight hyaluronic acid and low molecular weight hydroxypropyl methylcellulose resulted in a ~ 70% reduction in the total adhesion area relative to saline-treated controls. The use of rheological blends significantly increases the residence time of the blends in the peritoneum relative to hyaluronic acid-based materials used alone. The polymers comprising the blend can form an effective barrier without the need for any chemical or physical modification and exhibit no significant cytotoxicity and a benign tissue response in vivo. HA-HPMC blends are potentially clinical useful materials for the prevention of peritoneal adhesions.
Supplementary Material
Acknowledgments
TH thanks the Natural Sciences and Engineering Research Council of Canada for funding. DSK acknowledges support of the DuPont-MIT Alliance and NIH GM073626.
Footnotes
Supplementary Material: Rheological characterization of 4.5 wt% HA/3 wt% HPMC blends injected intraperitoneally in mice and recovered at defined time points is provided.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Todd Hoare, Email: hoaretr@mcmaster.ca.
Yoon Yeo, Email: yyeo@purdue.edu.
Evangelia Bellas, Email: evangelia.bellas@gmail.com.
Joost P. Bruggeman, Email: j.p.bruggeman@acta.nl.
Daniel S. Kohane, Email: Daniel.Kohane@childrens.harvard.edu.
References
- 1.Weibel MA, Majno G. Peritoneal adhesions and their relation to abdominal surgery. A postmortem study. Am J Surg. 1973;126:345–53. doi: 10.1016/s0002-9610(73)80123-0. [DOI] [PubMed] [Google Scholar]
- 2.diZerega GS. Peritoneum, peritoneal healing, and adhesion formation. In: diZerega GS, editor. Peritoneal Surgery. New York: Springer; 2000. pp. 3–37. [Google Scholar]
- 3.Cheong YC, Laird SM, Li TC, Shelton JB, Ledger WL, Cooke ID. Peritoneal healing and adhesion formation/reformation. Hum Reprod Update. 2001;7:556–66. doi: 10.1093/humupd/7.6.556. [DOI] [PubMed] [Google Scholar]
- 4.Coleman MG, McLain AD, Moran BJ. Impact of previous surgery on time taken for incision and division of adhesions during laparotomy. Dis Colon Rectum. 2000;43:1297–9. doi: 10.1007/BF02237441. [DOI] [PubMed] [Google Scholar]
- 5.Kirdak T, Uysal E, Korun N. Assessment of effectiveness of different doses of methylprednisolone on intraabdominal adhesion prevention. Ulus Travma Acil Cer. 2008;14:188–91. [PubMed] [Google Scholar]
- 6.Cheong YC, Shelton JB, Laird SM, Li TC, Ledger WL, Cooke ID. Peritoneal fluid concentrations of matrix metalloproteinase-9, tissue inhibitor of metalloproteinase-1, and transforming growth factor-beta in women with pelvic adhesions. Fertil Steril. 2003;79:1168–75. doi: 10.1016/s0015-0282(03)00079-7. [DOI] [PubMed] [Google Scholar]
- 7.Abe H, Campeau JD, Rodgers KE, Ellefson DD, Girgis W, Dizerega GS. Peritoneal-Lavage Fluid Protease Levels after in-Vivo Administration of Tolmetin in Hyaluronic-Acid. J Surg Res. 1993;55:451–6. doi: 10.1006/jsre.1993.1168. [DOI] [PubMed] [Google Scholar]
- 8.Aldemir M, Ozturk H, Erten G, Buyukbayram H. The preventive effect of rofecoxib in postoperative intraperitoneal adhesions. Acta Chir Belg. 2004;104:97–100. doi: 10.1080/00015458.2003.11978403. [DOI] [PubMed] [Google Scholar]
- 9.Kim S, Lee S, Greene AK, Arsenault DA, Le H, Meisel J, et al. Inhibition of intra-abdominal adhesion formation with the angiogenesis inhibitor sunitinib. J Surg Res. 2008;149:115–9. doi: 10.1016/j.jss.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Moraloglu O, Isik H, Kilic S, Sahin U, Caydere M, Ustun H, et al. Effect of bevacizumab on postoperative adhesion formation in a rat uterine horn adhesion model and the correlation with vascular endothelial growth factor and Ki-67 immunopositivity. Fertil Steril. 2011;95:2638–41. doi: 10.1016/j.fertnstert.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Montz FJ, Fowler JM, Wolff AJ, Lacey SM, Mohler M. The Ability of Recombinant Tissue Plasminogen-Activator to Inhibit Post-Radical Pelvic-Surgery Adhesions in the Dog-Model. Am J Obstet Gynecol. 1991;165:1539–42. doi: 10.1016/0002-9378(91)90402-d. [DOI] [PubMed] [Google Scholar]
- 12.Liu YC, Li H, Shu XZ, Gray SD, Prestwich GD. Crosslinked hyaluronan hydrogels containing mitomycin C reduce postoperative abdominal adhesions. Fertil Steril. 2005;83:1275–83. doi: 10.1016/j.fertnstert.2004.09.038. [DOI] [PubMed] [Google Scholar]
- 13.de la Portilla F, Ynfante I, Bejarano D, Conde J, Fernandez A, Ortega JM, et al. Prevention of peritoneal adhesions by intraperitoneal administration of vitamin E: An experimental study in rats. Dis Colon Rectum. 2004;47:2157–61. doi: 10.1007/s10350-004-0741-6. [DOI] [PubMed] [Google Scholar]
- 14.Ruoslahti E, Bhatia SN, Sailor MJ. Targeting of drugs and nanoparticles to tumors. The Journal of Cell Biology. 2010;188:759–68. doi: 10.1083/jcb.200910104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allen TM. Ligand-targeted therapeutics in anticancer therapy. Nat Rev Cancer. 2002;2:750–63. doi: 10.1038/nrc903. [DOI] [PubMed] [Google Scholar]
- 16.Ortegamoreno J, Caballerogomez JM. Postoperative Adhesion after Uterine Horn Surgery in the Rat, with the Use of Tc7. European Journal of Obstetrics Gynecology and Reproductive Biology. 1993;48:51–9. doi: 10.1016/0028-2243(93)90053-f. [DOI] [PubMed] [Google Scholar]
- 17.Rozga J, Ahren B, Bengmark S. Prevention of Adhesions by High-Molecular-Weight Dextran in Rats - Reevaluation in 9 Experiments. Acta Chir Scand. 1990;156:763–9. [PubMed] [Google Scholar]
- 18.Baca B, Boler DE, Onur E, Akca O, Hamzaoglu I, Karahasanoglu T, et al. Icodextrin and Seprafilm((R)) do not interfere with colonic anastomosis in rats. Eur Surg Res. 2007;39:318–23. doi: 10.1159/000104416. [DOI] [PubMed] [Google Scholar]
- 19.Yeo Y, Burdick JA, Highley CB, Marini R, Langer R, Kohane DS. Peritoneal application of chitosan and UV-cross-linkable chitosan. Journal of Biomedical Materials Research Part A. 2006;78A:668–75. doi: 10.1002/jbm.a.30740. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy R, Costain DJ, McAlister VC, Lee TDG. Prevention of experimental postoperative peritoneal adhesions by N,O-carboxymethyl chitosan. Surgery. 1996;120:866–70. doi: 10.1016/s0039-6060(96)80096-1. [DOI] [PubMed] [Google Scholar]
- 21.Wei CZ, Hou CL, Gu QS, Jiang LX, Zhu B, Sheng AL. Efficacy of Thermosensitive Hydroxybutyl Chitosan in Prevention of Post-operative Abdominal Adhesions in a Rat Model. Iran Polym J. 2009;18:355–64. [Google Scholar]
- 22.Moll HD, Schumacher J, Wright JC, Spano JS. Evaluation of Sodium Carboxymethylcellulose for Prevention of Experimentally Induced Abdominal Adhesions in Ponies. Am J Vet Res. 1991;52:88–91. [PubMed] [Google Scholar]
- 23.Nagelschmidt M, Saad S. Influence of polyethylene glycol 4000 and dextran 70 on adhesion formation in rats. J Surg Res. 1997;67:113–8. doi: 10.1006/jsre.1996.4973. [DOI] [PubMed] [Google Scholar]
- 24.Sawhney AS, Pathak CP, Vanrensburg JJ, Dunn RC, Hubbell JA. Optimization of Photopolymerized Bioerodible Hydrogel Properties for Adhesion Prevention. J Biomed Mater Res. 1994;28:831–8. doi: 10.1002/jbm.820280710. [DOI] [PubMed] [Google Scholar]
- 25.Bakkum EA, Trimbos JB, Dalmeijer RAJ, Vanblitterswijk CA. Preventing Postoperative Intraperitoneal Adhesion Formation with Polyactive(Tm), a Degradable Copolymer Acting as a Barrier. J Mater Sci-Mater M. 1995;6:41–5. [Google Scholar]
- 26.Zhang Z, Ni J, Chen L, Yu L, Xu JW, Ding JD. Biodegradable and thermoreversible PCLA-PEG-PCLA hydrogel as a barrier for prevention of post-operative adhesion. Biomaterials. 2011;32:4725–36. doi: 10.1016/j.biomaterials.2011.03.046. [DOI] [PubMed] [Google Scholar]
- 27.Cho WJ, Oh SH, Lee JH. Alginate Film as a Novel Post-Surgical Tissue Adhesion Barrier. J Biomat Sci-Polym E. 2010;21:701–13. doi: 10.1163/156856209X435835. [DOI] [PubMed] [Google Scholar]
- 28.Beck DE. The role of Seprafilm(TM) bioresorbable membrane in adhesion prevention. Eur J Surg. 1997;163:49–55. [PubMed] [Google Scholar]
- 29.Belluco C, Meggiolaro F, Pressato D, Pavesio A, Bigon E, Dona M, et al. Prevention of postsurgical adhesions with an autocrosslinked hyaluronan derivative gel. J Surg Res. 2001;100:217–21. doi: 10.1006/jsre.2001.6248. [DOI] [PubMed] [Google Scholar]
- 30.Sawada T, Tsukada K, Hasegawa K, Ohashi Y, Udagawa Y, Gomel V. Cross-linked hyaluronate hydrogel prevents adhesion formation and reformation in mouse uterine horn model. Hum Reprod. 2001;16:353–6. doi: 10.1093/humrep/16.2.353. [DOI] [PubMed] [Google Scholar]
- 31.Burns JW, Colt MJ, Skinner KC. Hyaluronic-Acid as a Surgical Aid in the Prevention of Adhesions. J Cell Biochem. 1993:110. [Google Scholar]
- 32.Hubbell JA. Hydrogel systems for barriers and local drug delivery in the control of wound healing. J Controlled Release. 1996;39:305–13. [Google Scholar]
- 33.Hillwest JL, Chowdhury SM, Sawhney AS, Pathak CP, Dunn RC, Hubbell JA. Prevention of Postoperative Adhesions in the Rat by in-Situ Photopolymerization of Bioresorbable Hydrogel Barriers. Obstet Gynecol. 1994;83:59–64. [PubMed] [Google Scholar]
- 34.Ahn HS, Lee HJ, Yoo MW, Jeong SH, Han TS, Kim WH, et al. Efficacy of an Injectable Thermosensitive Gel on Postoperative Adhesion in Rat Model. J Korean Surg Soc. 2010;79:239–45. [Google Scholar]
- 35.Yang B, Gong CY, Qian ZY, Zhao X, Li ZY, Qi XR, et al. Prevention of post-surgical abdominal adhesions by a novel biodegradable thermosensitive PECE hydrogel. BMC Biotechnol. 2010:10. doi: 10.1186/1472-6750-10-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yeo Y, Highley CB, Bellas E, Ito T, Marini R, Langer R, et al. In situ cross-linkable hyaluronic acid hydrogels prevent post-operative abdominal adhesions in a rabbit model. Biomaterials. 2006;27:4698–705. doi: 10.1016/j.biomaterials.2006.04.043. [DOI] [PubMed] [Google Scholar]
- 37.Yeo Y, Adil M, Bellas E, Astashkina A, Chaudhary N, Kohane DS. Prevention of peritoneal adhesions with an in situ cross-linkable hyaluronan hydrogel delivering budesonide. J Controlled Release. 2007;120:178–85. doi: 10.1016/j.jconrel.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 38.Yeo Y, Bellas E, Highley CB, Langer R, Kohane DS. Peritoneal adhesion prevention with an in situ cross-linkable hyaluronan gel containing tissue-type plasminogen activator in a rabbit repeated-injury model. Biomaterials. 2007;28:3704–13. doi: 10.1016/j.biomaterials.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 39.Falabella CA, Melendez MM, Weng LH, Chen WL. Novel Macromolecular Crosslinking Hydrogel to Reduce Intra-Abdominal Adhesions. J Surg Res. 2010;159:772–8. doi: 10.1016/j.jss.2008.09.035. [DOI] [PubMed] [Google Scholar]
- 40.Mitchell JD, Lee R, Hodakowski GT, Neya K, Harringer W, Valeri CR, et al. Prevention of Postoperative Pericardial Adhesions with a Hyaluronic-Acid Coating Solution - Experimental Safety and Efficacy Studies. J Thorac Cardiovasc Surg. 1994;107:1481–8. [PubMed] [Google Scholar]
- 41.Kocak I, Unlu C, Akcan Y, Yakin K. Reduction of adhesion formation with cross-linked hyaluronic acid after peritoneal surgery in rats. Fertil Steril. 1999;72:873–8. doi: 10.1016/s0015-0282(99)00368-4. [DOI] [PubMed] [Google Scholar]
- 42.Ito T, Yeo Y, Highley CB, Bellas E, Benitez CA, Kohane DS. The prevention of peritoneal adhesions by in situ cross-linking hydrogels of hyaluronic acid and cellulose derivatives. Biomaterials. 2007;28:975–83. doi: 10.1016/j.biomaterials.2006.10.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ito T, Yeo Y, Highley CB, Bellas E, Kohane DS. Dextran-based in situ cross-linked injectable hydrogels to prevent peritoneal adhesions. Biomaterials. 2007;28:3418–26. doi: 10.1016/j.biomaterials.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 44.Ito T, Fraser IP, Yeo Y, Highley CB, Bellas E, Kohane DS. Anti-inflammatory function of an in situ cross-linkable conjugate hydrogel of hyaluronic acid and dexamethasone. Biomaterials. 2007;28:1778–86. doi: 10.1016/j.biomaterials.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 45.Lapasin R, Pricl S. Rheology of Industrial Polysaccharides: Theory and Application. Cornwall, U.K: Blackie Academic and Professional; 1995. [Google Scholar]
- 46.Maltese A, Borzacchiello A, Mayol L, Bucolo C, Maugeri F, Nicolais L, et al. Novel polysaccharides-based viscoelastic formulations for ophthalmic surgery: rheological characterization. Biomaterials. 2006;27:5134–42. doi: 10.1016/j.biomaterials.2006.05.036. [DOI] [PubMed] [Google Scholar]
- 47.Gupta D, Tator CH, Shoichet MS. Fast-gelling injectable blend of hyaluronan and methylcellulose for intrathecal, localized delivery to the injured spinal cord. Biomaterials. 2006;27:2370–9. doi: 10.1016/j.biomaterials.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 48.Stanwick JC, Baumann MD, Shoichet MS. In vitro sustained release of bioactive anti-NogoA, a molecule in clinical development for treatment of spinal cord injury. International journal of pharmaceutics. 2012;426:284–90. doi: 10.1016/j.ijpharm.2012.01.035. [DOI] [PubMed] [Google Scholar]
- 49.Kang CE, Poon PC, Tator CH, Shoichet MS. A New Paradigm for Local and Sustained Release of Therapeutic Molecules to the Injured Spinal Cord for Neuroprotection and Tissue Repair. Tissue Eng Pt A. 2009;15:595–604. doi: 10.1089/ten.tea.2007.0349. [DOI] [PubMed] [Google Scholar]
- 50.Ballios BG, Cooke MJ, van der Kooy D, Shoichet MS. A hydrogel-based stem cell delivery system to treat retinal degenerative diseases. Biomaterials. 2010;31:2555–64. doi: 10.1016/j.biomaterials.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 51.Hoare T, Zurakowski D, Langer R, Kohane DS. Rheological blends for drug delivery. I. Characterization in vitro. J Biomed Mater Res A. 2010;92A:575–85. doi: 10.1002/jbm.a.32392. [DOI] [PubMed] [Google Scholar]
- 52.Hoare T, Bellas E, Zurakowski D, Kohane DS. Rheological blends for drug delivery. II. Prolongation of nerve blockade, biocompatibility, and in vitro-in vivo correlations. J Biomed Mater Res A. 2010;92A:586–95. doi: 10.1002/jbm.a.32420. [DOI] [PubMed] [Google Scholar]
- 53.Burns JM, Skinner K, Colt J, Sheidlin A, Bronson R, Yaacobi Y, et al. Prevention of tissue injury and postsurgical adhesions by precoating tissues with hyaluronic acid solutions. J Surg Res. 1995;59:644–52. doi: 10.1006/jsre.1995.1218. [DOI] [PubMed] [Google Scholar]
- 54.Zhong SP, Campoccia D, Doherty PJ, Williams RL, Benedetti L, Williams DF. Biodegradation of hyaluronic acid derivatives by hyaluronidase. Biomaterials. 1994;15:359–65. doi: 10.1016/0142-9612(94)90248-8. [DOI] [PubMed] [Google Scholar]
- 55.Edelstam GAB, Laurent UBG, Lundkvist ÖE, Fraser JRE, Laurent TC. Concentration and turnover of intraperitoneal hyaluronan during inflammation. Inflammation. 1992;16:459–69. doi: 10.1007/BF00918972. [DOI] [PubMed] [Google Scholar]
- 56.Price RD, Myers S, Leigh IM, Navsaria HA. The role of hyaluronic acid in wound healing: assessment of clinical evidence. American Journal of Clinical Dermatology. 2005;6:393–402. doi: 10.2165/00128071-200506060-00006. [DOI] [PubMed] [Google Scholar]
- 57.Yeo Y, Ito T, Bellas E, Highley CB, Marini R, Kohane DS. In situ cross-linkable hyaluronan hydrogels containing polymeric nanoparticles for preventing postsurgical adhesions. Annals of Surgery. 2007;245:819–24. doi: 10.1097/01.sla.0000251519.49405.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vrijland WW, Tseng LNL, Eijkman HJM, Hop WC, Jakimowicz JJ, Leguit P, et al. Fewer intraperitoneal adhesions with use of hyaluronic acid-carboxymethylcellulose membrane - A randomized clinical trial. Ann Surg. 2002;235:193–9. doi: 10.1097/00000658-200202000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wiseman DM. Animal adhsion models: design, variables, and relevance. In: diZerega GS, editor. Peritoneal Surgery. New York: Springer; 2000. pp. 459–76. [Google Scholar]
- 60.Yeo Y, Adil M, Bellas E, Astashkina A, Chaudhary N, Kohane DS. Prevention of peritoneal adhesions with an in situ cross-linkable hyaluronan hydrogel delivering budesonide. J Controlled Release. 2007;120:178–85. doi: 10.1016/j.jconrel.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 61.Adibelli MA, Ozcan AH, Kismet K, Erel S, Kilicoglu B, Gollu A, et al. Does povidone-iodine liposome hydrogel influence postoperative intraabdominal adhesions? Acta Chir Belg. 2006;106:578–80. doi: 10.1080/00015458.2006.11679955. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.