Abstract
Background
During laparoscopy, insufflation of an inert gas in the peritoneal cavity creates a working space to facilitate surgery. The space should be large enough to facilitate surgery without increasing intra-abdominal pressure (IAP) over a threshold limit (usually 15 mm Hg).
Objectives
This experimental study was performed to evaluate the effects of increasing in intra-abdominal pressure on internal organs.
Materials and Methods
Twenty female mixed breed dogs (20 ± 3 kg, 18 ± 1.2 months) were selected. They were randomly divided to two groups (n = 10). The intra-abdominal pressure was maintained 12 mm Hg and 20 mm Hg during the operation in control group and in test group respectively.
Results
Histopathologic evaluations revealed more pathological changes at the kidney of all the dogs in test group in comparison to control group.
Conclusions
Our findings revealed that organs that their blood supplies are related to one single or two arteries and their blood drainage are related to one or two veins are more sensitive to increased intra-abdominal pressure.
Keywords: Laparoscopy, Pneumoperitoneum, Kidney, Liver, Pancreas, Spleen
1. Background
Creation of working space by insufflating an inert gas during laparoscopy is essential in most procedures to facilitate surgery (1). The space should be large enough to facilitate surgery but it is mostly accepted not to reach over a threshold limit (usually 15 mm Hg) (1). Carbon dioxide has been commonly used to induce pneumoperitonium in laparoscopic operations. The valuable advantages make this gas widely preferable in laparoscopy surgeries, such as its high solubility and rapidly absorption in the blood, therefore minimizing the risk of gas embolism, (1, 2) and lose of the risk of combustion, (2) the possibility of permitting a safe electro cautery, (1) make CO2 a suitable and reliable gas for induction the space in abdominal cavity in laparoscopic operations. Although insufflate the intra-peritoneal space with CO2 have some potential disadvantages such as abdominal injuries and cardiovascular and respiratory disorders, but with exception of some critically ill patients, this procedures is widely accepted (1).
Most of laparoscopic complications occur during the entrance of trocars into the abdominal cavity. Indeed at least 50% of all complications at laparoscopic operations are related access technique and take place before the operation commences (3, 4). For decreasing the risk of entry-related injuries several methods have been explored over 50 years and no technique has been recognized as the safest access technique (5-9). One of the methods that described to surmount this complication is inducing peritoneal hyper-distention (10, 11). In this technique before the insertion of the first trocar, the intra-abdominal pressure reaches as much as 25 – 30 mm Hg by using a Veress needle (10). This technique creates greater space and therefore decreases the risk of inducing damages to the viscera by trocars. The intra-abdominal pressure reduces to 15 mm Hg immediately after entrance of trocars (4, 6, 10-12). It is important to mention that the greater intra-abdominal space will reduce the risk of complications during the entrance of trocars and during the operation (10, 11). Nowadays the important question is that “what happens if the intra-abdominal pressure remains in high levels?” Although there are some studies that revealed no significant cardiopulmonary effects in high intra-abdominal pressure, (12) the high pressure technique has not gained popularity. One possible reason is anesthetic concerns that may be influenced by high intra-peritoneal pressure (9, 13-17).
2. Objectives
The purpose of this study was to evaluate the pathological effects of intra-abdominal high-pressure (20 mmHg) on the viscera including Kidney, Pancreas, Spleen and Liver during laparoscopic operations.
3. Materials and Methods
Twenty female mixed breed dogs which were chose for an experimental procedure were prepared. Average of weight was 20 ± 3 kilograms and average of age was recorded 18 ± 1.2 months. Clinical and biochemical exams before operation were performed and did not show any sign of diseases or disturbances. All experiments were performed according to European Animal Care Committee guidelines. Dogs were used in laparoscopy training center of Tehran University of Medical Science as a model and undergoing a Cholecystectomy procedure with no technical complications and suffered operation with no mortality. They were randomly divided to two groups (n = 10). Acepromazine was administrated in all dogs (KELA Laboratoria NV. Hoostraten / Belgum) (0.05 mg/Kg) by intramuscular route as premedication. Induction of anesthesia was accomplished by intravenous injection of ketamine (10 mg/kg) (alfasan Woerden-Holland) and Diazepam (Dr. Amidi Ins. Iran) (0.2 mg/kg). For maintenance of anesthesia, slow infusion of ketamine (0.1 mg/kg/h) was used. All animals were treated pre-operativly with ketoprofen (2 mg/kg, IV). Laparoscopic procedure and induction of insufflation was performed with Richard WOLF devices and instruments.
In control group the intra-abdominal pressure was maintained 12 mm Hg and in test group 20 mm Hg during the operation (Insufflator: Richard WOLF 2233). This condition was maintained at least for 4 hours. The dogs were euthanized with IV injection of pentobarbital sodium and samples were taken from liver, pancreas, kidney and spleen for histopathologic evaluations. After standard fixation of the samples and preparation of the histological blocks, H&E staining was performed and several factors were evaluated.
Data were compared between control and test groups. Effects of intra-abdominal pressure on the mentioned tissues were evaluated by histopathologic indexes and the data were analyzed using an ANOVA for repeated measures.
4. Results
There were no differences between dogs in body weight, age and the procedure of general anesthesia. In heart rate evaluation at equal intervals, no significant differences were observed over time between the two groups. Also in respiratory rate, there were no significant differences (P>0.05). Results of end tidal CO2 measurements did not show severe hypoventilation during anesthesia in both groups. Comparison of this data between groups did not show any significant difference (P > 0.05). The mean of hemoglobin saturation measurements in the two groups did not show any significant difference (P > 0.05).
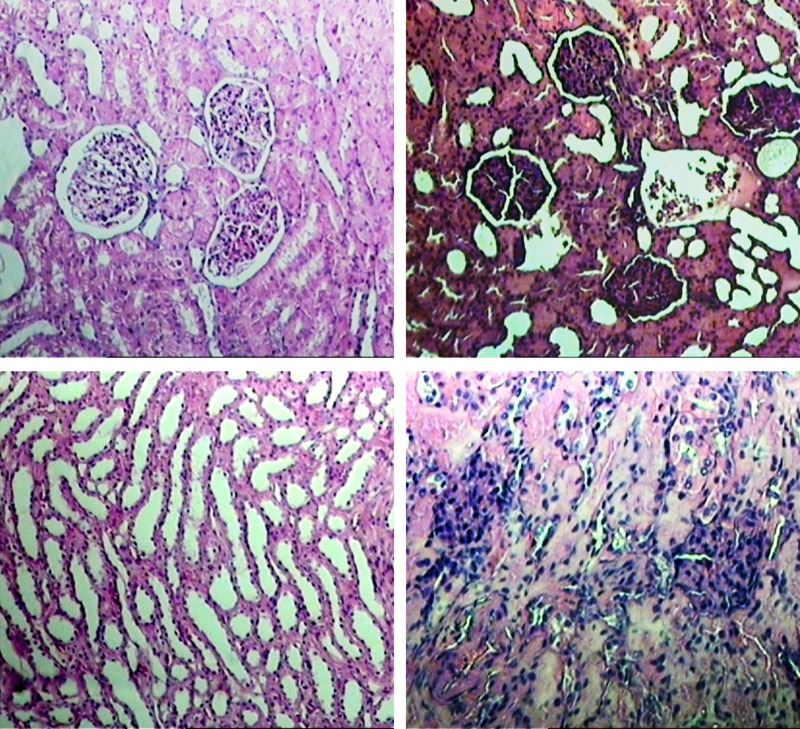
Histopathologic evaluations revealed pathological changes at the kidney of all the dogs in test group (intraabdominal pressure: 20 mm Hg) (Figure 1) in comparison to control group (intra-abdominal pressure: 12 mm Hg) (Figure 2). These pathological changes included: coagulation necrosis, glomerulonephritis and fatty changes. Fatty changes were stronger at distal tubules in comparison with proximal tubules.
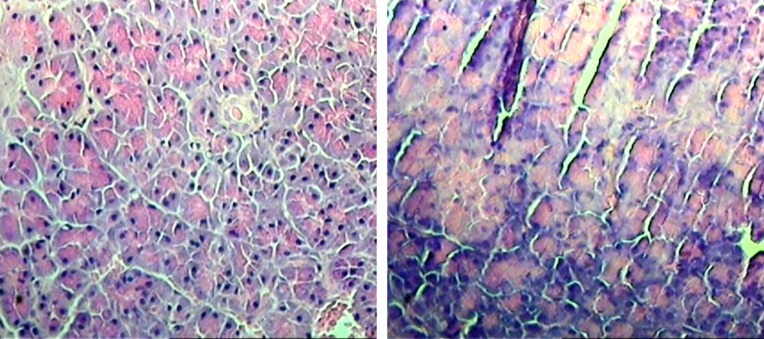
Figure 1. Pancreas Acinar Necrosis.
(a) normal acinar histological section of pancreas (control group), (b) acinar necrosis histopathological section of pancreas (test group; intraabdominal pressure: 20 mm Hg).
Figure 2. Kidney Histopathological Changes.
(a) Normal renal cortex histological section (control group), (b) necrosis of renal cortex (test group; intraabdominal pressure: 20 mm Hg), (c) normal medullary tubules (test group; intraabdominal pressure: 20 mm Hg), (d) more sever necrosis of renal cortex (test group; intraabdominal pressure: 20 mm Hg).
The pathologic changes at the liver were similar in both groups and were mild. These changes included mild coagulation necrosis in the parenchyma, hyperplasia at the smooth muscles and congestion. The differences between two groups were not significant. The pathologic change that was significant in test group at the pancreases was acinar necrosis. This change was observed only in samples of test group. Any pathologic change at the spleen was not detected in two groups.
5. Discussion
Nowadays laparoscopy procedures are performed widely all over the world for several purposes. It is essential to evaluate different aspects of this procedure and investigate about the possible complications in experimental studies. One of the most important aspects of laparoscopy procedures is intra-abdominal pressure during the operation.
Although Arterial PaO2, oxygen saturation, and end tidal Co2 remained unchanged in low and high levels of IAP, Yavuz et al. showed that in 24 mmHg tissue blood flow was significantly decreased in some organs such as spleen, pancreas, esophagus, and gastric mucosal in pigs (18) The present study investigates if this decrease of blood flow may cause degenerative changes in these organs.
Although Hung et al. in 1995 revealed that different limits of intra-abdominal pressure routinely used during laparoscopic surgery did not affect metabolic function, acid-base balance, or hemodynamics in the experimental model but absorption of Co2 across the peritoneum during the laparoscopic operations may affect vital organs by introduction of acidemia, hypercapnea, and depressed hemodynamics (19).
The present study showed that increase of intraabdominal pressure during the operation may cause pathological effects on internal organs. Although hemodynamic changes in kidney are mostly transient and reversible after a period of two hours in normal limits of intra-abdominal pressures, these degenerative changes may affects the kidneys permanently at high pressures (20). Three factors that may affect hemodynamic of kidney as an important organ during high levels of intra-abdominal pressure in laparoscopic surgeries, are local compressing effect, decreased cardiac output, and decreased venous return. Mild effects on renal parenchymal perfusion are probably related to local compressing effect during pneumoperitonium (21). Besides these effects, concentration of endothelin after renal vein compression that occurres during pneumoperitonium may elevate at high levels of intra-abdominal pressure and may contribute to oliguria (22). It is important to mention that intra-abdominal pressure has more influence on organs than type of the gas used for insufflations (23).
Present study showed that increased intra-abdominal pressure has pathological effects mostly on kidney and then pancreas. Also this study revealed that increased intra-abdominal pressure does not have any significant effects on liver or spleen. These finding showed that organs that their blood supplies are related to one single or two arteries and their blood drainage are related to one or two veins are more sensitive to increased intra-abdominal pressure.
Acknowledgments
We would like to thank Behnam Osouli, Manager of Aryan Tandorost Co., agent of Richard WOLF Germany Co., in Iran for providing the laparoscopic device and instruments.
Footnotes
Implication for health policy makers/practice/research/medical education:
Increasing the intra-abdominal pressure during the laparoscopic procedures may contribute to damage in organs such as kidney. Keeping the intra-abdominal pressure in standard and acceptable limits guarantees the health of internal organs.
Authors’ Contribution:
No distribution of activities been reported.
Financial Disclosure:
None declared.
Funding/Support:
This study was performed under financial support of laparoscopy training center, Aryan Tandorost Co (Richard-WOLF company) and Islamic Azad University, Khorramabad Branch (No of agreement: 05171382543).
References
- 1.Clergue F, Morel P, Pastor CM. Perioperative management of patients with increased risk of laparoscopy-induced hepatic hypoperfusion. Swiss medical weekly. 2004;134(3/4):39–43. doi: 10.4414/smw.2004.10355. [DOI] [PubMed] [Google Scholar]
- 2.Hadi MA, Zakaria H, Almulhim A, Alghamdi A, Mowafi H, Hussien A. Gas or Gas-Less Laparoscopic Cholecystectomy? Kuwait Medical Journal. 2002;34:292–5. [Google Scholar]
- 3.Vilos GA. Laparoscopic bowel injuries: forty litigated gynaecological cases in Canada. J Obstet Gynaecol Can. 2002;24(3):224–30. doi: 10.1016/s1701-2163(16)30222-5. [DOI] [PubMed] [Google Scholar]
- 4.Vilos GA, Vilos AG. Safe Laparoscopic Entry Guided by Veress Needle CO2 Insufflation Pressure. Journal Am Assoc Gyn Lap. 2003;10(3):415–20. doi: 10.1016/S1074-3804(05)60277-0. [DOI] [PubMed] [Google Scholar]
- 5.A consensus document concerning laparoscopic entry techniques: Middlesbrough, March 19–20 1999. Gynaecological Endoscopy. 1999;8(6):403–406. doi: 10.1046/j.1365-2508.1999.00309.x. [DOI] [Google Scholar]
- 6.Garry R. Towards evidence-based laparoscopic entry techniques: clinical problems and dilemmas. Gynaecol Endosc. 1999;8(6):315–26. doi: 10.1046/j.1365-2508.1999.00310.x. [DOI] [Google Scholar]
- 7.Merlin TL, Hiller JE, Maddern GJ, Jamieson GG, Brown AR, Kolbe A. Systematic review of the safety and effectiveness of methods used to establish pneumoperitoneum in laparoscopic surgery. Br J Surg. 2003;90(6):668–79. doi: 10.1002/bjs.4203. [DOI] [PubMed] [Google Scholar]
- 8.Molloy D, Kaloo PD, Cooper M, Nguyen TV. Laparoscopic entry: a literature review and analysis of techniques and complications of primary port entry. Aust N Z J Obstet Gynaecol. 2002;42(3):246–54. doi: 10.1111/j.0004-8666.2002.00246.x. [DOI] [PubMed] [Google Scholar]
- 9.Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer HJ, Cuschieri A, et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc. 2002;16(7):1121–43. doi: 10.1007/s00464-001-9166-7. [DOI] [PubMed] [Google Scholar]
- 10.Reich H, Rasmussen C, Vidali A. Peritoneal hyperdistention for trocar insertion. Gynaecol Endosc. 1999;8(6):375–7. doi: 10.1046/j.1365-2508.1999.00340.x. [DOI] [Google Scholar]
- 11.Reich H, Ribeiro SC, Rasmussen C, Rosenberg J, Vidali A. High-pressure trocar insertion technique. JSLS. 1999;3(1):45–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Phillips G, Garry R, Kumar C, Reich H. How much gas is required for initial insufflation at laparoscopy? Gynaecol Endosc. 1999;8(6):369–74. doi: 10.1046/j.1365-2508.1999.00342.x. [DOI] [Google Scholar]
- 13.Abu-Rafea B, Vilos GA, Vilos AG, Ahmad R, Hollett-Caines J, Al-Omran M. High-pressure laparoscopic entry does not adversely affect cardiopulmonary function in healthy women. J Minim Invasive Gynecol. 2005;12(6):475–9. doi: 10.1016/j.jmig.2005.07.393. [DOI] [PubMed] [Google Scholar]
- 14.Greim CA, Broscheit J, Kortlander J, Roewer N, Schulte am Esch J. Effects of intra-abdominal CO2-insufflation on normal and impaired myocardial function: an experimental study. Acta Anaesthesiol Scand. 2003;47(6):751–60. doi: 10.1034/j.1399-6576.2003.00135.x. [DOI] [PubMed] [Google Scholar]
- 15.Gutt CN, Oniu T, Mehrabi A, Schemmer P, Kashfi A, Kraus T, et al. Circulatory and respiratory complications of carbon dioxide insufflation. Dig Surg. 2004;21(2):95–105. doi: 10.1159/000077038. [DOI] [PubMed] [Google Scholar]
- 16.Ivankovich AD, Albrecht RF, Zahed B, Bonnet RF. Cardiovascular collapse during gynecological laparoscopy. IMJ Ill Med J. 1974;145(1):58–61 passim. [PubMed] [Google Scholar]
- 17.Motew M, Ivankovich AD, Bieniarz J, Albrecht RF, Zahed B, Scommegna A. Cardiovascular effects and acid-base and blood gas changes during laparoscopy. Am J Obstet Gynecol. 1973;115(7):1002–12. doi: 10.1016/0002-9378(73)90683-2. [DOI] [PubMed] [Google Scholar]
- 18.Yavuz Y, Rønning K, Lyng O, Mårvik R, Grønbech JE. Effect of increased intraabdominal pressure on cardiac output and tissue blood flow assessed by color-labeled microspheres in the pig. Surg Endosc. 2001;15(2):149–155. doi: 10.1007/s004640000336. [DOI] [PubMed] [Google Scholar]
- 19.Ho HS, Saunders CJ, Gunther RA, Wolfe BM. Effector of hemodynamics during laparoscopy: CO2 absorption or intra-abdominal pressure? J Surg Res. 1995;59(4):497–503. doi: 10.1006/jsre.1995.1198. [DOI] [PubMed] [Google Scholar]
- 20.Chiu AW, Chang LS, Birkett DH, Babayan RK. The impact of pneumoperitoneum, pneumoretroperitoneum, and gasless laparoscopy on the systemic and renal hemodynamics. J Am Coll Surg. 1995;181(5):397–406. [PubMed] [Google Scholar]
- 21.Chiu AW, Azadzoi KM, Hatzichristou DG, Siroky MB, Krane RJ, Babayan RK. Effects of intra-abdominal pressure on renal tissue perfusion during laparoscopy. J Endourol. 1994;8(2):99–103. doi: 10.1089/end.1994.8.99. [DOI] [PubMed] [Google Scholar]
- 22.Hamilton BD, Chow GK, Inman SR, Stowe NT, Winfield HN. Increased intra-abdominal pressure during pneumoperitoneum stimulates endothelin release in a canine model. J Endourol. 1998;12(2):193–7. doi: 10.1089/end.1998.12.193. [DOI] [PubMed] [Google Scholar]
- 23.Blobner M, Bogdanski R, Kochs E, Henke J, Findeis A, Jelen-Esselborn S. Effects of Intraabdominanlly Insufflated Carbon Dioxide and Elevated Intraabdominal Pressure on Splanchnic Circulation: An Experimental Study in Pigs. Anesthesiology. 1998;89(2):475–82. doi: 10.1097/00000542-199808000-00025. [DOI] [PubMed] [Google Scholar]