Abstract
Background:
Fatigue is a frequent and persistent problem among Hodgkin lymphoma (HL) survivors. We investigated the prevalence of clinically relevant fatigue in HL survivors and the relation between fatigue and anxiety and depression.
Methods:
Fatigue was measured through the generic European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (QLQ-C30) and Fatigue Assessment Scale (FAS). Anxiety and depression were measured with the Hospital Anxiety and Depression Scale. Questionnaires were mailed to 267 HL survivors. Results were compared with a Dutch age-matched normative population.
Results:
Response rate was 68% (median age 46 years, mean time since diagnosis 4.6 years). Prevalence of fatigue was significantly higher among HL survivors than in the norm population (FAS 41% vs 23%, QLQ-C30 43% vs 28%), as were fatigue levels. There was a significant association between fatigue, anxiety and depression. Of the HL survivors with high symptom levels of depression, 97% also reported fatigue. In multivariate analysis, depression was strongly associated with high levels of fatigue and, to a lesser extent, anxiety and comorbidity.
Conclusions:
Prevalence rates of fatigue are significantly higher in HL survivors than in the general population and differences are clinically relevant. Depression and anxiety were strongly associated with high levels of fatigue. Reducing fatigue levels by treatment of depression and anxiety should be further explored.
Keywords: Hodgkin lymphoma, cancer survivors, population based, quality of life, fatigue, anxiety, depression
Over the past decades, survival of Hodgkin lymphoma (HL) patients has improved dramatically with 5-year overall survival rates ranging from 90 to 95% (Engert et al, 2010, 2012). This has mainly been due to the introduction of multi-agent chemotherapy and improved radiotherapy techniques. However, with improved life expectancy, patients often face long-term effects caused by their treatment, such as treatment-induced secondary tumours or cardiovascular disease (van Leeuwen et al, 2000; Aleman et al, 2003; De Bruin et al, 2009; van den Belt-Dusebout et al, 2009).
Apart from these adverse physical effects, many HL survivors also report suffering from long-term psychosomatic and psychosocial problems (Loge et al, 1997, 2000; Hjermstad et al, 2005; Mols et al, 2006). A number of studies have focused on these psychosocial issues in HL survivors, mainly addressing overall health-related quality of life (HRQoL). A recent review of HRQoL in HL survivors showed persistent problems in physical, role physical, social and cognitive functioning (Oerlemans et al, 2011). These problems were most prevalent in HL patients treated with combined modality treatment, in women and in patients of older age. Furthermore, a number of studies have focused specifically on fatigue, because this is one of the most frequently reported and most persisting symptoms in HL survivors, and has consistently been reported to have significant impact on HR-QoL (Fobair et al, 1986; Joly et al, 1996; Flechtner et al, 1998; Loge et al, 1999; Ruffer et al, 2003; Hjermstad et al, 2005). The mechanism that causes fatigue is largely unknown. Associations between fatigue and clinical or patient characteristics have been made, mainly focusing on the influence of treatment, time since diagnosis and age. However, such studies have provided conflicting results (Loge et al, 1999; Ruffer et al, 2003; Hjermstad et al, 2005; Ng et al, 2005; Heutte et al, 2009). The impact of comorbid conditions, whether or not caused by cancer treatment, on perceived fatigue has been studied less frequently. All conducted studies reported increased fatigue in HL survivors with comorbidities (Knobel et al, 2001; Ng et al, 2005; Miltenyi et al, 2010). Of these studies, only Ng et al (2005) compared their results with a norm population consisting of a group of siblings. Fatigue in the HL survivors was more frequent and was associated with the presence of cardiac disease.
Fatigue is reported to be a frequent symptom of depression. Few studies have explored the relationship between fatigue and depression in HL survivors. Loge et al (2000) reported increased levels of psychological distress in nearly 50% of fatigued HL survivors; however, no comparison with a norm population was made. Ng et al (2005) found that having a psychiatric condition was a significant variable for increased fatigue. Because of high prevalence rates of fatigue in the general population, results on fatigue surveys of cancer survivors should be interpreted with caution and be compared with an age- and sex-matched norm population.
The purpose of this study was to investigate the prevalence of clinically relevant fatigue in HL survivors in The Netherlands compared with an age- and sex-matched Dutch population, and to determine the relationship between fatigue and depression, and other comorbid conditions.
Materials and Methods
HL survivors
A cross-sectional survey was conducted at the Eindhoven Cancer Registry (ECR) among HL survivors. The ECR records data on all newly diagnosed cancers in the southern part of the Netherlands, an area with 2.3 million inhabitants, 18 hospital locations and 2 large radiotherapy institutes. The ECR was used to select all patients who were diagnosed with HL between 1 January 1999 and 1 December 2010. Deceased patients were excluded by linking the ECR database with the Central Bureau for Genealogy. Hodgkin lymphoma survivors were contacted by mail through their physicians and were asked to participate in this cross-sectional study by completing and returning a set of questionnaires. In May 2009, patients between 6 months and 10 years after diagnosis received the first questionnaire. In November 2009, patients diagnosed between May 2008 and May 2009 were invited to participate, and in May 2011, patients diagnosed between May 2009 and December 2010 were invited. Ethical approval for this study was obtained from the University of Tilburg-certified Medical Ethics Committee.
Questionnaires
Survivors of HL were asked to complete the validated Dutch version of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30). The QLQ-C30 measures cancer-specific HRQoL and contains five functional scales (physical, cognitive, emotional, social and role functioning), a global health status/QoL scale, six single items assessing additional symptoms and three symptom scales (pain, fatigue and nausea/vomiting). For all items, Likert-type response scales are used, with total scores per item ranging from 4 to 7 points. All subscales and individual item responses are linearly converted to 0–100 scales (Aaronson et al, 1993). As a cut-off value for fatigue caseness, we defined a score >23.9 for the EORTC QLQ-C30 (Cocks et al, 2011), although the fatigue symptom subscale has not been validated as a stand-alone measure for fatigue. For partially incomplete questionnaires, imputation of the mean was used for scales containing at least 50% of the scores (http://groups.eortc.be/qol/).
Fatigue was also measured with the Fatigue Assessment Scale (FAS), a validated 10-item questionnaire reflecting mental and physical fatigue (Michielsen et al, 2003, 2005). Total scores range from 10 to 50, with a higher score reflecting a higher level of fatigue. A score over 21 points indicates probable caseness of fatigue (Michielsen et al, 2003).
Anxiety and depression were measured using the Hospital Anxiety and Depression Scale (HADS; Zigmond and Snaith, 1983; Snaith and Zigmond, 1986), which measures levels of symptoms of anxiety and depression in two subscales of seven items each. A score >8 on either subscale indicates a possible caseness for an anxiety or depressive disorder; a score >11 indicates a probable caseness. For HADS, a score >8 on either subscale was used as a cut-off value for defining caseness of anxiety or depression, as this score achieves an optimal balance between sensitivity and specificity (Zigmond and Snaith, 1983; Snaith and Zigmond, 1986; Bjelland et al, 2002).
Comorbidity was evaluated by the Self-administered Comorbidity Questionnaire (Sangha et al, 2003). Education and marital status were also recorded in the questionnaire. Information on tumour and treatment characteristics was available from the ECR.
Norm population
The norm population was selected from a reference cohort of ∼2200 individuals from the general Dutch population (CentER panel; van de Poll-Franse et al, 2011b). The set of questionnaires completed for this study included the QLQ-C30, FAS and HADS questionnaires, and also data on socio-demographics and comorbid conditions were provided. To compare the results with that of the HL survivor cohort, we made an age- and sex-matched selection from this normative population. This reference cohort is representative for the Dutch-speaking population in the Netherlands (van de Poll-Franse LV et al, 2011a, 2011b).
Statistical analysis
All statistical analyses were performed using SPSS version 20 (SPSS Inc., Chicago, IL, USA). Patient, tumour and treatment characteristics between respondents, non-respondents and patients with unverifiable addresses were compared using t-test (numerical variables) and χ2-test (categorical variables). A two-sided P-value<0.05 was considered statistically significant.
Differences between fatigue caseness from the EORTC QLQ-C30 and FAS, and/or caseness of anxiety or depression from the HADS in HL survivors and the norm population, were calculated by χ2-tests.
Mean fatigue scores from the EORTC QLQ-C30 and FAS were compared between HL survivors and the norm population using independent sample t-tests. Clinical relevance of the differences was defined according to guidelines for the interpretation of the EORTC QLQ-C30 (Cocks et al, 2011) and according to Norman's rule of thumb for the FAS, indicating a ±0.5 s.d. difference of the norm in scores as a discriminating change (Norman et al, 2003).
Multivariate logistic regression analyses using the dichotomous FAS score were performed to analyse the association of socio-demographic, tumour, treatment and comorbidity variables and fatigue. Variables were included into the model in separate steps. Demographic variables were added first, then clinical variables and, third, psychological distress. A two-sided P-value<0.05 was considered statistically significant.
Results
Characteristics of the respondents and non-respondents
In total, 180 (68%) of the 267 HL survivors completed and returned the questionnaires. Missing items on the completed questionnaires were <3% (n=17). Responders were more often male and older than non-responders and those with unverifiable addresses (Table 1). Mean time since diagnosis was 4.6 years, mean age at the time of survey among HL responders was 46 years and 55% had received combined modality treatment. Only 3% had been treated with radiotherapy alone. There were no statistically significant differences between HL responders and the norm population concerning marital status or education (Table 2). With regards to comorbidities, HL responders less often reported hypertension (9% vs 20%) but more often thyroid disease (9% vs 5%) and depression (11% vs 3%) than the norm population.
Table 1. Patient and treatment characteristics of the HL survivor cohort.
|
HL responders |
Non-responders |
Unverifiable address |
|
||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | P-value | |
|
Total |
180 |
|
35 |
|
52 |
|
|
|
Mean age at time of survey in years (s.d.) |
46 (15.6) |
|
40 (13.6) |
|
40 (13.9) |
|
0.01 |
| Range | 19–84 | 21–79 | 20–83 | ||||
| <40 | 75 | 41 | 18 | 51 | 34 | 65 | 0.02 |
| 40–60 | 70 | 39 | 14 | 40 | 14 | 27 | |
| >60 |
35 |
19 |
3 |
9 |
4 |
8 |
|
|
Mean time since diagnosis in years (s.d.) |
4.6 (2.9) |
|
5.9 (3.2) |
|
4.6 (3.0) |
|
0.07 |
| <5 | 102 | 57 | 14 | 40 | 29 | 56 | 0.11 |
| 5–10 | 76 | 42 | 19 | 54 | 23 | 44 | |
| >10 |
2 |
1 |
2 |
6 |
0 |
|
|
|
Sex |
|
|
|
|
|
|
0.06 |
| Male | 99 | 55 | 23 | 66 | 37 | 72 | |
| Female |
81 |
45 |
12 |
34 |
14 |
28 |
|
|
Stage at diagnosis |
|
|
|
|
|
|
0.60 |
| I | 31 | 17 | 7 | 20 | 9 | 17 | |
| II | 94 | 52 | 14 | 40 | 19 | 37 | |
| III | 26 | 15 | 6 | 17 | 12 | 23 | |
| IV |
18 |
10 |
4 |
12 |
6 |
12 |
|
|
Treatment |
|
|
|
|
|
|
0.50 |
| RT | 6 | 3 | 0 | 1 | 2 | ||
| CT | 74 | 41 | 18 | 51 | 25 | 48 | |
| RT+CT | 99 | 55 | 16 | 46 | 23 | 44 | |
Abbreviations: CT=chemotherapy only; HL=Hodgkin lymphoma; RT=radiotherapy only; RT+CT=radiotherapy and chemotherapy.
Table 2. Characteristics of the study participants.
|
HL responders |
Norm population |
|
|||
|---|---|---|---|---|---|
| N | % | N | % | P-value | |
|
Total |
180 |
|
327 |
|
|
|
Mean age at survey in years (s.d.) |
46.1 (15.6) |
|
48.8 (15.7) |
|
0.90 |
| Range | 19–84 | 20–85 | |||
| <40 | 75 | 42 | 117 | 36 | 0.28 |
| 40–60 | 70 | 39 | 129 | 39 | |
| >60 |
35 |
19 |
81 |
25 |
|
|
Sex |
|
|
|
|
0.43 |
| Male | 99 | 55 | 168 | 51 | |
| Female |
81 |
45 |
159 |
49 |
|
|
Self-reported comorbidity | |||||
| Cardiac | 17 | 9.4 | 21 | 6.4 | 0.07 |
| Stroke | 2 | 1.1 | 1 | 0.3 | 0.16 |
| Hypertension | 16 | 8.9 | 65 | 19.9 | 0.01 |
| COPD | 19 | 10.6 | 41 | 12.5 | 0.92 |
| Diabetes mellitus | 8 | 4.4 | 25 | 7.6 | 0.39 |
| Anaemia | 4 | 2.2 | 14 | 4.3 | 0.44 |
| Thyroid disease | 17 | 9.4 | 16 | 4.9 | 0.008 |
| Depression |
19 |
10.6 |
11 |
3.4 |
<0.001 |
|
Comorbidity conditions |
|
|
|
|
0.37 |
| No comorbidity | 87 | 48 | 149 | 46 | |
| ⩽2 Comorbidities | 63 | 35 | 134 | 41 | |
| >2 Comorbidities |
21 |
12 |
44 |
13 |
|
|
Marital status |
|
|
|
|
0.62 |
| Partner | 133 | 74 | 252 | 77 | |
| No partner |
44 |
24 |
75 |
23 |
|
|
Education level |
|
|
|
|
0.10 |
| Low | 14 | 8 | 13 | 4 | |
| Medium | 107 | 59 | 191 | 58 | |
| High | 56 | 31 | 122 | 37 | |
Abbreviations: COPD=chronic obstructive pulmonary disease; HL=Hodgkin lymphoma.
Fatigue prevalence and symptoms of anxiety and depression
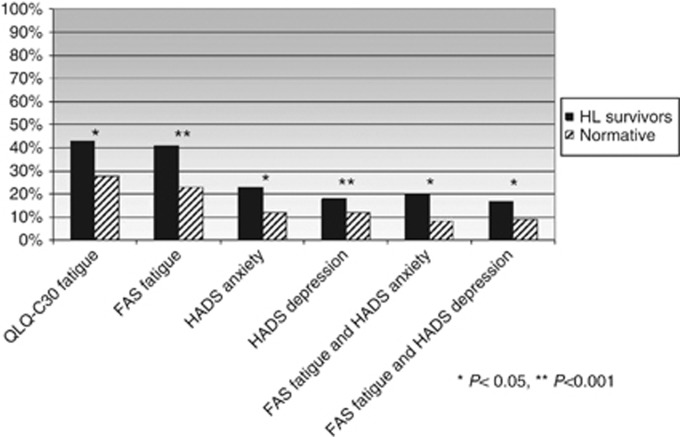
There were significantly more persons with fatigue among the HL survivors compared with the norm population (Figure 1 and Table 3). The QLQ-C30 fatigue subscale identified a 43% prevalence of fatigue among the HL survivors vs 28% in the norm population (P=0.002). The FAS questionnaire showed fatigue prevalence rates of 41% and of 23%, respectively (P<0.001). Identification of fatigue cases was consistent between the QLQ-C30 and the FAS questionnaire in 83% of the HL survivors and in 81% of the norm population. Among the HL patients, 23% had high symptom levels of anxiety and 18% of depression, compared with 13% and 12% in the norm population, respectively.
Figure 1.
Prevalence of caseness of fatigue. Prevalence of caseness of fatigue according to fatigue subscale of the EORTC QlQ-C30 and FAS, and caseness of anxiety or depression according to the HADS scale for both HL survivors and the age-matched Dutch population. The two last columns describe the prevalence of combined fatigue and anxiety or depression among all HL survivors and of the norm population. *P<0.05; **P<0.001.
Table 3. QLQ-C30, FAS and HADS mean scores for HL survivors vs norm population.
|
HL |
Norm |
|
||||
|---|---|---|---|---|---|---|
| Mean | s.d. | Mean | s.d. | P-value | Clinical relevance (Norman et al, 2003; Cocks et al, 2011) | |
|
QLQ-C30 | ||||||
|
Functional scales | ||||||
| Role functioning | 83.8 | 24.4 | 89.6 | 20.0 | 0.05 | Trivial |
| Physical functioning | 87.1 | 15.7 | 90.9 | 14.8 | 0.08 | Trivial |
| Cognitive functioning | 82.5 | 22.0 | 92.5 | 15.7 | <0.001 | Medium |
| Emotional functioning | 82.4 | 22.9 | 87.9 | 17.8 | 0.03 | Small |
| Social functioning |
86.4 |
22.2 |
92.8 |
17.6 |
<0.001 |
Small |
|
Symptom scales | ||||||
| Fatigue | 28.7 | 26.4 | 18.9 | 20.4 | <0.001 | Small |
| Pain | 13.0 | 22.4 | 14.2 | 20.9 | =0.54 | Trivial |
| Nausea/vomiting | 3.3 | 9.2 | 2.6 | 9.9 | =0.45 | Trivial |
| Global Health Status |
76.8 |
18.5 |
77.7 |
16.9 |
=0.57 |
Trivial |
|
FAS | ||||||
| Total fatigue score |
21.4 |
7.6 |
18.4 |
5.8 |
<0.001 |
Yes |
|
HADS | ||||||
| Anxiety mean scores | 4.7 | 4.2 | 3.8 | 4.3 | <0.001 | No |
| Anxiety mean score in fatigue cases | 7.6 | 4.5 | 6.5 | 4.0 | 0.31 | No |
| Depression mean scores | 3.7 | 3.8 | 3.4 | 3.2 | 0.02 | No |
| Depression mean score in fatigue cases | 6.6 | 4.1 | 6.4 | 4.0 | 0.83 | No |
Abbreviations: EORTC QLQ-C30=European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire Core-30; FAS=Fatigue Assessment Scale; HADS=Hospital Anxiety and Depression Scale; HL=Hodgkin's lymphoma.
Of all responding HL survivors, 20% were identified both as a fatigue case and an anxiety case; 17% were both fatigued and had symptoms of depression. These numbers were significantly lower in the norm population (8%, P<0.001, and 9%, P=0.004, respectively; Figure 1). The prevalence of fatigue among HL survivors with a high symptom level of depression was 97% compared with 76% in the norm population.
Similar relationships were found for cognitive functioning (impairment of concentration and memory) and fatigue, with significantly lower social functioning and especially lower cognitive functioning among HL survivors compared with the norm population (Table 3). There was a clear association between fatigue and cognitive impairment. The mean scores of cognitive function were lower among fatigued HL survivors and fatigued participants of the norm population (74.5 and 86.4 points, respectively) than in the non-fatigued participants (HL survivors 95.7 and norm population 98 points). Differences are clinically relevant in both groups, and reflect a large difference in the HL survivors group and a medium difference in the norm population.
Clinical relevance of fatigue scores
Fatigue scores were significantly higher among HL survivors than in the norm population, and these differences were clinically relevant (Table 3). Mean QLQ-C30 fatigue scores differed 9.8 points (28.7 vs 18.9), reflecting a small but clinically relevant difference. The FAS total fatigue scores were 21.4 vs 18.4 points (>0.5 s.d.), which also reflects a clinically relevant (albeit small) difference.
Association of fatigue with patient and treatment factors and comorbid conditions
Multivariate regression analysis using the FAS scores showed that a lower level of education was associated with a higher risk of fatigue (Table 4). After adding clinical variables to the regression analysis, the significance of level of education disappeared, and having one to two comorbid conditions (OR 4.7) or >2 comorbid conditions (OR 17.5) were significantly associated with fatigue.
Table 4. Logistic model of factors associated with fatigue using the FAS TOTAL score.
| |
Model: block 1 |
Model: block 1+2 |
Model: block 1+2+3 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value |
|
Block 1: Demographic variables | |||||||||
| Age | 0.99 | 0.97–1.02 | 0.64 | 0.97 | 0.95–1.01 | 0.09 | 0.97 | 0.94–1.02 | 0.19 |
| Male vs female | 1.42 | 0.74–2.73 | 0.29 | 1.33 | 0.64–2.76 | 0.43 | 2.1 | 0.79–5.70 | 0.13 |
| Education: low vs mid | 0.22 | 0.05–0.92 | 0.038 | 0.27 | 0.05–1.37 | 0.11 | 0.78 | 0.06–8.93 | 0.84 |
| Low vs high | 0.14 | 0.03–0.65 | 0.12 | 0.29 | 0.05–1.65 | 0.16 | 1.38 | 0.10–18.72 | 0.80 |
| Partner |
0.51 |
0.24–1.08 |
0.08 |
0.54 |
0.24–1.25 |
0.15 |
0.41 |
0.13–1.24 |
0.12 |
|
Block 2: Clinical variables | |||||||||
| Time since diagnosis | 0.97 | 0.86–1.11 | 0.73 | 0.96 | 0.81–1.15 | 0.70 | |||
| No comorbidity vs 1–2 | 4.73 | 2.10–10.64 | <0.001 | 2.76 | 0.93–8.12 | 0.06 | |||
| No comorbidity vs >2 | 17.49 | 4.27–71.51 | <0.001 | 4.25 | 0.68–26.39 | 0.12 | |||
| Treatment: CT vs RT | 0.69 | 0.77–6.09 | 0.73 | 1.22 | 0.09–16.03 | 0.88 | |||
| Treatment: CT vs CMT |
|
|
|
0.85 |
0.41–1.77 |
0.68 |
1.09 |
0.41–2.93 |
0.86 |
|
Block 3: Psychological variables | |||||||||
| HADS anxiety | 1.19 | 1.00–1.41 | 0.46 | ||||||
| HADS depression | 1.80 | 1.37–2.37 | <0.001 | ||||||
Abbreviations: CI=confidence interval; CMT=combined modality treatment; CT=chemotherapy; FAS=Fatigue Assessment Scale; HADS=Hospital Anxiety and Depression Scale; OR=odds ratio; RT=radiotherapy. Bold entries are the values from regression analysis reflecting statistically significant values.
After adding psychological distress symptoms, however, the influence of comorbidities lacked statistical significance. Symptoms of depression (OR 1.8) and anxiety (OR 1.2) were the only factors significantly associated with high levels of fatigue.
Logistic regression analysis of the QLQ-C30 fatigue data did not differ from the FAS data (data not shown). Using the QLQ-C30 having one to two comorbidities (OR, 3.0; 95% CI, 1.3–7.3; P=0.02) and symptoms of depression (OR, 1.2; 95% CI, 1.1–1.4; P=0.04) were the only variables associated with fatigue.
Discussion
In this cross-sectional study, we found a higher prevalence rate of fatigue in HL survivors compared with an age- and sex-matched Dutch normative population of 15% and 18% using two different validated fatigue measures (QLQ-C30 fatigue and FAS, respectively). We also observed a significant association between fatigue caseness and high levels of depression and anxiety, especially in the HL cohort. Mean fatigue levels were significantly increased in the HL survivors compared with the norm population, and differences were also found to be clinically relevant. Symptoms of depression, and (to a lesser extent) anxiety and comorbidities, were found to be the only variables associated with long-lasting fatigue.
One of the strengths of our study is that we measured fatigue through both a generic (QLQ-C30) and a fatigue-specific (FAS) questionnaire. Both questionnaires independently measured a significantly higher prevalence of fatigue in the HL survivors. We showed that the identification of fatigue cases between both questionnaires was consistent in 83% of the HL survivors and 81% of the norm population. Our data are robust, as missing items were <3%.
Our study not only shows that HL survivors more often suffer from chronic fatigue but also clearly shows an association between fatigue and depression or anxiety. We showed that a combination of both fatigue and anxiety occurred in 20% of all HL survivors and of fatigue and depression in 17%, compared with 8% and 9%, respectively, in the norm population. This significant association between fatigue and anxiety and depression has also been described by Loge et al (2000). They reported high HADS scores (anxiety and depression combined) in 52% of 109 fatigued HL survivors. Their results, however, were not compared with a control group or with a norm population. Our study further showed that almost all (97%) HL survivors with symptoms of depression were also fatigued. As both studies were cross-sectional by design, it is difficult to evaluate whether fatigue and anxiety or depression are two separate entities both occurring more often in HL survivors, or whether fatigue is a consequence of these psychological conditions. The lower level of cognitive functioning that we observed among the HL survivors, reflected in symptoms such as loss of concentration, might be explained as a manifestation of the impact of fatigue and/or psychological distress. In our multivariate analysis, we showed that depression and, to a lesser extent, anxiety were significantly associated with fatigue. However, due to the design of our study, a causal relation between fatigue, anxiety and depression cannot be established.
In daily practice, fatigue in HL survivors has proven to be a prominent problem. Many survivors report to suffer from chronic fatigue, with often significant impact on daily activities, which has proven extremely difficult to treat. Studies evaluating interventions aimed at improvement of fatigue in cancer survivors have often shown improvement in physical endurance, but limited improvement in the subjective feeling of fatigue and lack of energy (De Backer et al, 2008). Two recent meta-analyses concluded that exercise interventions in fatigued cancer patients had a near-moderate effect size in reducing fatigue at best (Kangas et al, 2008; Cramp and Byron-Daniel, 2012). Increased awareness of fatigue and of depression and anxiety among treating physicians is essential. However, fatigue is more common and need not be a symptom of depression or anxiety. Differentiating between these symptoms can be challenging in the clinical setting. A possible aid in defining depression could be to shift the focus from fatigue to other dimensions of depression. Symptoms of depression and anxiety could be amenable to treatment. Psychosocial therapies such as cognitive behavioural therapy or educational counselling have proven to be beneficial in reducing symptoms of anxiety and depression (Kangas et al, 2008).
It might be beneficial for both patients suffering from fatigue and for patients with depression or anxiety to receive treatment by professionals, although through different methods of focused psychosocial support or specific coping strategies, which might result in a clinically meaningful reduction of fatigue. This approach, however, should be explored in future studies. Ideally, HL survivors suffering from chronic fatigue should be invited for a diagnostic interview to distinguish between fatigue and depression, and then randomly assigned to specific psychosocial therapies. As HL survivors are at risk for a variety of comorbid conditions due to late treatment sequelae, such as cardiovascular diseases (Aleman et al, 2003; van den Belt-Dusebout et al, 2007), which could predispose for higher levels of fatigue, we examined the possible association of fatigue and comorbid conditions. Hodgkin lymphoma survivors self-reported depression more frequently than the norm population. Our multivariate analysis showed a trend for the association between self-reported comorbidities and fatigue. However, mean time since diagnosis and treatment in this survey was still relatively short (mean 4.6 years, range 6–122 months), which means that the majority of the cohort is not yet at risk for late treatment sequelae. Moreover, with a mean age of 46 years, a large part of both the cohort and the norm population would not yet suffer from serious comorbidities.
Rates of fatigue in HL survivors in this study (43% by using QLQ-C30 and 41% by using FAS) are slightly higher than the rates reported by others (Loge et al, 1999; Knobel et al, 2001; Hjermstad et al, 2005). These three studies reported fatigue rates of 26–30% in HL survivors, but all used the same HL cohort. More recent data on cancer-related fatigue in patients with other types of cancer using the EORTC QLQ-C30 and Multidimensional Fatigue Inventory showed prevalence rates of 36–48%, which are comparable to our results (Cella et al, 2001; Kuhnt et al, 2009; Schultz et al, 2011; Berger et al, 2012).
In conclusion, our results show a clinically relevant higher prevalence rate of fatigue in HL survivors when compared with an age- and sex-matched population. We also found a significant association between fatigue and anxiety or depression. The only factors significantly associated with high levels of fatigue were symptoms of depression and anxiety. This might have implications for the diagnosis and treatment of fatigue in the clinical setting, as psychosocial therapies have proven to be effective in reducing anxiety and depression, and could therefore be beneficial in reducing levels of fatigue as well. This should be further examined in future trials.
Acknowledgments
We thank all patients for their participation in the study. We are grateful for the support of colleagues in the following hospitals for their support of this study: Catharina-Hospital, Eindhoven; Jeroen Bosch Hospital, ‘s Hertogenbosch; Maxima Medical Centre, Eindhoven and Veldhoven; Saint Anna Hospital, Geldrop; St Elisabeth Hospital, Tilburg; Twee Steden Hospital, Tilburg; VieCurie Hospital, Venlo and Venray and Hospital Bernhoven, Oss. This study was partly supported by the charitable Jonker-Driessen Foundation and The Netherlands organisation for health research and development (Zon-MW), and through PHAROS: Populationbased HAematological Registry for Observational Studies (80-82500-98-01007). Dr Lonneke van de Poll-Franse is supported by a Cancer Research Award from the Dutch Cancer Society (UVT-2009-4349).
The authors declare no conflict of interest.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
References
- Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85 (5:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- Aleman BM, van den Belt-Dusebout AW, Klokman WJ, Van't Veer MB, Bartelink H, van Leeuwen FE. Long-term cause-specific mortality of patients treated for Hodgkin's disease. J Clin Oncol. 2003;21 (18:3431–3439. doi: 10.1200/JCO.2003.07.131. [DOI] [PubMed] [Google Scholar]
- Berger AM, Gerber LH, Mayer DK. Cancer-related fatigue: implications for breast cancer survivors. Cancer. 2012;118 (8 Suppl:2261–2269. doi: 10.1002/cncr.27475. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52 (2:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Cella D, Davis K, Breitbart W, Curt G. Cancer-related fatigue: prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. J Clin Oncol. 2001;19 (14:3385–3391. doi: 10.1200/JCO.2001.19.14.3385. [DOI] [PubMed] [Google Scholar]
- Cocks K, King MT, Velikova G, Martyn St-James M, Fayers PM, Brown JM. Evidence-based guidelines for determination of sample size and interpretation of the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. J Clin Oncol. 2011;29 (1:89–96. doi: 10.1200/JCO.2010.28.0107. [DOI] [PubMed] [Google Scholar]
- Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11:CD006145. doi: 10.1002/14651858.CD006145.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Backer IC, Vreugdenhil G, Nijziel MR, Kester AD, van BE, Schep G. Long-term follow-up after cancer rehabilitation using high-intensity resistance training: persistent improvement of physical performance and quality of life. Br J Cancer. 2008;99 (1:30–36. doi: 10.1038/sj.bjc.6604433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bruin ML, Sparidans J, Van't Veer MB, Noordijk EM, Louwman MW, Zijlstra JM, van den Berg H, Russell NS, Broeks A, Baaijens MH, Aleman BM, van Leeuwen FE. Breast cancer risk in female survivors of Hodgkin's lymphoma: lower risk after smaller radiation volumes. J Clin Oncol. 2009;27 (26:4239–4246. doi: 10.1200/JCO.2008.19.9174. [DOI] [PubMed] [Google Scholar]
- Engert A, Haverkamp H, Kobe C, Markova J, Renner C, Ho A, Zijlstra J, Kral Z, Fuchs M, Hallek M, Kanz L, Dohner H, Dorken B, Engel N, Topp M, Klutmann S, Amthauer H, Bockisch A, Kluge R, Kratochwil C, Schober O, Greil R, Andreesen R, Kneba M, Pfreundschuh M, Stein H, Eich HT, Muller RP, Dietlein M, Borchmann P, Diehl V. Reduced-intensity chemotherapy and PET-guided radiotherapy in patients with advanced stage Hodgkin's lymphoma (HD15 trial): a randomised, open-label, phase 3 non-inferiority trial. Lancet. 2012;379 (9828:1791–1799. doi: 10.1016/S0140-6736(11)61940-5. [DOI] [PubMed] [Google Scholar]
- Engert A, Plutschow A, Eich HT, Lohri A, Dorken B, Borchmann P, Berger B, Greil R, Willborn KC, Wilhelm M, Debus J, Eble MJ, Sokler M, Ho A, Rank A, Ganser A, Trumper L, Bokemeyer C, Kirchner H, Schubert J, Kral Z, Fuchs M, Muller-Hermelink HK, Muller RP, Diehl V. Reduced treatment intensity in patients with early-stage Hodgkin's lymphoma. N Engl J Med. 2010;363 (7:640–652. doi: 10.1056/NEJMoa1000067. [DOI] [PubMed] [Google Scholar]
- Flechtner H, Ruffer JU, Henry-Amar M, Mellink WA, Sieber M, Ferme C, Eghbali H, Josting A, Diehl V. Quality of life assessment in Hodgkin's disease: a new comprehensive approach. First experiences from the EORTC/GELA and GHSG trials. EORTC Lymphoma Cooperative Group. Groupe D'Etude des Lymphomes de L'Adulte and German Hodgkin Study Group. Ann Oncol. 1998;9 (Suppl 5:S147–S154. doi: 10.1093/annonc/9.suppl_5.s147. [DOI] [PubMed] [Google Scholar]
- Fobair P, Hoppe RT, Bloom J, Cox R, Varghese A, Spiegel D. Psychosocial problems among survivors of Hodgkin's disease. J Clin Oncol. 1986;4 (5:805–814. doi: 10.1200/JCO.1986.4.5.805. [DOI] [PubMed] [Google Scholar]
- Heutte N, Flechtner HH, Mounier N, Mellink WAM, Meerwaldt JH, Eghbali H, Van't Veer MB, Noordijk EM, Kluin-Nelemans JC, Lampka E, Thomas J, Lugtenburg PJ, Viterbo L, Carde P, Hagenbeek A, van der Maazen RWM, Smit WGJM, Brice P, Kooy MV, Baars JW, Poortmans P, Tirelli U, Leeksma OC, Tomsic R, Feugier P, Salles G, Gabarre J, Kersten MJ, Van Den Neste E, Creemers GJM, Gaillard I, Meijnders P, Tertian G, Reman O, Muller HP, Troncy J, Blanc M, Schroyens W, Voogt PJ, Wijermans P, Rieux C, Ferme C, Henry-Amar M. Quality of life after successful treatment of early-stage Hodgkin's lymphoma: 10-year follow-up of the EORTC-GELA H8 randomised controlled trial. Lancet Oncol. 2009;10 (12:1160–1170. doi: 10.1016/S1470-2045(09)70258-X. [DOI] [PubMed] [Google Scholar]
- Hjermstad MJ, Fossa SD, Oldervoll L, Holte H, Jacobsen AB, Loge JH. Fatigue in long-term Hodgkin's disease survivors: A follow-up study. J Clin Oncol. 2005;23 (27:6587–6595. doi: 10.1200/JCO.2005.09.936. [DOI] [PubMed] [Google Scholar]
- Joly F, HenryAmar M, Arveux P, Reman O, Tanguy A, Peny AM, Lebailly P, MaceLesech J, Vie B, Genot JY, Busson A, Troussard X, Leporrier M. Late psychosocial sequelae in Hodgkin's disease survivors: A French population-based case-control study. J Clin Oncol. 1996;14 (9:2444–2453. doi: 10.1200/JCO.1996.14.9.2444. [DOI] [PubMed] [Google Scholar]
- Kangas M, Bovbjerg DH, Montgomery GH. Cancer-related fatigue: a systematic and meta-analytic review of non-pharmacological therapies for cancer patients. Psychol Bull. 2008;134 (5:700–741. doi: 10.1037/a0012825. [DOI] [PubMed] [Google Scholar]
- Knobel H, Loge JH, Lund MB, Forfang K, Nome O, Kaasa S. Late medical complications disease and fatigue in Hodgkin's disease survivors. J Clin Oncol. 2001;19 (13:3226–3233. doi: 10.1200/JCO.2001.19.13.3226. [DOI] [PubMed] [Google Scholar]
- Kuhnt S, Ernst J, Singer S, Ruffer JU, Kortmann RD, Stolzenburg JU, Schwarz R. Fatigue in cancer survivors—prevalence and correlates. Onkologie. 2009;32 (6:312–317. doi: 10.1159/000215943. [DOI] [PubMed] [Google Scholar]
- Loge JH, Abrahamsen AF, Ekeberg O, Hannisdal E, Kaasa S. Psychological distress after cancer cure: a survey of 459 Hodgkin's disease survivors. Br J Cancer. 1997;76 (6:791–796. doi: 10.1038/bjc.1997.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loge JH, Abrahamsen AF, Ekeberg O, Kaasa S. Hodgkin's disease survivors more fatigued than the general population. J Clin Oncol. 1999;17 (1:253–261. doi: 10.1200/JCO.1999.17.1.253. [DOI] [PubMed] [Google Scholar]
- Loge JH, Abrahamsen AF, Ekeberg O, Kaasa S. Fatigue and psychiatric morbidity among Hodgkin's disease survivors. J Pain Sympt Manag. 2000;19 (2:91–99. doi: 10.1016/s0885-3924(99)00148-7. [DOI] [PubMed] [Google Scholar]
- Michielsen HJ, De VJ, Drent M, Peros-Golubicic T. Psychometric qualities of the Fatigue Assessment Scale in Croatian sarcoidosis patients. Sarcoidosis Vasc Diffuse Lung Dis. 2005;22 (2:133–138. [PubMed] [Google Scholar]
- Michielsen HJ, De VJ, Van Heck GL. Psychometric qualities of a brief self-rated fatigue measure: the Fatigue Assessment Scale. J Psychosom Res. 2003;54 (4:345–352. doi: 10.1016/s0022-3999(02)00392-6. [DOI] [PubMed] [Google Scholar]
- Miltenyi Z, Magyari F, Simon Z, Illes A. Quality of life and fatigue in Hodgkin's lymphoma patients. Tumori. 2010;96 (4:594–600. doi: 10.1177/030089161009600413. [DOI] [PubMed] [Google Scholar]
- Mols F, AJJM Vingerhoets, Coebergh JW, Vreugdenhil G, Aaronson NK, Lybeert MLM, de Poll-Franse LVV. Better quality of life among 10-15 year survivors of Hodgkin's lymphoma compared to 5-9 year survivors: a population-based study. Eur J Cancer. 2006;42 (16:2794–2801. doi: 10.1016/j.ejca.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Ng AK, Li S, Recklitis C, Neuberg D, Chakrabarti S, Silver B, Diller L. A comparison between long-term survivors of Hodgkin's disease and their siblings on fatigue level and factors predicting for increased fatigue. Ann Oncol. 2005;16 (12:1949–1955. doi: 10.1093/annonc/mdi407. [DOI] [PubMed] [Google Scholar]
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41 (5:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- Oerlemans S, Mols F, Nijziel MR, Lybeert M, van de Poll-Franse L. The impact of treatment, socio-demographic and clinical characteristics on health-related quality of life among Hodgkin's and non-Hodgkin's lymphoma survivors: a systematic review. Ann Hematol. 2011;90 (9:993–1004. doi: 10.1007/s00277-011-1274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffer JU, Flechtner H, Tralls P, Josting A, Sieber M, Lathan B, Diehl V. Fatigue in long-term survivors of Hodgkin's lymphoma; a report from the German Hodgkin Lymphoma Study Group (GHSG) Eur J Cancer. 2003;39 (15:2179–2186. doi: 10.1016/s0959-8049(03)00545-8. [DOI] [PubMed] [Google Scholar]
- Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49 (2:156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- Schultz SL, Dalton SO, Christensen J, Carlsen K, Ross L, Johansen C. Factors correlated with fatigue in breast cancer survivors undergoing a rehabilitation course, Denmark, 2002-2005. Psychooncology. 2011;20 (4:352–360. doi: 10.1002/pon.1739. [DOI] [PubMed] [Google Scholar]
- Snaith RP, Zigmond AS. The hospital anxiety and depression scale. Br Med J (Clin Res Ed) 1986;292 (6516:344. doi: 10.1136/bmj.292.6516.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Poll-Franse LV, Horevoorts N, van EM, Denollet J, Roukema JA, Aaronson NK, Vingerhoets A, Coebergh JW, De VJ, Essink-Bot ML, Mols F. The patient reported outcomes following initial treatment and long term evaluation of survivorship registry: scope, rationale and design of an infrastructure for the study of physical and psychosocial outcomes in cancer survivorship cohorts. Eur J Cancer. 2011;47 (14:2188–2194. doi: 10.1016/j.ejca.2011.04.034. [DOI] [PubMed] [Google Scholar]
- van de Poll-Franse LV, Mols F, Gundy CM, Creutzberg CL, Nout RA, Verdonck-de Leeuw IM, Taphoorn MJ, Aaronson NK. Normative data for the EORTC QLQ-C30 and EORTC-sexuality items in the general Dutch population. Eur J Cancer. 2011;47 (5:667–675. doi: 10.1016/j.ejca.2010.11.004. [DOI] [PubMed] [Google Scholar]
- van den Belt-Dusebout AW, Aleman BM, Besseling G, De Bruin ML, Hauptmann M, Van't Veer MB, de WR, Ribot JG, Noordijk EM, Kerst JM, Gietema JA, van Leeuwen FE. Roles of radiation dose and chemotherapy in the etiology of stomach cancer as a second malignancy. Int J Radiat Oncol Biol Phys. 2009;75 (5:1420–1429. doi: 10.1016/j.ijrobp.2009.01.073. [DOI] [PubMed] [Google Scholar]
- van den Belt-Dusebout AW, de WR, Gietema JA, Horenblas S, Louwman MW, Ribot JG, Hoekstra HJ, Ouwens GM, Aleman BM, van Leeuwen FE. Treatment-specific risks of second malignancies and cardiovascular disease in 5-year survivors of testicular cancer. J Clin Oncol. 2007;25 (28:4370–4378. doi: 10.1200/JCO.2006.10.5296. [DOI] [PubMed] [Google Scholar]
- van Leeuwen FE, Klokman WJ, Veer MB, Hagenbeek A, Krol AD, Vetter UA, Schaapveld M, van HP, Burgers JM, Somers R, Aleman BM. Long-term risk of second malignancy in survivors of Hodgkin's disease treated during adolescence or young adulthood. J Clin Oncol. 2000;18 (3:487–497. doi: 10.1200/JCO.2000.18.3.487. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67 (6:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]