Abstract
Health disparities are preventable differences in the burden of disease or opportunities to achieve optimal health that are experienced by socially disadvantaged population groups. Reducing health disparities has been identified as an ethical imperative by the World Health Organization’s Commission on Social Determinants of Health and numerous other national and international bodies. Significant progress has been made over the past years in identifying vulnerable groups, and ‘distal’ factors including political, economic, social, and community characteristics are now considered pivotal. It is thus unsurprising that the remarkable advances in the science and practice of dentistry have not led to notable reductions in oral health disparities. In this review, we summarize recent work and emphasize the need for a solid theoretical framing to guide oral health disparities research. We provide a theoretical framework outlining pathways that operate across the continuum of oral health determinants during the lifecourse and highlight potential areas for intervention. Because oral health disparities emanate from the unequal distribution of social, political, economic, and environmental resources, tangible progress is likely to be realized only by a global movement and concerted efforts by all stakeholders, including policymakers, the civil society, and academic, professional, and scientific bodies.
Keywords: inequalities, social determinants of health, injustice, globalization, health policy, theoretical framework
Introduction
During the past 3 decades, the issue of health disparities has been receiving increasing attention in the public health and policy discourse. The landmark 2008 report of the World Health Organization’s (WHO) Commission on Social Determinants of Health (CSDH, 2008) articulated an emphatic call for action on addressing health disparities, emphasizing the pivotal role of the social determinants of health (Marmot et al., 2008). This was further reflected in “The Marmot report” for the UK in 2010 (Marmot et al., 2010). The 2000 U.S. Surgeon General’s report on oral health raised an alarm for the existence of “profound disparities that affect those without the knowledge or resources to achieve good oral health care”. The U.S. Centers for Disease Control (CDC), as well as “Healthy People 2010” and “Health 2020”, has also articulated objectives regarding the elimination or reduction of health disparities.
Despite the numerous advances in oral health sciences, including the development of preventive, diagnostic, and therapeutic agents and methods, oral health disparities persist; in fact, some oral health disparities may be on the increase. Compounded with an increasingly interconnected but frequently divergent and disequalizing global community (Schrecker et al., 2008), substantial proportions of the population suffer a disproportionate burden of oral disease and impairment. Academic, research, policy, and community stakeholders concur that action is needed to reverse this unfairness. In this review we summarize recent work in oral health disparities research and emphasize the need for a solid theoretical framing to guide oral health disparities research. We provide a conceptual framework outlining the important role of the social determinants of oral health and illustrate pathways that may operate across the continuum of these determinants during the lifecourse, highlighting potential areas for intervention.
Definitions and Perspectives of Oral Health Disparities
Several definitions of health disparities exist. The common theme in all definitions is that health disparities are population-specific health differences (in the prevalence of disease, health outcomes, or access to health care) that are avoidable and unfair when regarded from social justice, ethical, and human rights perspectives. The U.S. CDC has defined health disparities (or inequities) as “differences in health outcomes and their determinants between segments of the population, as defined by social, demographic, environmental, and geographic attributes.” It follows that the complete absence of health disparities is typically defined as “health equity”. Healthy People 2020 defined health disparity as a “particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage”. These definitions, combined with the seminal report of the WHO-CSDH, imply the assignment of certain societal values (Diderichsen et al., 2001) in states of health, disease, and quality of life.
The unequal and inequitable distribution of the global burden of oral diseases and risks to oral health has been well-documented by the WHO (Petersen et al., 2005). The burden of oral disease is particularly high among disadvantaged and poor population groups in both developing and developed countries, indicating that social stratification (Diderichsen et al., 2001) and other social determinants of health are in play and may have similar, detrimental effects on both oral and general health (Sabbah et al., 2007). Indeed, oral health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their social and economic position, racial or ethnic group, religion, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation, gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion.
Oral health disparities are often conceptualized in terms of social determinants of health, with several factors such as income and education being involved across the social gradient (Jagger et al., 2013; Ravaghi et al., 2013). It must be noted, however, that several of the social determinants of health tend to cluster and co-vary, so that an ‘eco-social’ framework is best suited to study their causal effects on health and disease (Krieger, 1994). In the United States, health disparities, historically, have been viewed as predominantly racial, ethnic, and education differences. The U.S. Congress has charged the monitoring of disparities among these “priority populations” to the Agency for Healthcare Research and Quality, which produces an annual tracking of health disparities. However, there is ongoing debate on how best to examine racial/ethnic disparities in juxtaposition with all other social determinants of health, and whether racialization may perpetuate aspects of discrimination (Krieger, 2000).
A Proposed Framework
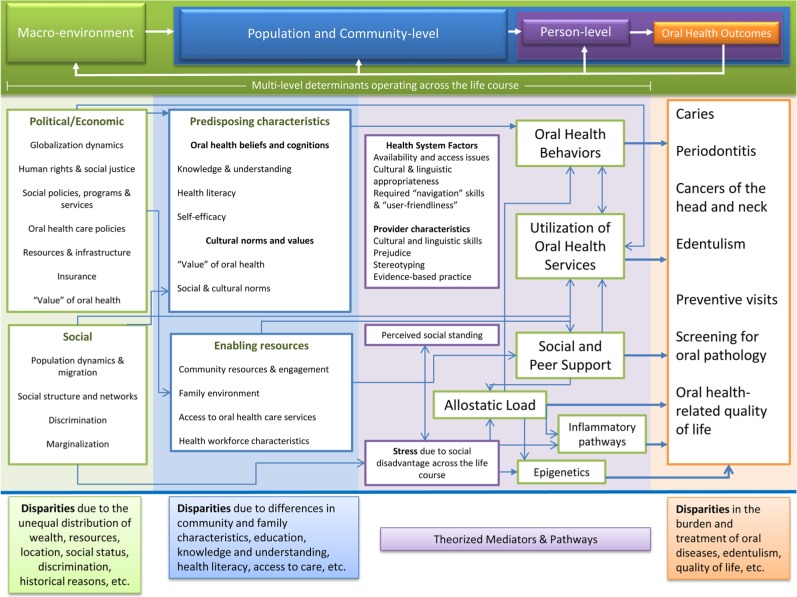
Oral health disparities are most commonly reported for caries, chronic periodontitis, and cancers of the head and neck, as well as for receipt of preventive dental visits, sealants, tooth loss, and quality of life (Dye et al., 2012; Thomson, 2012). In the Fig. we present a proposed framework for conceptualizing and addressing these oral health disparities. Although one model cannot possibly include all determinants, pathways, and oral health outcomes, it represents a detailed scheme of the current state of knowledge in the oral health disparities arena. The model is based on a modification of Andersen’s behavioral model and builds upon previous work on the multi-level influences of oral health (Fisher-Owens et al., 2007), as well as oral health disparities (Patrick et al., 2006; Watt and Sheiham, 2012). Acknowledging the pronounced social gradients of health and the fundamental causes of social inequalities as described by Diderichsen et al. (2001), our model emphasizes the major role of ‘distal’ and ‘upstream’ determinants, ranging from the dynamics of globalization, migration, and the social and political environment to community characteristics. Importantly, as our model explicitly illustrates, person-level or ‘proximal’ factors are nested within community and other ‘distal’ determinants, in a hierarchical fashion, which parallels their relative contribution in disparities, i.e., more upstream factors tend to have a greater impact. Further, we include a comprehensive number of mechanistic pathways that may be in play, including the emerging roles of perceived social standing and support, allostatic load, inflammatory pathways, and epigenetics. There may be a virtually infinite number of unobservable pathways that explain oral health outcomes at an individual level; however, on a population level, social, health care system, behavioral, and biological pathways are evident and important. Last, it must also be noted that feedback loops from oral health to biological, behavioral, community, and social factors are also plausible, likely, and warrant the field’s attention, since disparities and poor oral health in general have been shown to confer multi-level negative sequelae at all levels. While the framework will have to be validated, the need to approach oral health disparities from the perspectives of social justice and social determinants of health is warranted (Watt, 2007; Marmot et al., 2010; Sheiham et al., 2011).
Figure.
Proposed framework to conceptualize and act upon eliminating the sources of oral health disparities. The illustration outlines how hierarchically nested political, social, environmental, population, behavioral, and biological factors interact with each other to generate health disparities. A feedback loop of oral health outcomes on these factors is also depicted.
‘Distal’ Determinants of Health as Causes of Oral Health Disparities
There is overwhelming support for a bidirectional association between macro-level characteristics and health statuses of entire nations (Subramanian et al., 2002), involving the role of economic development, resources and infrastructure, population and societal characteristics, and others. As previously outlined, considerable work in oral health disparities has been centered on the social determinants of health, health systems, health policies, and politics. It has long been known that social disadvantage, measured in various ways, is associated with negative impacts on the oral health of affected segments of the population. Socio-economic status is known to underlie 3 major health determinants—health behaviors, environmental exposures, and health care—which are depicted more downstream in our model. The hierarchy or relative importance of these social or ‘distal’ determinants (i.e., social position vs. income) is not known and is likely heterogeneous across populations. Locker has contributed substantially to this topic by examining the relationship between different measures of deprivation and oral health (Locker, 2000).
Socio-economic Gradients, Social Inequalities, and Perceived Social Standing
A considerable body of recent evidence illustrates the impact of social stratification and actual and perceived social standing on oral health disparities (Thomson et al., 2004; Jamieson and Thomson, 2006; Patrick et al., 2006). The impact of social gradient in oral health is pervasive and global: Hosseinpooret al. (2012) used 2002-2004 World Health Survey data from 52 counties and showed that pro-rich inequalities in oral health care coverage were evident in most countries and were actually more pronounced among the low-income ones. Costa and colleagues (2012) recently carried out a systematic review of the relationship between socio-economic indicators and dental caries and found that, across 41 studies, education, income, occupation, and Gini coefficient were associated with higher rates of caries. Along these lines, Bernabé and Hobdell (2010) analyzed data from 48 countries and found that, among affluent countries, income inequality may be a stronger determinant of childhood dental caries than is absolute income.
Some data exist to support that, in some populations, disparities may be ethnically – not socio-economically – driven. Fisher-Owens et al. (2013) used 2007 National Survey of Children’s Health data and found that racial/ethnic disparities in children’s oral health status and health care access were attributable largely to socio-economic and health insurance factors, suggesting that reducing health disparities may be more efficacious if efforts are targeted to the latter (distal) determinants. Similarly, Telford et al. (2011) found that disparities in adolescents’ oral health status and related behaviors were diminished, but not fully explained, by known socio-demographic indicators. In another recent study by Iida and Rozier (2013), the investigators utilized U.S.-representative data to show that mothers’ (low) perceived social capital was associated with both less frequent preventive dental visits and more unmet dental needs in their children.
Other global data are equally confirmatory and are alarming of profound socio-economic inequalities in oral health in Europe, North America, South America, and Asia (Do, 2012). Analysis of recent Australian adult oral health survey data, reported by Armfield et al. (2013), reaffirmed the existence of pervasive socio-economic inequalities in oral health, by income, education, and employment, as well as by self-perceived social standing. The latter observation, along with findings of Sanders et al. (2006), reinforces the importance of considering both actual and perceived social standing as a determinant of health disparities.
Predisposing and Enabling Factors
The constellation of upstream factors, including social stratification and disadvantage, has been shown to be associated with a large number of “intermediate” determinants, such as health beliefs and cognitions, knowledge and understanding, health literacy, resilience, and self-efficacy. The mechanisms underlying these associations are complex, and links to individual health behaviors are not straightforward (McAlister et al., 2007); however, the aforementioned and other emerging determinants of oral health disparities may reveal modifiable risk-increasing (“predisposing”) or enabling (“protective”) characteristics at the population, community, family, or person level and warrant attention in dental public health research and practice. Accounting for the effects of distal determinants on oral health outcomes can aid in the identification of important intermediate factors, such as access to and utilization of care, unequal treatment, and other “systemic” issues that can be targets for interventions (Gilbert et al., 2003).
Another perspective in oral health disparities can be gained by considering location. Early reports by Locker (Locker and Ford, 1994; Locker, 2000) illustrated the utility of area-based measures as indicators of oral health disparities. More recently, Ahn and colleagues (2011) confirmed the existence of oral health disparities by residential rurality and suggested that oral health improvements in these populations are strongly related to access to oral health care and lifestyle changes. Similarly, Finlayson et al. (2010) found that adults living near more neighborhood resources were less likely to report fair or poor oral health. Saman et al. (2011) used geospatial illustration methods to provide additional insights into the distribution of oral health disparities and supported the need to account for place of residence in dental public health research.
Health System Factors
Receipt of oral health care is a major component of several models explaining oral health status (Fisher-Owens et al., 2007) and related disparities (Patrick et al., 2006). Above and beyond the barrier of access to care, however, appropriate use of available oral health resources is not automatic; this is particularly important for oral health information and services, since accumulating evidence indicates that the readability of such information and the skills required to navigate the oral health care system may be excessive for large portions of the population. To fill this gap, a National Institute of Dental and Craniofacial Research workgroup defined oral health literacy as “the degree to which individuals have the capacity to obtain, process, and understand basic oral health information and services needed to make appropriate health decisions”. The emerging literature on health literacy offers additional mechanisms via which social, educational, and economic disadvantages are linked to oral health disparities (Horowitz and Kleinman, 2008), offering opportunities for interventions that have the potential to alleviate the negative effects of low literacy. The barrier of health literacy is arguably contextual and can be alleviated if the demands of navigating the oral health system, including language used by professionals and the readability of health information, are tailored to more culturally and literacy-appropriate levels.
Broader health system factors affecting access to care are considered to be important structural determinants of disparities. One recent study carried out in 11 European countries suggested that oral health care systems relying on public coverage showed fewer inequalities and were superior in their use compared with systems lacking public coverage (Palència et al., 2013). This is consistent with earlier findings among population-based samples from Canada and the United States, reported by Lasser et al. (2006), who suggested that universal health care coverage reduced most disparities in access to care. In 2001, the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services issued a report (“Eliminating Health Disparities in the United States”) indicating that expanding access to health care is “a critical component” of the agency’s work to eliminate disparities. From a different angle, Horton and Barker (2010) provided unique insight into the accumulation of oral health disparities among children of migrant Mexican farmworkers. As Tomar and Cohen (2010) commented, an ideal oral health care system that, among other properties, would be equitable, would be culturally competent, and would be emphasize oral health promotion, is possible, but its realization “would require tremendous commitment and political will […] to bring it to fruition”.
Pathways and Mediators Underlying Oral Health Disparities
The discovery of specific pathways through which socio-economic factors, social standing, deprivation, minority status, and other distal determinants affect health outcomes is a daunting task. However, the identification of pathways that contain modifiable factors would be of public health significance and, in parallel with population-level approaches, might offer avenues to alleviate health disparities. Adler and Stewart (2010) provide an overview of the evolution of research in the field, which has now shifted its attention to the interaction of multiple-level environmental influences and genetic factors across the lifespan. Indeed, it is now understood that certain “social environments ‘get under the skin’ to cause disease” via multi-level influences of social and environmental factors on people’s health and disease.
Consistent with this theory are findings of an association between high levels of chronic stress, depressive symptoms, and material hardship and fair or poor oral health (Finlayson et al., 2010). Recent evidence highlights possible neurobiological pathways that may link socio-economic position with health and disease (Gianaros and Manuck, 2010), including pathways of systemic stress, known to be associated with oral health outcomes. A concept that fits this mechanistic model is that of “allostatic load”, or the physiological consequences of stress and hardship (McEwen and Stellar, 1993), otherwise known as the “wear and tear of the body”. Although evidence in this domain is limited, one study found support for a role of allostatic load in explaining socio-economic disparities in the prevalence of chronic periodontitis (Sabbah et al., 2008). Emerging lines of research now examine biological markers of aging, such as telomere length attrition, to determine whether socio-economic disadvantage factors operating along the lifecourse may be reflected in one’s DNA (Cherkas et al., 2006). One additional and likely complementary mechanism is offered by epigenetics (Adler and Stewart, 2010; Thayer and Kuzawa, 2011), a pathway wherein social disadvantage can be imprinted on one’s genetic backbone to affect disease occurrence. It must be acknowledged, however, that while the cognitive and biological “imprinting” of perceived social position can be considered an important health determinant along the lifecourse, a complex and possibly bi-directional relationship between health and social position has been proposed (Garbarski, 2010).
Gao et al. (2010) offered unique insight into the behavioral pathways that may explain disparities in children’s oral health. In their study, they found that parents’ knowledge, attitudes, and practices partially explained children’s ethnic and socio-economic oral health disparities, with deprivation having a direct effect on dental attendance and ethnicity influencing home care practices. Dietary factors are also considered to be part of causal pathways linking economic and social disadvantage with (oral) health disparities. Although diet is to some degree culturally and behaviorally influenced, it is also determined by the availability of, access to, and affordability of healthy foods, elements which are largely correlates of location and economic means. Similarly, in the study by Finlayson et al. (2010), higher levels of self-esteem and mastery have been shown to be protective, and more religious adults were also less likely to report fair or poor oral health.
The Relationship between Distal and Proximal Determinants: Theories and Measurement
Conceptualizing and quantifying relationships between social determinants of health and proximal ones, such as behaviors, the underlying biology and health outcomes to guide research in health disparities are intellectually and philosophically rigorous exercises. Krieger (2001) has offered an excellent critical review of social epidemiology theories that have been used to explain health and disease distribution in the population, including the psychosocial, social production/political economy, and eco-social family of theories. Although a detailed presentation of these theories and their applications is beyond the scope of this review, understanding the key element of ‘embodiment’, reflecting the process of “how we literally incorporate, biologically, the material and social world in which we live”, is worthwhile. In a commentary, Sisson (2007) acknowledged that existing theoretical explanations for social inequalities in oral health vary in their focus and standpoint and reviewed available evidence supporting “materialist”, cultural/behavioral, psychosocial, and lifecourse perspectives. While various models and approaches for the conceptualization and estimation of effects of distal determinants of oral health exist, it must be underscored that a complex theoretical framework should be accompanied by appropriate analytical tools. Newton and Bower (2005) provide an excellent overview of oral epidemiology methods and strategies that can be applied to conceptualize and study the complex and frequently multi-level causal networks in the social determinants of oral health arena. Mackenbach and Kunst (1997) provided a detailed overview of available measures to quantify the magnitude of socio-economic inequalities in health. Blair et al. (2013) and Jagger et al. (2013) recently offered detailed examinations of different approaches and measures to quantify socio-economic oral health disparities.
Proposed Actions
Tackling oral health disparities will require strategic, concerted, and bold actions at local, national, and global levels. Although the current economic globalization does not guarantee better health, the globalization process may offer opportunities for the formation of a global health governance structure, where one can envision oral health being a fundamental human right, with health promotion and prevention prioritized over treatment and restoration. Current efforts and activities in the context of the International Association for Dental Research on addressing oral health disparities are summarized in the online Appendix. In the Table, we list 10 proposed actions that, if materialized, could help alleviate disparities. These actions include the creation of a global health governance framework (Frenk and Moon, 2013), adherence to human rights and democratic principles (Gregorio and Gregorio, 2013), community empowerment (Marmot et al., 2010) and emphasis on common risk factor and prevention approaches (Sheiham et al., 2011). Examples of successful population-based approaches in reducing oral health disparities include the introduction of community water fluoridation, likely the most successful dental public health intervention to date (Riley et al., 1999). Other approaches may include community- and school-based programs based on a common risk-factor (smoking, diet, alcohol use, stress, trauma, and more) approach (Sheiham and Watt, 2000), inter-professional education and collaboration, reshaping and improving the existing and future workforce, and utilizing new technologies to improve health communication with hard-to-reach populations (Glassman et al., 2012).
Table.
Proposed Actions for Eliminating Sources of Health Inequalities and Reducing Oral Health Disparities
| Support a framework of global health governance that safeguards oral health as a human right via international and national policies. |
| Upgrade the role, funding, and capacity of the World Health Organization to function as a key player influencing politics and policies to reduce oral health disparities. |
| Align with intersectoral efforts and strategies aiming to reduce poverty and marginalization via democratic processes and community empowerment. |
| Support research informing policy on the social determinants of health. |
| Link communities with public health and research agents, including public, community, and non-governmental health organizations. |
| Identify and support effective and efficient community-based holistic (non-compartmentalized) oral health promotion interventions utilizing a common risk factor approach. |
| Promote actions that eliminate barriers of access to oral health information, care, and utilization of health services, including an appropriately trained and distributed workforce. |
| Facilitate the formation of and ensure adherence to culturally, linguistically, and health-literacy-appropriate standards in all aspects of oral health care. |
| Translate ‘omics discoveries into public-health-relevant and actionable knowledge and utilize same. |
| Disseminate the importance and value of oral health as part of overall health, in terms of wellness, oral health promotion, and disease prevention across the lifecourse. |
Taking into consideration the constellation of distal determinants of oral health, including macro-level and social factors, it is understood that population-level approaches are considered superior to high-risk group identification and targeting, whereas combinations of both strategies can be most efficacious (Watt, 2007; Sheiham et al., 2011). There are several reasons why efforts should be invested primarily on addressing population-level influences. First, action on the fundamental disparities-generating or “upstream” causes is an ethical imperative from human rights and social justice perspectives. Second, population-level and common risk-factor approaches have the potential to confer equitable health promotion benefits in substantial population groups, consistent with Rose’s paradigm (Rose, 1985). Third, high-risk-group and ‘individual behavior’ approaches do not address the root causes of health disparities, perpetuate the existence of high-risk groups, and, although popular during the past decades, have failed to reduce the oral disease burden gap between disadvantaged and more affluent groups of the population (Watt, 2007).
Summary and Recommendations
Oral health disparities are downstream of major sources of inequalities in the distribution of wealth, education, social status, and other social determinants of health, such as minority status. The eradication of health disparities may be utopic in a political, social, or health system that creates or perpetuates such inequalities. Today, a global health governance framework strong enough to catalyze the necessary changes does not exist. Nevertheless, all stakeholders, each from its own standpoint, can and must undertake efforts to reduce or alleviate oral health disparities and their consequences within the current system, wherein certain vulnerable groups of the population are susceptible to experience a disproportionate burden of disease and diminished opportunities to achieve optimal health. Multiple distal determinants and oral-health-disparities-generating pathways exist; research that moves beyond the detection of differences between/among population subgroups or individual risk behaviors is warranted. Ideally, research in the arena of oral health disparities should strive to consider all operational levels, including global dynamics and trends, political and economic factors, the social context, and health system and provider-level factors.
A roadmap to address the issue of oral health disparities must include both policy and science. It must be underscored that unless macro-level factors are considered, oral health disparities will be perpetuated. The ethical imperative of eliminating health disparities will require bold policies and scientific inquiry on the root causes of the problem, including the global misdistribution of resources and power, and pronounced social gradients. At the same time, empowerment of communities via increased opportunities for education, child care, employment, community-building and economic revitalization, and housing can help close the oral health disparities gap in the foreseeable future. However, tangible progress is likely to be realized only via the creation of global movement and concerted efforts by all stakeholders, including international organizations, policymakers, the civil society, and academic, research, and professional bodies. Is there a better cause or time for an oral health academic activism wave?
Footnotes
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
The authors acknowledge support from the National Institute of Dental and Craniofacial Research (grant RO1DE018045).
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Adler NE, Stewart J. (2010). Health disparities across the lifespan: meaning, methods, and mechanisms. Ann NY Acad Sci 1186:5-23. [DOI] [PubMed] [Google Scholar]
- Ahn S, Burdine JN, Smith ML, Ory MG, Phillips CD. (2011). Residential rurality and oral health disparities: influences of contextual and individual factors. J Prim Prev 32:29-41. [DOI] [PubMed] [Google Scholar]
- Armfield JM, Mejía GC, Jamieson LM. (2013). Socioeconomic and psychosocial correlates of oral health. Int Dent J 63:202-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernabé E, Hobdell MH. (2010). Is income inequality related to childhood dental caries in rich countries? J Am Dent Assoc 141:143-149. [DOI] [PubMed] [Google Scholar]
- Blair YI, McMahon AD, Macpherson LM. (2013). Comparison and relative utility of inequality measurements: as applied to Scotland’s child dental health. PLoS One 8:e58593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherkas LF, Aviv A, Valdes AM, Hunkin JL, Gardner JP, Surdulescu GL, et al. (2006). The effects of social status on biological aging as measured by white-blood-cell telomere length. Aging Cell 5:361-365. [DOI] [PubMed] [Google Scholar]
- Commission on Social Determinants of Health (2008). CSDH final report: closing the gap in a generation: health equity through action on the social determinants of health. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Costa SM, Martins CC, Bonfim Mde L, Zina LG, Paiva SM, Pordeus IA, et al. (2012). A systematic review of socioeconomic indicators and dental caries in adults. Int J Environ Res Public Health 9:3540-3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diderichsen F, Evans T, Whitehead M. (2001). The social basis of disparities in health. In: Challenging inequities in health: from ethics to action. New York, NY: Oxford University Press, pp; 12-23. [Google Scholar]
- Do LG. (2012). Distribution of caries in children: variations between and within populations. J Dent Res 91:536-543. [DOI] [PubMed] [Google Scholar]
- Dye BA, Li X, Thorton-Evans G. (2012). Oral health disparities as determined by selected healthy people 2020 oral health objectives for the United States, 2009-2010. NCHS Data Brief 104:1-8. [PubMed] [Google Scholar]
- Finlayson TL, Williams DR, Siefert K, Jackson JS, Nowjack-Raymer R. (2010). Oral health disparities and psychosocial correlates of self-rated oral health in the National Survey of American Life. Am J Public Health 100(Suppl 1):246-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader MJ, Bramlett MD, et al. (2007). Influences on children’s oral health: a conceptual model. Pediatrics 120:e510-e520. [DOI] [PubMed] [Google Scholar]
- Fisher-Owens SA, Isong IA, Soobader MJ, Gansky SA, Weintraub JA, Platt LJ, et al. (2013). An examination of racial/ethnic disparities in children’s oral health in the United States. J Public Health Dent 2013. 73:166-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenk J, Moon S. (2013). Governance challenges in global health. N Engl J Med 368:936-942. [DOI] [PubMed] [Google Scholar]
- Garbarski D. (2010). Perceived social position and health: is there a reciprocal relationship? Soc Sci Med 70:692-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao XL, Hsu CY, Xu YC, Loh T, Koh D, Hwarng HB. (2010). Behavioral pathways explaining oral health disparity in children. J Dent Res 89:985-990. [DOI] [PubMed] [Google Scholar]
- Gianaros PJ, Manuck SB. (2010). Neurobiological pathways linking socioeconomic position and health. Psychosom Med 72:450-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert GH, Duncan RP, Shelton BJ. (2003). Social determinants of tooth loss. Health Serv Res 38(6 Pt 2):1843-1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glassman P, Harrington M, Namakian M, Subar P. (2012). The virtual dental home: bringing oral health to vulnerable and underserved populations. J Calif Dent Assoc 40:569-577. [PubMed] [Google Scholar]
- Gregorio LE, Gregorio DI. (2013). Polity and health care expenditures: the association among 159 nations. J Epidemiol Glob Health 3:49-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz AM, Kleinman DV. (2008). Oral health literacy: the new imperative to better oral health. Dent Clin North Am 52:333-344. [DOI] [PubMed] [Google Scholar]
- Horton S, Barker JC. (2010). Stigmatized biologies: examining the cumulative effects of oral health disparities for Mexican American farmworker children. Med Anthropol Q 24:199-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosseinpoor AR, Itani L, Petersen PE. (2012). Socio-economic inequality in oral healthcare coverage: results from the World Health Survey. J Dent Res 91:275-281. [DOI] [PubMed] [Google Scholar]
- Iida H, Rozier RG. (2013). Mother-perceived social capital and children’s oral health and use of dental care in the United States. Am J Public Health 103:480-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagger DC, Sherriff A, Macpherson LM. (2013). Measuring socio-economic inequalities in edentate Scottish adults – cross-sectional analyses using Scottish Health Surveys 1995-2008/09. Community Dent Oral Epidemiol 41:499-508. [DOI] [PubMed] [Google Scholar]
- Jamieson LM, Thomson WM. (2006). Adult oral health inequalities described using area-based and household-based socioeconomic status measures. J Public Health Dent 66:104-109. [DOI] [PubMed] [Google Scholar]
- Krieger N. (1994). Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med 39:887-903. [DOI] [PubMed] [Google Scholar]
- Krieger N. (2000). Refiguring “race”: epidemiology, racialized biology, and biological expressions of race relations. Int J Health Serv 30:211-216. [DOI] [PubMed] [Google Scholar]
- Krieger N. (2001). Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol 30:668-677. [DOI] [PubMed] [Google Scholar]
- Lasser KE, Himmelstein DU, Woolhandler S. (2006). Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. Am J Public Health 96:1300-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locker D. (2000). Deprivation and oral health: a review. Community Dent Oral Epidemiol 28:161-169. [DOI] [PubMed] [Google Scholar]
- Locker D, Ford J. (1994). Evaluation of an area-based measure as an indicator of inequalities in oral health. Community Dent Oral Epidemiol 22:80-85. [DOI] [PubMed] [Google Scholar]
- Mackenbach JP, Kunst AE. (1997). Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med 44:757-771. [DOI] [PubMed] [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S; Commission on Social Determinants of Health (2008). Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 372:1661-1669. [DOI] [PubMed] [Google Scholar]
- Marmot M, Atkinson T, Bell J, Black C, Broadfoot P, Cumberlege J, et al. (2010). Fair society, healthy lives: the Marmot Review. Strategic review of health inequalities in England post-2010 (The Marmot Review: UK). URL accessed on 10/16/2013 at: http://www.marmotreview.org/.
- McAlister AL, Perry CL, Parcel GS. (2007). How individuals, environments, and health behaviours interact: social cognitive theory. In: Health behaviour and health education; theory, research, and practice. Glanz K, Rimer BK, Viswanath K, editors. San Francisco, CA: Jossey Bass, pp. 169-188. [Google Scholar]
- McEwen BS, Stellar E. (1993). Stress and the individual. Mechanisms leading to disease. Arch Intern Med 153:2093-2101. [PubMed] [Google Scholar]
- Newton JT, Bower EJ. (2005). The social determinants of oral health: new approaches to conceptualizing and researching complex causal networks. Community Dent Oral Epidemiol 33:25-34. [DOI] [PubMed] [Google Scholar]
- Palència L, Espelt A, Cornejo-Ovalle M, Borrell C. (2013). Socioeconomic inequalities in the use of dental care services in Europe: what is the role of public coverage? Community Dent Oral Epidemiol [Epub ahead of print 6/20/2013] (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick DL, Lee RS, Nucci M, Grembowski D, Jolles CZ, Milgrom P. (2006). Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health 6(Suppl 1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. (2005). The global burden of oral diseases and risks to oral health. Bull World Health Organ 83:661-669. [PMC free article] [PubMed] [Google Scholar]
- Ravaghi V, Quiñonez C, Allison PJ. (2013). The magnitude of oral health inequalities in Canada: findings of the Canadian health measures survey. Community Dent Oral Epidemiol 41:490-498. [DOI] [PubMed] [Google Scholar]
- Riley JC, Lennon MA, Ellwood RP. (1999). The effect of water fluoridation and social inequalities on dental caries in 5-year-old children. Int J Epidemiol 28:300-305. [DOI] [PubMed] [Google Scholar]
- Rose G. (1985). Sick individuals and sick populations. Int J Epidemiol 14:32-38. [DOI] [PubMed] [Google Scholar]
- Sabbah W, Tsakos G, Chandola T, Sheiham A, Watt RG. (2007). Social gradients in oral and general health. J Dent Res 86:992-996. [DOI] [PubMed] [Google Scholar]
- Sabbah W, Watt RG, Sheiham A, Tsakos G. (2008). Effects of allostatic load on the social gradient in ischaemic heart disease and periodontal disease: evidence from the Third National Health and Nutrition Examination Survey. J Epidemiol Community Health 62:415-420. [DOI] [PubMed] [Google Scholar]
- Saman DM, Johnson AO, Arevalo O, Odoi A. (2011). Geospatially illustrating regional-based oral health disparities in Kentucky. Public Health Rep 126:612-618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders AE, Slade GD, Turrell G, Spencer AJ, Marcenes W. (2006). The shape of the socioeconomic-oral health gradient: implications for theoretical explanations. Community Dent Oral Epidemiol 34:310-319. [DOI] [PubMed] [Google Scholar]
- Schrecker T, Labonté R, De Vogli R. (2008). Globalisation and health: the need for a global vision. Lancet 372:1670-1676. [DOI] [PubMed] [Google Scholar]
- Sheiham A, Watt RG. (2000). The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol 28:399-406. [DOI] [PubMed] [Google Scholar]
- Sheiham A, Alexander D, Cohen L, Marinho V, Moysés S, Petersen PE, et al. (2011). Global oral health inequalities: task group—implementation and delivery of oral health strategies. Adv Dent Res 23:259-267. [DOI] [PubMed] [Google Scholar]
- Sisson KL. (2007). Theoretical explanations for social inequalities in oral health. Community Dent Oral Epidemiol 35:81-88. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Belli P, Kawachi I. (2002). The macroeconomic determinants of health. Annu Rev Public Health 23:287-302. [DOI] [PubMed] [Google Scholar]
- Telford C, Coulter I, Murray L. (2011). Exploring socioeconomic disparities in self-reported oral health among adolescents in California. J Am Dent Assoc 142:70-78. [DOI] [PubMed] [Google Scholar]
- Thayer ZM, Kuzawa CW. (2011). Biological memories of past environments: epigenetic pathways to health disparities. Epigenetics 6:798-803. [DOI] [PubMed] [Google Scholar]
- Thomson WM. (2012). Social inequality in oral health. Community Dent Oral Epidemiol 40(Suppl 2):28-32. [DOI] [PubMed] [Google Scholar]
- Thomson WM, Poulton R, Milne BJ, Caspi A, Broughton JR, Ayers KM. (204). Socioeconomic inequalities in oral health in childhood and adulthood in a birth cohort. Community Dent Oral Epidemiol 32:345-353. [DOI] [PubMed] [Google Scholar]
- Tomar SL, Cohen LK. (2010). Attributes of an ideal oral health care system. J Public Health Dent 70(Suppl 1):6-14. [DOI] [PubMed] [Google Scholar]
- Watt RG. (2007). From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol 35:1-11. [DOI] [PubMed] [Google Scholar]
- Watt RG, Sheiham A. (2012). Integrating the common risk factor approach into a social determinants framework. Community Dent Oral Epidemiol 40:289-296. [DOI] [PubMed] [Google Scholar]