Abstract
Airway stenting is the chosen treatment for patients affected by subglottic tracheal stenosis and unfit for surgery. Among the different types of prostheses, the Dumon stent is a valid option especially in patients without tracheotomy. Insertion is usually achieved by pushing the stent off from a loader using a prosthesis pusher. If the stent is expelled below the stenosis, rigid forceps grasping the proximal end of the stent retract it above the stenosis. However, in difficult cases such as rigid stenosis with a luminal diameter smaller than the profile of the stent, such a manoeuvre may be difficult in non-expert hands. Thus, we proposed a simple and safe technique to facilitate the placement of a Dumon stent. We passed a long thread from outside to the inside of the stent. After the dilatation of the stenosis, the stent was pushed and, if needed, easily retracted with the thread into the proper position to ensure airway patency and to avoid migration. In addition, our procedure could be useful also to rapidly remove the stent if its size turned out to be inaccurate for the stenosis. With such a simple method we successfully treated 7 consecutive patients affected by complex subglottic stenosis and unfit for surgery.
Keywords: Tracheal stenosis, Dumon Stent, Rigid bronchoscopy
INTRODUCTION
Airway stenting is the chosen treatment for patients affected by subglottic tracheal stenosis and unfit for surgery [1]. Among the different types of prostheses, a Dumon stent is a valid option especially in patients without tracheotomy. Unfortunately, its placement may be difficult in the management of complex stenosis (lesion >1 cm, an A-shape fracture of the cartilaginous airway or with concomitant malacia) [2, 3]. We describe a simple and safe technique to introduce and place a Dumon stent in patients with complex tracheal stenosis close to the vocal folds.
METHODS
All procedures were performed in the operating theatre under general anaesthesia. Prior to intubation for the procedure, the stent was loaded with silk suture thread (Silkam®, B Braun, Aesculap, Tuttlingen, Germany; length: 250 cm; size: 2) and then carried into a classical introducer. The size of the stent was determined by measuring the length of the lesion and the diameters of airway at the level of the cricoid, proximal and mid-trachea using a preoperative computed tomography scan. Patients were intubated with a 14 diameter rigid bronchoscopy KARL STORZ GmbH & Co. KG, Tuttlingen, Germany). Ventilation was ensured via the sideport of the bronchoscope. After the initial endoscopic intervention including balloon dilatation, radial incision and microdebridement of the endoluminal component of the stenosis with Nd:Yag laser, the stenosis was dilatated with rigid bronchoscopes of increasing diameters. Then the bronchoscope was positioned with the tip distally to the stenotic lesion. The introducer previously loaded with the stent was passed through the open bronchoscope, and the prosthesis pusher expelled the stent into the stenotic segment. During expulsion, the bronchoscope was simultaneously retracted over a distance equal to the length of the stent. If the stent was positioned below the stenosis, the thread easily retracted the stent above the stenosis to cover at least 0.5 cm of normal airway at each end of the stenosis. At the end of the procedure, the thread was removed. Postoperatively, all patients underwent bronchoscopy at 48 h and then on a monthly basis. Yet, we usually recommended immediate saline nebulization, adding steroid for the first 5 days after the procedure. The technique is fully described in Fig. 1; an example is reported in Supplementary Video 1.
Figure 1:
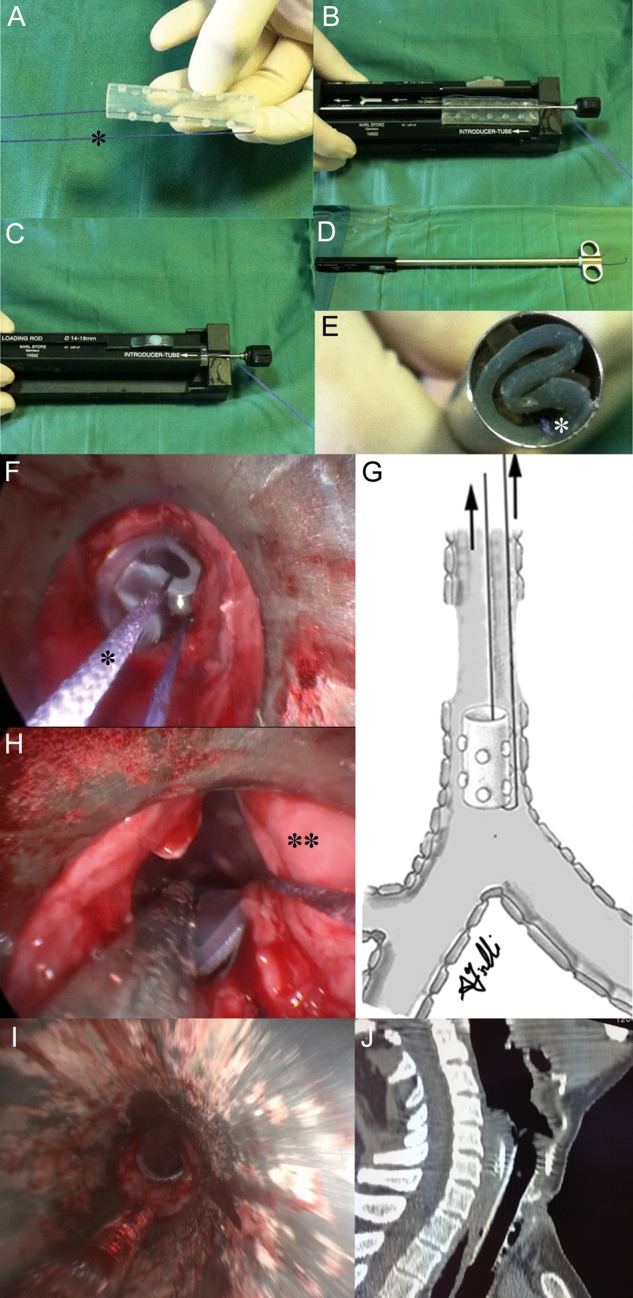
A Dumon stent, previously treated with a spray lubricant, was loaded with a long thread (*) (A). The stent was positioned in a Tonn™ (Novatech) stent applicator and locked in the loading rod (B). The folding system was closed and the rod was removed (C). The introducer was inserted into the folding system and then loading rod was inserted in the opposite end of the system to load the stent into the introducer (D). The stent with the thread (*) was loaded in the introducer and made ready for deployment through rigid bronchoscopy (E). The stent with the thread (*) was extracted below tight and rigid stenosis, distant from the vocal folds 1 cm (F). The stent was easily retracted above the stenosis (G) and positioned just under the vocal folds in order to preserve airway patency and phonation (H). At the end of the procedure, the thread was removed (I). A chest tomography scan, performed 3 weeks after the procedure, showed the exact position of the stent (J).
Supplementary Video 1:
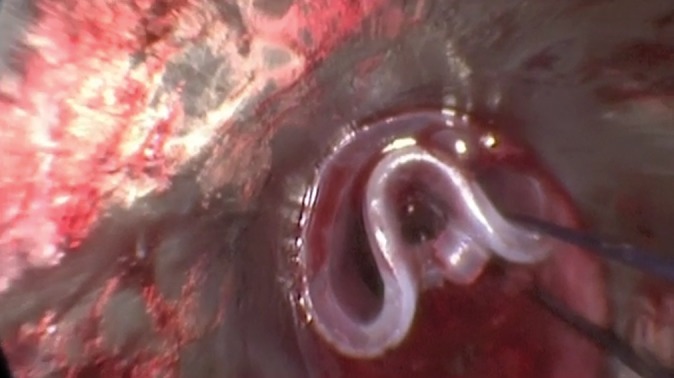
After stenosis dilatation, the stent was expelled below the stenosis. It was then easily retracted by the thread above the stenosis and placed under the vocal folds. The stent covered the whole stenosis, and 0.5 cm of normal airway at the proximal and distal end of the stenosis.
RESULTS
This procedure was adopted in 7 consecutive patients as summarized in Table 1. Our cohort included patients with multiple cardiovascular, pulmonary and systemic comorbidities that precluded surgery at the time of diagnosis. All lesions were complex with a mean length of 21 ± 6.2 mm (range 15–30 mm), a mean airway lumen of 6.5 ± 1.7 mm (range 4–9 mm) and a mean distance from the vocal folds of 14 ± 3.1 mm (range 10–18 mm). An exclusion criterion was the presence of tracheotomy, because in such a case we preferred to use a T-tube rather than a Dumon stent. Using this technique, in all patients the stent was correctly applied without problems preserving airway patency and phonation. Patients were monitored monthly after the procedure. We observed mucus plugging in 1 patient and granulation tissue formation at the proximal end of the stent in another. All these patients were successfully managed with bronchoscopy without removing the stent [4]. No case of spontaneous migration was reported.
Table 1:
Characteristics of the study population
| Patient | Sex | Age | Aetiology | Length of stenosis (mm) | Lumen of stenosis (mm) | Distance from the vocal folds (mm) | Stent size (mm) | Operation time (min) | Complication | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 65 | Post-intubation | 25 | 8 | 15 | 17/60 | 95 | Granulation formation | 15 |
| 2 | M | 55 | Post-intubation | 20 | 9 | 16 | 18/40 | 100 | – | 12 |
| 3 | M | 71 | Thyroid cancer | 20 | 4 | 10 | 18/40 | 90 | Mucus plugging | 8 |
| 4 | M | 57 | Post-tracheotomy | 30 | 5 | 18 | 16/60 | 85 | – | 7 |
| 5 | F | 73 | Post-intubation | 15 | 7 | 10 | 16/40 | 80 | – | 6 |
| 6 | F | 61 | Post-intubation | 20 | 6 | 13 | 16/40 | 70 | – | 6 |
| 7 | M | 67 | Thyroid cancer | 20 | 7 | 16 | 18/40 | 70 | – | 4 |
DISCUSSION
Surgical resection and reconstruction is the best treatment for the management of tracheal stenosis close to the vocal folds [1]. In patients unfit for surgery, treatment options include a tracheotomy, Montgomery T tube or Dumon silicon stent. The Dumon stent is an attractive option that preserves laryngeal function and does not require the presence of a stoma [1, 2]. Insertion is usually achieved by pushing the stent off from a loader using a prosthesis pusher. If the stent is expelled below the stenosis, rigid forceps grasping the proximal end of the stent retract it above the stenosis. At the end of the procedure, the stent should cover at least 0.5 cm of normal airway at each end of the stenosis to preserve airway patency and avoid migration [5]; in addition, it should be distant from the vocal folds to preserve phonation and avoid formation of tissue granulation. However, in difficult cases such as rigid stenosis with a luminal diameter smaller than the profile of the stent, such a manoeuvre may be difficult in non-expert hands. Thus, we proposed a simple and safe technique, not reported before, in order to facilitate the placement of the Dumon stent.
We passed a long thread from outside to the inside of the stent. After the dilatation of the stenosis using a rigid bronchoscopy, the stent was pushed and, if needed, easily retracted with the thread above the stenosis into the proper position to assure airway patency and to avoid migration. In addition, our procedure could be useful also to rapidly remove the stent if its size resulted to be inaccurate for the stenosis. Although our procedure may seem cumbersome, the learning curve is short as confirmed by serial reduction in operating times seen in our cohort. However, for the first time we suggest to load the stent with thread before intubation in order to reduce the duration of anaesthesia. No migration and no case of changing stent were registered. However, the mean follow-up of our population was 8.2 ± 3.8 months (range 4–15 months); thus our results should be corroborated by a longer follow-up.
In conlusion, our method is easy to perform, safe and cheap. It facilitates a challenging procedure of placing a Dumon stent in complex subglottic stenosis. Thus, it may be particularly useful for young surgeons (2/7 stenting of our series were performed by trainees assisted by a senior surgeon) and/or in small centres where a large variety of forceps is not available.
Supplementary material
Supplementary material is available at ICVTS online.
Conflict of interest: none declared.
REFERENCES
- 1.Saghebi SR, Zangi M, Tajali T, Farzanegan R, Farsad SM, Abbasidezfouli A, et al. The role of T-tubes in the management of airway stenosis. Eur J Cardiothorac Surg. 2013;43:934–9. doi: 10.1093/ejcts/ezs514. [DOI] [PubMed] [Google Scholar]
- 2.Majid A, Fernandez-Bussy S, Kent M, Folch E, Fernandez L, Cheng G, et al. External fixation of proximal tracheal airway stents: a modified technique. Ann Thorac Surg. 2012;93:e167–9. doi: 10.1016/j.athoracsur.2012.01.094. [DOI] [PubMed] [Google Scholar]
- 3.Galluccio G, Lucantoni G, Battistoni P, Paone G, Batzella S, Lucifora V, et al. Interventional endoscopy in the management of benign tracheal stenoses: definitive treatment at long-term follow-up. Eur J Cardiothorac Surg. 2009;35:429–33. doi: 10.1016/j.ejcts.2008.10.041. [DOI] [PubMed] [Google Scholar]
- 4.Fiorelli A, Mazzone S, Mazzone A, Santini M. The digital AcuBlade laser system to remove huge vocal fold granulations following subglottic airway stent. Interact CardioVasc Thorac Surg. 2013;17:591–3. doi: 10.1093/icvts/ivt226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Venuta F, Rendina EA, De Giacomo T. Airway Stenting. CTSNet. [published 21 August 2008] (3 May 2013, date last accessed) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


