Abstract
Objective. To evaluate the efficacy of case-based learning to teach pharmacy students health literacy concepts and skills in managing patients with limited health literacy.
Design. A health literacy patient case was developed and incorporated into a case-based learning laboratory. The case involved a patient with limited health literacy and required students to evaluate and formulate a care plan.
Assessment. A comparison of pretest and posttest scores demonstrated that students gained health literacy knowledge and skills through completion of the patient case. Students believed that the case-based exercise was successful in meeting specific learning objectives for the course.
Conclusions. Addition of a case-based learning was effective in teaching pharmacy students health literacy concepts and skills.
Keywords: health literacy, health literacy education, case-based learning
INTRODUCTION
The Institute of Medicine defines health literacy as, “The degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”1 Adequate health literacy requires the ability to read, understand, and apply health information in order to make health-care related decisions.
The first national assessment of health literacy in the United States was conducted by the 2003 National Assessment of Literacy (NAAL). The 2003 NAAL health literacy report estimated that more than one-third of patients have basic or below basic health literacy skills.2 Low health literacy is associated with a higher risk for hospitalization and use of emergency services.3
Despite the negative impact of poor health literacy, physicians continue to overestimate their patients’ literacy levels, while pharmacists rarely address health literacy issues with their patients.4,5 Health care providers play an essential role in communicating health-related information; thus, receiving adequate health literacy training and education is essential to improving patient care. Pharmacists can play a distinctive role in overcoming health literacy barriers by identifying patients with poor health literacy and improving patient medication adherence and outcomes through more effective medication education.
In efforts to address poor health literacy, the Institute of Medicine advocates the need to incorporate health literacy education into the curricula and competencies of professional schools.1 The Accreditation Council for Pharmacy Education (ACPE) has supported this by requiring pharmacy colleges and schools to include health literacy in their curriculum.6 Little published data exist regarding formal health literacy education as part of the curricula in pharmacy education. While some published evidence demonstrates the use of different active-learning strategies, only 1 study reported the use of a patient case to enhance health literacy knowledge.7-9 Case-based learning is commonly used in health professional education. Although it appears to be an effective educational tool, most claims for the efficacy of case-based learning relies on subjective student feedback. Strong objective evidence is lacking.10-16
At the Feik School of Pharmacy, Applied Pharmacy Care is a series of 6 courses that focuses on the application of pharmaceutical care principles, pharmaceutical knowledge, and professional techniques to solve patient- and medication-related issues.17 Health literacy had been taught in only 1 course, Applied Pharmacy Care II, to first-year (P1) pharmacy students. The health literacy module involved a 1-hour lecture and a 3-hour laboratory. To increase and enhance health literacy education in the curriculum and to assess case-based learning as a learning tool for health literacy, investigators decided to incorporate health literacy education into the Applied Pharmacy Care V course. The objective of this study was to evaluate the efficacy of case-based learning in teaching basic health literacy concepts and pharmacist skills in managing patients with limited health literacy. This study assessed case-based learning as an education tool for health literacy education.
DESIGN
In Applied Pharmacy Care V, third-year (P3) pharmacy students used therapeutics knowledge and evidence-based medicine to develop and design care plans for patient cases. Each student was assigned to 1 of 3 weekly 3-hour laboratory classes, with approximately 32 to 33 students in each class. Class sessions took place in a large room equipped with wireless Internet access.
This laboratory course covered 12 patient cases, and students worked in assigned groups of 4 or 5 to review disease state and drug information, assess patient cases, and develop care plans. One case was assigned each week and generally covered a specific disease state. One day prior to each patient case, students were assigned reading materials and assignments to prepare for the case. During the weekly laboratory session, students were allotted 2 hours to assess the case and design specific care plans. In addition to assigned readings, computer laptops, and computer Internet access, students could use textbooks and other references to assist with case exercises. Each group was required to develop 1 formal SOAP note to submit for grading. Each SOAP note had to be typed and submitted to instructors electronically. At the end of each session, the laboratory facilitator led a discussion with the students of the patient cases and care plans.
The instructional design of this course was learner focused and relied significantly on group interaction. Students could share ideas and opinions, as well as discuss any pertinent issues or important concepts. This method of learning encouraged a teamwork approach and allowed students to develop essential skills for collaborative patient care. The instructor primarily served as the facilitator and each laboratory class had a different facilitator, thus, requiring a total of 3 facilitators a week. Postgraduate year 1 pharmacy residents from local programs functioned as the facilitator for a majority of the laboratory sessions. The 2 faculty members who coordinated the course were responsible for grading the SOAP notes and facilitating a limited number of laboratories.
To incorporate health literacy education concepts, 1 of the 12 planned patient cases involved a patient with poor health literacy (Appendix 1). Assigned reading materials included, “Quick Guide to Health Literacy,” “Health Literacy and Patient Safety: Help Patients Understand,” and “Chapter Three: Health Literacy and Medication Use.”18-20 Students also were given case-guided questions during the laboratory (Appendix 1). The case-guided questions directed students to focus on major health literacy concepts and expected learning objectives. The learning objectives of this patient case exercise were (1) to define and review basic health literacy concepts, (2) to identify risk factors for limited health literacy, (3) to recognize common signs of patients with limited health literacy, (4) to review the impact of limited health literacy on patient health status and medication adherence, and (5) to learn and design different strategies to overcome limited health literacy. Upon completion of this exercise, students should be able to apply basic health literacy concepts and skills to practice.
The health literacy case-based exercise engaged both the lower levels of learning within Bloom’s taxonomy (knowledge and comprehension) and the higher levels (application and synthesis). This study was approved by the University of the Incarnate Word Institutional Review Board. Informed consent was obtained from each student who participated in the study.
EVALUATION AND ASSESSMENT
To assess student achievement of the defined learning objectives, faculty course coordinators developed a 10-item test consisting of 5 multiple-choice questions and 5 true/false questions (Appendix 2). Questions 1, 5, 7, and 8 were designed to evaluate student knowledge on basic health literacy concepts. Questions 2, 3, and 4 evaluated students’ abilities to identify risk factors for limited health literacy and assessed abilities to recognize common signs of patients with limited health literacy. Questions 6 and 9 assessed student knowledge on the impact of limited health literacy on patient health status and medication adherence, while question 10 assessed knowledge on strategies to address limited health literacy. Each question was worth 1 point for a total value of 10 points for the test. No partial credit was given for any question. To measure baseline knowledge and skills, the test was initially given as a pretest at the beginning of the course in week 1. Students were not given answers to the questions after completion of the pretest. To objectively measure student learning as gained knowledge and skills, the test was again administered as a posttest. The posttest was given during laboratory class in week 8, immediately after students completed the health literacy case exercise and class discussion. All pretests, posttests, and student evaluations were completed anonymously.
A two-sample t test of unequal variances was used for statistical analysis. Ninety-seven students were enrolled in the course and all 97 completed both the pretest and posttest. The mean average score for the pretest was 6.9±1.5, and the mean average score for the posttest was 9.4±0.8. The increase in test score was significant (p< 0.001).
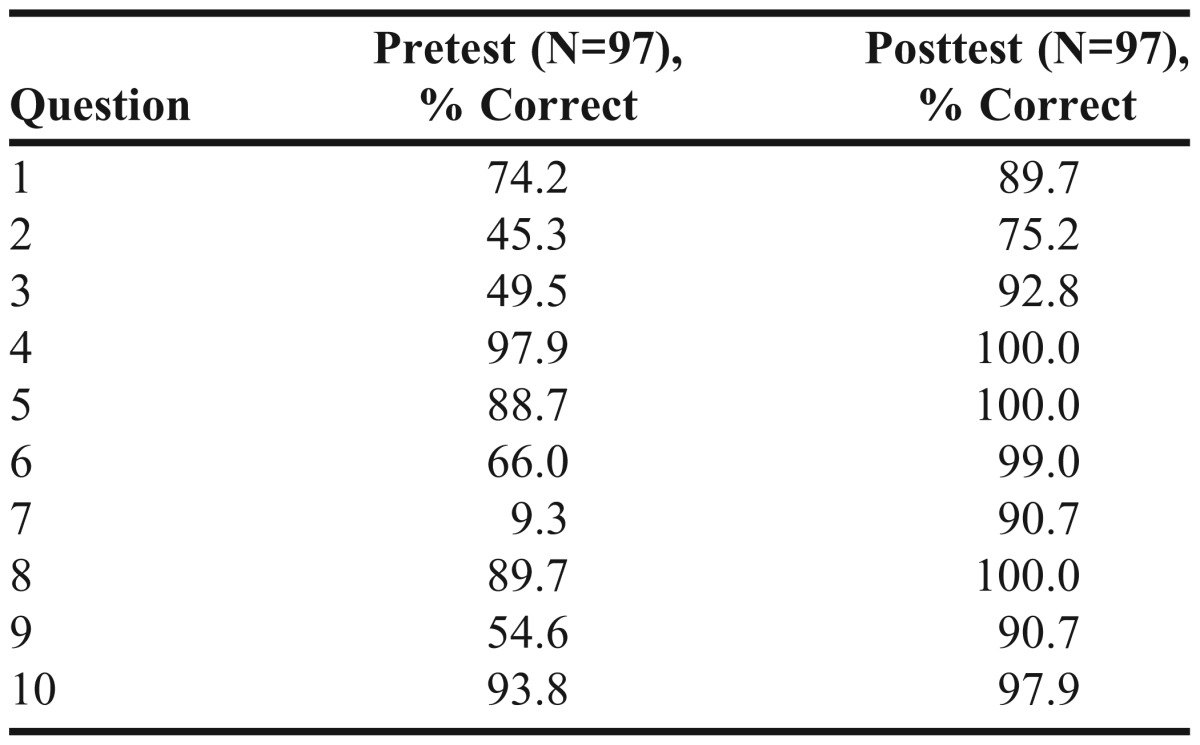
When reviewing student performance on individual questions, the percent of students correctly answering the question was highest for questions 1, 4, 5, 8, and 10. The percent of students correctly answering the question was lowest for questions 2, 3, 6, 7, and 9. In comparing pretest and posttest student performance on individual questions, student performance most improved on questions 2, 3, 6, 7, and 9, too (Table 1).
Table 1.
Student Performance on Individual Questions for Pretest and Posttest
Additionally, SOAP notes from each group were submitted for grading and used to assess overall application of materials. SOAP notes were graded based on a rubric, and each SOAP note was worth 10 points. The mean average score on the SOAP notes for the health literacy case exercise was 10.
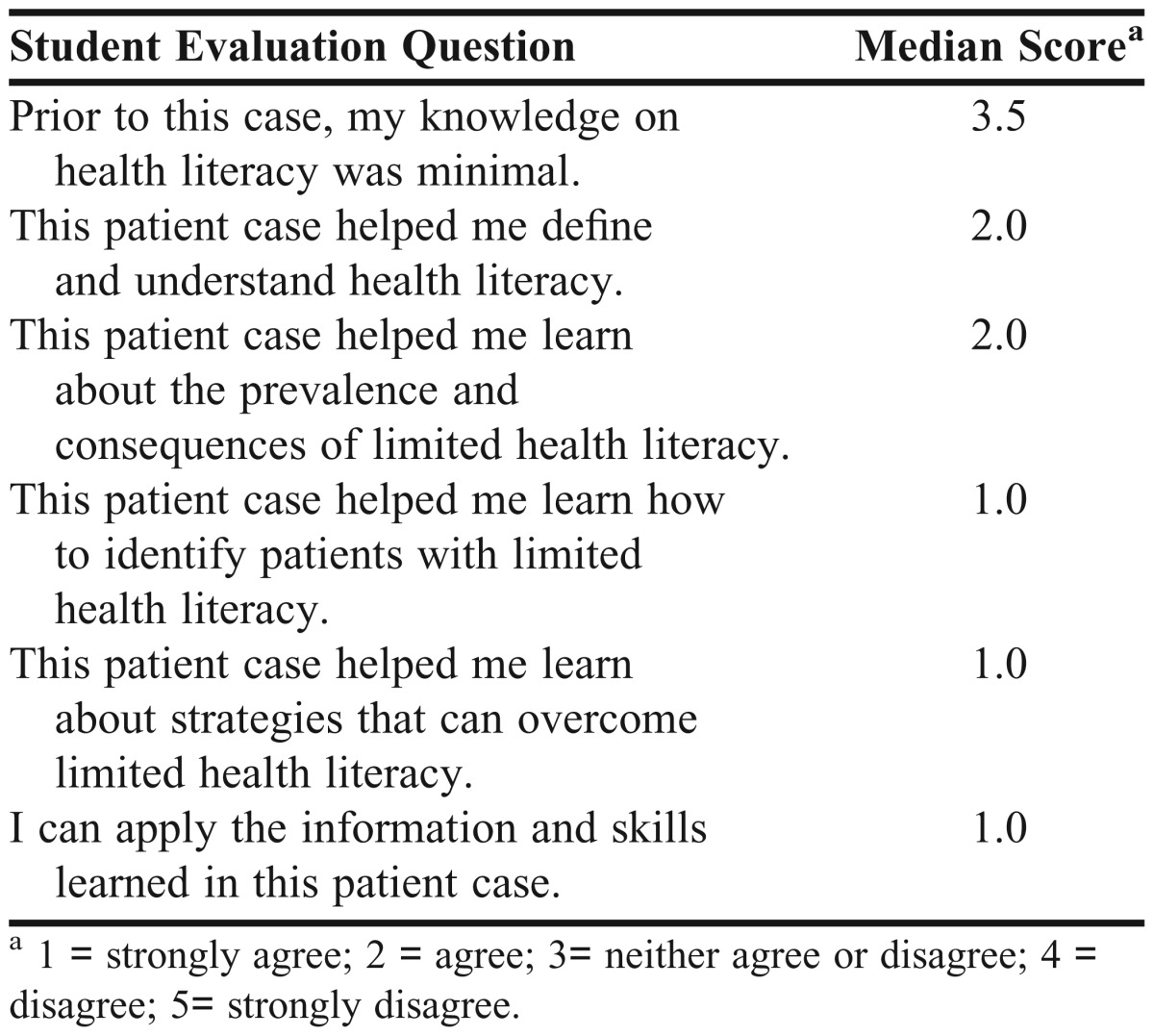
Student evaluations also were completed to assess student perception on the effectiveness of the health literacy case exercise in teaching the expected learning objectives (Table 2). The scale used for student evaluation questions ranged from 1 (strongly agree) to 5 (strongly disagree). Ninety-six of 97 students completed the evaluation. Overall, 44.3% of students disagreed, 22.6% neither agreed nor disagreed and 22.6% agreed that their knowledge on health literacy was minimal (Table 1). All students either strongly agreed or agreed that the patient case was effective in teaching the defined learning objectives. Students also strongly agreed that they would be able to apply the information and skills from the case-based exercise to practice.
Table 2.
Results for Student Evaluations on Health Literacy Case-Based Learning Exercise
DISCUSSION
Case-based learning is commonly used in health professions education. Although it appears to be an effective educational tool, Thistlethwaite and colleagues found that there is little objective data in the literature to support the efficacy of case-based learning in health professions education.10 From their review of 104 papers on case-based learning in health professional training programs, they found there was no consensus among colleges and schools on the definition of case-based learning, that different methodologies were used to administer case-based learning, and that there was evidence from student feedback that students enjoy and learn from case-based learning. Based on studies specific to case-based learning in pharmacy education, student feedback is the most commonly used method of assessment.13-16 Although student feedback is a frequently used and acceptable tool for assessment of learning, it is a subjective measure that can be susceptible to bias as students may rate a learning activity based on personal preference regarding a topic or even the instructor. Smits and colleagues compared case-based learning and traditional text-based learning in medical education and found no difference in student knowledge between the 2 teaching methods.11 Another study evaluating the efficacy of case-based computer modules did find improvements in short-term knowledge, but the improvement was not maintained longterm.12 In pharmacy education, Romero and colleagues reported enhanced student learning in a pharmaceutics course that used case-based learning, but the observation was based on a positive correlation between case study grades and course examination scores.21 Brown and colleagues found that students who completed a case-based toxicology elective course performed better on the toxicology subsection of the Pharmacy Curriculum Outcomes Assessment examination than students who had not completed the course.22 One study that assessed the efficacy of case-based learning by comparing pretest and posttest scores and overall pharmacology examination scores found that students’ posttest scores and examination scores significantly improved.23 Based on these limited studies, case-based learning appeared to increase student knowledge, but there is still a need for strong objective evidence.
For our Applied Pharmacy Care V course, case-based learning was added to provide pharmacy students with real-life cases to prepare them for clinical practice. We evaluated the efficacy of case-based learning in teaching basic health literacy concepts and pharmacist skills using both objective test scores and subjective student feedback. Posttest scores were significantly higher, demonstrating that cased-based learning allowed students to gain knowledge and skills on health literacy. This provides evidence that the case-based exercise was effective in teaching students the defined learning objectives. Based on their performance on the pretest, students appeared to have proficient baseline knowledge in basic health literacy concepts and baseline skills in designing strategies used to overcome limited health literacy. In contrast, pretest scores demonstrated that students had poor baseline skills in identifying risk factors for limited health literacy, recognizing common signs for limited health literacy, and poor baseline knowledge on the impact of limited health literacy. Based on posttest scores, students had considerable improvement in these areas, thus demonstrating that the case-based exercise was effective in teaching the learning objectives. Mean average SOAP note grades from this health literacy case were generally higher than average SOAP note grades for other patient case topics, probably because of the creative nature of the treatment or “Plan” portion for this case. For this case, students were encouraged to be more innovative and allowed to explore different options when designing a plan to help their patients with health literacy problems. The treatment for cases involving an actual disease state is more objective, and involves more specific drug therapy and evidenced-based medicine. Grading for such is much more technical and stringent.
Feedback from student evaluations on the exercise was positive. Although most students perceived that they had baseline knowledge on health literacy, students felt that the case-based learning exercise did effectively teach them the defined learning objectives. Most importantly, students believed they would be able to apply basic health literacy concepts and skills learned in the exercise to practice.
With the updated ACPE requirements for the inclusion of health literacy in pharmacy school curricula, it will be imperative for pharmacy colleges and schools to consider various methods for incorporating health literacy education.6 Published literature discusses some strategies including: (1) a required course on health literacy that includes lectures and active-learning strategies; and (2) short modules on health literacy that involve lecture and active-learning sessions incorporated into an established, relevant course (eg, a communications or cultural competency course).7-9 In our curriculum, we expanded health literacy education by incorporating a health literacy patient case into an established case-based learning laboratory. Because we found that the patient case exercise was effective in teaching, we will likely continue to use it as a teaching tool for health literacy in our curriculum.
This study had several limitations. First, because informed consent was obtained prior to the study, students were aware that the health literacy case exercise was part of a study. This may have influenced their performances on pretests, posttests, and SOAP note writing. Also, the pretest and posttest examinations administered were not validated tools. Because the tests were conducted anonymously, we were not able to match a student’s pretest and posttest and thereby analyze improvements in individual performance. Without pairing the data, we cannot be sure that every student’s posttest score improved. Additionally, this study involved only P3 pharmacy students, making it difficult to generalize the study results to all pharmacy and health professions students.
SUMMARY
We increased health literacy education in the pharmacy curriculum by incorporating a health literacy patient case into a case-based learning laboratory. The primary objective was to evaluate the efficacy of case-based learning in teaching basic health literacy concepts and pharmacist skills in managing patients with limited health literacy. Students gained knowledge and skills in health literacy. The case-based exercise also was effective in having students achieve the learning objectives. Students felt they achieved the learning objectives and believed they would be able to apply basic health literacy concepts and skills learned in practice. Pharmacists can play a pivotal role in identifying patients with limited health literacy and educating them about their diseases and medications; thus, it is vital to incorporate and expand health literacy education in the pharmacy curriculum.
ACKNOWLEDGEMENTS
The authors thank the following pharmacy students who helped with data analysis: Maureen Ezeh, David Wilson, Stephanie Folts, and Priya Jassal. Additionally, the authors extend special appreciation to Dr. David Fike who assisted with statistical analysis.
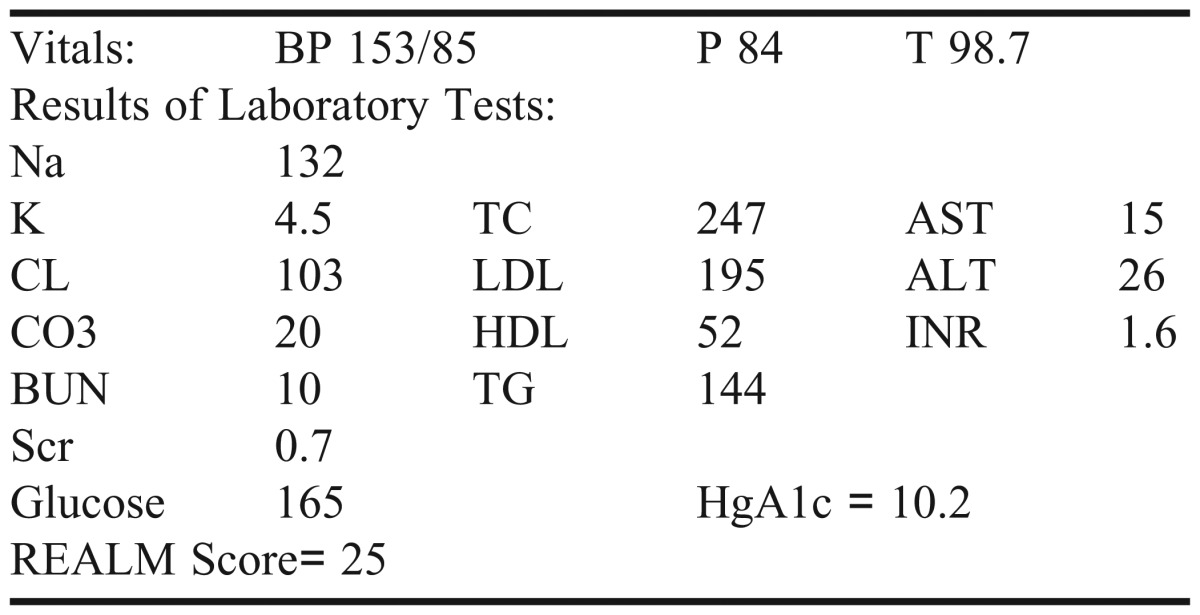
Appendix 1. Health literacy patient case and case-guided questions.
CC: I am not sure why I am here.
HPI: JG is a 66 yo Hispanic female who is referred to your MTM Clinic for medication education. Per her physician’s records, JG frequently misses doctor appointments and fails to take her medications consistently. She reports that she knows her medications and often uses the pill color to help her. You ask her to read the medication labels on her prescription bottles, but she replies, “I need my glasses.” All her prescription bottles are old and outdated (You notice that each bottle is marked with different letters in different colors). Per her medication refill history, she is frequently late in refilling her prescriptions.
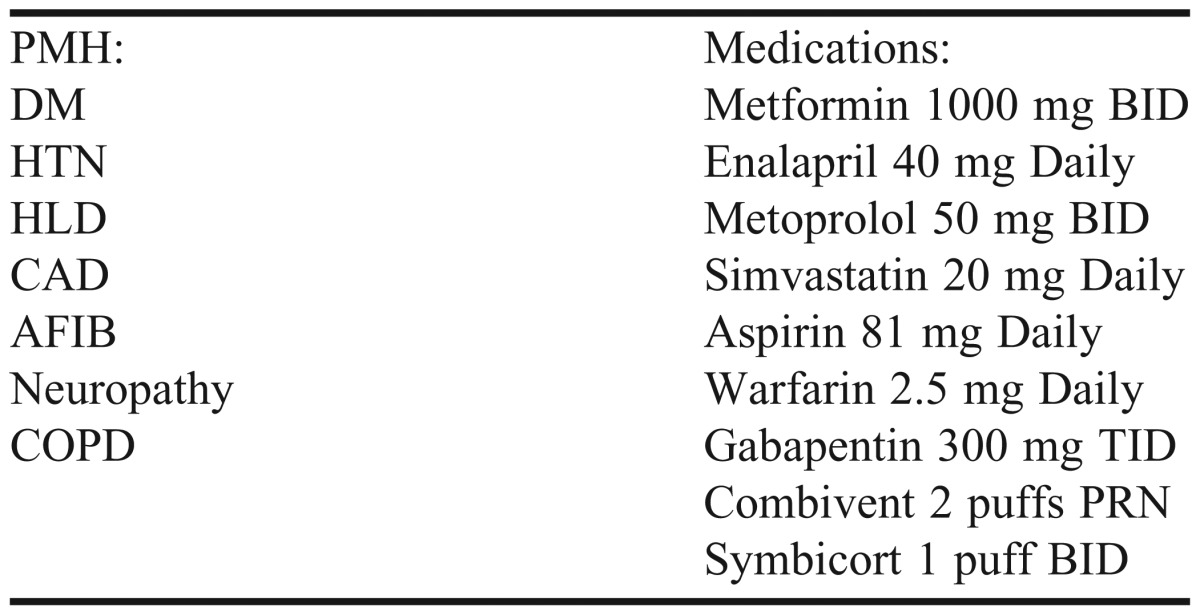
SH: Highest level of education – 7th grade, lives with her sister; Her primary language is Spanish, but she speaks English
FH: Noncontributory
Problems:
Medication Education for patient with limited health literacy
Case: Health Literacy
Case-Guided Questions
1. Define health literacy.
2. What percent of the population have limited health literacy?
3. What patient characteristics put JG at risk for limited health literacy?
4. What common signs suggest that JG may have low health literacy?
5. What is the REALM? What other tests are available? Based on JG’s REALM score, what is her literacy level?
6. What reading level is most health information written at? What is the average reading level for adult Americans?
7. What potential effects could low literacy have on JG’s health status or outcomes?
8. What potential effects could low health literacy have on JG’s ability to take her medications?
9. What strategies can help improve JG’s ability to take her medications?
Appendix 2. Pretest and posttest questions.
1. True or False: Health literacy is the ability to read or write
- 2. Which of the following groups are at high risk for low health literacy? Select all that apply
- a. Minorities
- b. Age greater than 65
- c. Have less than a high school diploma
- d. Medicaid patients
- 3. Which of the following are common signs that patients with low health literacy might display? Select all that apply
- a. Have difficulty following instructions
- b. Commonly late in refilling medications
- c. Does not ask questions for clarification
- d. Fails to show up for appointments
4. True or False: When picking up refills, patients with limited health literacy may ask the pharmacist for the old bottles because they depend on their personal markings to identify the medication.
5. True or False: The REALM test can be used to assess the health literacy of a patient.
6. True or False: Patients with poor health literacy have less knowledge about their diseases.
- 7. What level is most health information is written at?
- a. 6th – 8th grade level
- b. 9th- 10th grade level
- c. 11th-12th grade level
- d. None of the above
8. True or False: Many studies show that most health information is written at the appropriate level.
- 9. Patients with poor health literacy: Select all that apply
- a. are unable to identify their own medications
- b. may have difficulty using MDI
- c. are less likely to be adherent to their medication regimens
- d. None of the above
- 10. Which of the following strategies can help overcome limited health literacy? Select all that apply
- a. Take the time to verbally counsel patients
- b. Use medical terminology when speaking to patients
- c. Use pictures
- d. None of the above
REFERENCES
- 1.Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 2.Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006–483). Washington, DC: National Center for Education Statistics; 2006. US Dept. of Education. [Google Scholar]
- 3.Berkman ND, DeWalt DA, Pignone MP, et al. Literacy and Health Outcomes. Evidence Report/Technology Assessment No. 87. Rockville, MD: Agency for Health Care Research and Quality; 2004. AHRQ Publication No. 04-E007-2 US Dept. of Health and Human Services. [Google Scholar]
- 4.Kripalani S, Weiss BD. Teaching about health literacy and clear communication. J Gen Intern Med. 2006;21(8):888–890. doi: 10.1111/j.1525-1497.2006.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Praska JL, Kripalani S, Antoinette SL, Jacobson T. Identifying and assisting low-literacy patients with medication use: a survey of community pharmacies. Ann Pharmacother. 2005;39(9):1441–1445. doi: 10.1345/aph.1G094. [DOI] [PubMed] [Google Scholar]
- 6.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Adopted. January, 15, 2006. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed May 31, 2012. [Google Scholar]
- 7.Sicat BL, Hill LH. Enhancing student knowledge about the prevalence and consequences of low health literacy. Am J Pharm Educ. 2005;69(4):Article 62. [Google Scholar]
- 8.Devraj R, Butler LM, Gupchup GV, Poirier TI. Active learning strategies to develop health literacy knowledge and skills. Am J Pharm Educ. 2010;74(8):Article 137. doi: 10.5688/aj7408137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poirier TI, Butler LM, Devraj R, Gupchup GV, Santanello C, Lynch JC. A cultural competency course for pharmacy students. Am J Pharm Educ. 2009;73(5):Article 81. doi: 10.5688/aj730581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thistlethwaithe JE, Davies D, Ekeocha S, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No.23. Med Teach. 2012;34(6):e421–e444. doi: 10.3109/0142159X.2012.680939. [DOI] [PubMed] [Google Scholar]
- 11.Smits PB, de Graaf L, Radon K, et al. Case-based e-learning to improve the attitude of medical students towards occupational health, a randomized controlled trial. Occup Environ Med. 2012;69(4):280–283. doi: 10.1136/oemed-2011-100317. [DOI] [PubMed] [Google Scholar]
- 12.Mounsey A, Reid A. A randomized controlled trial of two different types of web-based instructional methods: one with case-based scenarios and one without. Med Teach. 2012;34(9):e654–e658. doi: 10.3109/0142159X.2012.689442. [DOI] [PubMed] [Google Scholar]
- 13.Sims P. Utilizing the peer group method with case studies to teach pharmaceutics. Am J Pharm Educ. 1994;58(1):78–81. [Google Scholar]
- 14.Sims P. Utilizing the peer group method with case studies to teach pharmacokinetics. Am J Pharm Educ. 1994;58(1):73–77. [Google Scholar]
- 15.Popovich N, Wood OB, Brooks LA, Black DR. An elective, interdisciplinary health care case studies course. Am J Pharm Educ. 2000;64(4):363–371. [Google Scholar]
- 16.Currie BL, Chapman RL, Christoff JJ, Sikorski L. Patient-related case studies in medicinal chemistry. Am J Pharm Educ. 1994;58(4):446–450. [Google Scholar]
- 17.University of the Incarnate Word. Student Handbook and Academic Catalog. San Antonio, TX: Feik School of Pharmacy; 2008. Feik School of Pharmacy. [Google Scholar]
- 18.Office of Disease Prevention and Health Promotion. Quick Guide to Health Literacy. Washington, DC: US Department of Health and Human Services; http://www.health.gov/communication/literacy/quickguide/. Accessed July, 1, 2012. [Google Scholar]
- 19.Weiss BD. Health Literacy and Patient Safety: Help Patients Understand, Manual for Clinicians. Chicago, IL: American Medical Association Foundation; 2007. 2nd. [Google Scholar]
- 20.Bazaldua OV, Kripalani S. In: Chapter 3. Health Literacy and Medication Use. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. Talbert RL, DiPiro JT, Matzke GR, Yee GC, Wells BG, Posey LM, editors. Vol. 2011. New York, NY: The McGraw Hill Companies; http://accesspharmacy.com/content.aspx?aid=7965616.Accessed July, 20, 2012. [Google Scholar]
- 21.Romero RM, Eriksen SP, Haworth IS. A decade of teaching pharmaceutics using case studies and problem-based learning. Am J Pharm Educ. 2004;68(2):Article 31. [Google Scholar]
- 22.Brown SD, Pond BB, Creekmoore KA. A case-based toxicology elective course to enhance student learning in pharmacotherapy. Am J Pharm Educ. 2011;75(6):Article 118. doi: 10.5688/ajpe756118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herrier RN, Jackson TR, Consroe PF. The use of student-centered, problem-based, clinical case discussions to enhance learning in pharmacology and medicinal chemistry. Am J Pharm Educ. 1997;61(4):441–446. [Google Scholar]


