Abstract
Objective. To quantify, describe, and categorize patient drug-related problems (DRPs) and recommendations identified by fourth-year (P4) student pharmacists during a live medication reconciliation activity within a patient-centered medical home (PCMH).
Methods. Fourth-year student pharmacists conducted chart reviews, identified and documented DRPs, obtained live medication histories, and immediately provided findings and recommendations to the attending physicians. Documentation of DRPs and recommendations were analyzed retrospectively.
Results. Thirty-eight students completed 99 medication reconciliation sessions from June 2011 to October 2012 during their advanced pharmacy practice experience (APPE). The students obtained 676 patient medication histories and identified or intervened on 1308 DRPs. The most common DRPs reported were incomplete medication list and diagnostic/laboratory testing needed. Physicians accepted 1,018 (approximately 78%) recommendations.
Conclusion. Student pharmacists successfully identified and reduced DRPs through a live medication reconciliation process within an academic-based PCMH model. Their medication history-taking skills improved and medication use was optimized.
Keywords: student pharmacist, medication reconciliation, patient-centered medical home, drug-related problems, adverse drug effects, primary care
INTRODUCTION
There are approximately 1 billion visits to physician offices annually in the United States, and 80% of those visits result in at least 1 medication prescription.1,2 Inaccurate medication profiles subject patients to DRPs and potential adverse drug events (ADEs).2 Drug-related problems are defined as “any circumstance related to the patient’s use of a drug that actually or potentially prevents the patient from gaining the intended benefit of the drug,” while ADEs are defined as “the injuries that result from a medical intervention caused by a DRP.”3,4 Approximately 25% of all outpatients who received at least 1 prescription medication experienced an ADE within the subsequent 3 months. Approximately 60% of drug-related hospital admissions are considered preventable.5-7 Additionally, the costs associated with ADEs exceed the costs of the medications themselves.8 Despite electronic documentation, an estimated 60% of outpatient medication records still contain discrepant information.9 Identifying and resolving DRPs before ADEs occur is critical to improving patient safety and minimizing medical costs.
The PCMH model is a comprehensive approach to improving the delivery of primary care that involves 6 core principles: personal physician, physician-directed medical practice, whole-person orientation, coordinated and integrated care, quality and safety, enhanced access, and payment that recognizes added value.10,11 The role for pharmacists functioning within a PCMH model continues to evolve.12,13 As health reform continues, integrating comprehensive medication management into primary care practices will be mandatory to optimize patient outcomes.14 As part of medical home teams, pharmacists have been effective in achieving desired treatment goals and resolving drug-therapy problems, particularly for patients with chronic conditions. Johnson and colleagues reported reductions in body mass index, blood pressure, and A1C and cholesterol levels in 222 patients with diabetes and an A1C level greater than 9% who were referred to comprehensive pharmacy services, compared to 262 patients who received standard care in a safety-net clinic medical home for uninsured patients.15 Edwards described a feasible and effective method to completing diabetes-related standards of care through a planned visit with a pharmacist within a PCMH.16 Isetts reported that 40% of diabetic patients in the team-based sites involving pharmacists met the 5 diabetes performance-related treatment goals compared to only 17% of patients in a statewide group. More than 4,000 DRPs were resolved within a 15-month study period.17
For pharmacists to remain effective in reducing DRPs and optimizing medication outcomes, appropriate training in multidisciplinary, interprofessional healthcare settings must be provided for student pharmacists. The American Association of Colleges of Pharmacy supports practice models that promote safe medication practices as the standard of care in all practice settings.18 The academic-based PCMH setting has been described as the ideal model for training the next generation of pharmacists because PCMH credentialing requires significant optimization of medication regimens to improve clinical outcomes.19 Most studies have evaluated students’ medication history-taking skills in the acute care setting and through simulation. Few studies have addressed student pharmacists’ abilities to reduce DRPs through a live medication reconciliation process specifically in an academic-based PCMH model.20 The primary objective of this study was to quantify, describe, and categorize DRPs identified by student pharmacists as part of a medication history-taking activity conducted in an academic-based PCMH. The secondary objective was to describe and quantify recommendations made from DRPs identified, and to report the percentage of recommendations accepted by the attending physician.
METHODS
Participants were P4 student pharmacists in a required ambulatory care practice experience at the Family Medicine Center, a family medicine-based, free-standing outpatient clinic, between June 1, 2011, and October 31, 2012. This Institutional Review Board-approved study did not exclude student participants. It only excluded patient medication history documentation that was illegible or incomplete.
The medication reconciliation activity was added to an existing APPE within the Pharmacotherapy Service at the Family Medicine Center. Attending physicians each covered 2 examination rooms and saw 12 to 15 patients per half-day session. The students used a computer for electronic medical record (EMR) access. This activity consisted of P4 students conducting a patient chart review, identifying and documenting DRPs, and creating medication action plans after meeting with a pharmacist preceptor. Students spent an average of 3 to 4 hours conducting chart reviews, depending on patient load and knowledge base. The pharmacist preceptor spent approximately 1.5 to 2 hours reviewing 1 clinic session assignment. Following preceptor review, the P4 student pharmacists obtained live medication histories and immediately provided findings and recommendations to the attending physician before the physician-patient interaction during a morning or afternoon 4-hour clinic session.
The assessed documentation included the P4 student’s tracking form (paper form or Excel spreadsheet) and the attending physician’s electronically signed EMR notes. The following data were collected: number and type of DRPs found, number and type of recommendations made, and number and type of recommendation accepted by the attending physician. Data collection also included the number of students and physicians who participated, the average number of DRPs found per student, the average number of recommendations made per student, and the average percentage of recommendations accepted per student pharmacist. Published frameworks by Steven Chen and Robert Cipolle were used to categorize the DRPs, recommendations, and acceptance types.21,22 Descriptive statistics were used to describe these data.
Certain types of recommendations could be classified as specific (ie, “start famotidine 20 mg bid”) or general (ie, “start H2 blocker”). To determine if acceptance rates differed based on this variable, 2 raters categorized the recommendations to substitute a drug, add a drug, change dose, change dose interval, change duration of therapy, change “as needed” medication to scheduled, and substitute dosage form as either specific or general recommendations. The Cohen kappa was produced to evaluate inter-rater agreement. Further analysis was completed using a chi-square or Fisher exact test, as appropriate, to compare number of recommendations accepted between each pair of recommendation types, cumulative general and specific recommendations, and individual general and specific recommendations by recommendation type. All analyses were performed using SAS, version 9.3 (SAS Institute, Cary, NC) with an a priori level of significance α=0.05.
RESULTS
From June 2011 to October 2012, 38 P4 student pharmacists in an 8-week ambulatory care practice experience completed 99 live medication reconciliation sessions at the patient-centered medical home. Six attending physicians participated in the project. The student pharmacists performed 676 medication histories with 1308 DRPs identified and interventions made (Table 1). Less than 10 medication histories were excluded because of ineligible or incomplete documentation.
Table 1.
Summary of Fourth-Year Student Pharmacists’ Medication Reconciliation Activity in a Patient-Centered Medical Home
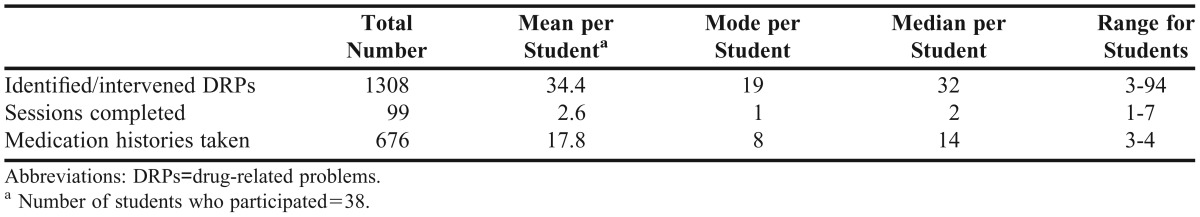
The mean number of patients seen per student was approximately 18 over an average of 3 clinic sessions per student. The number of patients seen per student ranged from 3 to 45. The number of sessions per student ranged from 1 to 7 during the 8-week practice experience. The number of DRPs identified or interventions made ranged from 3 to 94 with an average of 35 DRPs per student (Table 1).
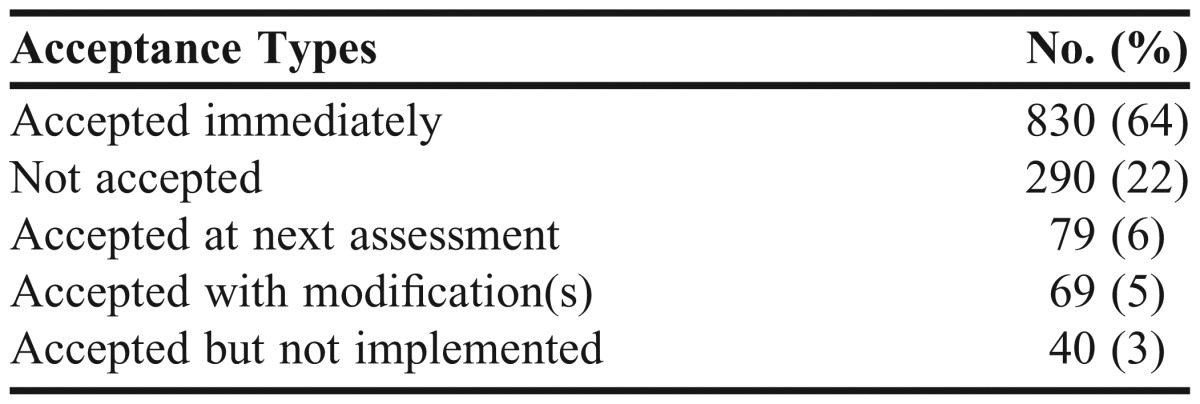
Seventy-eight percent (1018/1308) of the students’ recommendations were accepted by the attending physicians during the live medication reconciliation session. Attending physicians accepted 830 (64%) of the recommendations immediately. They accepted some recommendations with modifications by the physician (5%; 69/1308). Seventy-nine (6%) recommendations were accepted at the next patient assessment and 40 (3%) were accepted but not implemented because of patient preference. Only 290 (22%) of the student pharmacist’s recommendations were not accepted at all (Table 2).
Table 2.
Acceptance Types of Student Pharmacist Recommendations (N=1308)
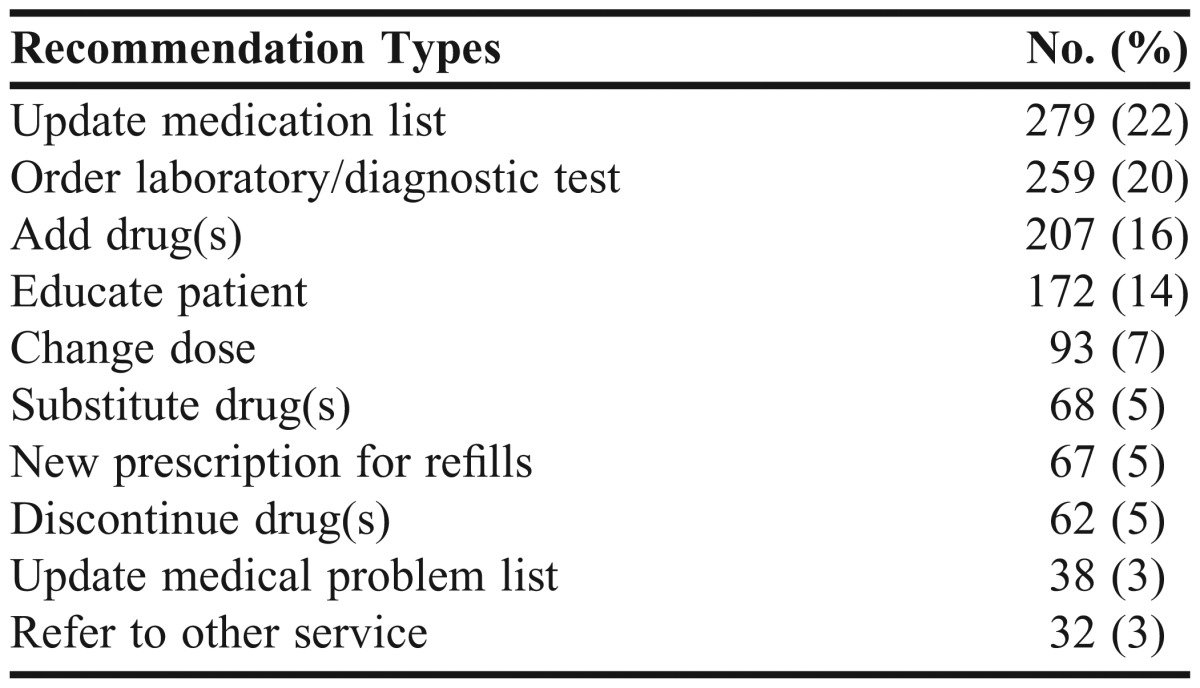
The most common DRPs found were incomplete medication list, with 259 reported instances, and diagnostic/laboratory testing needed, with 254 reported instances. These 2 categories made up 23% of all problems identified. As a result, the most common recommendations made were to update a medication list and order testing with 280 (22%) and 259 (20%) recommendations, respectively. Notably, 197 (17%) of the DRPs identified were under/suboptimal treatments and 100 (9%) were inappropriate use of medications (misuse/not taking as directed). There were 207 (16%) recommendations made to add a new medication and 172 (14%) recommendations made for patient education on appropriate medication use. Table 3 and Table 4 illustrate the top 9 most common DRPs identified and the top 10 recommendations made.
Table 3.
Top 9 Patient Drug-Related Problems Found by Student Pharmacists, (N=1308)
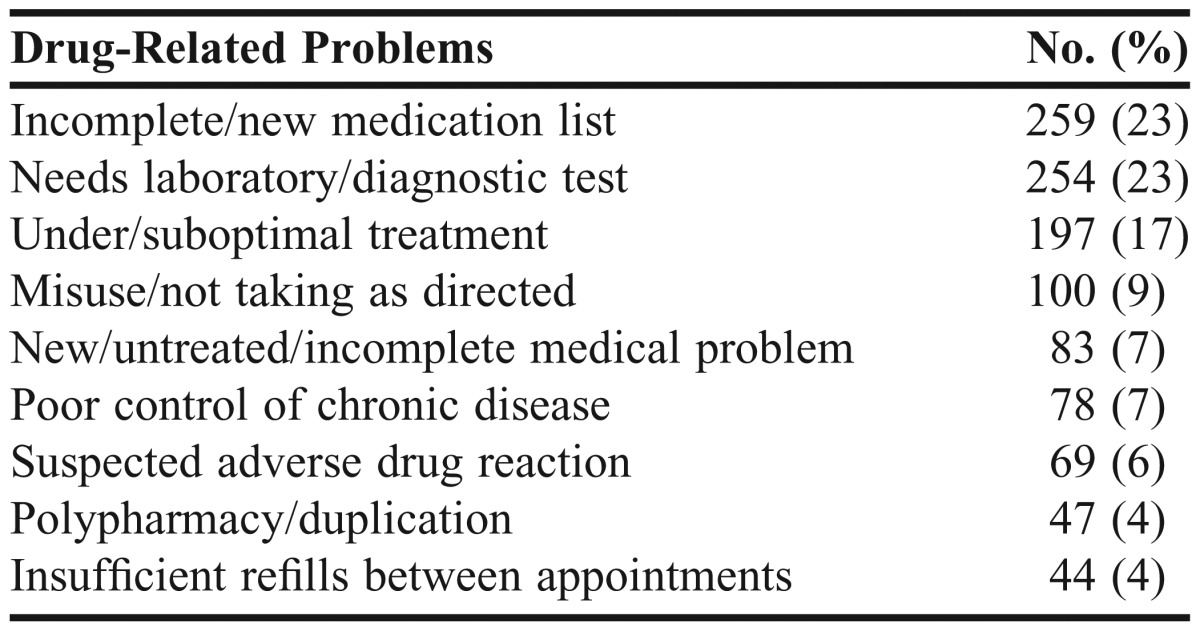
Table 4.
Top 10 Student Pharmacist Recommendations for Patient Drug-Related Problems (N=1308)
Chi-square analyses of the acceptance rates based on recommendation type were performed among all recommendations. No clinical significance could be derived from recommendations made fewer than 10 times, so these were excluded from the analysis. The recommendation to educate patients on medication use had a higher rate of acceptance compared to all other recommendation types made (99.4%), followed by the recommendation to provide a new prescription for refills (94%). A significant difference was found between each of these 2 recommendation types and all others (Table 5).
Table 5.
Acceptance Rates of Student Pharmacist Recommendations Based on Recommendation Category
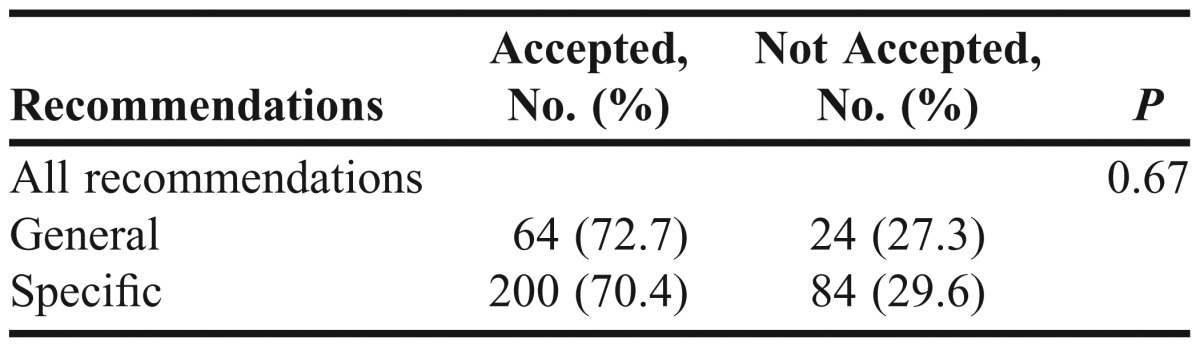
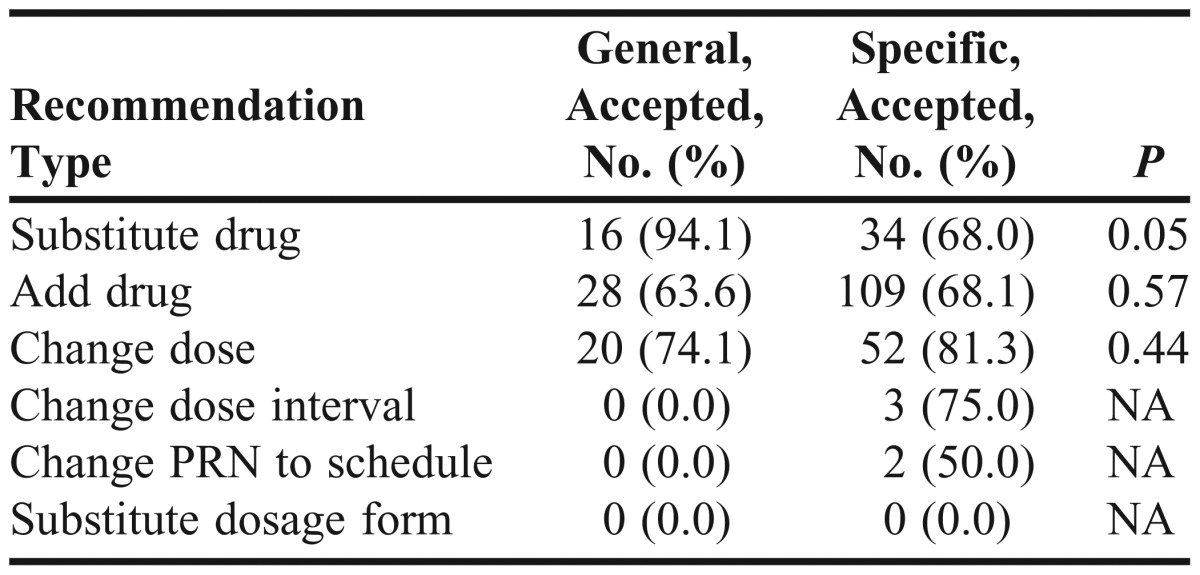
There were 380 recommendations to substitute a drug, add a drug, change dose, change dose interval, change duration of therapy, change PRN medication to scheduled, or substitute dosage form. There were no recommendations to change duration of treatment; therefore, this specific recommendation is not described. Recommendations to change dose interval, change PRN to scheduled, and substitute dosage form were included in the comparison between general and specific acceptance rates among all recommendations, but each had fewer than 10 observations, so they were not analyzed individually based on lack of potential clinical significance. Of the 380 recommendations, 8 were not categorized as general or specific because of incomplete or unclear documentation, leaving 372 recommendations that were further classified as general or specific (Table 6). There was perfect inter-rater agreement between classifications of recommendations as general or specific (k=1.0). Although 72.7% of all general recommendations were accepted compared to 70.4% of specific recommendations, no significant difference was detected between the 2 (p=0.67). Additionally, there were no significant differences observed when comparing percent accepted between specific and general recommendations for individual recommendation types (substitute drug, p=0.05; add drug, p=0.57; change dose, p=0.44; other recommendation types not included in analysis as observed cell counts were too low to measure significance) (Table 7).
Table 6.
Acceptance Rates Based on Nature of Recommendations and Recommendation Type
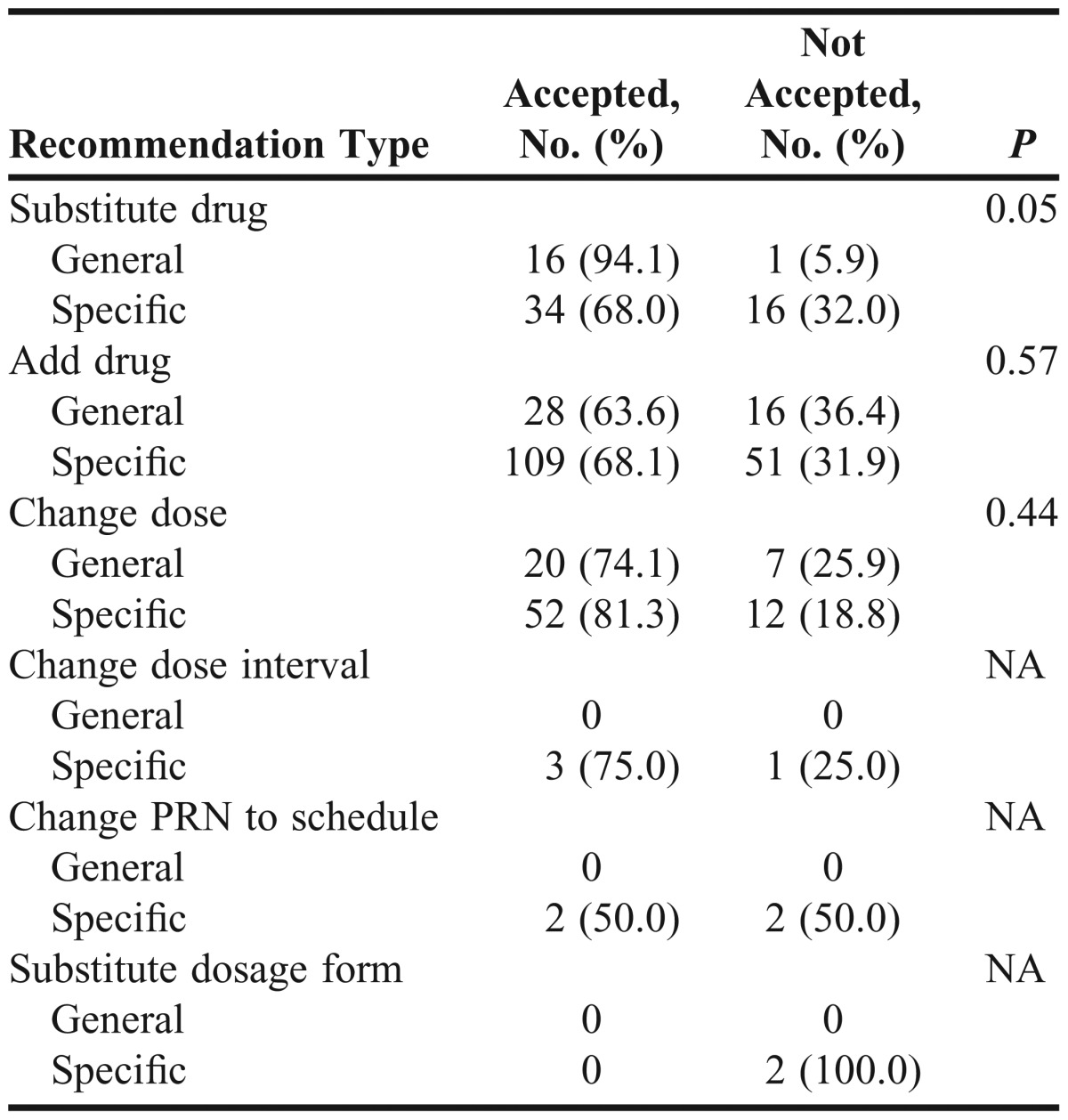
Table 7.
Acceptance Rate by Category for Each Recommendation Type
DISCUSSION
With over 1300 DRPs identified by student pharmacists over a 17-month period and a 78% acceptance rate of recommendations to resolve these DRPs, an APPE medication history-taking activity with physician collaboration was an effective method in identifying DRPs and preventing potential ADEs. This was the largest study to date to describe this type of student pharmacist involvement specifically in an academic-based PCMH setting.
The 2 types of recommendations accepted more often than any other was to educate the patient on proper medication use and provide prescription refills. This is likely because of the limited time and effort required for a physician to address these, whereas with the other recommendations, additional clinical factors must be considered and time becomes a factor. Priority of each recommendation must also be considered. Education on proper medication use is essential to optimize medication efficacy, and therefore safety is likely considered a high priority. In addition, refills are automatically of high priority as any treatment will necessarily cease if medication is not available as needed. Although no significant difference in acceptance rates was identified between general and specific recommendations, suggesting general recommendations are accepted at the same rate as specific, students must strive to optimize medication regimens with the intent to improve outcomes, not solely to make recommendations that physicians will accept, which was the intent of this activity.
This activity also supported Center for the Advancement of Pharmaceutical Education recommendations that student pharmacists train in multidisciplinary, interprofessional healthcare settings. By conducting medication reconciliation activities in an academic-based, primary care PCMH model, students learned to manage medications for both acute and chronic conditions for all patients regardless of age, race, gender, or ethnicity. Students had more intentional physician interactions during live patient care encounters, and students’ confidence in crafting and executing a therapeutic recommendation increased.
One study that evaluated the impact of student pharmacists’ ability to intervene on DRPs found 75% of recommendations made to the physician were accepted, while a second study found that only 32% of recommendations were accepted.23,24 Recommendations were done through the patient or via fax; therefore, lower rates of accepted recommendations were likely a reflection of the indirect communication with physicians. Abdelhalim and Lundquist measured the acceptance rates of recommendations made by students who had direct contact with attending physicians in the primary care setting.25,26 Acceptance rates by attending physician were 93.8% and 88.6%, respectively. These findings, along with our results, provide further evidence that direct interaction with physicians in a live environment may be the most effective method in which to resolve drug-related problems in an outpatient setting.
A limitation of this study was inconsistent student documentation of the medication reconciliation activity. A universal worksheet was not provided; therefore, each student organized patient information and notes from the live interview differently to complete a final medication recommendation form. Moreover, clinical outcomes were not addressed. While the impact of the student pharmacists’ interventions was not determined, the direct student-physician interaction promoted a multidisciplinary approach to patient care with a focus on optimizing drug therapy. The student pharmacists were able to identify DRPs and provide interventions; which reduced the amount of DRPs that could have led to clinically significant ADEs.
CONCLUSIONS
The student pharmacists successfully identified and reduced DRPs during their APPE in the PCMH setting. An intentional live medication reconciliation activity can prevent potential ADEs by addressing and resolving DRPs. This study offers a framework for other institutions to support an APPE activity that allows student pharmacists to improve their medication history-taking skills through an integrated care approach.
ACKNOWLEDGEMENTS
The authors thank Dr. Ashley Chasse and Dr. Debbie Leung for their participation in data collection for the project. Dr. Chasse and Dr. Leung were P4 student pharmacists who completed an APPE research practice experience during the time of the study.
REFERENCES
- 1.Centers for Disease Control and Prevention. FastStats A to Z. National Ambulatory Medical Care Survey: 2010 summary tables. http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. Accessed May 28, 2013.
- 2.Centers for Disease Control. Ambulatory medical care utilization estimates for 2007. Vital and Health Statistics. Series 13, No. 169. http://www.cdc.gov/nchs/data/series/sr_13/sr13_169.pdf. Published April 2011. Accessed December 19, 2012.
- 3.Van Mil JF, Westerlund LT, Hersberger KE, Schaefer MA. Drug-related problem classification systems. Ann Pharmacother. 2004;38(5):859–867. doi: 10.1345/aph.1D182. [DOI] [PubMed] [Google Scholar]
- 4.Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA. 1995;274(1):29–34. [PubMed] [Google Scholar]
- 5.Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348(16):1556–1564. doi: 10.1056/NEJMsa020703. [DOI] [PubMed] [Google Scholar]
- 6.Winterstein AG, Sauer BC, Hepler CD, Poole C. Preventable drug-related hospital admissions. Ann Pharmacother. 2002;36(7/8):1238–1248. doi: 10.1345/aph.1A225. [DOI] [PubMed] [Google Scholar]
- 7.McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36(9):1331–1336. doi: 10.1345/aph.1A333. [DOI] [PubMed] [Google Scholar]
- 8.Smith DL. The effect of patient non-compliance on health care costs. Med Interface. 1993;6(4):74–76,78,84. [Google Scholar]
- 9.Linsky A, Simon SR. Medication discrepancies in integrated electronic health records. BMJ Qual Saf. 2013;22(2):103–109. doi: 10.1136/bmjqs-2012-001301. doi: 10.1136/bmjqs-2012-001301. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Family Physicians. American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint principles of the patient-centered medical home. http://www.acponline.org/running_practice/delivery_and_payment_models/pcmh/demonstrations/jointprinc_05_17.pdf. Published March 2007. Accessed July 9, 2013.
- 11.Hoff T, Weller W, DePuccio M. The patient-centered medical home: a review of recent research. Med Care Res Rev. 2012;69(6):619–644. doi: 10.1177/1077558712447688. [DOI] [PubMed] [Google Scholar]
- 12.Smith M, Bates DW, Bodenheimer T, Cleary PD. Why pharmacists belong in the medical home. Health Aff (Millwood). 2010;29(5):906–913. doi: 10.1377/hlthaff.2010.0209. [DOI] [PubMed] [Google Scholar]
- 13.Berdine H, Dougherty T, Ference J, et al. The pharmacists' role in the patient-centered medical home (PCMH): a white paper created by the Health Policy Committee of the Pennsylvania Pharmacists Association (PPA) Ann Pharmacother. 2012;46(5):723–750. doi: 10.1345/aph.1R189. [DOI] [PubMed] [Google Scholar]
- 14. Patient Centered Primary Care Collaborative. The Patient-Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes. Patient-Centered Primary Care Collaborative; 2010.
- 15.Johnson KA, Chen S, Cheng I, et al. The impact of clinical pharmacy services integrated into medical homes on diabetes-related clinical outcomes. Annals Pharmacother. 2010;44(12):1877–1886. doi: 10.1345/aph.1P380. [DOI] [PubMed] [Google Scholar]
- 16.Edwards HD, Webb RD, Scheid DC, Britton ML, Armor BL. A pharmacist visit improves diabetes standards in a patient-centered medical home (PCMH) Am J Med Qual. 2012;27(6):529–534. doi: 10.1177/1062860612444304. [DOI] [PubMed] [Google Scholar]
- 17.Isetts BJ, Brummel AR, de Oliveira DR, Moen DW. Managing drug-related morbidity and mortality in the patient-centered medical home. Med Care. 2012;50(11):997–1001. doi: 10.1097/MLR.0b013e31826ecf9a. [DOI] [PubMed] [Google Scholar]
- 18.American Association of Colleges of Pharmacy. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. https://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed November 10, 2012.
- 19.Haines SL, DeHart RM, Flynn AA, et al. Academic pharmacy and patient-centered health care: a model to prepare the next generation of pharmacists. J Am Pharm Assoc. 2011;51(2):194–202. doi: 10.1331/JAPhA.2011.10158. [DOI] [PubMed] [Google Scholar]
- 20.Mersfelder TL, Bouthillier MJ. Value of the student pharmacist to experiential practice sites: a review of the literature. Ann Pharmacother. 2012;46(4):541–548. doi: 10.1345/aph.1Q544. [DOI] [PubMed] [Google Scholar]
- 21.Chen SW, O’Callaghan R, Reta AM, Johnson KA. Medication therapy management provided through a community pharmacy in collaboration with a safety net medical clinic. Final project report for the Community Pharmacy Foundation. http://www.communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_74861.pdf. Accessed June 18, 2013.
- 22.Cipolle RJ, Strand L, Morley P. Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management. 3rd edition. McGraw-Hill; 2012. Drug Therapy Problems; pp. 156–169. [Google Scholar]
- 23.Hata M, Klotz R, Sylvies R, et al. Medication therapy management services provided by student pharmacists. Am J Pharm Educ. 2012;76(3):Article 51. doi: 10.5688/ajpe76351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCollum M, Nuffer W, Ellis SL, Turner CJ. Physician acceptance of pharmacotherapy recommendations made by pharmacy students in a rural pharmacy-based diabetes care and education clinic. Am J Pharm Educ. 2009;73(2):Article 24. doi: 10.5688/aj730224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abdelhalim D, Mohundro BL, Evans JD. Role of student pharmacists in the identification and prevention of medication-related problems. J Am Pharm Assoc. 2011;51(5):627–630. doi: 10.1331/JAPhA.2011.09101. [DOI] [PubMed] [Google Scholar]
- 26.Lundquist LM, Moye PM. Resident physicians’ acceptance of pharmacy students’ pharmacotherapy recommendations during an ambulatory care advanced pharmacy practice experience. Am J Pharm Educ. 2009;73(8):Article 145. doi: 10.5688/aj7308145. [DOI] [PMC free article] [PubMed] [Google Scholar]


