Abstract
Purpose
Anatomically, the eyes and paranasal sinuses are neighboring structures and some studies have mentioned eye disease in conjunction with chronic rhinosinusitis (CRS). However, to the best of our knowledge, no prior research has investigated the risk of developing open-angle glaucoma (OAG) among CRS patients. This study aims to provide an estimated risk of developing OAG among patients with CRS by using a population-based data set in Taiwan.
Methods
This retrospective cohort study used data sourced from the ‘Longitudinal Health Insurance Database 2000'. A total of 15 642 CRS patients were included in the study cohort and 46 926 subjects were randomly extracted as a comparison cohort. A cox proportional-hazards regression analysis was performed to calculate the 5-year risk of subsequently developing OAG following a diagnosis of CRS between the study cohort and the comparison cohort.
Results
The incidence rate of developing OAG over the 5-year follow-up period was 5.45 (95% CI: 4.95–5.98) per 1000 person-years for the study cohort and 2.80 (95% CI: 2.60–3.03) per 1000 person-years for the comparison cohort. After censoring the cases that died over the 5-year period and adjusting for the factors of monthly income, geographic region, hypertension, diabetes, coronary heart disease, hyperlipidemia, and hypothyroidism the hazard ratio for developing OAG over the 5-year period for subjects with CRS to subjects without CRS was 1.73 (95% CI: 1.53–1.96).
Conclusion
We found that those subjects with CRS had a significantly higher risk of developing OAG over the 5-year follow-up period as compared with subjects without CRS.
Keywords: chronic rhinosinusitis, open-angle glaucoma, glaucoma
Introduction
Chronic rhinosinusitis (CRS) is defined as an inflammation of the paranasal sinuses with symptoms consisting of nasal blockage, obstruction, congestion, or discharge lasting for longer than 3 months.1, 2 CRS is one of the most common diseases in the otolaryngologic field, affecting between 18 and 22 million adults in the United States each year.3 In Europe, CRS also affects over 10% of the population.4 CRS has a significant adverse impact on the quality of life, health burden, and daily functioning of its sufferers.5, 6, 7
Anatomically, the eyes and paranasal sinuses are neighboring structures. Mojon et al8 found a positive correlation between the respiratory disturbance index and intraocular pressure (IOP). Purvin et al9 also demonstrated that intracranial pressure increases as a result of episodic hypoxemia and hypercapnia, thereby leading to papilledema and an increased risk of eye disease. Moreover, previous studies have presented that ostial obstructions in CRS limit airflow and cause hypoxia within the sinus cavity thus blocking mucus drainage from the sinuses leading to mucus retention and hypoxia.10, 11 CRS might also alter the normal physiologic balance and lead to hypoxia, thereby increasing the risk of developing open-angle glaucoma (OAG). However, to the best of our knowledge, no prior research has investigated the risk of developing OAG among patients with CRS. The goal of this study is to provide an estimation of risk of developing OAG among patients with CRS by using a cohort study design from a population-based data set in Taiwan.
Methods
Database
We retrieved all the subjects for this retrospective matched-cohort study from the ‘Longitudinal Health Insurance Database 2000 (LHID2000)'. Taiwan has been implementing its National Health Insurance (NHI) program since 1995 and the coverage rate has been maintained at over 96% since its implementation. The LHID2000, which was released by the Taiwan National Health Research Institute, includes all the original medical claims and registration files for 1 000 000 enrollees in the NHI program. These 1 000 000 enrollees are randomly selected from all the enrollees listed in the 2000 Registry of Beneficiaries (n=23.72 million) under the NHI program. Prior studies have demonstrated the high validity of the data from the NHI progam.2, 12
This study is exempt from a full review by the Institutional Review Board of Taipei Medical University because the LHID2000 consists of de-identified, secondary data released to the public for research purposes.
Study sample
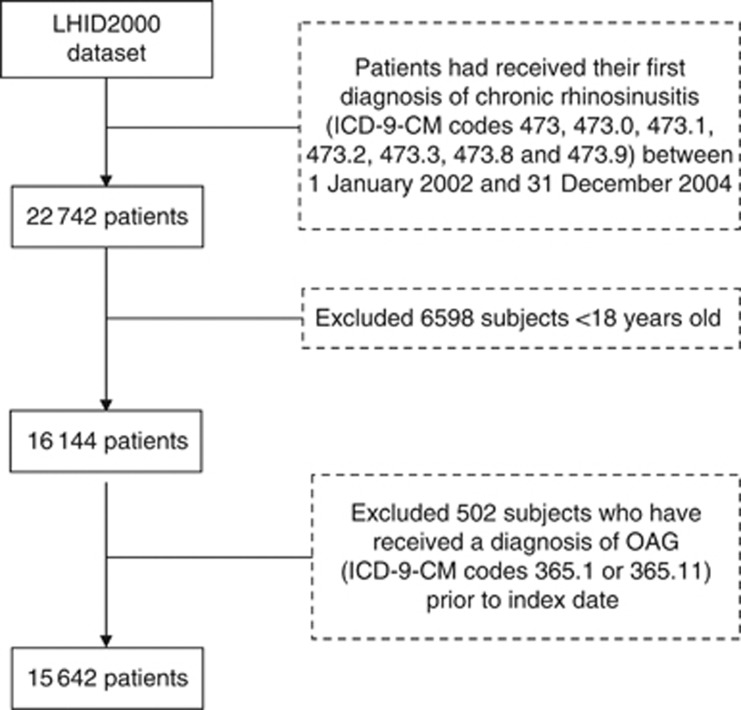
For the study cohort, we first identified 22 742 patients who had received their first diagnosis of CRS (ICD-9-CM codes 473, 473.0, 473.1, 473.2, 473.3, 473.8, and 473.9) during ambulatory care visits (including outpatient departments of hospitals or clinics) between 1 January 2002 and 31 December 2004. These cases of CRS were all diagnosed by otolaryngologists. We excluded subjects under 18 years of age (n=6598) in order to limit the study sample to the adult population. The date of the first ambulatory care visit for which the subjects were diagnosed with CRS was assigned as an index date. Subjects who received a diagnosis of OAG (ICD-9-CM codes 365.1 or 365.11) before the index date (n=502) were also excluded. As a result, 15 642 CRS patients were included in the study cohort. Figure 1 shows the selection criteria and process.
Figure 1.
Procedures of the cases selection.
The comparison cohort was also retrieved from the LHID2000. Similarly, we only selected subjects 18 years and older and excluded those subjects who had received a diagnosis of CRS since the initiation of the NHI program in 1995. We then used the SAS program proc SurveySelect (SAS System for Windows, Version 8.2; Cary, NC, USA) to randomly select 46 926 comparison subjects (three comparison subjects per study subject) to match the study subjects in terms of sex, age group (18–29, 30–39, 40–49, 50–59, 60–69, and >69 years), urbanization level (five levels, with one referring to the most urbanized and five referring to the least), and index date. The reason for matching the comparison cohort to the study cohort on this variable of urbanization was to help control for errors associated with unmeasured neighborhood socioeconomic characteristics. The index date for the study subjects was the year in which they received their first CRS diagnosis. However, the index date for the comparison subjects were simply a matched year in which the comparison subjects first used a medical service. None of the selected comparison subjects had received a diagnosis of OAG before their corresponding index date.
Study end point
All subjects in this study (n=62 568) were individually tracked for 5 years following their index date to distinguish subjects who received a subsequent diagnosis of OAG during this follow-up period. These cases of OAG were all diagnosed by ophthalmologists. Furthermore, we only included cases of OAG who received treatment with topical antiglaucoma medications in order to increase the validity of the OAG diagnoses sourced from the data set. We also censored patients who died during the 5-year period in the regression model. Of the sampled patients, 3973 died—974 from the study cohort (6.3% of study cohort) and 2999 from the comparison cohort (6.4% of the comparison cohort).
Statistical analysis
The SAS statistical package (SAS System for Windows, Version 8.2) was used to conduct all statistical analyses. χ2 tests were performed to investigate the differences in monthly income (0, NT$1-NT15 840, NT15 841-NT25 000, ≥NT25 001) and geographic location (Northern, Central, Eastern, and Southern Taiwan) as well as the medical co-morbidities (hypertension, diabetes, coronary heart disease (CHD), hyperlipidemia, and hypothyroidism) between subjects with and without CRS. We used the Kaplan–Meier method for univariate analyses to examine OAG-free survival times of baseline variables at time 0. We also used a log-rank test to compare the differences in 5-year OAG-free survival rates between the study and comparison cohorts. Furthermore, a cox proportional hazards regression analysis (stratified by sex, age group, urbanization level, and index date) was performed to calculate the 5-year estimated risk of a subsequent OAG diagnosis following a diagnosis of CRS between the study cohort and the comparison cohort. Through this study we found that the proportional hazards assumption was satisfied, as the survival curves for both strata as patients in the study cohort and comparison cohort had hazard functions that were proportional over time. The alpha level was set as P<0.05.
Results
Of the 15 642 CRS cohort subjects and 46 926 comparison subjects, the mean age was 41.5±15.3 years. After matching for sex, age group, urbanization level, and index date, no significant difference was found in monthly income or geographic region between the study and comparison cohort. This can be seen in Table 1. However, the study cohort did had a significantly higher prevalence of co-morbidities for hypertension, diabetes, CHD, hyperlipidemia, and hypothyroidism than the comparison cohort (all P<0.001).
Table 1. Demographic characteristics of subjects with chronic rhinosinusitis and comparison subjects in Taiwan (n=62 568).
| Variable |
Subjects with chronic rhinosinusitis (n=15 642) |
Comparison subjects (n=46 926) |
P value | ||
|---|---|---|---|---|---|
| Total no. | % | Total no. | % | ||
| Sex | 1.000 | ||||
| Male | 7247 | 46.3 | 21 741 | 46.3 | |
| Female | 8395 | 53.7 | 25 185 | 53.7 | |
| Age (years) | 1.000 | ||||
| 18–29 | 3874 | 24.8 | 11 622 | 24.8 | |
| 30–39 | 3862 | 24.7 | 11 586 | 24.7 | |
| 40–49 | 3424 | 21.9 | 10 272 | 21.9 | |
| 50–59 | 2250 | 14.4 | 6750 | 14.4 | |
| 60–69 | 1321 | 8.4 | 3963 | 8.4 | |
| ≥70 | 911 | 5.8 | 2733 | 5.8 | |
| Urbanization level | 1.000 | ||||
| 1 (Most urbanized) | 5288 | 33.8 | 15 864 | 33.8 | |
| 2 | 4571 | 29.2 | 13 713 | 29.2 | |
| 3 | 2648 | 17.0 | 7944 | 17.0 | |
| 4 | 1896 | 12.1 | 5688 | 12.1 | |
| 5 (Least urbanized) | 1239 | 7.9 | 3717 | 7.9 | |
| Monthly income | 0.072 | ||||
| 0 | 4315 | 27.6 | 13 224 | 28.2 | |
| NT$1–15 840 | 2489 | 15.9 | 7468 | 15.9 | |
| NT$15 841–25 000 | 5286 | 33.8 | 16 035 | 34.2 | |
| ≥NT$25 001 | 3552 | 22.7 | 10 199 | 21.7 | |
| Geographic region | 0.182 | ||||
| Northern | 7602 | 48.6 | 23 122 | 49.3 | |
| Central | 4183 | 26.7 | 12 330 | 26.3 | |
| Southern | 3520 | 22.5 | 10 381 | 22.1 | |
| Eastern | 337 | 2.2 | 1093 | 2.3 | |
| Hypertension | 3334 | 21.3 | 8076 | 17.2 | <0.001 |
| Diabetes | 1831 | 11.7 | 4238 | 9.0 | <0.001 |
| Hyperlipidemia | 2775 | 17.7 | 6261 | 13.3 | <0.001 |
| Coronary heart disease | 1844 | 11.8 | 3737 | 8.0 | <0.001 |
| Hypothyroidism | 143 | 0.9 | 182 | 0.4 | <0.001 |
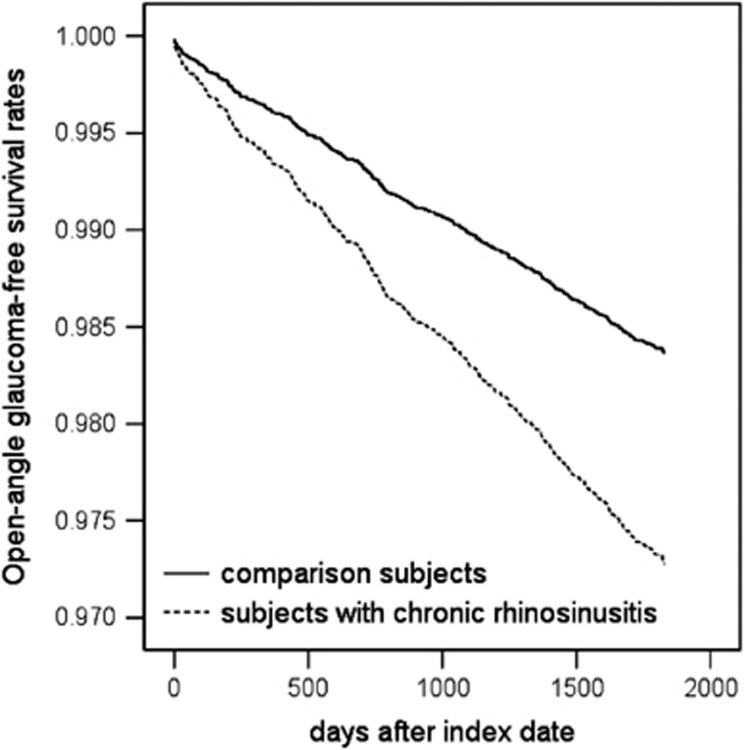
The incidence of OAG diagnoses over the 5-year follow-up period following a diagnosis of CRS is presented in Table 2. Of all the 62 568 sampled subjects, 1.8% received a diagnosis of OAG over the 5-year follow-up period, 2.7% and 1.5% for the study cohort and comparison cohorts, respectively. The incidence rate of OAG diagnoses over the 5-year follow-up period was 5.45 (95% CI: 4.95–5.98) per 1000 person-years for the study cohort and 2.80 (95% CI: 2.60–3.03) per 1000 person-years for the comparison cohort. Furthermore, the log-rank test suggested that study subjects with CRS had a significantly lower 5-year OAG-free survival rate than comparison subjects (log-rank test; χ2 value=75.27; P<0.001). The 5-year OAG-free survival curves for the study and comparison cohort by the Kaplan–Meier method is displayed in Figure 2.
Table 2. Incidence rate, crude, and adjusted hazard ratio for open-angle glaucoma among the sampled patients.
| Presence of open-angle glaucoma |
Total (n=62 568) |
Subjects with chronic rhinosinusitis (n=15 642) |
Comparison subjects (n=46 926) |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| 5-Year follow-up period | ||||||
| Yes | 1111 | 1.8 | 426 | 2.7 | 658 | 1.5 |
| Incidence rate per 1000 Person-years (95% CI) | 3.82 (3.61–4.04) | 5.45 (4.95–5.98) | 2.80 (2.60–3.03) | |||
| Adjusteda,b HR (95% CI) | — | 1.73* (1.53–1.96) | 1.00 | |||
*P<0.001.
Hazard ratio was calculated by using stratified Cox proportional regression (stratified on sex, age group, urbanization level, and the year of index date) with cases censored if individuals died during the 5-year follow-up period.
Adjustment for patient's monthly income, geographic region, hypertension, diabetes, coronary heart disease, hyperlipidemia, and hypothyroidism.
Figure 2.
Open-angle glaucoma-free survival rates for subjects with chronic rhinosinusitis and comparison subjects.
Table 2 also presents the hazard ratio (HR) for developing OAG over the 5-year follow-up period between the study cohort and the comparison cohort. A cox proportional hazards regression stratified by sex, age group, urbanization level, and index year, suggested that the HR for developing OAG over the 5-year follow-up period for the study cohort was 1.73 (95% CI: 1.53–1.96) when compared with the comparison cohort after adjusting for monthly income, geographic region, hypertension, diabetes, CHD, hyperlipidemia, and hypothyroidism and censoring the cases who died over the 5-year follow-up period.
Discussion
To the best of our knowledge, this study is the first to use a nationwide population-based data set to examine the association between CRS and the development of OAG. This study succeeded in reporting an increased risk of developing OAG over the first 5 years following a diagnosis of CRS. We found that the adjusted HR for OAG over the 5-year follow-up period was 1.73 compared with the comparison cohort.
CRS is a heterogeneous disease with a complicated pathophysiology.13, 14 Phenotypes of CRS can be differentiated based on mucosal remodeling and inflammatory patterns.4 IOPs have a critical role in the development and/or progression of glaucoma.15 Mojon et al8 found a positive correlation between the respiratory disturbance index and IOP. Purvin et al9 also demonstrated that intracranial pressure increases as a result of episodic hypoxemia and hypercapnia, thereby leading to papilledema and an increased risk of eye disease. Moreover, previous studies presented that ostial obstructions in CRS limit airflow, which cause hypoxia within the sinus cavity and blocks mucus drainage from sinuses leading to mucus retention and hypoxia.10, 11 Marcus et al16 suggested that repeated intermittent periods of hypoxia may influence the progression of ganglion cell loss. CRS might alter the normal physiologic balance and lead to hypoxia, thereby increasing the risk of developing OAG. Further studies are needed to confirm our findings and explore the underlying mechanisms.
The strength of our study lies in the longitudinal database and large population size to avoid problems of selection biases inherent in studies that take data from voluntary registries or hospital-referred study patients. Nevertheless, the findings of this study need to be interpreted within the context of several limitations. First, this investigation may have been the victim to a surveillance bias in that patients with CRS are more likely to frequent outpatient clinics, which may lead to an early detection of a separate and possibly unrelated condition because of the increased exposure to medical services. Therefore, we have assured that all patients receiving CRS and OAG diagnoses were made by certified otolaryngologists and ophthalmologists, respectively. Second, some factors including IOP, age, racial background, and family history may have an influence on the development of OAG.17 Third, the relationship between CRS and OAG observed in this study may have been due to the side effects of CRS medications such as topical or systemic corticosteroids, some of which may increase the risk of OAG.18, 19 However, many prior studies failed to establish the link between nasal steroids and IOP.20, 21, 22 Future large-scale prospective studies are needed to clarify the incidence of steroid-induced IOP elevation in CRS patients treated with intranasal steroids. Fourth, over 98% of Taiwan's residents are of Han Chinese ethnicity. Therefore, the association found in this study may only be valid for this population and caution should be exercised in extrapolating to a non-Chinese population. Fifth, subjects who were suffering from OAG asymptomaticlly could be undiagnosed in this study. Finally, the distributions of cardiovascular parameters are significantly different in both cohorts; although, we have taken this factor into consideration in the regression models.
Despite these limitations, we found that those patients with CRS had a significantly higher risk of developing OAG compared with patients without CRS. The adjusted HR of OAG was 1.73 times greater in cases than comparison subjects. Otolaryngologists and physicians should be alerted to the possibility of their patients developing OAG. Ophthalmologists should be aware of the association of CRS with OAG and consider giving patient referrals to otolaryngologists for investigation and possible treatment options.
Acknowledgments
This study was supported by a grant SKH-TMU-102-03 in Taiwan. This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health, Taiwan, and managed by the National Health Research Institutes. The interpretations and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health, or the National Health Research Institutes.
The authors declare no conflict of interest.
References
- Zuliani G, Carron M, Gurrola J, Coleman C, Haupert M, Berk R, et al. Identification of adenoid biofilms in chronic rhinosinusitis. Int J Pediatr Otorhinolaryngol. 2006;70:1613–1617. doi: 10.1016/j.ijporl.2006.05.002. [DOI] [PubMed] [Google Scholar]
- Lin HC, Xirasagar S, Chen CH, Hwang YT. Physician's case volume of intensive care unit pneumonia admissions and in-hospital mortality. Am J Respir Crit Care Med. 2008;177:989–994. doi: 10.1164/rccm.200706-813OC. [DOI] [PubMed] [Google Scholar]
- Murr AH, Goldberg AN, Pletcher SD, Dillehay K, Wymer LJ, Vesper SJ. Some chronic rhinosinusitis patients have elevated populations of fungi in their sinuses. Laryngoscope. 2012;122:1438–1445. doi: 10.1002/lary.23295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachert C, Zhang N. Chronic rhinosinusitis and asthma: novel understanding of the role of IgE "above atopy". J Intern Med. 2012;272:133–143. doi: 10.1111/j.1365-2796.2012.02559.x. [DOI] [PubMed] [Google Scholar]
- Gliklich RE, Metson R. The health impact of chronic sinusitis in patients seeking otolaryngologic care. Otolaryngol Head Neck Surg. 1995;113:104–109. doi: 10.1016/S0194-59989570152-4. [DOI] [PubMed] [Google Scholar]
- Meltzer EO, Hamilos DL, Hadley JA, Lanza DC, Marple BF, Nicklas RA, et al. Rhinosinusitis: Establishing definitions for clinical research and patient care. Otolaryngol Head Neck Surg. 2004;131:S1–S62. doi: 10.1016/j.otohns.2004.09.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavin RG, Spector SL, Bernstein IL, Kaliner MA, Kennedy DW, Virant FS, et al. The diagnosis and management of sinusitis: a practice parameter update. J Allergy Clin Immunol. 2005;116:S13–S47. doi: 10.1016/j.jaci.2005.09.048. [DOI] [PubMed] [Google Scholar]
- Mojon DS, Hess CW, Goldblum D, Fleischhauer J, Koerner F, Bassetti C, et al. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology. 1999;1069:1009–1012. doi: 10.1016/S0161-6420(99)00525-4. [DOI] [PubMed] [Google Scholar]
- Purvin VA, Kawasaki A, Yee RD. Papilledema and obstructive sleep apnea syndrome. Arch Ophthalmol. 2000;118:1626–1630. doi: 10.1001/archopht.118.12.1626. [DOI] [PubMed] [Google Scholar]
- Matsune S, Kono M, Sun D, Ushikai M, Kurono Y. Hypoxia in paranasal sinuses of patients with chronic sinusitis with or without the complication of nasal allergy. Acta Otolaryngol. 2003;123:519–523. doi: 10.1080/0036554021000028113. [DOI] [PubMed] [Google Scholar]
- Early SB, Hise K, Han JK, Borish L, Steinke JW. Hypoxia stimulates inflammatory and fibrotic responses from nasal-polyp derived fibroblasts. Laryngoscope. 2007;117:511–515. doi: 10.1097/MLG.0b013e31802e927b. [DOI] [PubMed] [Google Scholar]
- Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf. 2011;20:236–242. doi: 10.1002/pds.2087. [DOI] [PubMed] [Google Scholar]
- Payne SC, Han JK, Huyett P, Negri J, Kropf EZ, Borish L, et al. Microarray analysis of distinct gene transcription profiles in non-eosinophilic chronic sinusitis with nasal polyps. Am J Rhinol. 2008;22:568–581. doi: 10.2500/ajr.2008.22.3233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin HW, Cho K, Kim DW, Han DH, Khalmuratova R, Kim SW, et al. Hypoxia-inducible factor 1 mediates nasal polypogenesis by inducing epithelial-to-mesenchymal transition. Am J Respir Crit Care Med. 2012;185:944–954. doi: 10.1164/rccm.201109-1706OC. [DOI] [PubMed] [Google Scholar]
- Faridi O, Park SC, Liebmann JM, Ritch R. Glaucoma and obstructive sleep apnea syndrome. Clin Experiment Ophthalmol. 2012;40:408–419. doi: 10.1111/j.1442-9071.2012.02768.x. [DOI] [PubMed] [Google Scholar]
- Marcus DM, Costarides AP, Gokhale P, Papastergiou G, Miller JJ, Johnson MH, et al. Sleep disorders: a risk factor for normal-tension glaucoma. J Glaucoma. 2001;10:177–183. doi: 10.1097/00061198-200106000-00006. [DOI] [PubMed] [Google Scholar]
- Cedrone C, Mancino R, Cerulli A, Cesareo M, Nucci C. Epidemology of primary glaucoma: prevalence, incidence, and blinding effects. Prog Brain Res. 2008;173:3–14. doi: 10.1016/S0079-6123(08)01101-1. [DOI] [PubMed] [Google Scholar]
- Razeghinejad MR, Katz LJ. Steroid-induced iatrogenic glaucoma. Ophthalmic Res. 2012;47:66–80. doi: 10.1159/000328630. [DOI] [PubMed] [Google Scholar]
- Bui CM, Chen H, Shyr Y, Joos KM. Discontinuing nasal steroids might lower intraocular pressure in glaucoma. J Allergy Clin Immunol. 2005;116:1042–1047. doi: 10.1016/j.jaci.2005.07.031. [DOI] [PubMed] [Google Scholar]
- Garbe E, LeLorier J, Boivin JF, Suissa S. Inhaled and nasal glucocorticoids and the risks of ocular hypertension or open-angle glaucoma. JAMA. 1997;277:722–727. [PubMed] [Google Scholar]
- Spiliotopoulos C, Mastronikolis NS, Petropoulos IK, Mela EK, Goumas PD, Gartaganis SP. The effect of nasal steroid administration on intraocular pressure. Ear Nose Throat J. 2007;86:394–395. [PubMed] [Google Scholar]
- Ozturk F, Yuceturk AV, Kurt E, Unlü HH, Ilker SS. Evaluation of intraocular pressure and cataract formation following the long-term use of nasal corticosteroids. Ear Nose Throat J. 1998;77:846–848. [PubMed] [Google Scholar]