Sir,
Management of traumatic endophthalmitis is challenging because of the presence of virulent organisms, polymicrobial infections in 20% cases and collateral ocular damage.1 Knowledge of possible organism helps in specific early management. We report the first case of traumatic endophthalmitis following fishhook injury by a marine organism, Shewanella putrefaciens.
Case report
A 25-year-old fisherman presented with sudden painful decrease of vision in right eye (OD), 11 days after trauma with a fishhook. He had a vision of light perception with inaccurate projection of rays. Slit lamp examination revealed self-sealed corneal perforation, shallow anterior chamber and exudates in pupillary area (Figure 1a). Left eye was within normal limits with 20/20 vision. Ultrasonography revealed low reflective dot echoes in vitreous cavity along with thickened choroid. With a diagnosis of OD post-traumatic endophthalmitis, he underwent pars plana lensectomy, vitrectomy, and intraocular antibiotic injection (vancomycin 1 mg/0.1 ml and ceftazidime 2.25 mg/0.1 ml). Undiluted vitreous sample was inoculated on sheep blood and chocolate agar, thioglycollate broth, brain heart infusion broth (BHI), Robertson's cooked meat medium (RCM) and Sabouraud dextrose agar. RCM and BHI showed turbidity after 48 h, which on subculture on blood agar grew gray, moist, β-hemolytic colonies. A motile Gram-negative bacillus grew on MacConkey's agar as non-lactose fermenting colonies, did not utilize glucose and citrate, produced oxidase and urease, and was indole negative. Vitek 2 (BiMerieux, Marcy-I'Etoile, France) confirmed the organism to be Shewanella putrefaciens. Using Kirby–Bauer method, it was sensitive to cefazoline, chloramphenicol, ciprofloxacin, gatifloxacin, moxifloxacin and ofloxacin.
Figure 1.
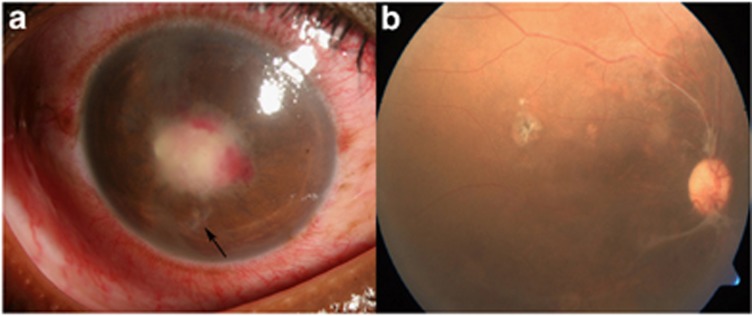
(a) Slit lamp photograph of the right eye taken under diffuse illumination at presentation showing self-sealed full thickness corneal tear (black arrow), shallow anterior chamber and pupillary exudates. (b) Fundus photograph 17 months after injury showing an attached retina and an epiretinal membrane around the disc.
The patient was started on topical and oral gatifloxacin, topical corticosteroids, and mydriatics. He improved but developed ocular hypotony (IOP 02 mm Hg) and pupillary membrane. Membranectomy and silicon oil infusion was done followed by oil removal after 6 months. At 17 months follow-up, the eye was quiet, BCVA was 20/120 and IOP was 15 mm Hg with an attached retina (Figure 1b).
Comments
An unusual mode of injury and isolation of a rare organism makes this case unique. Published literature on S. putrefaciens, has reported sensitivity to aminoglycosides, fluoroquinolones, third/fourth-generation cephalosporins, and resistance to penicillin.2, 3, 4 A prior knowledge of possibility of S. putrefaciens infection in fishhook injuries and its antibiotic susceptibility pattern will help in better institution of empirical therapy for such infections.
Acknowledgments
The study was supported by Hyderabad Eye Research Foundation, Hyderabad.
The authors declare no conflict of interest.
References
- Das T, Kunimoto DY, Sharma S, Jalali S, Majji AB, Nagaraja Rao T, et al. Relationship between clinical presentation and visual outcome in postoperative and post traumatic endophthalmitis in south central India. Indian J Ophthalmol. 2005;53 (1:5–16. doi: 10.4103/0301-4738.15298. [DOI] [PubMed] [Google Scholar]
- Kim JH, Cooper RA, Welty WK, Harrell LJ, Zwadyk P, Klotman ME. Pseudomonas putrefaciens bacteremia. Rev Infect Dis. 1989;11 (1:97–104. [PubMed] [Google Scholar]
- To KK, Wong SS, Cheng VC, Tang BS, Li IW, Chan JF, et al. Epidemiology and clinical features of Shewanella infection over an eight-year period. Scand J Infect Dis. 2010;42 (10:757–762. doi: 10.3109/00365548.2010.490562. [DOI] [PubMed] [Google Scholar]
- Holt HM, Sogaard P, Gahrn-Hansen B. Ear infections with Shewanella alga: a bacteriologic, clinical and epidemiologic study of 67 cases. Clin Microbiol Infect. 1997;3 (3:329–334. doi: 10.1111/j.1469-0691.1997.tb00622.x. [DOI] [PubMed] [Google Scholar]


