Summary
A remote vaginal metastasis from a colo-rectal carcinoma is extremely rare. Only few cases have been described in the literature. The radiological appearances of a vaginal metastasis from colon-rectal cancer have not been extensively investigated. We report the MRI findings with clinical and pathological correlations of a remote and isolated vaginal metastasis revealing a mid-sigmoid adenocarcinoma in a 67 years old woman.
Keywords: Sigmoid Neoplasms, Magnetic Resonance Imaging, Neoplasm Metastasis, Adenocarcinoma
Background
A remote vaginal metastasis from a colo-rectal carcinoma is extremely rare. Only few cases have been described in the literature, in which the vagina as well as other organs showed the secondary involvement by a known cancer or, very rarely, the vaginal metastasis was the first mark as well as the isolated secondary location of an unknown distant adenocarcinoma. All these cases are focused on the clinical presentation and the histological features [1–9]. The radiological appearances of a vaginal metastasis from colon-sigmoid cancer have not been extensively investigated.
We herein report the MRI findings of a remote and isolated vaginal metastasis revealing a mid-sigmoid adenocarcinoma.
Case Report
In February 2012, a 67 years old woman (gravida 3 para 3) was admitted in our hospital for vaginal bleeding.
The patient presented a history of type II diabetes, arterial hypertension, hypercholesterolemia and recurrent renal colics. A hystero-annexectomy had been performed 18 years before because of diffuse and nodular uterine leiomyomatosis associated to erosive cervicitis. The direct gynaecological examination disclosed a solid lesion of the anterior vaginal wall. The general laboratory tests were unremarkable.
To evaluate the vaginal lesion, a MRI was performed with a 3T device (Siemens Magnetom Trio). The following sequences were executed: TSE T2 weighted on coronal, axial and sagittal plane; TSE T1 weighted on axial plane; EPI DWI with ADC map calculation on axial and sagittal plane; 3D-T1-VIBE on axial and sagittal plane before and after injection of Gd-DTPA.
The MRI confirmed the presence of a solid infiltrating nodular lesion (22×25 mm axial diameters) at middle-inferior level of the anterior vaginal wall, isointense on T1w and faintly hyperintense on T2w images respect to the muscle, hypervascularized on the contrast enhanced sequence (Figure 1A, 1B). Moreover a stenosing thickening of the sigmoid wall, 4 cm in longitudinal extension, was observed (Figure 1C). Both the vaginal and sigmoid lesions showed a DWI restriction with low ADC values consistent with malignancy. A secondary vaginal lesion from a sigmoid-colon cancer was suggested.
Figure 1.
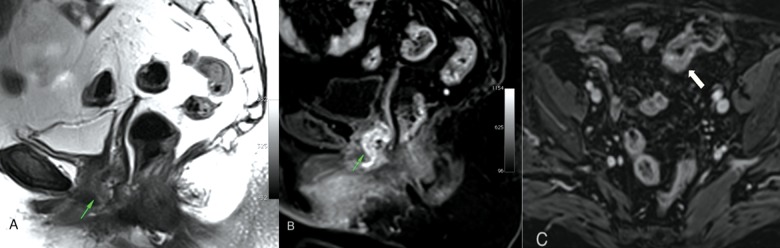
A solid nodular lesion of the anterior vaginal wall appears faintly hyperintense on TSE-T2 sagittal plane (A) and hypervascularized on T1-VIBE contrast enhanced sagittal plane (B). T1-VIBE contrast enhanced axial plane (C) shows a stenosing thickening of the sigmoid wall.
A colonoscopy confirmed the presence of a sigmoid-colon neoplasm. The biopsy of both sigmoid and vaginal lesions was executed. The histological examination disclosed an adenocarcinoma of the sigmoid colon associated to a vaginal metastasis (Figure 2).
Figure 2.
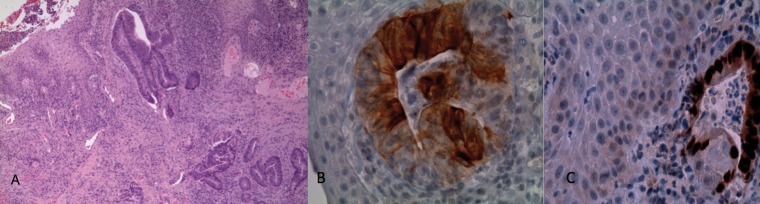
On microscopic examination the vaginal mucosa was infiltrated by an adenocarcinoma of intermediate grade, with focal necrosis. Microphotographs of vaginal biopsy (A) showed the stroma infiltrated by neoplastic glands (yellow arrows) beneath the intact squamous epithelium of vagina [hematoxylin-and-eosin stain (H&E) magnification, 40×]. The immunostaining showed the neoplastic glands strongly positive for cytokeratin 20 (B) and CDX2 (C); the cytokeratin 7 and estrogen receptors were negative [400×]. On the basis of the morphology and immunohistochemical profile a diagnosis of vaginal infiltration by colonic adenocarcinoma was made.
Thoracic and abdominal CT scan was performed (Toschiba Aquilion 64 CT scan) in order to staging the cancer. The examination showed both sigmoid and vaginal lesions. The remote metastatic involvement of other organs was not observed.
The patient had an anterior resection for the primary sigmoid carcinoma and a local excision of the secondary vaginal lesion. At the histological examination the primary tumor was classified as pT3N0M1.
Discussion
The adenocarcinomas represents the 8% of vaginal cancers. Most of the vaginal adenocarcinomas are secondary either to a spread from a primary uterine, rectum and ovary cancer or represent distant metastasis from other tumors (mostly breast, pancreas and kidney) [4,5].
Vaginal remote metastases from a colo-rectal cancer are extremely rare. To the best of our knowledge, only 20 cases have been described in the literature (pubmed search criteria: colon, sigmoid, cancer, adenocarcinoma, vagina, metastasis, metastases): the vaginal symptoms were the first clinical mark in ten cases [1,5,6], while the vaginal involvement was subsequent to the discovery of the colonic cancer, often years after surgery, in the others [2,4,7]. Moreover the majority of these cases presented other metastatic locations, while only three patients showed exclusively a remote isolated vaginal metastasis [2,5,6].
Vaginal metastasis can involve all the part of the vagina [2,6] and are thought to be due most likely to a venous pathway of spread. Indeed through the vertebral vein system (a system which is constantly subject to arrests and reversals in the direction of flow of blood) neoplastic cells can go from the colon to the ovarian plexus or to the parametrial veins and from here, finally, to the vaginal veins [2,6]. Other hypotheses have been advanced to explain the spread of tumoral cells from colon to vagina: direct infiltration via ischio-rectal fossa, infiltration through the lymphatic channels and spread from the colonic serosa via the fallopian tubes and the uterus to the vagina [6].
Regarding the pathological diagnosis is important to note that there is a lot of favorable date on the use of CK7 and CK20 (cytokeratine 7 and 20 respectively) in order to asses the origin of metastatic adenocarcinoma of an unknown primary tumor. Indeed CK 7 is usually present in tissues such as vagina, breast, lung and ovary but not in colon. On the other hand CK 20 is present in the gastrointestinal tract and is a powerful marker to distinguish cells of a gastrointestinal origin from other tumors [5]. Thus, since a colonic carcinoma shows a CK7−/CK20+ phenotype while a gynaecological carcinoma show a CK7+/CK20− phenotype, the analysis of the cells from an eteroplastic lesion of the vagina showing the first profile, should lead to a detailed study of the intestinal tract looking for a primary tumor.
Thus our patient represents a very rare combination in whom the vaginal bleeding caused by a distant isolated metastasis was the first clinical mark of an unknown sigmoid-colon cancer.
Another peculiar aspect of our case is represented by the role of MRI in suggesting the correct diagnosis. It is difficult to suggest the appropriate diagnosis of a vaginal lesion based exclusively on the features of the MRI morphology and signal.
Squamous cell carcinoma is the most frequent of the vaginal primary cancers and can have different appearances (ulcerative, fungating and annular) with a T2w intermediate and a T1w hypointense signal on MRI. Vaginal adenocarcinomas are described to be generally hyperintense in T2w images. Other primary vaginal tumors are melanoma, that shows a peculiar T1 hyperintensity, and leiomyosarcoma, that can show areas of high T2-weighted signal intensity corresponding to cystic necrosis and areas of high T1-weighted signal intensity corresponding to acute haemorrhage. Vaginal metastases from gynaecologic or non-gynaecologic malignancies show a MRI signal reflecting the features of the original tumor [10].
In our case the vaginal lesion appeared as a solid infiltrating nodule, isointense on T1w and faintly hyperintense on T2w images, hypervascularized on the contrast enhanced images and characterized by restriction of the signal on DWI sequence. Although this MRI appearance suggested an aggressive neoplastic lesion, the morphological and signal features were not specific for a secondary vaginal involvement from a gastro-intestinal neoplasm. As a consequence the identification of the sigmoid-colon lesion represented really the basic clue to suggest the correct diagnosis.
Conclusions
In conclusion, in a MRI dedicated to the characterization of a vaginal lesion, the radiologists should take into account the possibility of a secondary remote vaginal involvement from colo-rectal cancer and as consequence should have a careful look to the intestinal segments included in the planes of the MRI study.
References
- 1.Whitelaw GP, Leard SE, Pearson L, et al. Carcinoma of large bowel with metastases to genitalia: report of two cases. AMA Arch Surg. 1956;73:171–78. doi: 10.1001/archsurg.1956.01280010173023. [DOI] [PubMed] [Google Scholar]
- 2.Raider L. Remote vaginal metastases from carcinoma of the colon. Am J Roentgenol Radium Ther Nucl Med. 1966;97:944–50. doi: 10.2214/ajr.97.4.944. [DOI] [PubMed] [Google Scholar]
- 3.Chagpar A, Kanthan SC. Vaginal metastasis of colon cancer. Am Surg. 2001;67:171–72. [PubMed] [Google Scholar]
- 4.Yagci G, Cetiner S, Dede M, et al. True vaginal metastasis of rectal cancer. Indian J Surg. 2005;67:270–72. [Google Scholar]
- 5.Marchal F, Leroux A, Hoffstetter S, et al. Vaginal metastasis revealing colon adenocarcinoma. Int J Colorectal Dis. 2006;21:861–62. doi: 10.1007/s00384-004-0734-x. [DOI] [PubMed] [Google Scholar]
- 6.Ceccaroni M, Paglia A, Ruffo G, et al. Symptomatic vaginal bleeding in a postmenopausal woman revealing colon adenocarcinoma metastasizing exclusively to the vagina. J Minim Invasive Gynecol. 2010;17(6):779–81. doi: 10.1016/j.jmig.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 7.Tanaka T, Kanda T, Sakaguchi S, et al. Vaginal Stump Metastasis from Sigmoid Colon Cancer. Acta Cytologica. 2012;56:92–96. doi: 10.1159/000330815. [DOI] [PubMed] [Google Scholar]
- 8.Lorente L, Alonso S, Pascual M, et al. Vaginal metastasis of colon cancer. Rev Esp Enferm Dig. 2011;103(8):435–36. doi: 10.4321/s1130-01082011000800011. [DOI] [PubMed] [Google Scholar]
- 9.Lee SM, Whiteley HW. Unusual metastatic sites of colonic and rectal carcinoma: report of four cases. Dis Colon Rectum. 1974;17:560–61. doi: 10.1007/BF02587036. [DOI] [PubMed] [Google Scholar]
- 10.Parikh FH, Barton DP, Ind TE, et al. MR imaging features of vaginal malignancies. Radiographics. 2008;28(1):49–63. doi: 10.1148/rg.281075065. [DOI] [PubMed] [Google Scholar]


