Abstract
Background
Nonrecurrent laryngeal nerve (NRLN) is a risk factor for nerve injury during thyroidectomy or parathyroidectomy. It is usually associated with abnormal vasculature that can be identified by several imaging methods. The aim of this study was to retrospectively analyze the preoperative diagnosis and intraoperative protection of NRLN.
Material/Methods
Of the 7169 patients who underwent thyroid surgery at our hospital between August 2008 and January 2013, 5 patients with NRLN were identified. Preoperative chest X-rays, neck ultrasonography (US), and computed tomography (CT) findings were reviewed. NRLNs were carefully and systematically searched for in surgery.
Results
Preoperative CT predicted NRLN in all 5 cases (100% accuracy). The detection rate of NRLN by CT was 0.4% (5/1170). NRLNs were confirmed in surgery. All of them were right-sided NRLN with type IIA variant. The CT scans clearly revealed the vascular anomalies. The review of US images suggested that vascular anomalies could be identified on the images in 1 patient. No postoperative complications occurred in any patient.
Conclusions
The preoperative CT scan was a reliable and effective method for identifying abnormal vasculature to indirectly predict NRLN. Combining the CT and US findings with adequate surgical technique may help to reduce the risk of nerve damage, in addition to preventing nerve palsy.
Keywords: Abnormal Vascular, Computed Tomography, Parathyroidectomy, Thyroidectomy, Recurrent Laryngeal Nerve Injuries
Background
Recurrent laryngeal nerve (RLN) palsy is one of the most common complications after thyroid surgery. Therefore, reducing the rate of temporary and, especially, permanent nerve palsy is essential. Although an important anatomic landmark, Zuckerkandl’s’ tubercles, could help us to locate and dissect the RLN during thyroid surgery, anatomic variations such as nonrecurrent laryngeal nerve (NRLN) might increase the rate of RLN damage [1].
NRLN is a rare anomaly that represents a major risk factor for injury during neck surgery. Because of its special anatomical position, it may be misdiagnosed and damaged, with subsequent vocal cord paralysis that can decrease the overall physical and psychological quality of life [2,3].
Vascular anomaly of the aortic arches during early embryonic development results in the formation of NRLN, which was first reported by Stedman in 1823 [4]. The absence of brachiocephalic artery and the presence of an aberrant right subclavian artery (arteria lusoria) is the feature used to identify NRLN. Surgeons seek ways to make a preoperative diagnosis of NRLN to reduce the risk of inadvertent nerve injury.
The aim of this study was to retrospectively analyze the methods of preoperative judgment and intraoperative identification and protection of NRLN during thyroidectomy or parathyroidectomy.
Material and Methods
Of the 7169 patients who underwent thyroidectomy or parathyroidectomy at our hospital between August 2008 and January 2013, 5 patients who had NRLN were included in this study. We retrospective reviewed the medical records and intraoperative findings in identifying the NRLN. Preoperative chest X-rays, neck ultrasonography (US), and CT findings were reviewed. Due to the cost, CT scans were mainly performed for the patients with suspected malignancy and lymph node metastasis. We also performed CT scans to evaluate massive and intrathoracic goiters. CT examination was performed for 1170 patients. The study was approved by the Ethics Committee at our hospital.
Due to embryologic reasons, NRLN is always associated with vascular anomalies of the aortic arch. On the right side, the absence of brachiocephalic artery and the presence of an “arteria lusoria” is the feature used to identify NRLN. In CT scan images, the “arteria lusoria” was identified as an aberrant right subclavian artery that originated from the left part of the aortic arch, crossed the mediastinum behind the esophagus, and entered the right base of the neck. The diagnosis of “arteria lusoria” was rejected when the brachiocephalic artery was found [5]. In the US scans, the division of the brachiocephalic artery into the right common carotid artery and the right subclavian artery has been described as the “Y sign” (Figure 1A) [6].
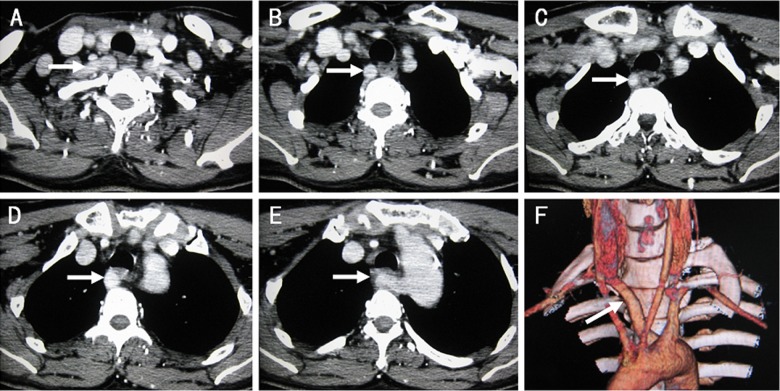
Figure 1.
Ultrasonographic image of normal arterial anatomy: the division of the brachiocephalic artery into the right common carotid artery and the right subclavian artery has been described as the “Y sign” (A). Ultrasonographic image of the abnormal artery anatomy: The right common carotid artery originated directly from the aortic arch and separated from the right subclavian artery, the brachiocephalic truck was absence (B). RCCA, right common carotid artery; RSA, right subclavian artery; BCT, brachiocephalic truck; AO, aortic arch.
According to the intraoperative findings, the NRLN was classified into 3 types based on the traveling approaches. Type I arises directly from the vagus nerve and running along with the superior thyroid vessels; type IIA originates from the vagus on the level of the trunk of inferior thyroid artery; and type IIB originate from the vagus and travels under the level of the trunk of inferior thyroid artery or between the branches.
Results
Five NRLN patients were identified in this period, and all were female. The mean age was 38.6 years, with a range of 26–48 years. We retrospectively reviewed patient information, including clinical presentation, physical examination, diagnostic investigations, therapeutic interventions, and pathology results. The normal preoperative vocal cord function of all patients were confirmed by fibrolaryngoscope, and none of them presented symptoms related to recurrent laryngeal nerve, such as hoarseness or bucking. In our group, near total thyroidectomy was performed in 2 patients, right lobectomy was performed in 2 patients, and subtotal thyroidectomy was performed in 1 patient. Lymph node dissection was performed in 4 patients. The postoperative histopathological diagnosis included 3 papillary carcinomas, 1 follicular carcinoma, and 1 nodular goiter (Table 1).
Table 1.
Cases of nonrecurrent laryngeal nerve.
| Patient | Age (y) | Sex | Diagnosis | Operation type | NRLN side | NRLN type |
|---|---|---|---|---|---|---|
| 1 | 48 | F | Papillary cancer | Near total thyroidectomy | Right | IIA |
| 2 | 26 | F | Follicular cancer | Lobectomy | Right | IIA |
| 3 | 39 | F | Papillary cancer | Near total thyroidectomy | Right | IIA |
| 4 | 35 | F | Papillary cancer | Lobectomy | Right | IIA |
| 5 | 45 | F | Nodular goiter | Subtotal thyroidectomy | Right | IIA |
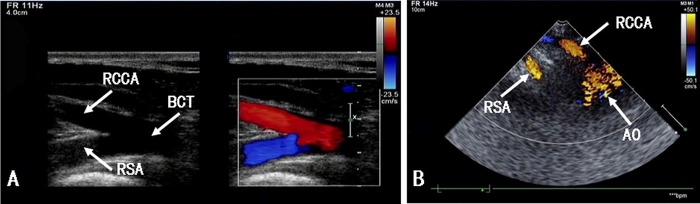
All of the 5 patients received preoperative chest X-ray, US, and CT imaging. All of them were suspected of NRLN according to the preoperative CT findings. We retrospectively reviewed the chest X-ray, US, and CT results. In our study, patients with NRLN had lacked the brachiocephalic trunk and had an “arteria lusoria” on CT images. The right subclavian artery originated directly from the left side of aortic arch, crossed the mediastinum behind the esophagus, and entered to the right side of the neck (Figure 2). We found no features of chest X-ray and US results to identify the NRLN before surgery. However, by reviewing the US images, we found that the right common carotid artery originated directly from the aortic arch and separated from the right subclavian artery, and the brachiocephalic truck was absent (Figure 1B).
Figure 2.
Contrast-enhanced CT scans of the neck and upper mediastinum in a patient with “arteria lusoria”. From image (A–E), the right subclavian artery (white arrow) originates from the left part of the aortic arch, crossed the mediastinum behind the esophagus, the brachiocephalic artery is absent. Image (F) shows the three-dimensional reconstruction CT scan of “arteria lusoria” (white arrow).
All surgical procedures of the 5 patients were performed by experienced surgeons. When a preoperative “arteria lusoria” diagnosis was given by CT findings, the surgical procedure of NRLN identification was performed. After dissection of the upper pole, we gently mobilized the thyroid inherent capsule, dissected the middle cervical vein and the inferior thyroid vessels, isolated and mobilized the thyroid lobe, and pulled it to the left. NRLN was found on the level of the inferior thyroid artery or cartilage and entered into the larynx at its usual location (Figure 3). In searching for the normal recurrent laryngeal nerve, blunt isolation was used to expose the tracheoesophageal groove. The absence of a normally recurrent laryngeal nerve at its normal position was confirmed. Careful intraoperative dissection also allowed for detection of NRLN in cases not detected by preoperative CT scan. The 5 patients with NRLN all had the right-side type IIA variation.
Figure 3.
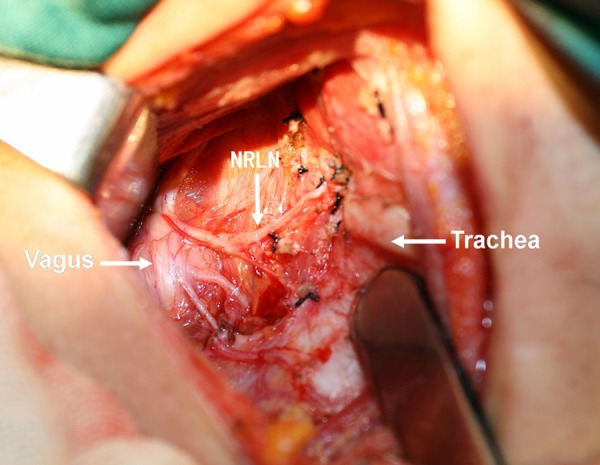
Intraoperative image showed the anatomy structure around the type IIA NRLN (white arrow).
Discussion
NRLN results from abnormal embryological development of the aortic arches. The nerve wraps around the sixth arch in the normal embryo stage. On the right, the nerve moves up as high as the fourth arch, which forms a portion of the subclavian artery. In the absence of the fourth aortic arch, the right recurrent laryngeal nerve goes directly into the larynx, forming a right NRLN. The incidence of right NRILN is 0.3–1.6% in the general population. Because the formation needs the coexistence of situs inversus viscerum, left NRLN is extremely rare, with an incidence of 0.04% [7,8]. The detection rate of arteria lusoria by CT for the prediction of NRLN was 0.4% (5/1170) in our group.
NRLN protection without recognition before surgery is very difficult for the surgeon. If the abnormal vasculature is identified, the risk of NRLN damage is reduced. In our group, although the vascular anomaly was recognized in preoperative neck CT findings, we also carefully explored the origin trunk of NRLN after we identified it. The tissue between the thyroid lobe and the carotid sheath was bluntly isolated, not dissected directly, to expose all the structure originating from the vagus nerve up to the larynx. NRLN includes 3 types based on the running course, of which type IIA is the most common [9]. In the present study, no NRLN injury occurred.
Several imaging methods aimed at the preoperative identification of NRLN have been recommended, including chest X-rays, barium esophagogram, vagal neurostimulation, and US and CT examinations. Each procedure has limitations because of the variable diagnostic accuracy, cost, and invasiveness.
Chest X-rays may present a special linear shadow on the frontal view and a rounded image travelling upward and right from the top of the aortic arch, but these features exist in less than 20% of cases [8,10,11].
Barium esophagogram may present an extrinsic compression on the left edge of the posterior esophagus notch at the third thoracic vertebral level below the aortic arch, which is called the “bayonet sign”. A few patients showed this esophagus compression symptom caused by “arteria lusoria”. Because the sign can be easily missed if the superior thoracic esophagus is not carefully examined and the lateral or oblique views are not obtained [8,12], we recommend barium esophagogram only for dysphagic cases.
Brauckhoff et al. [13,14] reported that selective vagal neurostimulation is an easy and reliable method to identify NRLN. They showed that a latency threshold of 3.5 ms after ipsilateral vagus nerve stimulation was able to distinguish between NRLN and recurrent laryngeal nerve (RLN). However, the lack of a standard with which to estimate variability and the high false positive results limit the use of this method [7,15].
US is an easy to perform, cost-effective, and noninvasive technique for preoperative recognition of NRLN. Maurizio et al. [16] reported that US can easily identify the absence of the brachiocephalic trunk and indirectly predicts NRLN with 100% accuracy. Its main limitation is that the results of US examinations depend on the sonographer; if the US operator does not look for the “Y sign”, NRLN cannot be predicted in routine preoperative US examination [9].
CT of the neck has become a common procedure before neck surgery. They are often performed to evaluate thyroid cancers with lymph node metastasis, intrathoracic goiters, or hyperparathyroidism [17,18]. For diagnosis of “arteria lusoria”, CT scanning is reliable. NRLN can be accurately predicted before surgery using CT by identifying the “arteria lusoria” and the absence of the brachiocephalic trunk without additional examination [19,20]. Wang et al. [5] reported 6 of 9 patients with NRLN had an “arteria lusoria” in CT images. In another study, although only 5 of the 20 patients with NRLN were suspected before surgery, all patients had the “arteria lusoria” feature found by reviewing the CT images in after the operation [9].
Conclusions
In our experience, preoperative CT scanning is a simple and effective method for identifying abnormal vasculature to indirectly predict NRLN. Combining CT and US findings with careful and systematic dissection of the RLN area may help reduce the risk of nerve damage and prevent nerve palsy.
Footnotes
Source of support: This research was supported by the Innovation Team Project of the Education Department of Liaoning Province (No: LT2010102); the Liaoning Baiqianwan Talents Program (No: 2010921070); Colleges and Universities Doctoral Discipline Scientific Fund (No: 20122104110006); and the Science and Technology Plan Program of Liaoning Province (No: 2012225087)
Disclosure
The authors declare no conflicts of interest in this work.
Ethical approval
Our study protocol was approved by the Ethics Committee of the First Affiliated Hospital of China Medical University, Shenyang, China. Written informed consent was obtained from all study participants.
References
- 1.Pelizzo MR, Toniato A, Gemo G. Zuckerkandl’s tuberculum: an arrow pointing to the recurrent laryngeal nerve (constant anatomical landmark) J Am Coll Surg. 1998;187:333–36. doi: 10.1016/s1072-7515(98)00160-4. [DOI] [PubMed] [Google Scholar]
- 2.Kern KA. Medicolegal analysis of errors in diagnosis and treatment of surgical endocrine disease. Surgery. 1993;114:1167–74. [PubMed] [Google Scholar]
- 3.Smith E, Taylor M, Mendoza M, et al. Spasmodic dysphonia and vocal fold paralysis: outcomes of voice problems on work-related functioning. J Voice. 1998;12:223–32. doi: 10.1016/s0892-1997(98)80042-8. [DOI] [PubMed] [Google Scholar]
- 4.Stedman GW. A singular distribution of some of the nerves and arteries of the neck and the top of the thorax. Edindeli Med Surg J. 1823;19:564–65. [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Y, Ji Q, Li D, Wu Y, et al. Preoperative CT diagnosis of right nonrecurrent inferior laryngeal nerve. Head Neck. 2011;33:232–38. doi: 10.1002/hed.21434. [DOI] [PubMed] [Google Scholar]
- 6.Iacobone M, Viel G, Zanella S, et al. The usefulness of preoperative ultrasonographic identification of nonrecurrent inferior laryngeal nerve in neck surgery. Langen-becks Arch Surg. 2008;393:633–38. doi: 10.1007/s00423-008-0372-9. [DOI] [PubMed] [Google Scholar]
- 7.Toniato A, Mazzarotto R, Piotto A, et al. Identification of nonrecurrent laryngeal nerve during thyroid surgery: 20 year experience. World J Surg. 2004;28:659–61. doi: 10.1007/s00268-004-7197-7. [DOI] [PubMed] [Google Scholar]
- 8.Henry JF, Audiffret J, Denizot A, Plan M. The nonrecurrent inferior laryngeal nerve: review of 33 cases, including two on the left side. Surgery. 1988;104:977–84. [PubMed] [Google Scholar]
- 9.Lee YS, Son EJ, Chang HS, et al. Computed tomography is useful for preoperative identification of nonrecurrent laryngeal nerve in thyroid cancer patients. Otolaryngol Head Neck Surg. 2011;145:204–7. doi: 10.1177/0194599811406670. [DOI] [PubMed] [Google Scholar]
- 10.Watanabe A, Kawabori S, Osanai H, et al. Preoperative computed tomography diagnosis of non-recurrent inferior laryngeal nerve. Laryngoscope. 2001;111:1756–59. doi: 10.1097/00005537-200110000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Nagayama I, Okabe Y, Katoh H, Furukawa M. Importance of pre-operative recognition of the nonrecurrent laryngeal nerve. J Laryngol Otol. 1994;108:417–19. doi: 10.1017/s0022215100126957. [DOI] [PubMed] [Google Scholar]
- 12.De Luca L, Bergman JJ, Tytgat GN, Fockens P. EUS imaging of the arteria lusoria: case series and review. Gastrointest Endosc. 2000;52:670–73. doi: 10.1067/mge.2000.109808. [DOI] [PubMed] [Google Scholar]
- 13.Brauckhoff M, Walls G, Brauckhoff K, et al. Identification of the non-recurrent inferior laryngeal nerve using intraoperative neurostimulation. Langenbecks Arch Surg. 2002;386:482–87. doi: 10.1007/s00423-001-0253-y. [DOI] [PubMed] [Google Scholar]
- 14.Brauckhoff M, Machens A, Sekulla C, et al. Latencies shorter than 3.5 ms after vagus nerve stimulation signify a nonrecurrent inferior laryngeal nerve before dissection. Ann Surg. 2011;253:1172–77. doi: 10.1097/SLA.0b013e3182128b9e. [DOI] [PubMed] [Google Scholar]
- 15.Dralle H, Sekulla C, Lorenz K, et al. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg. 2008;32:1358–66. doi: 10.1007/s00268-008-9483-2. [DOI] [PubMed] [Google Scholar]
- 16.Iacobone M, Viel G, Zanella S, et al. The usefulness of preoperative ultrasonographic identification of nonrecurrent inferior laryngeal nerve in neck surgery. Langenbecks Arch Surg. 2008;393:633–38. doi: 10.1007/s00423-008-0372-9. [DOI] [PubMed] [Google Scholar]
- 17.Choi YJ, Yun JS, Kook SH, et al. Clinical and imaging assessment of cervical lymph node metastasis in papillary thyroid carcinomas. World J Surg. 2010;34:1494–99. doi: 10.1007/s00268-010-0541-1. [DOI] [PubMed] [Google Scholar]
- 18.Singh A, Butuc R, Lopez R. Metastatic papillary thyroid carcinoma with absence of tumor focus in thyroid gland. Am J Case Rep. 2013;14:73–75. doi: 10.12659/AJCR.883834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hermans R, Dewandel P, Debruyne F, Delaere PR. Arteria lusoria identified on preoperative CT and nonrecurrent inferior laryngeal nerve during thyroidectomy: a retrospective study. Head Neck. 2003;25:113–17. doi: 10.1002/hed.10180. [DOI] [PubMed] [Google Scholar]
- 20.Materazzi G, Berti P, Iacconi P, Miccoli P. Nonrecurrent laryngeal nerve predicted before thyroidectomy by preoperative imaging. J Am Coll Surg. 2000;191:580. doi: 10.1016/s1072-7515(00)00692-x. [DOI] [PubMed] [Google Scholar]