Abstract
The associations between specific intra- and inter-personal psychosocial factors and dietary patterns were explored in a healthy, working adult population. Participants (N= 640) were enrolled in a prospective predictive health study and characterized by a mean age of 48(SD = 11) years, 67% women, and 30% minority. Baseline psychosocial measures of perceived stress, depressive symptoms, social support, and family functioning were examined for their relationships with three diet quality indices - AHEI, DASH, and the Mediterranean. Dietary intake was of moderate quality in this high income, well-educated, psychosocially healthy population. Social support was positively associated with better diet quality for all three indices (p< .01). Further research should focus on socio-environmental factors associated with diet quality.
Keywords: diet quality, diet patterns AHEI, DASH, Mediterranean diet, psychosocial
Introduction
The link between unhealthy dietary patterns and morbidity and mortality is well established (World Health Organization, 2003). Poor diet quality is a significant contributor to four of the leading causes of death in the United States (US), including cardiovascular disease, cancer, type 2 diabetes, and hypertension (Hurley et al., 2009). Furthermore, the 2010 estimates determined that 68% of American adults are overweight or obese (Flegal, Carroll, Ogden, & Curtin, 2010).
Although the Dietary Guidelines for Americans promote healthy dietary patterns, it is estimated that as few as 3–4% of Americans follow all the national recommendations (Hornick, Krester, & Nicklas, 2008), and virtually no one meets recommendations for vegetable and whole grain consumption (Krebs-Smith, Guenther, Subar, Kirkpatrick, & Dodd, 2010). Overall, the typical American diet is low in micronutrient density and high in saturated fat, sugar, and sodium (Millen et al., 2005). Only 14% of American adults are consuming the Healthy People 2010 goals of two or more fruits and three or more vegetables per day, with the southeast region of the US particularly low in fruit and vegetable consumption (Centers for Disease Control and Prevention, 2009).
To prevent the morbidity and mortality associated with diet-related diseases, it is important to gain a greater understanding about modifiable influences of eating behavior, especially those beyond specific individual characteristics. It has been demonstrated that good social support is associated with a higher quality diet, but less is known about the contribution of family level factors such as family functioning to adult dietary patterns. Family functioning may be an important modifiable target for interventions aimed at improving dietary quality among adults. The purpose of this study was to examine several intrapersonal (depressive symptoms and perceived stress) and interpersonal (family functioning and social support) factors related to diet quality in a healthy, working adult sample from an academic health center in the southeastern US. Examining dietary quality among employed health professionals was deemed important because of the significant influence that providers’ own lifestyle behaviors have on prioritizing health promotion activities with their patients (Zhu, Norman & While, 2011).
Conceptual Framework
The conceptual framework that guided this study was the ecological model of health behavior as adapted by Story and colleagues (2008) for eating behavior. The adapted ecological model outlines four broad contexts of health influence defined in relation to eating behavior as:
intrapersonal (individual), including cognitions, skills and behavior, lifestyle, biological factors, and demographics;
interpersonal (social environments), including interactions with family, friends, peers, and community members;
settings (physical environments), including settings such as worksites, home, school, childcare, neighborhoods, restaurants, and retail food outlets
macro-level environment, encompassing the legislative and policy influences related to the food system.
Because eating behavior is complex and influenced by all these contexts, an ecological model is an ideal framework for understanding eating behavior. The ability to assess physical or macro-level environments exceeded the scope of this study, however, we examined influences of eating behavior beyond the more commonly examined individual level factors. Figure 1 depicts the ecological model adapted for this study. The intrapersonal (individual) and interpersonal (social/family) influences were posited to influence eating behavior, which then determined diet quality. We hypothesized that fewer depressive symptoms, lower perceived stress, better family functioning, and higher levels of social support would be associated with higher diet quality.
Figure 1. Adapted Ecological Framework for Influences on Eating Behavior and Diet Quality.
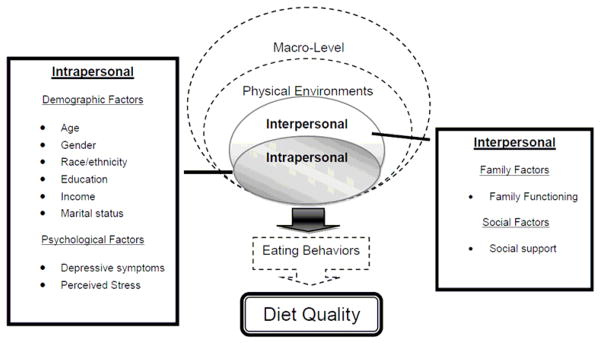
Note. The Ecological Framework for Eating Influences was adapted from Story et al. (2008). The intrapersonal and interpersonal factors as depicted in the boxes were assessed in this study.
Intrapersonal Influences
Intrapersonal or individual-level influences on healthy eating have been widely studied among many populations and many intrapersonal factors have been associated with diet quality. As depicted in Story et al.’s (2008) ecological framework, the intrapersonal influences include cognitions, skills and behavior, lifestyle, biological factors, and demographics. In this study, we examined selected demographic and cognitive or psychological factors known to influence diet quality. The demographic factors included age, gender, race/ethnicity, education, income, and marital status. Psychological factors examined were depressive symptoms and perceived stress.
Several demographic factors influence diet quality, with most investigators finding that increased age, higher education, higher income, and non-minority race/ethnicity are associated with higher diet quality (Barker et al., 2009; Rifas-Shiman, Rich-Edwards, Kleinman, Oken, & Gillman, 2009). Higher perceived stress, depression, and anxiety are strongly associated with poorer diet quality (Grossniklaus et al., 2010; Ng & Jeffery, 2003). Because a major critique of many nutrition studies is the singular focus on the individual with little focus on other possibly more influential factors such as family, social support, and environmental influences (Story et al., 2008), we also examined some interpersonal influences in relation to diet quality.
Interpersonal Influences
The interpersonal or social environment influences include interactions with family, friends, peers, and community members. For this study, we examined family-level influences and general social support. Family was defined broadly to include census (blood-relatives, marriage, adoption), biologic (genetic), household (cohabitants), and functional (involved in the everyday routines) configurations (Medalie & Cole-Kelly, 2002). Family functioning was examined through three dimensions; problem solving, defined as the family’s ability to resolve problems at a level sufficient for effective family functioning; communication, defined as how the family exchanges information; and overall general family functioning, which captures a snapshot of the multiple family functioning dimensions (Aarons, McDonald, Connelly, & Newton, 2007). Social support was defined as the perception and belief that one is cared for and loved, esteemed, and a member of a mutually obligated network or group (Cobb, 1976).
Family-Level Influences
Three main sources constitute the family-level influences on health: genetics, a shared physical environment, and a shared social environment (Medalie & Cole-Kelly, 2002). There is a substantial body of literature regarding the importance of family influence on children’s eating patterns (Pearson, Biddle & Gorely, 2009), but less attention has been devoted to family influences on adult eating patterns. This lack of study focus is particularly true for populations not on a prescriptive diet for a specific disease. Investigators who studied family functioning with adult diabetics and heart failure patients have found family functioning and support to be strongly related to dietary behavior (Dunbar, Clark, Quinn, Gary, & Kaslow, 2008; Wen, Parchman, & Sheperd, 2004).
Due to the multifactorial complexity of the obesity epidemic, there is a resurgence of interest in designing family-based interventions to target both childhood and adult obesity (Gruber & Haldeman, 2009). Although supportive social environments have been demonstrated to be beneficial in dietary change (Shaikh, Yaroch, Nebeling, Yeh, & Resnicow, 2008), Gruber and Haldeman (2009) suggested that the family is the social context most likely to support making health behavior changes. The family context provides support that directly affects health, specifically cardiovascular health (Heitman, 2004). Investigators conducting a population-based study to examine the contribution of family to health status determined that, depending on family structure, 4.5% - 26.1% of the variance in individual health status could be determined by family influences (Ferrer, Palmer, & Burge, 2005).
Social Support
Social support has long been recognized as an important influence on health and a major factor in determining diet quality and predicting success in diet-related interventions (Greaves et al., 2011). Particularly in interventions focused on improving adherence to prescriptive diets, higher levels of social support resulted in better dietary outcomes (Spahn et al., 2010). Social support is also a key influencing factor in determining diet quality among general populations (Lawrence et al., 2011). Furthermore, being married and marital relationship quality are important influences in determining prescriptive diet adherence (Kamphuis, et al., 2006; Trief, Ploutz-Snyder, Britton, & Weinstock, 2004).
Researchers have demonstrated the important role of social support and family in managing chronic disease, including adherence to dietary recommendations (Chang, Nitzke, Guilford, Adair, & Hazard, 2008; Dunbar et al., 2005; Dunbar et al., 2008; Rosland et al., 2008). Little is known specifically, however, about the influence of family functioning on diet quality among healthy adult populations. Examining the social relationships of family functioning and social support is an important next step in understanding social-environmental influences on healthy eating and diet quality.
Dietary Patterns
There has been a growing appreciation of the importance of assessing total dietary patterns, as opposed to single nutrients, especially in determining diet and disease associations (Hu, 2002). Diets high in fruits, vegetables, and whole grains, and low in saturated fat, sugar, and sodium are protective from chronic disease (Fung, Schulze, Manson, Willett, & Hu, 2004; Hu & Willett, 2002; Sonnenberg et al., 2005). One method of examining total diet quality is through diet indices or scores, which categorize the quality of the dietary pattern based on ‘a priori’ dietary recommendations or other specific diet patterns (Waijers, Feskens, & Ocke, 2007). Among the various available diet indices, three often examined in relation to chronic disease are the Alternate Healthy Eating Index (AHEI), the Dietary Approaches to Stopping Hypertension (DASH), and the Mediterranean Diet Score.
The AHEI was developed from the Healthy Eating Index (HEI)to measure a diet pattern that demonstrated greater protection from chronic disease (McCullough et al., 2002). The AHEI differs from the HEI by incorporating more specific dietary recommendations, such as moderate alcohol consumption, the ratio of red to white meat, detailed fat ratios, and multivitamin use. Since its development in 2002, the AHEI has been used in several studies to determine diet quality. Adherence to the AHEI pattern has demonstrated protection against multiple diseases, including risk of diabetes (Fung, McCullough, van Dam, & Hu, 2007), cardiovascular disease risk factors (Fargnoli et al., 2008), Parkinson’s disease risk factors (Gao et al., 2007), age-related macular degeneration(Montgomery et al., 2010), and colorectal cancer(Reedy et al., 2008).
Developed to test nutrition interventions for the treatment of hypertension, the Dietary Approaches to Stopping Hypertension (DASH) dietary pattern is now recommended in the Dietary Guidelines for Americans (U.S. Department of Agriculture [USDA] and U.S. Department of Health and Human Services [USDHHS], 2010). The DASH diet emphasizes an eating plan that is high in the consumption of fruits, vegetables, whole grains, and legumes, and low for the intake of sweets (Appel et al., 1997). Adherence to the DASH diet pattern resulted in significant reductions in blood pressure in the DASH trial (Harsha et al., 1999). The National Heart, Lung and Blood Institute, the National High Blood Pressure Education Program, the American Heart Association, and the Dietary Guidelines for Americans recommend the DASH eating plan for cardiovascular health(USDA and USDHHS, 2010; USDHHS, National Institutes of Health, 2004; USDHHS, 2006).
Investigators have examined the DASH eating pattern in association with other health outcomes. Greater adherence to the DASH eating pattern is associated with a decreased incidence of type 2 diabetes (Liese, Nichols, Sun, D’Agostino, & Haffner, 2009), and heart failure (Levitan, Wolk, & Mittleman, 2009), as well as decreased risk of colorectal adenoma (Dixon et al., 2007; Fung et al., 2010), and cardiovascular disease (Azadbakht et al., 2011; Chen, Maruthur, & Appel, 2010).
The third diet index, the Mediterranean Diet Score (MDS), was developed based on a traditional Greek diet that demonstrated protective effects from cardiovascular disease; it is characterized by high intakes of fruits, vegetables, legumes, whole grains, and fish (Trichopoulou, Costacou, Bamia, & Trichopoulos, 2003). Findings from many studies have demonstrated the beneficial health outcomes associated with adherence to a Mediterranean diet. These benefits include decreased risk for cardiovascular disease and stroke (Fung et al., 2009), type 2 diabetes (Kastorini & Panagiotakos, 2009), colorectal cancer (Dixon et al., 2007; Reedy et al., 2008), metabolic syndrome (Paletas et al., 2010), and improved longevity (Trichopoulou et al., 2003).
The three diet patterns and their associated indices share some commonalities in their scoring methodologies, specifically with the categorization of vegetables, fruits, and nuts/soy protein intake. There are some important differences among the diets, however, that make it useful to examine the quality of diet by all three indices. The DASH is the only index, for example, in which sugar and sodium intake are examined and scored. Assessing sugar and sodium intake is important because a high intake of highly processed, low nutrient foods is associated with increased sodium and sugar consumption (Millen et al., 2005). The AHEI and the MDS indices also examine alcohol intake and the ratio of white to red meat intake, both of which are associated with diet quality and disease outcomes (McCullough et al., 2002).
A last difference among the three diet indices is that multivitamin intake is only assessed with the AHEI. Currently, there is little research focused specifically on the use of multivitamins and diet quality or risk for chronic disease. A recent large cohort study of older adults, however, found no association between multivitamin use and risk for type 2 diabetes mellitus (T2DM; Song et al., 2011).
Because much remains to be learned about which specific nutrients or dietary components are related to chronic disease, we believed it was important to examine diet patterns and quality by multiple indices that highlight different dietary components (Hu, 2002). We specifically chose the AHEI, DASH, and MDS as measures of diet quality based on their demonstrated association with chronic disease reduction. Intrapersonal influences of depressive symptoms and perceived stress, along with interpersonal influences of family functioning and social support were examined in relation to each of the three dietary patterns. We hypothesized that fewer depressive symptoms, lower perceived stress, better family functioning, and higher levels of social support would be associated with higher diet quality.
Methods
Sample, Procedures, and Data Collection
Participants in this study were part of an ongoing prospective cohort predictive health study at a Southeastern university and health care institute. Recruitment methods have been described in greater detail elsewhere (Rask, Brigham, & Johns, 2011). Employees of the university and academic health center who had been employed at least 2 years, and were covered by a university-sponsored health insurance plan (N = 6464) were randomly sampled and invited to participate in the predictive health study. Every 10th employee from a master alphabetical list was invited to participate. Of those sampled and invited by email to participate, about 30% agreed to be screened, and 10% of those were enrolled based on the inclusion/exclusion criteria. Participants were asked to commit to the 5-year study with an assessment at baseline and 6 months during the first year and annually thereafter. Informed consent was obtained at the baseline visit by the Center staff.
Multiple health indicators were measured longitudinally, including psychosocial factors such as depressive symptoms, and perceived stress, habitual macro- and micronutrient intake, biomarkers of inflammation and oxidative stress, body composition measures, exercise tolerance and vascular function. Questionnaires were completed either via an internet-based data entry system or by hard-copy. Biological measures were obtained through blood tests, DexaScan, vascular ultrasound, and a treadmill exercise test. Only baseline results for demographics, psychosocial factors, and diet quality are reported in this analysis. As of December 2010, 640 enrollees had completed baseline measurements; they comprise the sample for this study. All study protocols were approved by the University Institutional Review Board.
Inclusion criteria were age ≥ 18 years, and no history in the preceding year of either –hospitalization due to acute or chronic disease, Axis I psychosocial disorder, a significant change in a chronic disease condition (e.g. hypertension or diabetes) requiring new medication, substance/drug abuse, or alcoholism. Exclusion criteria included current, active, malignant neoplasms or history of malignancies (other than localized basal cell cancer of skin) during the previous 5 years, any acute illness in the 2 weeks before baseline studies, inability to undergo study assessments over the course of the study, and inability to give informed consent.
Measures
Sociodemographic data were obtained by self-report on a form designed for this study. The form included personal demographic questions about birth date, gender, education and income level, marital status, and race/ethnicity.
Perceived stress
Perceived stress was measured with the 14-item Cohen Perceived Stress Scale (PSS). Scores range from 0–56, with higher perceived stress represented by higher scores with no designated cutoffs(Cohen, Kamarck, & Mermelstein, 1983). The scale has been tested in multiple samples, including a healthy, general adult population, and determined to have internal consistency with Cronbach’s alpha values of .75 and .86 (Cohen et al., 1983; Cohen, S. W. G., 1988). In this study, Cronbach’s alpha for the PSS was acceptable at .86.
Depressive symptoms
Depressive symptoms were measured with the 21-item Beck Depression Inventory II (BDI-II; Beck, Steer, & Brown, 1996). The BDI has with good internal consistency (alpha = .90) as demonstrated in a sample of community-dwelling, healthy adults (Segal, Coolidge, Cahill, & O’Riley, 2008). In this study, Cronbach’s alpha for the BDI-II was .84. Scores range from 0–63, with higher scores indicating more depressive symptoms. BDI-II scores of < 13 reflect minimal depression, scores of 14–19 reflect mild depression, scores of 20–28 indicate moderate depression, and scores ranging from 29–63 suggest severe depressive symptoms (Beck et al., 1996).
Social support
The measure of social support was the Enhancing Recovery in Coronary Heart Disease (ENRICHD) Social Support Instrument (ESSI), a 7-item scale developed to measure perceived social support among cardiac patients(Mitchell et al., 2003). The scale measures the structural, instrumental, and emotional aspects of social support. Scores range from 8–34, with those > 18 indicating high levels of social support. The instrument has demonstrated reliability (alpha = .86 and .88) in two adult samples with cardiovascular disease (Mitchell, et al., 2003; Vaglio et al., 2004). Cronbach’s alpha for the ESSI in this study was .86.
Family functioning
Three scales of the McMaster Family Assessment Device (FAD; Miller, Epstein, Bishop, & Keitner, 1985) were used to measure family functioning - the General Family Functioning scale (12-items), the Communication scale (9-items), and the Problem Solving scale (6-items). Scores for each scale are calculated by summing and averaging the responses, with each scale score ranging from 1–4. Higher scores indicate poorer functioning, with the unhealthy cutoff for the general family functioning scale set at > 2.0 and for the communication and problem solving scales at 2.2 (Kabacoff, Miller, Bishop, Epstein, & Keitner,1990; Miller, et al., 1985). The FAD has been validated in previous studies (Kabacoff, et al., 1990; Miller, et al., 1985). Reliability for a general community adult sample for each of the scales was adequate; α = .87 for general family functioning; alpha = .74 for communication; alpha = .74 for problem solving (Aarons et al., 2007). In this study, Cronbach’s alphas for each of the subscales were: General Family Functioning, .83; Family Communication, .85; Family Problem-Solving, .83.
Dietary intake
The 2005 Block Food Frequency Questionnaire (FFQ; NutritionQuest, 2009), a 110 food-item instrument that measures habitual intake over the previous year, was used to measure dietary intake. The analysis of the FFQ is provided by NutritionQuest, who distributes and analyzes the Block FFQ. The FFQ analyses include average daily total calories, serving sizes of major food groups, and micro- and macronutrients. For each participant, diet quality was defined and scored into the three diet indices– the AHEI, DASH, and MDS.
The AHEI was scored according to the methods designed by McCullough and colleagues (2002). Eight components, scored from 0 points to 10 points each, include vegetables, fruits, nuts and soy protein, the ratio of white to red meat, cereal fiber, trans fat, polyunsaturated to saturated fat ratio, and sex-specific alcohol intake. The ninth component, multivitamin use, was scored from 2.5–7.5, with 7.5 points awarded if multivitamin intake was greater than or equal to five years of multivitamin use, and 2.5 points awarded for less than five years of use. Maximum points were awarded if the participant’s dietary intake met the serving criteria, indicating a high level of dietary adherence. By contrast, a score of 0 (or 2.5 points for no multivitamin use) indicated the least adherence to that diet component. Intermediate intakes of all eight of the dietary components were scored proportionately between 0 and 10. The AHEI is scored from 2.5 to 87.5, with higher scores indicating better dietary quality (McCullough et al., 2002).
The DASH index used for this study was a modified version of the Folsom method (Folsom, Parker, & Harnack, 2007). Consistent with the Folsom method, we included 11 dietary components in the index, representing total grains, whole grains, vegetables, fruits, dairy foods, meats/poultry/fish, nuts/seeds/beans, sweets, sodium, and energy percentage from total fat and saturated fat. Instead of measuring the sweets consumption in servings per day, however, we measured the sweets intake as a percentage of total caloric intake as described by Dixon and colleagues (Dixon, 2007). A maximum score of 1 point was assigned in each dietary category to participants who met the specific DASH recommendations, 0.5 point was assigned to those who had more moderate intake, and 0 points were awarded to those who did not meet the specific recommendations. Total scores range from 0–11, with higher scores reflecting greater adherence to the DASH pattern.
The Mediterranean Diet Score was calculated as outlined by Trichopoulou et al. (2003). The MDS ranges from 0–9 with higher scores indicating greater adherence. Each dietary component is scored by assigning 1 point for daily servings of vegetables, fruit, legumes, cereals, fish, and ratio of monounsaturated to saturated fats of equal or greater value than the sex-specific median intake of the study sample. One point is assigned for moderate intake of alcohol, defined as 5–25 grams for women and 10–50 grams for men, with no points assigned for intakes outside these ranges. No points were assigned for meat and dairy servings that were higher than the sex-specific median intakes.
Data Analyses
Analyses were performed using SPSS 18. Prior to statistical analyses, all variables were examined for accuracy of data entry, missing values, and the assumptions for multivariate analysis. Due to the low representation of African-American, Asian, and other racial groups in the sample, race was regrouped into categories of white and non-white for the analysis. Dichotomization also was done for marital status – 62.3% were married and the remaining 37.7% were single, divorced, or widowed (these categories were collapsed into one category for “single”). This sample represented a very high income group, with more than 57% making greater than $100,000 per year. Therefore, income also was dichotomized at the approximate median level of $100,000 annual salary. Comparisons of means were made using t-tests (for normally distributed measures) and Mann-Whitney tests (for skewed measures). Comparisons of proportions were made using Chi-square tests of association. Bivariate associations between continuous measures were assessed using Pearson’s product-moment correlation coefficient for normally distributed measures and Spearman’s Rho for ordinal or skewed measures. To determine the association between demographic factors and psychosocial measures in relation to diet quality, stepwise multiple linear regression models were created separately for the AHEI, DASH and MDS dietary scores, each evaluated as continuous variables.
We found underlying multicollinearity between the intrapersonal demographic, intrapersonal psychological, and interpersonal family and social variables, with correlations greater than .3 noted between: income and race; marital status and education; marital status and social support; depressive symptoms, perceived stress, and all three subscales of the FAD; perceived stress, social support, and all three subscales of the FAD; and between social support and all three subscales of the FAD. Stepwise variable selection methods (probability of F using .05 for entry and .10 for removal) were used for building the multiple linear regression models. The variables considered for inclusion in each model were: the intrapersonal demographic variables of gender, age, income (dichotomized <$100K, ≥ $100K), race (dichotomized white, non-white), marital status (dichotomized married, non-married), and education; the intrapersonal psychological variables of depressive symptoms (BDI-II) and perceived stress; and the interpersonal variables of social support (ESSI) and three subscales of the FAD - general family functioning (GFF), family problem-solving (PS), and family communication (Comm) scores.
Results
Study Population
Participants included 640 working adults, 67.7% women, 70% Caucasian, 25%African-American, mean age 48 (SD = 11.2) years (Table 1). Most participants had 4years of college or more (81%), 58% had an annual income greater than $100,000, and 62% were married. Mean body mass index (BMI) was 28 (SD = 6.4), with 66% of participants classified as overweight or obese.
Table 1.
Characteristics of the Study Population
| Characteristics | n | Study Sample |
|---|---|---|
| Age, mean years (SD) | 640 | 48.0 (11.2) |
| Women, % | 637 | 67.7 |
| Race, % | 632 | |
| White | 69.8 | |
| African-American | 24.8 | |
| Asian | 4.8 | |
| American Indian/Alaska Native | 0.5 | |
| Education, % | 637 | |
| < 4 years college | 19.3 | |
| ≥ 4 years college | 80.7 | |
| Income, % | 601 | |
| <$100,000/year | 42.3 | |
| ≥$100,000/year | 57.7 | |
| Marital status, % | 637 | |
| Married | 62.3 | |
| BMI, mean (SD) | 630 | 28.0 (6.4) |
| Perceived Stress, mean (SD) | 609 | 19.74 (7.1) |
| Depressive symptoms, mean (SD) | 595 | 5.5 (5.4) |
| Social support, mean (SD) | 593 | 28.0 (5.1) |
| Family Assessment: | 591 | |
| General Family Functioning, mean (SD) | 1.76 (0.49) | |
| Healthy, % | 64.3 | |
| Unhealthy, % | 35.7 | |
| Communication, mean (SD) | 589 | 1.97 (0.47) |
| Healthy, % | 66.6 | |
| Unhealthy, % | 33.4 | |
| Problem-Solving, mean (SD) | 591 | 1.92 (0.48) |
| Healthy, % | 80.9 | |
| Unhealthy, % | 19.1 |
The mean perceived stress score of 19.7 (SD = 7.1)was comparable to other nonclinical populations (Cohen, S. W. G., 1988). The majority of the sample reported minimal depressive symptoms and high social support, 91% and 93%, respectively. Over half the respondents reported good general family functioning (64%), healthy family problem-solving (81%), and healthy family communication (67%). The demographic characteristics and psychosocial results of the sample are highlighted in Table 1.
Table 2 displays the mean intake by gender for all nutrients that comprised the dietary indices. The AHEI scoring methodology and the results for each of the AHEI dietary components are summarized in Table 3. AHEI scores ranged from 13.5–75.5 with a mean of 47.8 (SD = 10.6). A summary of the DASH scoring methodology, along with individual dietary component results, is depicted in Table 4. Total DASH scores ranged from 1–9 with a mean of 4.41 (SD = 1.29). The MDS scoring was based on the median intake of the sample for men and women separately; the median cutoff points that determined the scoring for this sample are summarized in Table 5. Mediterranean Diet Scores ranged from 0–9 with a mean of 4.44 (SD = 1.78). The dietary scores were all correlated, r’s ranging from .52 to .73, with the MDS and the AHEI sharing the highest correlation.
Table 2.
Consumption of Foods and Nutrients
| Component | Intake for Men n = 204 M (SD) |
Intake for Women n = 431 M (SD) |
|---|---|---|
| Kilocalories | 1922.46 (741.96) | 1621.80 (608.60) |
| Vegetables, (servings/day) | 2.25 (1.07) | 2.29 (1.12) |
| Fruit, (servings/day) | 1.44 (0.87) | 1.34 (0.82) |
| Nuts and soy protein | ||
| (servings/day) | 1.31 (1.25) | 1.3 (1.13) |
| (servings/week) | 9.15 (8.72) | 9.10 (7.91) |
| Total Meat, (servings/day) | 2.80 (2.15) | 2.23 (1.56) |
| Total Fish, (servings/day) | 0.92 (0.81) | 0.88 (0.91) |
| Ratio of white to red meat | 1.60 (3.57) | 2.0 (3.46) |
| Total Grain, (servings/day) | 5.52 (2.57) | 4.51 (2.28) |
| Whole Grain, (servings/day) | 1.44 (0.96) | 1.23 (0.88) |
| Cereal fiber, (grams/day) | 20.98 (8.80) | 19.86 (9.31) |
| Total Fat, (grams/day) | 95.91 (36.31) | 65.25 (27.82) |
| Saturated fatty acids, (% of energy) | 10.13 (2.51) | 10.20 (2.38) |
| Ratio of monounsaturated fat to saturated fat | 1.42 (0.32) | 1.47 (0.37) |
| Trans Fat, (% of energy) | 2.43 (7.41) | 3.34 (10.64) |
| Ratio of Polyunsaturated to | 0.86 (0.28) | 0.90 (0.29) |
| Saturated Fat | ||
| Sodium, (mg/day) | 3193.17 (1275.50) | 2760.83 (1111.79) |
| Duration of multivitamin use, (years) | 4.82(1.91) | 4.69(2.17) |
| Alcohol | ||
| (servings/day) | 1.19 (1.33) | 0.57 (0.79) |
| (grams/day) | 15.43 (17.34) | 7.41 (10.32) |
Table 3.
AHEI Scoring Method and the Study Population Scores
| Component | Criteria for minimum scorea | Criteria for maximum scorea | Mean intakes for Men | Mean intakes for Women | AHEI mean scores |
|---|---|---|---|---|---|
| Vegetables (servings/day) | 0 | 5 | 2.25 (1.07) | 2.29 (1.12) | 4.05 (2.24) |
| Fruit (servings/day) | 0 | 4 | 1.44 (0.87) | 1.34 (0.82) | 2.94 (2.09) |
| Nuts and soy protein (servings/day) | 0 | 1 | 1.31 (1.25) | 1.30 (1.13) | 7.32 (3.18) |
| Ratio of white to red meat | 0 | 4 | 1.60 (3.57) | 2.00 (3.46) | 3.16 (2.93) |
| Cereal fiber (grams/day) | 0 | 15 | 20.98 (8.80) | 19.86 (9.31) | 9.20 (1.70) |
| Trans Fat (% of energy) | >4 | <0.5 | 2.43 (7.41) | 3.34 (10.64) | 7.66 (2.05) |
| Polyunsaturated to Saturated Fat ratio | <0.1 | >1 | 0.86 (0.28) | 0.90 (0.29) | 8.18 (1.65) |
| Duration of multivitamin useb | <5 y | >5 y | 4.82 (1.91) | 4.69 (2.17) | 3.97 (2.27) |
| Alcohol (servings/day) | Men: 0 or >3.5 |
Men: 1.5–2.5 |
1.19 (1.33) | 0.57 (0.79) | Men: 1.72 (3.61) |
| Women: 0 or >2.5 |
Women: 0.5–1.5 |
Women: 2.80 (4.34) |
|||
|
|
|||||
| Total AHEI score | |||||
| Men | |||||
| Range | 13.5 – 76.5 | ||||
| Mean (SD) | 47.6 (10.4) | ||||
| Women | |||||
| Range | 21.5 – 77.5 | ||||
| Mean (SD) | 49.5 (11.3) | ||||
| All | |||||
| Range | 13.5 – 77.5 | ||||
| Mean (SD) | 48.9 (11.0) | ||||
Note.
Intermediate intakes were scored proportionately between 0 and 10.
Minimum score is 2.5 and maximum score is 7.5.
Table 4.
DASH Scoring method and the Study Population Scores
| Component | Criteria for minimum score of 0 | Criteria for moderate score of 0.5 | Criteria for maximum score of 1 | Mean intakes |
|---|---|---|---|---|
| Vegetables (servings/day) | <2 | 2–3 | ≥4 | 2.28 (1.13) |
| Fruit (servings/day) | <2 | 2–3 | ≥4 | 1.38(0.83) |
| Nuts and soy protein (servings/week) | <2 | 2–3 | ≥4 | 9.13 (8.17) |
| Meat/poultry/fish (servings/day) | ≥4 | 3 | ≤2 | 2.45 (1.79) |
| Total Grain (servings/day) | <5 | 5–6 | ≥7 | 4.83 (2.42) |
| Whole Grain (servings/day) | <1 | 1 | ≥2 | 1.30 (0.92) |
| Dairy (servings/day) | <1 | 1 | ≥2 | 1.24 (0.82) |
| Total fat (% of energy) | ≥33 | 31–32 | ≤30 | 35.14 (7.17) |
| Saturated fatty acids (% of energy) | ≥13 | 11–12 | ≤10 | 10.17 (2.42) |
| Sweets (% of energy) | ≥5.1 | 3.3–5.0 | ≤3.2 | 11.43(7.51) |
| Sodium (milligrams/day) | ≥2401 | 1501–2400 | ≤1500 | 2898.26 (1807.50) |
| Total score | 4.4 (1.3) |
Table 5.
Mediterranean Diet Score Cutoff Points in the Study Population
| Component | Median cutoff for men | Median cutoff for women |
|---|---|---|
| Vegetables1 (servings/day) | 1.965 | 2.130 |
| Fruit1 (servings/day) | 1.315 | 1.190 |
| Nuts and soy protein1 (servings/week) | 0.963 | 0.976 |
| Fish1 (servings/day) | 0.695 | 0.634 |
| Total Grain1 (servings/day) | 5.310 | 4.070 |
| Meat2 (servings/day) | 2.935 | 2.035 |
| Dairy2 (servings/day) | 1.205 | 0.969 |
| Ratio of monounsaturated fat to saturated fat1 | 1.345 | 1.402 |
| Alcohol3 (grams/day) | 10–50 | 5–25 |
Note.
Intakes above this median receive a score of 1, and below the intake, receive a 0.
Intakes below this median, receive a score of 1, and above the intake, receive a 0.
Intakes within these ranges receive a score of 1, and outside the range, receive a 0.
Demographic, Psychosocial Factors and Diet Quality Scores
For dietary quality measured by the AHEI, the final model included the demographic variables of gender, age, and race and the interpersonal variable, social support (ESSI). Together, these variables explained 6.2% of the variance in AHEI (Table 6). For dietary quality measured by the DASH, the only demographic variable to remain in the model was race, and social support was the only interpersonal variable retained. Race and social support explained 2.6% of the variance in diet quality. In the regression model for MDS, both demographic variables of race and education and the interpersonal variable of social support were significant. Together these three variables accounted for 3.8% of variance in diet quality as measured by the MDS.
Table 6.
Multiple Linear Regression Analysis for Intrapersonal and Interpersonal Variables and AHEI, DASH and MDS Indices
| Variable | B | SE B | β | p-value |
|---|---|---|---|---|
| Outcome: AHEI (n = 568) | Model adjusted R2 = .062 (p<.001) | |||
|
| ||||
| Intercept constant | 31.154*** | 4.101 | .001 | |
| Gender | 3.080** | 0.985 | 0.130 | .002 |
| Age | 0.141*** | 0.042 | 0.141 | .001 |
| Race | −2.883** | 1.000 | −0.121 | .004 |
| Social Support | 0.330*** | 0.088 | 0.153 | .000 |
| Outcome: DASH (n = 506) | Model adjusted R2 = .026 (p=.001) | |||
|
| ||||
| Intercept constant | 3.856*** | 0.369 | .001 | |
| Race | −0.303* | 0.129 | −0.104 | .019 |
| Social Support | 0.033** | 0.011 | 0.129 | .003 |
| Outcome: MEDI (n=574) | Model adjusted R2 = .038 (p<.001) | |||
|
| ||||
| Intercept constant | 2.998*** | 0.571 | .001 | |
| Education | 0.043* | 0.017 | 0.108 | .011 |
| Race | −0.391* | 0.164 | −0.101 | .017 |
| Social Support | 0.038** | 0.015 | 0.109 | .008 |
Note: AHEI = Alternate Healthy Eating Index; DASH = Dietary Approaches to Stopping Hypertension; MDS = Mediterranean Diet Score. Variables Considered and Selection Using Stepwise Selection Method: intrapersonal demographic factors of Gender, Age, Race [white (1)/non-white (2)], Marital Status [single (1)/married (2)], Education, Income [<$100K (0)/≥$100K (1)]; intrapersonal factors of Depressive Symptoms and Perceived Stress; and family and social Factors of FAD-GFF = general family functioning, FAD-PS = family problem-solving, FAD-Comm = family communication, and Social Support. β indicates standardized coefficients.
Discussion
In this study of 640 healthy, employed adults, we expected that fewer depressive symptoms, lower perceived stress, better family functioning, and higher levels of social support would be associated with higher diet quality. Our findings support the relationship between higher levels of social support and better diet quality. Stronger social support was modestly, but significantly, associated with better dietary quality represented by diet scores from all three indices - the AHEI, DASH, and MDS. That these associations were modest is likely related to the low variance in social support; 93% of the sample reported high social support, so there were few participants with low levels of social support. The expected influence of family functioning, however, was not found. This may be due to the stronger association of social support with diet quality. Furthermore, social support and family functioning may not be independent, distinctive concepts as evidenced by the significant correlation between social support (ESSI) and all three subscales of the Family Assessment Device (r = −.46, −.51, −.53). Aspects of family functioning may be considered a part of the larger concept of overall social support and should be investigated further. Certain demographic variables were associated with dietary quality but differed based on the diet index, although minority race was associated with poorer diet quality in all three indices. Our findings are similar to findings from a systematic review in which the authors reported that higher income and being married (a possible surrogate marker for higher social support) were the most influential factors in determining higher fruit and vegetable intake(Kamphuis et al., 2006).
Participants of both genders reported better diet quality as defined by the AHEI than in the study conducted by McCullough and colleagues (2002). There was less difference, however, between men in our study and those in McCullough et al.’s, (M = 47.6, SD = 10.4) versus 45 (SD = 11.1)than for women, (M = 49.6, SD = 11.3)versus 38.4 (SD = 10.3) in the McCullough et al. study (2002). In our study, the dietary components that were least likely to be consistent with USDA dietary guidelines included lower intakes of fruits, vegetables, and dairy, and higher intakes of sweets and sodium. This non-adherence with the guidelines is comparable with findings of a recent study of the general US population which showed that a very low percentage of individuals living in the US are consuming diets that meet all major federal dietary recommendations (Krebs-Smith et al., 2010).
Although the predictive health study initiative from which these data were derived is not designed as a worksite health program, its participants are largely drawn from the work setting. In a recent review of worksite dietary interventions it was determined that most programs focused on diet education resulted in only moderate improvements in dietary intake(Ni Mhurchu, Aston, & Jebb, 2010). The investigators concluded that there is a need to intervene at multiple levels of the work environment to really have any significant improvement in dietary quality. Our findings suggest an opportunity to focus greater attention on diet quality through worksite interventions that focus on increased social support.
Findings from our analysis show there is a significant opportunity to improve diet quality even in a population with relatively high socioeconomic resources. Because poor diet quality is often associated with lower income and education (Darmon & Drewnowski, 2008), many nutrition interventions are targeted to lower resource population groups. Our data suggest, however, that this focus should also be expanded to higher resource groups. Improving diet quality among health care providers is especially critical, given the significant influence that providers’ own lifestyle behaviors have on prioritizing health promotion activities with their patients (Zhu et al., 2011).
Limitations and Strengths
Several limitations to this study are worth noting. First, this study was based on a cross sectional design with secondary analysis of the baseline data from a larger predictive health study. Consequently, no conclusions can be drawn about temporal sequence in the association between demographic or psychosocial factors and diet quality. Factors that may influence diet quality were limited to the variables selected for the larger study and this restricted the explanatory possibilities for understanding variance in diet quality. The complexity of understanding influences of eating behavior and diet quality is underscored by the small amount of variance in diet quality explained by the variables that we examined. Future studies examining influences on diet quality in a working, adult population would be enhanced by assessing environmental and policy components consistent with the ecological model as adapted by Story and colleagues (2008) for eating behavior. For example, inadequate workplace nutrition quality and work environments that do not support mealtime breaks have been identified as contributing to poor diet quality among health care professionals (Lemaire, Wallace, Dinsmore, & Roberts, 2011). Other important influences on diet quality may also include time constraints (Welch, McNaughton, Hunger, Hume, & Crawford, 2009), or self efficacy for healthy eating (Shaikh et al., 2008), access/availability, and cost (Williams, Thornton& Crawford, 2011). Future study specifically of family and social-level influences should broaden the focus beyond family functioning and general social support. Finally, the 10% enrollment rate of potentially eligible participants due to inclusion/exclusion criteria and inability to commit to the time requirements of the study may limit the generalizability of our findings. Specifically, our study sample tended to be psychosocially healthy, primarily white, female, married, and highly educated with high incomes.
This study also has notable strengths. To the authors’ knowledge, this is the first study in which these three dietary indices were calculated from the Block Food Frequency Questionnaire (FFQ). Although we do not think that calculating dietary quality from the FFQ rather than from a 24-hour recall or 3-day food record had any significant impact on the outcomes, it is worth confirming that the dietary index calculations are possible with the commonly utilized FFQ instrument. As noted in recent reviews of national data, dietary quality is relatively poor among the general American population (Krebs-Smith et al., 2010). Findings from our study illustrate that even in a sample where participants worked in an academic health setting and had a number of resources available, overall diet quality was moderate and non-adherent to the Dietary Guidelines for Americans. Traditional risk factors, including low income, low education, and depression, that are typically associated with poor diet quality do not account for the inadequate diet quality found in this study. Our dataunder score the complexity of the influences on diet quality and support further study of physical and macro-level environmental influences.
Conclusion
Comparable to national data, results from this study highlight the inadequate diet of many American adults. Our findings suggest that improving social support may be an important strategy to improve overall diet quality. Furthermore, the worksite may be astrategic environment in which to test interventions targeted at improved social support to enhance diet quality. It is evident that the traditional focus on intrapersonal factors of socioeconomic status and demographic factors may not offer any new insight into explaining or addressing improvements in dietary quality. Future research and interventions should be directed beyond the individual-level to a population approach that addresses broader social and environmental influences.
Acknowledgments
Financial Support: Supported in part by PHS Grant (TL1RR025010) from the Clinical and Translational Science Award program, National Institutes of Health, National Center for Research Resources and the Center for Health Discovery and Well Being Study (CHDWB) is supported by the CF Foundation, Inc., and Emory University.
Contributor Information
Erin Poe Ferranti, Email: epoe@emory.edu, Doctoral Student, Nell Hodgson Woodruff School of Nursing, Emory University, 1520 Clifton Road, NE, Atlanta, GA 30322, Telephone: 404-808-3685; Fax: 404-727-0536.
Sandra B. Dunbar, FAHA Associate Dean for Academic Advancement, Charles Howard Candler Professor of Cardiovascular Nursing, Nell Hodgson Woodruff School of Nursing, Emory University.
Melinda Higgins, Associate Research Professor/Senior Biostatistician, Nell Hodgson Woodruff School of Nursing, Emory University.
Jun Dai, Assistant Professor, The Department of Applied Health Science, Indiana University, Bloomington, IN.
Thomas R. Ziegler, Professor, School of Medicine, Emory University.
Jennifer K. Frediani, Bionutrition Research Director, School of Medicine, Emory University.
Carolyn Reilly, Assistant Professor, Nell Hodgson Woodruff School of Nursing, Emory University.
Kenneth L. Brigham, Associate Vice-President for Health Affairs and Director of the Predictive Health Institute, Emory University.
References
- Aarons GA, McDonald EJ, Connelly CD, Newton RR. Assessment of family functioning in Caucasian and Hispanic Americans: Reliability, validity, and factor structure of the Family Assessment Device. Family Process. 2007;46:557–569. doi: 10.1111/j.1545-5300.2007.00232.x. [DOI] [PubMed] [Google Scholar]
- Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. The New England Journal of Medicine. 1997;336:1117–1124. doi: 10.1056/nejm199704173361601. [DOI] [PubMed] [Google Scholar]
- Azadbakht L, Fard NR, Karimi M, Baghaei MH, Surkan PJ, Rahimi M, Willett WC. Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients: A randomized crossover clinical trial. Diabetes Care. 2011;34:55–57. doi: 10.2337/dc10-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker M, Lawrence W, Crozier S, Robinson S, Baird J, Margetts B, Cooper C. Educational attainment, perceived control and the quality of women’s diets. Appetite. 2009;52:631–636. doi: 10.1016/j.appet.2009.02.011. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. BDI-II Manual. 2. San Antonio, TX: Harcourt Brace & Company; 1996. [Google Scholar]
- Centers for Disease Control and Prevention. State indicator report on fruits and vegetables, 2009. 2009 Retrieved from http://www.fruitsandveggiesmatter.gov/downloads/StateIndicatorReport2009.pdf.
- Chang MW, Nitzke S, Guilford E, Adair CH, Hazard DL. Motivators and barriers to healthful eating and physical activity among low-income overweight and obese mothers. Journal of the American Dietetic Association. 2008;108:1023–1028. doi: 10.1016/j.jada.2008.03.004. [DOI] [PubMed] [Google Scholar]
- Chen ST, Maruthur NM, Appel LJ. The effect of dietary patterns on estimated coronary heart disease risk: Results from the Dietary Approaches to Stop Hypertension (DASH) trial. Circulation Cardiovascular quality and outcomes. 2010;3:484–489. doi: 10.1161/circoutcomes.109.930685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb S. Presidential Address-1976. Social support as a moderator of life stress. Psychosomatic Medicine. 1976;38:300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen SWG. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage; 1988. pp. 31–67. [Google Scholar]
- Darmon N, Drewnowski A. Does social class predict diet quality? American Journal of Clinical Nutrition. 2008;87:1107–1117. doi: 10.1093/ajcn/87.5.1107. [DOI] [PubMed] [Google Scholar]
- Dixon LB, Subar AF, Peters U, Weissfeld JL, Bresalier RS, Risch A, Hayes RB. Adherence to the USDA Food Guide, DASH Eating Plan, and Mediterranean dietary pattern reduces risk of colorectal adenoma. Journal of Nutrition. 2007;137:2443–2450. doi: 10.1093/jn/137.11.2443. [DOI] [PubMed] [Google Scholar]
- Dunbar SB, Clark PC, Deaton C, Smith AL, De AK, O’Brien MC. Family education and support interventions in heart failure: A pilot study. Nursing Research. 2005;54:158–166. doi: 10.1097/00006199-200505000-00003. [DOI] [PubMed] [Google Scholar]
- Dunbar SB, Clark PC, Quinn C, Gary RA, Kaslow NJ. Family influences on heart failure self-care and outcomes. Journal of Cardiovascular Nursing. 2008;23:258–265. doi: 10.1097/01.JCN.0000305093.20012.b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fargnoli JL, Fung TT, Olenczuk DM, Chamberland JP, Hu FB, Mantzoros CS. Adherence to healthy eating patterns is associated with higher circulating total and high-molecular-weight adiponectin and lower resistin concentrations in women from the Nurses’ Health Study. The American Journal of Clinical Nutrition. 2008;88:1213–1224. doi: 10.3945/ajcn.2008.26480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer RL, Palmer R, Burge S. The family contribution to health status: A population-level estimate. Annals of Family Medicine. 2005;3:102–108. doi: 10.1370/afm.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Folsom AR, Parker ED, Harnack LJ. Degree of concordance with DASH diet guidelines and incidence of hypertension and fatal cardiovascular disease. American Journal of Hypertension. 2007;20:225–232. doi: 10.1016/j.amjhyper.2006.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung TT, Hu FB, Wu K, Chiuve SE, Fuchs CS, Giovannucci E. The Mediterranean and Dietary Approaches to Stop Hypertension (DASH) diets and colorectal cancer. The American Journal of Clinical Nutrition. 2010;92:1429–1435. doi: 10.3945/ajcn.2010.29242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung TT, McCullough M, van Dam RM, Hu FB. A prospective study of overall diet quality and risk of type 2 diabetes in women. Diabetes Care. 2007;30:1753–1757. doi: 10.2337/dc06-2581. [DOI] [PubMed] [Google Scholar]
- Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119:1093–1100. doi: 10.1161/circulationaha.108.816736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung TT, Schulze M, Manson JE, Willett WC, Hu FB. Dietary patterns, meat intake, and the risk of type 2 diabetes in women. Archives of Internal Medicine. 2004;164:2235–2240. doi: 10.1001/archinte.164.20.2235. [DOI] [PubMed] [Google Scholar]
- Gao X, Chen H, Fung TT, Logroscino G, Schwarzschild MA, Hu FB, Ascherio A. Prospective study of dietary pattern and risk of Parkinson disease. The American Journal of Clinical Nutrition. 2007;86:1486–1494. doi: 10.1093/ajcn/86.5.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greaves CJ, Sheppard KE, Abraham C, Hardeman W, Roden M, Evans PH, Schwarz P Image Study Group. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11(119) doi: 10.1186/1471-2458-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossniklaus DA, Dunbar SB, Tohill BC, Gary R, Higgins MK, Frediani J. Psychological factors are important correlates of dietary pattern in overweight adults. The Journal of Cardiovascular Nursing. 2010;25:450–460. doi: 10.1097/JCN.0b013e3181d25433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber KJ, Haldeman LA. Using the family to combat childhood and adult obesity. Preventing Chronic Disease. 2009;6(3):A106. [PMC free article] [PubMed] [Google Scholar]
- Harsha DW, Lin PH, Obarzanek E, Karanja NM, Moore TJ, Caballero B. Dietary Approaches to Stop Hypertension: A summary of study results. DASH Collaborative Research Group. Journal of the American Dietetic Association. 1999;99(8 Suppl):S35–39. doi: 10.1016/s0002-8223(99)00414-9. [DOI] [PubMed] [Google Scholar]
- Heitman LK. Social support and cardiovascular health promotion in families. Journal of Cardiovascular Nursing. 2004;19:86–91. doi: 10.1097/00005082-200401000-00013. [DOI] [PubMed] [Google Scholar]
- Hornick BA, Krester AJ, Nicklas TA. Menu modeling with MyPyramid food patterns: Incremental dietary changes lead to dramatic improvements in diet quality of menus. Journal of the American Dietetic Association. 2008;108:2077–2083. doi: 10.1016/j.jada.2008.09.010. [DOI] [PubMed] [Google Scholar]
- Hu FB. Dietary pattern analysis: A new direction in nutritional epidemiology. Current Opinion in Lipidology. 2002;13(1):3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- Hu FB, Willett WC. Optimal diets for prevention of coronary heart disease. JAMA. 2002;288:2569–2578. doi: 10.1001/jama.288.20.2569. [DOI] [PubMed] [Google Scholar]
- Hurley KM, Oberlander SE, Merry BC, Wrobleski MM, Klassen AC, Black MM. The healthy eating index and youth healthy eating index are unique, nonredundant measures of diet quality among low-income, African American adolescents. Journal of Nutrition. 2009;139:359–364. doi: 10.3945/jn.108.097113. 11910.1186/1471-2458-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabacoff RI, Miller I, Bishop DS, Epstein NB, Keitner GI. A psychometric study of the McMaster Family Assessment Device in psychiatric, medical, and nonclinical samples. Journal of Family Psychology. 1990;3:431–439. [Google Scholar]
- Kamphuis CBM, Giskes K, de Bruijn GJ, Wendel-Vos W, Brug J, van Lenthe FJ. Environmental determinants of fruit and vegetable consumption among adults: A systematic review. British Journal of Nutrition. 2006;96:620–635. doi: 10.1079/bjn20061896. [DOI] [PubMed] [Google Scholar]
- Kastorini CM, Panagiotakos DB. Dietary patterns and prevention of type 2 diabetes: From research to clinical practice; A systematic review. Current Diabetes Reviews. 2009;5:221–227. doi: 10.2174/157339909789804341. [DOI] [PubMed] [Google Scholar]
- Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. The Journal of Nutrition. 2010;140:1832–1838. doi: 10.3945/jn.110.124826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence W, Schlotz W, Crozier S, Skinner TC, Haslam C, Robinson S, Inskip H, Univ S. Specific psychological variables predict quality of diet in women of lower, but not higher, educational attainment. Appetite. 2011;56:46–52. doi: 10.1016/j.appet.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemaire JB, Wallace JE, Dinsmore K, Roberts D. Food for thought: An exploratory study of how physicians experience workplace nutrition. Nutrition Journal. 2011;10(1):18. doi: 10.1186/1475-2891-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitan EB, Wolk A, Mittleman MA. Relation of consistency with the dietary approaches to stop hypertension diet and incidence of heart failure in men aged 45 to 79 years. The American Journal of Cardiology. 2009;104:1416–1420. doi: 10.1016/j.amjcard.2009.06.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liese AD, Nichols M, Sun X, D’Agostino RB, Jr, Haffner SM. Adherence to the DASH diet is inversely associated with incidence of type 2 diabetes: The insulin resistance atherosclerosis study. Diabetes Care. 2009;32:1434–1436. doi: 10.2337/dc09-0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB, Willett WC. Diet quality and major chronic disease risk in men and women: Moving toward improved dietary guidance. American Journal of Clinical Nutrition. 2002;76:1261–1271. doi: 10.1093/ajcn/76.6.1261. [DOI] [PubMed] [Google Scholar]
- Medalie JH, Cole-Kelly K. The clinical importance of defining family. American Family Physician. 2002;65:1277–1279. [PubMed] [Google Scholar]
- Millen BE, Quatromoni PA, Pencina M, Kimokoti R, Nam BH, Cobain S, Kozak W, Appugliese DP, Ordovas J, D’Agostino RB. Unique dietary patterns and chronic disease risk profiles of adult men: The Framingham nutrition studies. Journal of the American Dietetic Association. 2005;105:1723–1734. doi: 10.1016/j.jada.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Miller IV, Epstein NB, Bishop DS, Keitner GI. The McMaster Family Assessment Device: Reliability and validity. Journal of Marital and Family Therapy. 1985;11:345–356. [Google Scholar]
- Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, Berkman LF. A short social support measure for patients recovering from myocardial infarction: The ENRICHD Social Support Inventory. Journal of Cardiopulmonary Rehabilitation. 2003;23:398–403. doi: 10.1097/00008483-200311000-00001. [DOI] [PubMed] [Google Scholar]
- Montgomery MP, Kamel F, Pericak-Vance MA, Haines JL, Postel EA, Agarwal A, Schmidt S. Overall diet quality and age-related macular degeneration. Ophthalmic Epidemiology. 2010;17:58–65. doi: 10.3109/09286580903450353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology. 2003;22:638–642. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- Ni Mhurchu C, Aston LM, Jebb SA. Effects of worksite health promotion interventions on employee diets: A systematic review. BMC Public Health. 2010;10:62. doi: 10.1186/1471-2458-10-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NutritionQuest. Assessment Tools and Analysis Services, 2010. 2009 Retrieved from http://www.nutritionquest.com/assessment/
- Paletas K, Athanasiadou E, Sarigianni M, Paschos P, Kalogirou A, Hassapidou M, Tsapas A. The protective role of the Mediterranean diet on the prevalence of metabolic syndrome in a population of Greek obese subjects. Journal of the American College of Nutrition. 2010;29:41–45. doi: 10.1080/07315724.2010.10719815. [DOI] [PubMed] [Google Scholar]
- Pearson N, Biddle SJ, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: A systematic review. Public Health Nutrition. 2009;12:267–283. doi: 10.1017/s1368980008002589. [DOI] [PubMed] [Google Scholar]
- Rask KJ, Brigham KL, Johns MME. Integrating comparative effectiveness research programs into predictive health: A unique role for academic health centers. Academic Medicine. 2011;86:718–723. doi: 10.1097/ACM.0b013e318217ea6c. 10.1097?ACM.0b013e318217ea6c. [DOI] [PubMed] [Google Scholar]
- Reedy J, Mitrou PN, Krebs-Smith SM, Wirfalt E, Flood A, Kipnis V, Subar AF. Index-based dietary patterns and risk of colorectal cancer: The NIH-AARP Diet and Health Study. American Journal of Epidemiology. 2008;168:38–48. doi: 10.1093/aje/kwn097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rifas-Shiman SL, Rich-Edwards JW, Kleinman KP, Oken E, Gillman MW. Dietary quality during pregnancy varies by maternal characteristics in Project Viva: A US cohort. Journal of the American Dietetic Association. 2009;109:1004–1011. doi: 10.1016/j.jada.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosland AM, Kieffer E, Israel B, Cofield M, Palmisano G, Sinco B, Heisler M. When is social support important? The association of family support and professional support with specific diabetes self-management behaviors. Journal of General Internal Medicine. 2008;23:1992–1999. doi: 10.1007/s11606-008-0814-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal DL, Coolidge FL, Cahill BS, O’Riley AA. Psychometric properties of the Beck Depression Inventory II (BDI-II) among community-dwelling older adults. Behavior Modification. 2008;32:3–20. doi: 10.1177/0145445507303833. [DOI] [PubMed] [Google Scholar]
- Shaikh AR, Yaroch AL, Nebeling L, Yeh MC, Resnicow K. Psychosocial predictors of fruit and vegetable consumption in adults: A review of the literature. American Journal of Preventive Medicine. 2008;34:535–543. doi: 10.1016/j.amepre.2007.12.028. [DOI] [PubMed] [Google Scholar]
- Song Y, Xu Q, Park Y, Hollenbeck A, Schatzkin A, Chen H. Multivitamins, individual vitamin and mineral supplements, and risk of diabetes among older U.S. adults. Diabetes Care. 2011;34:108–114. doi: 10.2337/dc10-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnenberg L, Pencina M, Kimokoti R, Quatromoni P, Nam BH, D’Agostino R, Millen B. Dietary and the metabolic syndrome in obese and non-obese Framingham women. Obesity Research. 2005;13:153–162. doi: 10.1038/oby.2005.20. [DOI] [PubMed] [Google Scholar]
- Spahn JM, Reeves RS, Keim KS, Laqautra I, Kellogg M, Jortberg B, Clark NA. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. Journal of the American Dietetic Association. 2010;110:879–891. doi: 10.1016/j.jada.2010.03.021. [DOI] [PubMed] [Google Scholar]
- Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annual Review of Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. New England Journal of Medicine. 2003;348:2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS. The relationship between marital quality and adherence to the diabetes care regimen. Annals of Behavioral Medicine. 2004;27:148–154. doi: 10.1207/s15324796abm2703_2. [DOI] [PubMed] [Google Scholar]
- United States Department of Agriculture and United States Department of Health and Human Services. Dietary Guidelines for Americans, 2010. Washington D.C: U.S. Government Printing Office; 2010. [Google Scholar]
- United States Department of Health and Human Services National Institutes of Health. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. 2004 (04-5230). Retrieved from http://www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf.
- United States Department of Health and Human Services, National Institutes of Health., National Heart Lung and Blood Institute. Your guide to lowering your blood pressure with DASH. 2006 (06-4082). Retrieved from http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf.
- Vaglio J, Jr, Conard M, Poston WS, O’Keefe J, Haddock CK, House J, Spertus JA. Testing the performance of the ENRICHD social support instrument in cardiac patients. Health and Quality of Life Outcomes. 2004;2:24. doi: 10.1186/1477-7525-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waijers PM, Feskens EJ, Ocke MC. A critical review of predefined diet quality scores. British Journal of Nutrition. 2007;97:219–231. doi: 10.1017/S0007114507250421. [DOI] [PubMed] [Google Scholar]
- Welch N, McNaughton SA, Hunter W, Hume C, Crawford D. Is the perception of time pressure a barrier to healthy eating and physical activity among women? Public Health Nutrition. 2009;12:888–895. doi: 10.1017/s1368980008003066. [DOI] [PubMed] [Google Scholar]
- Wen LK, Parchman ML, Shepherd MD. Family support and diet barriers among older Hispanic adults with type 2 diabetes. Family Medicine. 2004;36:423–430. [PubMed] [Google Scholar]
- Williams LK, Thornton L, Crawford D. Optimising women’s diets. An examination of factors that promote healthy eating and reduce the likelihood of unhealthy eating. Appetite. 2011;59:41–46. doi: 10.1016/j.appet.2012.03.014. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Diet, nutrition and the prevention of chronic diseases. 2003 Retrieved from http://whqlibdoc.who.int/trs/who_TRS_916.pdf. [PubMed]
- Zhu DQ, Norman IJ, While AE. The relationship between doctors’ and nurses’ own weight status and their weight management practices: A systematic review. Obesity Reviews. 2011;12:459–469. doi: 10.1111/j.1467-789X.2010.00821.x. [DOI] [PubMed] [Google Scholar]


