Abstract
Transnasal endoscopy (TNE) is an upper endoscopy method which is performed by the nasal route using a thin endoscope less than 6 mm in diameter. The primary goal of this method is to improve patient tolerance and convenience of the procedure. TNE can be performed without sedation and thus eliminates the risks associated with general anesthesia. In this way, TNE decreases the cost and total duration of endoscopic procedures, while maintaining the image quality of standard caliber endoscopes, providing good results for diagnostic purposes. However, the small working channel of the ultra-thin endoscope used for TNE makes it difficult to use for therapeutic procedures except in certain conditions which require a thinner endoscope. Biopsy is possible with special forceps less than 2 mm in diameter. Recently, TNE has been used for screening endoscopy in Far East Asia, including Japan. In most controlled studies, TNE was found to have better patient tolerance when compared to unsedated endoscopy. Nasal pain is the most significant symptom associated with endoscopic procedures but can be reduced with nasal pretreatment. Despite the potential advantage of TNE, it is not common in Western countries, usually due to a lack of training in the technique and a lack of awareness of its potential advantages. This paper briefly reviews the technical considerations as well as the potential advantages and limitations of TNE with ultra-thin scopes.
Keywords: Transnasal endoscopy, Transoral endoscopy, Ultra-thin endoscopy, Sedated endoscopy, Unsedated endoscopy
Core tip: Transnasal endoscopy with ultra-thin endoscopes improves patient tolerance and convenience of the procedure, prevents the risks associated with general anesthesia, and decreases the cost and total duration. However, there are some drawbacks of the procedure with the technical limitations of scopes. These are discussed briefly in this review.
INTRODUCTION
Conventional transoral endoscopy (TOE) is the standard diagnostic method used to visualize the upper part of the gastrointestinal tract, including the duodenum. It can be performed without sedation, using only a topical oropharyngeal anesthesia such as lidocaine spray, or under sedation, which generally results in better patient tolerance and comfort. Sedated TOE is more common in most developed countries, including Western Europe and the United States[1,2]. However, sedated TOE increases the risk of adverse cardio-respiratory events, especially in elderly patients and patients with co-morbidities, and requires careful patient monitoring and increased nursing time, which can increase the cost of the procedure[3-6]. Therefore, routine diagnostic TOE is currently being done without sedatives, using only topical or pharyngeal anesthesia, in many high volume endoscopy centers[7,8]. This approach significantly increases patient discomfort, which decreases the tolerability of the procedure, and thus could potentially decrease the quality of examination as a result of retching and general patient discomfort[9,10].
Unsedated transnasal upper endoscopy (TNE) using ultra-thin endoscopes (UTE), where the outer diameter is less than 6 mm, has been introduced as an alternative method to both sedated and unsedated TOE[11-15]. TNE has been performed predominantly in primary care health institutions and in private clinics to facilitate comfortable endoscopy without requiring sedative drugs[16-18]. Several studies have reported that unsedated TNE is safe, well tolerated and significantly reduces patient discomfort when compared to unsedated TOE[18-20]. TNE is also comparable to sedated TOE in terms of patient tolerance and comfort but is safer and cheaper than sedated TOE since it does not require deep anesthesia[21-24].
As mentioned above, although the advantages of TNE have been shown in a wide range of studies from many countries, there is a significant geographic disparity in the usage of unsedated TNE[19,25]. In Far East Asia, particularly Japan, TNE is very popular among endoscopists and nearly half of all endoscopies are currently done by the transnasal route[19,26]. However, in Western countries, approximately 2/3 of endoscopists are not aware of the advantages associated with this method or do not have the required training to perform TNE. A survey among 624 endoscopists from different European countries revealed that only 31% of respondents practice the procedure and 34% of them lack any formal training in the transnasal approach[27]. In addition, 74% of endoscopists practicing TNE use this technique in less than 20% of all eligible patients. In this survey, the most common responses for not adopting TNE into daily practice were uncertainties about its potential advantages and lack of training in the procedure. The reasons for its limited use by endoscopists trained in the procedure were concerns about image quality and maneuverability. This survey elucidates that many endoscopists are still not familiar with TNE and that there is great need to discuss the technical aspects and potential advantages of this novel endoscopic method.
TECHNICAL CONSIDERATIONS OF TRANSNASAL ENDOSCOPY
Transnasal endoscopes, also known as small-caliber, ultra-thin or ultra-slim endoscopes, are very similar to standard or slim endoscopes except for their outer diameter, which is less than 6 mm, and their working channel, which is usually only 2 mm in diameter. There are small differences in the outer diameter of transnasal scopes among different manufacturers. Scopes with outer diameters from 5 to 6 mm usually have both up-down and right-left knobs, similar to standard endoscopes. Transnasal scopes in which the outer diameter is less than 5 mm generally only have an up-down knob. The working length, bending capability and field of view for transnasal endoscopes are usually comparable with standard endoscopes. However, their working channel is not suitable for standard biopsy forceps and other endoscopic catheters. Thus, they require special biopsy forceps to enter through the narrow working channel. Their aspiration capacity is also limited due to the narrow working channel when compared to standard endoscopes with a working channel of at least 2.8 mm. A color image can be generated in transnasal endoscopes by a charge-coupled device (CCD) camera located in the tip of the scope. The image quality of transnasal endoscopes is comparable to that of standard endoscopes and previous studies were unable to find significant differences in their diagnostic capabilities when compared to standard endoscopes[22,28]. They do not require special video processors and light sources and are compatible with model processors of their manufacturer. They do not have high-definition video capture capabilities but some models have advanced imaging features such as narrow-band imaging[29]. The numbers of procedures that can be performed with an ultra-thin endoscope, as well as the cost of scopes and the length of warranty, are comparable to standard endoscopes. Reimbursement rate of TNE is same with unsedated TOE in most countries or they are paid under the same codes.
The main concern during a nasal endoscopic procedure, for both the endoscopist and the patient, is passing the scope through the nasal passageway. This makes nasal pretreatment and the application of local anesthesia one of the most critical aspects of the procedure. The methods for nasal pretreatment in TNE are not standardized[30]. The most common practice starts by applying topical lidocaine to the nostrils. A vasoconstrictor such as naphzoline or oxymetazoline may also be applied to facilitate decongestion. Topical anesthesia of the oropharynx with 1-2 sprays of lidocaine is also recommended. This allows the endoscopist to switch to an oral endoscope easily should the transnasal route fail. Using a special nasal catheter coated with an anesthetic gel can achieve good local anesthesia throughout the nasal passageway (see Figure 1). It is applied through the nostril which allows the patient to breathe the most easily and is removed after 4 to 5 min. The diameter of a 14/16 F catheter is very similar to the diameter of ultra-thin endoscopes, making it ideal for anesthetic gel application. Many studies addressing the utility of TNE have only used topical lidocaine application to the nostril using a spray or gauze/cotton swab instead of catheters for pretreatment, which makes good local anesthesia deep inside the nasal passage unlikely[18,21,31-33]. We believe pretreatment using a 14/16 F catheter to apply an anesthetic gel is the most reliable method to increase the tolerability and comfort of TNE. In our daily practice, we use a combination of lidocaine spray and a lidocaine coated catheter for an effective anesthesia.
Figure 1.
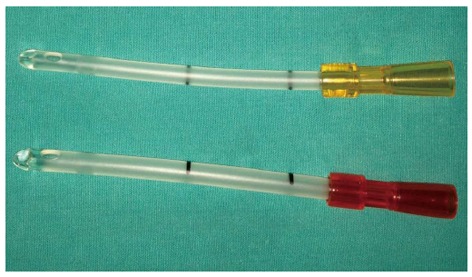
Pretreatment delivery catheter for transnasal endoscopy (Fujinon, Fujilm, Japan).
TNE is usually done when the patient is in the left lateral position. In special circumstances, it can also be performed in the sitting position. The understanding and orientation to the nasal anatomy facilitates transnasal endoscope insertion. Lubrication of the endoscope tip will help the passage into the nasopharyngeal space. The endoscope can be passed either along the floor of the nose or between the middle and inferior turbinate. It is important to apply gentle pressure on the shaft of the scope and avoid sudden movement as it enters the nose in order to prevent intranasal pressure and patient discomfort. Nasopharyngeal closure, tongue base, hypopharynx, vocal fold motion and pooling of oral secretions should all be evaluated during the procedure. The patient’s head should be flexed forward as the scope is passed into the upper esophageal sphincter. The patient should be asked to swallow as the scope is gently advanced, air is insufflated into the esophagus, and the entire length is then evaluated. At this point, the upper GI examination can be completed in an identical manner to a standard oral endoscopic procedure. If a biopsy sample is needed, it can be obtained using dedicated 1.8 mm biopsy forceps for TNE. During the removal of the endoscope, the tip should be kept in the middle of the lumen by hand control to prevent rubbing to the nasal septum and turbinates.
ADVANTAGES OF THE TRANSNASAL ROUTE
The greatest advantage of TNE when compared to conventional unsedated TOE is that it provides a more comfortable and tolerable procedure for the patient. The nasal route is less sensitive than the uvula, palatine arches and base of tongue, which minimizes the gag reflex and increases patient tolerance. Most studies comparing TNE with conventional unsedated TOE found that TNE is better tolerated and considerably reduces nausea, gagging, choking and overall patient discomfort[5,10,11,20,22,26]. In a current prospective, randomized study, our group compared TNE, using a 5.9 mm diameter ultra-thin endoscope, with unsedated TOE, using a 9.3 mm standard endoscope, in 400 patients undergoing an upper endoscopy for dyspeptic symptoms[34]. All patients were asked to complete a questionnaire using a 10 cm (10 point) visual analog scale (VAS) after the procedure. Mean VAS scores for throat pain, retching, breathlessness, abdominal discomfort/pain, tolerability, overall distress and difficulty of the procedure were significantly lower in TNE patients when compared to TOE patients (Table 1). A repeat procedure, if needed, was significantly more acceptable for TNE patients when compared to TOE patients (82.4% and 60.5%, respectively).
Table 1.
Patients’ evaluation of transnasal endoscopy and transoral endoscopy by visual analog scale (mean ± SD)[34]
| Evaluation criteria | TOE | TNE |
| Pain inside the nosea | 1.2 ± 0.7 | 3.4 ± 1.9 |
| Pain in the throata | 4.3 ± 2.5 | 1.7 ± 0.8 |
| Retching and breathlessness feelinga | 5.4 ± 3.1 | 2.1 ± 1.4 |
| Abdominal discomfort and paina | 3.9 ± 1.7 | 2.3 ± 1.2 |
| Tolerabilitya | 4.8 ± 2.4 | 2.6 ± 2.1 |
| Overall distress and difficultya | 4.4 ± 2.9 | 3.1 ± 1.8 |
TNE: Transnasal endoscopy; TOE: Transoral endoscopy. Visual analog scale: 0 = none; 10 = unbearable.
P < 0.05.
The results of studies comparing TNE with sedated TOE are controversial in terms of patient tolerance and acceptability. Stroppa et al[21] reported that TNE without sedation was better accepted than conventional sedated TOE in 30 patients who underwent both procedures on consecutive days. However, patient tolerance has been found to be similar or better in sedated TOE when compared to unsedated TNE in other studies[35-37]. Sedation, in general, causes extension of the total procedure time and increases the overall cost of the procedure[22,38]. In comparison to sedated TOE, TNE had fewer adverse effects on cardiopulmonary function and the autonomic nervous system[22,37,39]. This is likely due to the fact that TNE, with an ultra-thin scope, induces less sympathetic stimulation and causes smaller changes in both blood pressure and heart rate. In most studies, TNE was found to be safer, did not result in any adverse cardiovascular effects and showed a smaller reduction in oxygen saturation when compared to conventional TOE[22,37]. Most morbidity and mortality associated with upper endoscopic procedures are related to sedation[4,6]. Therefore, unsedated TNE prevents many side effects associated with endoscopy and eliminates the risks of upper endoscopy attributed to sedation. In addition, no intravenous line is necessary on a routine basis. TNE is also likely to be safer in elderly and bedridden patients with a high risk of aspiration pneumonia[3] since TOE may stimulate salivary secretion and increase the risk of aspiration.
TNE decreases the total expense of the endoscopic procedure by eliminating the need for sedation, sedation-related complications, sedation-related work loss, post-procedural monitoring and post-procedure transportation. In several studies, the cost-effectiveness of unsedated TNE was investigated. They found that the mean procedure time, recovery time and cost of unsedated TNE was significantly lower than sedated TOE[12,40].
Lastly, during unsedated TNE the patient is able to speak and observe the procedure. This provides a significant advantage over sedated TOE since patients can discuss the endoscopic images with the endoscopist during the procedure and the endoscopist can see the nasal cavity, pharynx, larynx and vocal cords. Since TNE does not require a mouthpiece, it is also a useful technique in patients with dental problems or unconscious patients who cannot open their mouth. TNE can also be performed in the sitting position which may be an advantage in patients who have difficulty lying down. The nasal endoscope is very thin in appearance when compared to standard endoscopes and this may contribute to patient satisfaction visually (Figure 2).
Figure 2.

Relative diameters of an ultra-thin endoscope (left, 5.9 mm) and a standard gastroscope (right, 8.8 mm).
LIMITATIONS OF THE TRANSNASAL ROUTE
The most important concern in nasal endoscopy, for both the endoscopist and patient, is passing the scope through the nasal passageway. From the patient’s perspective, the most unfavorable side effect of TNE is nasal pain and nasal discomfort. Some patients may think that the insertion through nose is more irritating hypothetically, even before the procedure. Younger patients are generally more sensitive than elderly patients and have more discomfort during the insertion and withdrawal of the scope[41]. If patients have a recent history of rhinitis or other nasal problems, this may increase nasal sensitivity and result in greater pain and discomfort. In our study, patients in the TNE group reported significantly more nasal pain than those in the TOE group (Table 1) but most of them marked it as tolerable. In another study, in which TNE patients were specifically asked about pain, 55% of patients reported that the most painful region was the nose during the procedure. However, 65% of the patients who underwent a TOE in the same study also reported that the pharynx was the most painful region[42]. In another study, discomfort during the insertion was reported at the same rate in TNE and sedated TOE groups[21]. Pain during insertion was reported at the same rate among TNE, unsedated conventional TOE and ultra-thin TOE groups in a randomized trial[43]. These results show that some patients may suffer from nasal pain and discomfort during nasal insertion of the endoscope but it is generally well tolerated and comparable to pain and discomfort caused by oral insertion. Nasal pretreatment and application of an appropriate local anesthesia are likely the most critical procedures to reduce nasal pain and increase patient tolerance. The experience of the endoscopist will also affect the severity of nasal pain and discomfort of the patient. To our knowledge, there is currently no published data on this but we have observed that patients usually reported greater pain when the endoscopist was in the learning phase of TNE, especially in first cases.
The most significant and common complication of TNE is epistaxis[19,26]. It is reported as between 1% to 5% in clinical studies and generally described as mild, self-limited, stopping within a few minutes of the termination of the procedure, and not requiring any intervention[18,21,22,25,42-44]. No epistaxis was reported with scopes under 5 mm in diameter[45,46]. The rate of epistaxis was 4% in our studies using a 5.9 mm scope, which was comparable to what is published in the literature[47]. We observed that epistaxis was often related to a recent history of rhinitis which had not been reported previously by the patient. We suggest that in patients with a recent history of rhinitis, TNE should be postponed or TOE should be preferred. The difficulty in withdrawing the scope has not been reported in the literature but a presentation reported that it is a rare complication (rate of 0.1%)[19]. We have not experienced such a problem in over 1000 cases in our daily practice. Mucous discharge, transient light-headedness, dizziness and headache have also been reported in a small number of patients following TNE[18]. TNE should not be attempted in patients with a history of previous nasal trauma, nasal surgery or nasal anatomical problems.
From the endoscopist’s perspective, the major limitations of TNE are its narrow working channel and poor suction and air functions when compared to standard endoscopes[48]. In addition, the extreme flexibility of the endoscope may cause difficulty in some manipulations, such as passing through the pylorus. Special biopsy forceps with a diameter of 1.8 mm are required for the working channel. Biopsy samples with these forceps are also smaller but some studies showed no difference in pathological diagnosis of targeted lesions between small and standard diameter forceps[28,49,50]. Nasal scopes have a limited number of available endoscopic accessories and are not appropriate for therapeutic procedures through the working channel. The suction of secretions, gastric content and blood is limited. Thus, TNE is mostly used for diagnostic purposes, except in certain conditions which require a thinner endoscope. The inability of TNE to be used for the delivery of endotherapy due to the small working channel is a true limitation of this method. If it is a planned or likely interventional endoscopy, TOE should be preferred.
There is some controversy about the image capabilities of ultra-thin endoscopes. With improvement in endoscopic technology, ultra-thin scopes with CCD cameras now have good image quality and their field of view is similar to standard endoscopes (Figure 3). Their diagnostic accuracy is nearly the same as standard scopes[25,43,49,51]. However, they do not have high-definition (HD) image capabilities and this may decrease their rate of small lesion detection compared to HD scopes[52,53].
Figure 3.
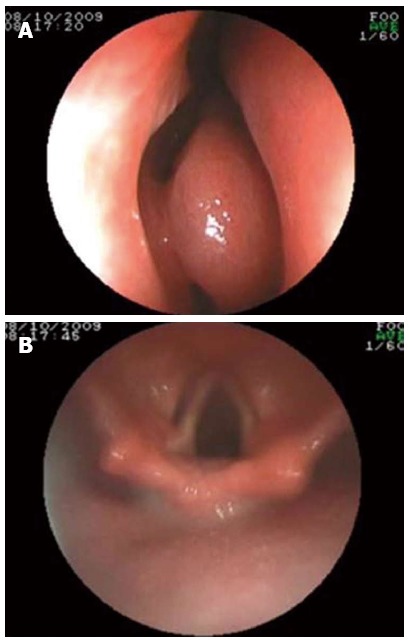
Endoscopic images of transnasal endoscopy during insertion from nose (A) and oropharynx (B).
Endoscopists must also receive training in order to perform TNE, particularly those unfamiliar with nasal anatomy. However, in our experience, the learning curve is very short for an experienced endoscopist and they are usually successful at TNE in their first attempts, particularly if under the supervision of a trainer[46].
The failure of endoscopic insertion is greater in TNE when compared to TOE and a 0 to 10% failure rate has been reported previously[25,43,44,54]. In a large study consisting of 1100 patients, the failure rate was 6.1%[44]. In this study, 5.3 and 5.9 mm diameter endoscopes were used and it was reported that the larger endoscope diameter, as well as being female under 35 years old, was predictive for TNE failure. It is important to acknowledge that the failure rate may vary according to patient history, experience of the endoscopist, scope diameter, nasal pretreatment and other potential differences in procedural protocol. Importantly, while insertion failure may be considered a drawback of TNE, it is quite easy to switch to the oral route and this imposes no negative effect on patients. Pharyngeal topical anesthesia during pretreatment makes such a switch easier. In our study, the endoscope insertion failure was 3.5% and the procedure was completed in these patients via the oral route without delay.
After pretreatment, the examination time of TNE is usually between 5 and 10 min. It is generally a bit longer than the duration of TOE in clinical studies but this had no impact on the tolerability of the procedure[19,25,26,40,54]. However, when pretreatment and post-procedural monitoring times are taken into consideration, the total time of procedure is shorter for TNE than sedated TOE. Table 2 summarizes the overall advantages and limitations of TNE.
Table 2.
Advantages and limitations of transnasal endoscopy
| Advantages of transnasal endoscopy | Limitations of transnasal endoscopy |
| More comfortable and tolerable than unsedated TOE | Needs nasal pretreatment |
| Safer and cost-effective than sedated TOE | Nasal pain and discomfort |
| Elimination of all side effects due to sedation | Mild epistaxis |
| Total procedure time is shorter than sedated TOE | Limited functionality (suction, air, water) |
| No or minimal hemodynamic changes | Extreme flexibility of scope body |
| No intravenous line is necessary routinely | Narrow working channel. Not appropriate for through the scope interventional procedures |
| Patient can speak, watch and discuss during procedure | Needs extra training |
| No need for mouthpiece | No HD image capabilities |
| Evaluation of nasal cavity, pharynx and larynx | Higher insertion failure rate |
| Can be done in sitting position | Longer examination time |
| Visual satisfaction for patients | Not appropriate for patients with nasal problems |
TOE: Transoral endoscopy; HD: High-definition.
OTHER APPLICATIONS USING ULTRA-THIN ENDOSCOPES
Apart from TNE, ultra-thin endoscopes (UTE) may have some advantages in some special cases due to their thinner diameter, which can be used for interventional purposes by the transnasal or transoral route. The thin diameter of these scopes is an important advantage to pass through gastrointestinal strictures where standard scopes have failed. In a prospective study, our group showed that a 5.9 mm UTE was successful in 49 of 62 patients (79%) with advanced gastrointestinal stricture which standard endoscopes had failed to pass through[55]. In addition to contributing to patient diagnosis, UTE were also used in interventional procedures in 1/3 of those cases. In recent years, using the advantage of their thin diameter, UTE has been used for different endoscopic therapeutic applications, including nasojejunal feeding tube insertion, percutaneous gastrostomy and jejunostomy, direct cholangioscopy with biopsy and lithotripsy, and a double scope technique for some endoscopic interventions[25,54-60]. These are not discussed in detail here since our focus is to review transnasal endoscopy.
CONCLUSION
TNE is better tolerated than unsedated conventional TOE and offers a more comfortable diagnostic endoscopic procedure to patients. It is safer and less expensive when compared to sedated TOE. Therefore, it should be considered a viable alternative to both unsedated and sedated conventional TOE. Nasal pretreatment is the most important part of TNE to ensure patient tolerance. We believe all endoscopists should be aware of the technical specifications, advantages and limitations of TNE and all eligible patients for TNE should be informed of this method and offered TNE as an alternative to standard oral endoscopy when appropriate. Lastly, the practice of TNE should become a standard part of gastroenterology fellowship training programs to ensure that this procedure becomes part of daily use in endoscopy units.
Footnotes
P- Reviewers: Beech TJ, Teramoto-Matsubara OT S- Editor: Wen LL L- Editor: Roemmele A E- Editor: Zhang DN
References
- 1.Feld AD. Endoscopic sedation: medicolegal considerations. Gastrointest Endosc Clin N Am. 2008;18:783–788, x. doi: 10.1016/j.giec.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Lazzaroni M, Bianchi Porro G. Preparation, premedication, and surveillance. Endoscopy. 2005;37:101–109. doi: 10.1055/s-2004-826149. [DOI] [PubMed] [Google Scholar]
- 3.Travis AC, Pievsky D, Saltzman JR. Endoscopy in the elderly. Am J Gastroenterol. 2012;107:1495–501; quiz 1494, 1502. doi: 10.1038/ajg.2012.246. [DOI] [PubMed] [Google Scholar]
- 4.Ginzburg L, Greenwald D, Cohen J. Complications of endoscopy. Gastrointest Endosc Clin N Am. 2007;17:405–432. doi: 10.1016/j.giec.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Abraham NS, Fallone CA, Mayrand S, Huang J, Wieczorek P, Barkun AN. Sedation versus no sedation in the performance of diagnostic upper gastrointestinal endoscopy: a Canadian randomized controlled cost-outcome study. Am J Gastroenterol. 2004;99:1692–1699. doi: 10.1111/j.1572-0241.2004.40157.x. [DOI] [PubMed] [Google Scholar]
- 6.Wang CY, Ling LC, Cardosa MS, Wong AK, Wong NW. Hypoxia during upper gastrointestinal endoscopy with and without sedation and the effect of pre-oxygenation on oxygen saturation. Anaesthesia. 2000;55:654–658. doi: 10.1046/j.1365-2044.2000.01520.x. [DOI] [PubMed] [Google Scholar]
- 7.Baudet JS, Borque P, Borja E, Alarcón-Fernández O, Sánchez-del-Río A, Campo R, Avilés J. Use of sedation in gastrointestinal endoscopy: a nationwide survey in Spain. Eur J Gastroenterol Hepatol. 2009;21:882–888. doi: 10.1097/MEG.0b013e328314b7ca. [DOI] [PubMed] [Google Scholar]
- 8.Conigliaro R, Rossi A. Implementation of sedation guidelines in clinical practice in Italy: results of a prospective longitudinal multicenter study. Endoscopy. 2006;38:1137–1143. doi: 10.1055/s-2006-944842. [DOI] [PubMed] [Google Scholar]
- 9.Faulx AL, Vela S, Das A, Cooper G, Sivak MV, Isenberg G, Chak A. The changing landscape of practice patterns regarding unsedated endoscopy and propofol use: a national Web survey. Gastrointest Endosc. 2005;62:9–15. doi: 10.1016/s0016-5107(05)00518-3. [DOI] [PubMed] [Google Scholar]
- 10.Thanvi BR, Munshi SK, Vijayakumar N, Taub N, Lo TC. Acceptability of oesophagogastroduodenoscopy without intravenous sedation: patients’ versus endoscopist’s perception with special reference to older patients. Postgrad Med J. 2003;79:650–651. doi: 10.1136/pmj.79.937.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mulcahy HE, Riches A, Kiely M, Farthing MJ, Fairclough PD. A prospective controlled trial of an ultrathin versus a conventional endoscope in unsedated upper gastrointestinal endoscopy. Endoscopy. 2001;33:311–316. doi: 10.1055/s-2001-13692. [DOI] [PubMed] [Google Scholar]
- 12.Garcia RT, Cello JP, Nguyen MH, Rogers SJ, Rodas A, Trinh HN, Stollman NH, Schlueck G, McQuaid KR. Unsedated ultrathin EGD is well accepted when compared with conventional sedated EGD: a multicenter randomized trial. Gastroenterology. 2003;125:1606–1612. doi: 10.1053/j.gastro.2003.08.034. [DOI] [PubMed] [Google Scholar]
- 13.Chak A, Rothstein RI. Sedationless upper endoscopy. Rev Gastroenterol Disord. 2006;6 Suppl 1:S3–11. [PubMed] [Google Scholar]
- 14.Campo R, Montserrat A, Brullet E. Transnasal gastroscopy compared to conventional gastroscopy: a randomized study of feasibility, safety, and tolerance. Endoscopy. 1998;30:448–452. doi: 10.1055/s-2007-1001306. [DOI] [PubMed] [Google Scholar]
- 15.Dumortier J, Ponchon T, Scoazec JY, Moulinier B, Zarka F, Paliard P, Lambert R. Prospective evaluation of transnasal esophagogastroduodenoscopy: feasibility and study on performance and tolerance. Gastrointest Endosc. 1999;49:285–291. doi: 10.1016/s0016-5107(99)70002-7. [DOI] [PubMed] [Google Scholar]
- 16.Peery AF, Hoppo T, Garman KS, Dellon ES, Daugherty N, Bream S, Sanz AF, Davison J, Spacek M, Connors D, et al. Feasibility, safety, acceptability, and yield of office-based, screening transnasal esophagoscopy (with video) Gastrointest Endosc. 2012;75:945–953.e2. doi: 10.1016/j.gie.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilkins T, Gillies RA. Office-based ultrathin esophagogastroduodenoscopy in a primary care setting. J Am Board Fam Pract. 2004;17:438–442. doi: 10.3122/jabfm.17.6.438. [DOI] [PubMed] [Google Scholar]
- 18.Cho S, Arya N, Swan K, Cirocco M, Kandel G, Kortan P, Marcon N. Unsedated transnasal endoscopy: a Canadian experience in daily practice. Can J Gastroenterol. 2008;22:243–246. doi: 10.1155/2008/514297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tatsumi Y, Harada A, Matsumoto T, Tani T, Nishida H. Current status and evaluation of transnasal esophagogastroduodenoscopy. Dig Endosc. 2009;21:141–146. doi: 10.1111/j.1443-1661.2009.00891.x. [DOI] [PubMed] [Google Scholar]
- 20.Murata A, Akahoshi K, Sumida Y, Yamamoto H, Nakamura K, Nawata H. Prospective randomized trial of transnasal versus peroral endoscopy using an ultrathin videoendoscope in unsedated patients. J Gastroenterol Hepatol. 2007;22:482–485. doi: 10.1111/j.1440-1746.2006.04730.x. [DOI] [PubMed] [Google Scholar]
- 21.Stroppa I, Grasso E, Paoluzi OA, Razzini C, Tosti C, Andrei F, Biancone L, Palmieri G, Romeo F, Pallone F. Unsedated transnasal versus transoral sedated upper gastrointestinal endoscopy: a one-series prospective study on safety and patient acceptability. Dig Liver Dis. 2008;40:767–775. doi: 10.1016/j.dld.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 22.Ai ZL, Lan CH, Fan LL, Lan L, Cao Y, Li P, Song O, Chen DF. Unsedated transnasal upper gastrointestinal endoscopy has favorable diagnostic effectiveness, cardiopulmonary safety, and patient satisfaction compared with conventional or sedated endoscopy. Surg Endosc. 2012;26:3565–3572. doi: 10.1007/s00464-012-2367-4. [DOI] [PubMed] [Google Scholar]
- 23.Thota PN, Zuccaro G, Vargo JJ, Conwell DL, Dumot JA, Xu M. A randomized prospective trial comparing unsedated esophagoscopy via transnasal and transoral routes using a 4-mm video endoscope with conventional endoscopy with sedation. Endoscopy. 2005;37:559–565. doi: 10.1055/s-2005-861476. [DOI] [PubMed] [Google Scholar]
- 24.Kim CY, O’Rourke RW, Chang EY, Jobe BA. Unsedated small-caliber upper endoscopy: an emerging diagnostic and therapeutic technology. Surg Innov. 2006;13:31–39. doi: 10.1177/155335060601300106. [DOI] [PubMed] [Google Scholar]
- 25.Lee SY, Kawai T. Transnasal route: new approach to endoscopy. Gut Liver. 2008;2:155–165. doi: 10.5009/gnl.2008.2.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maffei M, Dumonceau JM. Transnasal esogastroduodenoscopy (EGD): comparison with conventional EGD and new applications. Swiss Med Wkly. 2008;138:658–664. doi: 10.4414/smw.2008.12220. [DOI] [PubMed] [Google Scholar]
- 27.Dumonceau JM, Dumortier J, Deviere J, Kahaleh M, Ponchon T, Maffei M, Costamagna G. Transnasal OGD: practice survey and impact of a live video retransmission. Dig Liver Dis. 2008;40:776–783. doi: 10.1016/j.dld.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 28.Shariff MK, Bird-Lieberman EL, O’Donovan M, Abdullahi Z, Liu X, Blazeby J, Fitzgerald R. Randomized crossover study comparing efficacy of transnasal endoscopy with that of standard endoscopy to detect Barrett’s esophagus. Gastrointest Endosc. 2012;75:954–961. doi: 10.1016/j.gie.2012.01.029. [DOI] [PubMed] [Google Scholar]
- 29.Kawai T, Takagi Y, Yamamoto K, Hayama Y, Fukuzawa M, Yagi K, Fukuzawa M, Kataoka M, Kawakami K, Itoi T, et al. Narrow-band imaging on screening of esophageal lesions using an ultrathin transnasal endoscopy. J Gastroenterol Hepatol. 2012;27 Suppl 3:34–39. doi: 10.1111/j.1440-1746.2012.07068.x. [DOI] [PubMed] [Google Scholar]
- 30.Iwamoto J, Mizokami Y, Shimokobe K, Ito M, Hirayama T, Saito Y, Honda A, Ikegami T, Matsuzaki Y. Pretreatment methods in transnasal endoscopy. Hepatogastroenterology. 2011;58:842–845. [PubMed] [Google Scholar]
- 31.Dean R, Dua K, Massey B, Berger W, Hogan WJ, Shaker R. A comparative study of unsedated transnasal esophagogastroduodenoscopy and conventional EGD. Gastrointest Endosc. 1996;44:422–424. doi: 10.1016/s0016-5107(96)70092-5. [DOI] [PubMed] [Google Scholar]
- 32.Bampton PA, Reid DP, Johnson RD, Fitch RJ, Dent J. A comparison of transnasal and transoral oesophagogastroduodenoscopy. J Gastroenterol Hepatol. 1998;13:579–584. doi: 10.1111/j.1440-1746.1998.tb00693.x. [DOI] [PubMed] [Google Scholar]
- 33.Zaman A, Hapke R, Sahagun G, Katon RM. Unsedated peroral endoscopy with a video ultrathin endoscope: patient acceptance, tolerance, and diagnostic accuracy. Am J Gastroenterol. 1998;93:1260–1263. doi: 10.1111/j.1572-0241.1998.00406.x. [DOI] [PubMed] [Google Scholar]
- 34.Kadayıfçı A, Serap P, Aydınlı M, Dag MS, Demir U, Savas MC. Unsedated Transnasal versus Conventional Oral Endoscopy in endoscopy naïve patients. Acta gastro-enterologica Belgica. 2014;77:In press. [PubMed] [Google Scholar]
- 35.Zaman A, Hahn M, Hapke R, Knigge K, Fennerty MB, Katon RM. A randomized trial of peroral versus transnasal unsedated endoscopy using an ultrathin videoendoscope. Gastrointest Endosc. 1999;49:279–284. doi: 10.1016/s0016-5107(99)70001-5. [DOI] [PubMed] [Google Scholar]
- 36.Faulx AL, Catanzaro A, Zyzanski S, Cooper GS, Pfau PR, Isenberg G, Wong RC, Sivak MV, Chak A. Patient tolerance and acceptance of unsedated ultrathin esophagoscopy. Gastrointest Endosc. 2002;55:620–623. doi: 10.1067/mge.2002.123274. [DOI] [PubMed] [Google Scholar]
- 37.Kataoka H, Hayano J, Mizushima T, Tanaka M, Kubota E, Shimura T, Mizoshita T, Tanida S, Kamiya T, Nojiri S, et al. Cardiovascular tolerance and autonomic nervous responses in unsedated upper gastrointestinal small-caliber endoscopy: a comparison between transnasal and peroral procedures with newly developed mouthpiece. Dig Endosc. 2011;23:78–85. doi: 10.1111/j.1443-1661.2010.01064.x. [DOI] [PubMed] [Google Scholar]
- 38.Frieling T, Schindler P, Kuhlbusch-Zicklam R, Heise J, Hülsdonk A, Kreysel C. Krefeld CONTRA study: conventional peroral Esophago-Gastro-Duodenoscopy (EGD) vs. transnasal EGD--a prospective and randomised study with independent evaluation of conscious sedation, endoscope diameter, and access path. Z Gastroenterol. 2010;48:818–824. doi: 10.1055/s-0029-1245275. [DOI] [PubMed] [Google Scholar]
- 39.Kawai T, Miyazaki I, Yagi K, Kataoka M, Kawakami K, Yamagishi T, Sofuni A, Itoi T, Moriyasu F, Osaka Y, et al. Comparison of the effects on cardiopulmonary function of ultrathin transnasal versus normal diameter transoral esophagogastroduodenoscopy in Japan. Hepatogastroenterology. 2007;54:770–774. [PubMed] [Google Scholar]
- 40.Gorelick AB, Inadomi JM, Barnett JL. Unsedated small-caliber esophagogastroduodenoscopy (EGD): less expensive and less time-consuming than conventional EGD. J Clin Gastroenterol. 2001;33:210–214. doi: 10.1097/00004836-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 41.Murata A, Akahoshi K, Motomura Y, Matsui N, Kubokawa M, Kimura M, Ouchi J, Honda K, Endo S, Nakamura K, et al. Prospective comparative study on the acceptability of unsedated transnasal endoscopy in younger versus older patients. J Clin Gastroenterol. 2008;42:965–968. doi: 10.1097/MCG.0b013e318126bb19. [DOI] [PubMed] [Google Scholar]
- 42.Watanabe H, Watanabe N, Ogura R, Nishino N, Saifuku Y, Hitomi G, Okamoto Y, Tominaga K, Yoshitake N, Yamagata M, et al. A randomized prospective trial comparing unsedated endoscopy via transnasal and transoral routes using 5.5-mm video endoscopy. Dig Dis Sci. 2009;54:2155–2160. doi: 10.1007/s10620-008-0614-2. [DOI] [PubMed] [Google Scholar]
- 43.Trevisani L, Cifalà V, Sartori S, Gilli G, Matarese G, Abbasciano V. Unsedated ultrathin upper endoscopy is better than conventional endoscopy in routine outpatient gastroenterology practice: a randomized trial. World J Gastroenterol. 2007;13:906–911. doi: 10.3748/wjg.v13.i6.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dumortier J, Napoleon B, Hedelius F, Pellissier PE, Leprince E, Pujol B, Ponchon T. Unsedated transnasal EGD in daily practice: results with 1100 consecutive patients. Gastrointest Endosc. 2003;57:198–204. doi: 10.1067/mge.2003.59. [DOI] [PubMed] [Google Scholar]
- 45.Dumortier J, Josso C, Roman S, Fumex F, Lepilliez V, Prost B, Lot M, Guillaud O, Petit-Laurent F, Lapalus MG, et al. Prospective evaluation of a new ultrathin one-plane bending videoendoscope for transnasal EGD: a comparative study on performance and tolerance. Gastrointest Endosc. 2007;66:13–19. doi: 10.1016/j.gie.2006.11.058. [DOI] [PubMed] [Google Scholar]
- 46.Maffei M, Dumortier J, Dumonceau JM. Self-training in unsedated transnasal EGD by endoscopists competent in standard peroral EGD: prospective assessment of the learning curve. Gastrointest Endosc. 2008;67:410–418. doi: 10.1016/j.gie.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 47.Kadayıfçı A, Serap P, Aydınlı M, Koruk İ, Demir U, Balkan A, Koruk I, Savas MC, Koruk M. Tolerability and feasibility of transnasal endoscopy without sedation. Turkish J Gastroenterol. 2009;20(Suppl 1):754. [Google Scholar]
- 48.Kawai T, Yamamoto K, Fukuzawa M, Sakai Y, Moriyasu F. [Ultra-thin transnasal esophagogastroduodenoscopy] Nihon Rinsho. 2010;68:1264–1267. [PubMed] [Google Scholar]
- 49.Jobe BA, Hunter JG, Chang EY, Kim CY, Eisen GM, Robinson JD, Diggs BS, O’Rourke RW, Rader AE, Schipper P, et al. Office-based unsedated small-caliber endoscopy is equivalent to conventional sedated endoscopy in screening and surveillance for Barrett’s esophagus: a randomized and blinded comparison. Am J Gastroenterol. 2006;101:2693–2703. doi: 10.1111/j.1572-0241.2006.00890.x. [DOI] [PubMed] [Google Scholar]
- 50.Saeian K, Staff DM, Vasilopoulos S, Townsend WF, Almagro UA, Komorowski RA, Choi H, Shaker R. Unsedated transnasal endoscopy accurately detects Barrett’s metaplasia and dysplasia. Gastrointest Endosc. 2002;56:472–478. doi: 10.1067/mge.2002.128131. [DOI] [PubMed] [Google Scholar]
- 51.Sorbi D, Gostout CJ, Henry J, Lindor KD. Unsedated small-caliber esophagogastroduodenoscopy (EGD) versus conventional EGD: a comparative study. Gastroenterology. 1999;117:1301–1307. doi: 10.1016/s0016-5085(99)70280-5. [DOI] [PubMed] [Google Scholar]
- 52.Toyoizumi H, Kaise M, Arakawa H, Yonezawa J, Yoshida Y, Kato M, Yoshimura N, Goda K, Tajiri H. Ultrathin endoscopy versus high-resolution endoscopy for diagnosing superficial gastric neoplasia. Gastrointest Endosc. 2009;70:240–245. doi: 10.1016/j.gie.2008.10.064. [DOI] [PubMed] [Google Scholar]
- 53.Horiuchi A, Nakayama Y, Hidaka N, Ichise Y, Kajiyama M, Tanaka N. Prospective comparison between sedated high-definition oral and unsedated ultrathin transnasal esophagogastroduodenoscopy in the same subjects: pilot study. Dig Endosc. 2009;21:24–28. doi: 10.1111/j.1443-1661.2008.00826.x. [DOI] [PubMed] [Google Scholar]
- 54.Rodriguez SA, Banerjee S, Desilets D, Diehl DL, Farraye FA, Kaul V, Kwon RS, Mamula P, Pedrosa MC, Varadarajulu S, et al. Ultrathin endoscopes. Gastrointest Endosc. 2010;71:893–898. doi: 10.1016/j.gie.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 55.Aydinli M, Koruk I, Dag MS, Savas MC, Kadayifci A. Ultrathin endoscopy for gastrointestinal strictures. Dig Endosc. 2012;24:150–153. doi: 10.1111/j.1443-1661.2011.01206.x. [DOI] [PubMed] [Google Scholar]
- 56.Aydinli M, Koruk I, Koruk S, Aydin U, Kadayifci A. Intraoperative cholangioscopy with an ultrathin endoscope for hemobilia. Endoscopy. 2011;43 Suppl 2 UCTN:E410. doi: 10.1055/s-0030-1256897. [DOI] [PubMed] [Google Scholar]
- 57.Yuki M, Amano Y, Komazawa Y, Fukuhara H, Shizuku T, Yamamoto S, Kinoshita Y. Unsedated transnasal small-caliber esophagogastroduodenoscopy in elderly and bedridden patients. World J Gastroenterol. 2009;15:5586–5591. doi: 10.3748/wjg.15.5586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Moon JH, Choi HJ. The Role of Direct Peroral Cholangioscopy Using an Ultraslim Endoscope for Biliary Lesions: Indications, Limitations, and Complications. Clin Endosc. 2013;46:537–539. doi: 10.5946/ce.2013.46.5.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Parsi MA, Stevens T, Vargo JJ. Diagnostic and therapeutic direct peroral cholangioscopy using an intraductal anchoring balloon. World J Gastroenterol. 2012;18:3992–3996. doi: 10.3748/wjg.v18.i30.3992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lee DK, Jahng JH. Alternative methods in the endoscopic management of difficult common bile duct stones. Dig Endosc. 2010;22 Suppl 1:S79–S84. doi: 10.1111/j.1443-1661.2010.00960.x. [DOI] [PubMed] [Google Scholar]


