Abstract
Increased lung vascular permeability and alveolar edema are cardinal features of inflammatory conditions such as acute respiratory distress syndrome (ARDS) and ventilator-induced lung injury (VILI). We previously demonstrated that pre–B-cell colony-enhancing factor (PBEF)/NAMPT, the proinflammatory cytokine encoded by NAMPT, participates in ARDS and VILI inflammatory syndromes. The present study evaluated posttranscriptional regulation of PBEF/NAMPT gene expression in human lung endothelium via 3′-untranslated region (UTR) microRNA (miRNA) binding. In silico analysis identified hsa-miR-374a and hsa-miR-568 as potential miRNA candidates. Increased PBEF/NAMPT transcription (by RT-PCR) and expression (by Western blotting) induced by 18% cyclic stretch (CS) (2 h: 3.4 ± 0.06 mRNA fold increase (FI); 10 h: 1.5 ± 0.06 protein FI) and by LPS (4 h: 3.8 ± 0.2 mRNA FI; 48 h: 2.6 ± 0.2 protein FI) were significantly attenuated by transfection with mimics of hsa-miR-374a or hsa-miR-568 (40–60% reductions each). LPS and 18% CS increased the activity of a PBEF/NAMPT 3′-UTR luciferase reporter (2.4–3.25 FI) with induction reduced by mimics of each miRNA (44–60% reduction). Specific miRNA inhibitors (antagomirs) for each PBEF/NAMPT miRNA significantly increased the endogenous PBEF/NAMPT mRNA (1.4–3.4 ± 0.1 FI) and protein levels (1.2–1.4 ± 0.1 FI) and 3′-UTR luciferase activity (1.4–1.7 ± 0.1 FI) compared with negative antagomir controls. Collectively, these data demonstrate that increased PBEF/NAMPT expression induced by bioactive agonists (i.e., excessive mechanical stress, LPS) involves epigenetic regulation with hsa-miR-374a and hsa-miR-568, representing novel therapeutic strategies to reduce inflammatory lung injury.
Keywords: miRNA, PBEF/NAMPT, ARDS, ventilator-induced lung injury, endothelial cells
Clinical Relevance
Targeting of pre–B-cell colony-enhancing factor/NAMPT, a critical inflammatory biomarker in acute respiratory distress syndrome and ventilator-induced lung injury, via specific microRNAs is a potentially promising novel therapeutic strategy to reduce lung vascular permeability/edema and inflammation in acute respiratory distress syndrome and ventilator-induced lung injury.
Acute lung injury (ALI), acute respiratory distress syndrome (ARDS), and ventilator-induced lung injury (VILI) are devastating syndromes characterized by profound lung inflammation, increased lung vascular permeability, and protein-rich alveolar edema (1, 2). Despite improved understanding of ARDS pathophysiology, the morbidity and mortality of ARDS continue to be unacceptably high (3), and the mechanisms underlying VILI in the setting of ARDS remain unclear. Furthermore, effective pharmacotherapy for ARDS or VILI has yet to emerge. Using genomic-intensive expression profiling in canine and murine models of human ALI, we previously identified pre–B-cell colony enhancing factor (PBEF), a proinflammatory cytokine and nicotinamide adenine dinucleotide biosynthetic enzyme (nicotinamide phosphoribosyltransferase) (4–6) encoded by NAMPT, as a novel biomarker in ARDS and as an ARDS and VILI candidate gene (7). PBEF/NAMPT levels are increased in visceral fat, leading to its renaming as visfatin, an adipokine regulating metabolic syndrome, and diabetes (8). PBEF/NAMPT is up-regulated in murine, canine, and human ARDS, with spatial localization to lung leukocytes and the vascular endothelium (7). PBEF/NAMPT is also an inflammatory mediator secreted in the development of VILI (9) and influences ARDS severity (10). Supporting the human and animal ARDS data, PBEF/NAMPT alters vascular barrier integrity via Ca2+–dependent cytoskeletal rearrangement and enhances the inflammatory response in experimental and clinical sepsis through regulation of neutrophil apoptosis and inflammatory cytokine secretion (11, 12). A number of stimuli associated with inflammation and infection (LPS, TNF-α, oxidized low-density lipoprotein, IL-1β, IL-6, and cyclic stretch) up-regulate PBEF/NAMPT expression (4, 13–15). Despite the multifunctionality of PBEF as an important proinflammatory and immune system regulator, the mechanisms governing PBEF/NAMPT expression are poorly understood.
MicroRNAs (miRNAs) are small, conserved, noncoding RNAs that regulate gene expression posttranscriptionally by targeting the 3′-untranslated region (3′-UTR) of specific messenger RNAs (mRNAs) for degradation or translational repression. Emerging evidence supports miRNAs as critical regulators of biological processes such as cell differentiation, proliferation, apoptosis, metabolism, neuronal development, brain morphogenesis, DNA repair, and methylation and stem cell division (16–18). Because miRNA deregulation is linked to inflammatory conditions (19, 20), metabolic disorders (21), cancer (22, 23), cardiovascular (24, 25), myeloproliferative (26), autoimmune (27), and neurodegenerative diseases (28), miRNAs have emerged as novel biomarkers and therapeutic targets. In the present study, we explored the role of miRNAs in ARDS/VILI pathogenesis, focusing on posttranscriptional PBEF gene regulation using the PBEF/NAMPT 3′-UTR luciferase reporter, overexpression of mature miRNAs, and endogenous miRNA inhibition by antagomirs. Preliminary in silico analysis identified two miRNA candidates, hsa-miR-374a and hsa-miR-568, as potentially binding to the 3′-UTR of PBEF/NAMPT. We investigated whether these miRNAs participate in regulation of LPS- and 18% cyclic stretch (CS)-induced NAMPT gene expression in vitro.
Materials and Methods
Reagents
LPS from Escherichia coli was obtained from Sigma-Aldrich (St. Louis, MO). Human PBEF 3′-UTR cloned downstream of a firefly luciferase gene was obtained from SwitchGear Genomics (Menlo Park, CA). Rabbit polyclonal anti-PBEF antibodies (Ab) were obtained from Bethyl Laboratories, Inc. (Montgomery, TX), and mouse monoclonal Ab against β-actin was obtained from Sigma-Aldrich. Unless specified, biochemical reagents were obtained from Sigma-Aldrich.
Cell Culture
Human pulmonary artery endothelial cells (ECs) were obtained from Lonza Inc. (Allendale, NJ) and cultured in endothelial basal medium-2 with 10% FBS at 37°C in a humidified incubator with 5% CO2 as previously described (29). ECs at passages 5 through 9 were used for all experiments.
Bioinformatics Analysis and miRNA Prediction
To predict miRNAs that potentially regulate PBEF/NAMPT mRNA, three computational algorithms were used: TargetScan 6.2 (http://www.targetscan.org/), developed by Whitehead Institute for Biomedical Research (Cambridge, MA) (30, 31); MiRanda (http://www.microrna.org/microrna/home.do), developed by Computational and Systems Biology Center, Memorial Sloan-Kettering Cancer Center (New York, NY) (32); and DIANA-microT-CDS (http://diana.cslab.ece. ntua.gr/microT/), developed by DIANA-Lab, Institute of Molecular Oncology, Biomedical Sciences Research Center “Alexander Fleming” (Vari, Greece) (33). Further details are provided in the online supplement.
Transient Transfections and Reporter Assays
Transfection of luciferase reporter constructs and miRNA or miRNA inhibitors was performed according to the manufacturer's protocol. Luciferase activity was measured using the Dual Luciferase Assay System (Promega, Fitchburg, WI) following the manufacturer’s protocol. Further details are provided in the online supplement.
Cyclic Stretch Experiments
All CS experiments were performed using the FX-4000T Flexcell Tension Plus system (Flexcell International, Hillsborough, NC) equipped with a 25-mm BioFlex loading station designed to provide uniform radial and circumferential strain across a membrane surface along all radii as we described previously (34, 35). Further details are provided in the online supplement.
RNA Extraction and Quantitative Real-Time PCR Analysis
Total RNA from ECs was isolated using Trizol and purified using miRNeasy columns (Qiagen, Valencia, CA). All procedures were performed according the manufacturer’s recommendations for each assay as described in detail in the online supplement.
Immunoblotting
Protein extracts were separated by SDS-PAGE, transferred to nitrocellulose or polyvinylidene difluoride membranes (30 V for 18 h or 100 V for 1.5 h), and immunoreacted with an Ab that recognizes PBEF or β-actin. Immunoreactive proteins were detected with the enhanced chemiluminescent detection system according to the manufacturer's directions (Amersham, Little Chalfont, UK). Intensities of immunoreactive protein bands were quantified using ImageQuant software (Molecular Dynamics, Sunnyvale, CA).
Statistical Analysis
Results are expressed as mean ± SE of three to six independent experiments. We performed statistical comparison among treatment groups by unpaired Student’s t test or by randomized-design two-way ANOVA followed by the Newman-Keuls post hoc test for multiple groups. Results with P < 0.05 were considered statistically significant.
Results
Inflammatory Agonists Increase PBEF/NAMPT Gene Expression and 3′-UTR Reporter Activity in Human Lung ECs
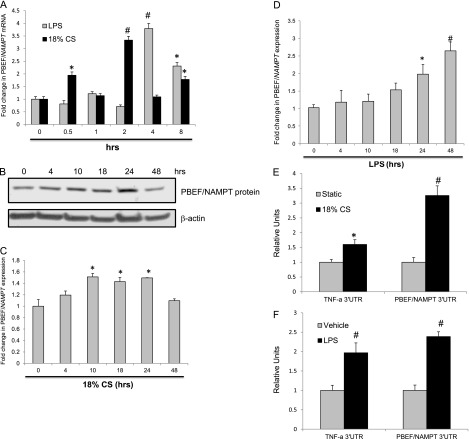
LPS and excessive mechanical stress are important contributors to the development and severity of ARDS and VILI. To elucidate the effect of inflammatory agonists on PBEF/NAMPT gene expression, we quantified PBEF/NAMPT protein levels (0–48 h), PBEF/NAMPT mRNA levels (0–8 h), and the activity of a PBEF/NAMPT 3′-UTR luciferase reporter in ECs exposed to LPS (100 ng/ml) or to 18% CS. LPS and 18% CS independently induced sustained increased levels of PBEF/NAMPT protein and PBEF/NAMPT mRNA. CS at 18% induced early elevation in PBEF/NAMPT mRNA (maximum 3.4 ± 0.06 fold increase [FI] at 2 h) and protein levels in ECs (maximum 1.5 ± 0.06 FI at 10 h), with levels remaining elevated for up to 24 hours. In contrast, LPS augmented PBEF/NAMPT transcript levels that reached maximum levels at 4 hours (3.8 ± 0.2 FI), with PBEF/NAMPT protein levels reaching a maximum at 48 hours (2.65 ± 0.25 FI) (Figures 1A–1D). Agonist-induced PBEF/NAMPT increases were also observed using PBEF/NAMPT 3′-UTR luciferase reporter activity with a 3.2 ± 0.3 FI after 18% CS exposure (Figure 1E) and a 2.4 ± 0.12 FI after LPS challenge (Figure 1F) (24 h) compared with unstimulated cells. These data suggest that PBEF/NAMPT EC expression is altered by exposure to 18% CS or LPS.
Figure 1.
Effects of inflammatory agonists on pre–B-cell colony-enhancing factor (PBEF)/NAMPT expression and 3′-untranslated region (UTR) reporter activity. Total RNA was isolated from human pulmonary artery endothelial cells (ECs) challenged with control vehicle or LPS (100 ng/ml) or exposed to 18% cyclic stretch (CS) for 0 to 8 hours. PBEF/NAMPT mRNA levels were detected via real-time PCR (A). Data are presented as fold change in mRNA level over vehicle-treated control and expressed as mean ± SE from three independent experiments. *P < 0.05 versus unstimulated control. #P < 0.01 versus unstimulated control. Confluent ECs were treated with control vehicle or 18% CS (B) and LPS for the indicated times, and endogenous PBEF was detected via immunoblot. The bar graphs represent relative densitometry (18% CS [C]; LPS [D]). Data are presented as fold changes in PBEF/NAMPT over vehicle-treated control and expressed as means ± SE from three independent experiments. *P < 0.05 versus unstimulated control. #P < 0.01 versus unstimulated control. ECs were cotransfected with PBEF/NAMPT 3′-UTR reporter together with phRL-TK, a Renilla luciferase normalization control vector, and exposed to 18% CS (E) or treated with LPS (F) (24 h), and luciferase activity was measured using the Dual Luciferase Assay System according the manufacturer’s protocol. TNF-α luciferase reporter was used as a positive control. The bar graph represents relative luciferase units. Data are presented as relative luciferase units over vehicle-treated control and expressed as means ± SE from three independent experiments. *P < 0.05 versus unstimulated control. #P < 0.01 versus unstimulated control.
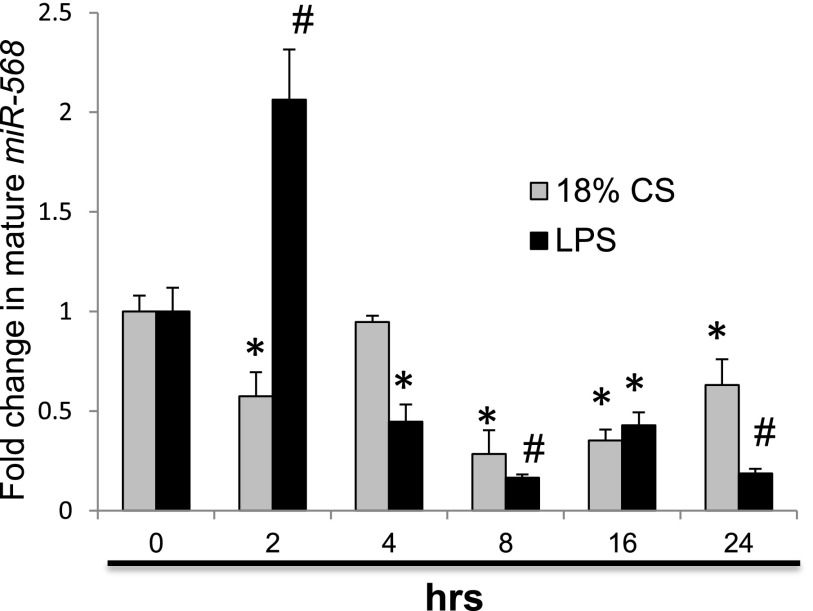
The miRNA miR-568 Is Down-Regulated in 18% CS- and LPS-Challenged Human ECs
To identify candidate miRNAs potentially targeting PBEF/NAMPT mRNAs, we used in silico prediction programs and identified miR-374a and miR-568 as potential miRNAs regulating PBEF/NAMPT gene expression by 3′-UTR binding with miR-374a exhibiting two potential 3′-UTR binding sites. As predicted, the potential binding site on PBEF/NAMPT 3′-UTR for miR-374a is broadly conserved among mammals. Moreover, we noted that MYLK, an ARDS candidate gene (36) encoding myosin light chain kinase, is a potential target of miR-374a (37). In recent studies, we noted that expression of the mature miR-374a is significantly decreased by 18% CS, TNF-α, or LPS, with maximal decreases by 4 hours (37). These results suggested that changes in miR-374a expression may play a role in PBEF/NAMPT posttranscriptional regulation. To investigate whether miR-568 participates in PBEF/NAMPT epigenetic regulation, similar to miR-374a, we determined whether 18% CS and LPS regulate mature miR-568 expression in ECs. Confluent human pulmonary ECs were exposed to 18% CS or LPS for 0 to 24 hours, and mature miRNA expression was assessed by quantitative real-time PCR analysis. Figure 2 demonstrates that mature miR-568 expression is significantly decreased by these agonists with maximal reduction in expression at 8 hours; these results were negatively correlated with agonist-mediated augmented PBEF/NAMPT expression (Figures 1A–1D) and 3′-UTR reporter activity (Figures 1E and 1F). These results are consistent with the observation that the majority of miRNAs affect target gene expression by translational repression and subsequent mRNA degradation (38). Overall, such inverse correlation between expression levels of putative miRNA and mRNA and/or protein increases the likelihood that this interaction is functional in vivo (39). A limited number of examples have been described showing a positive correlation between miRNAs and target mRNAs (40, 41).
Figure 2.
Time-dependent effects of inflammatory agonists on mature miR-568 expression in human lung ECs. Total RNA was isolated from ECs and treated with control vehicle, 18% CS, or LPS (100 ng/ml) for 0 to 24 hours, and the level of miR-568 was determined via real-time PCR. Data are presented as fold change in microRNA level over vehicle-treated control and expressed as means ± SE from three independent experiments. *P < 0.05 versus unstimulated control. #P < 0.01 versus unstimulated control.
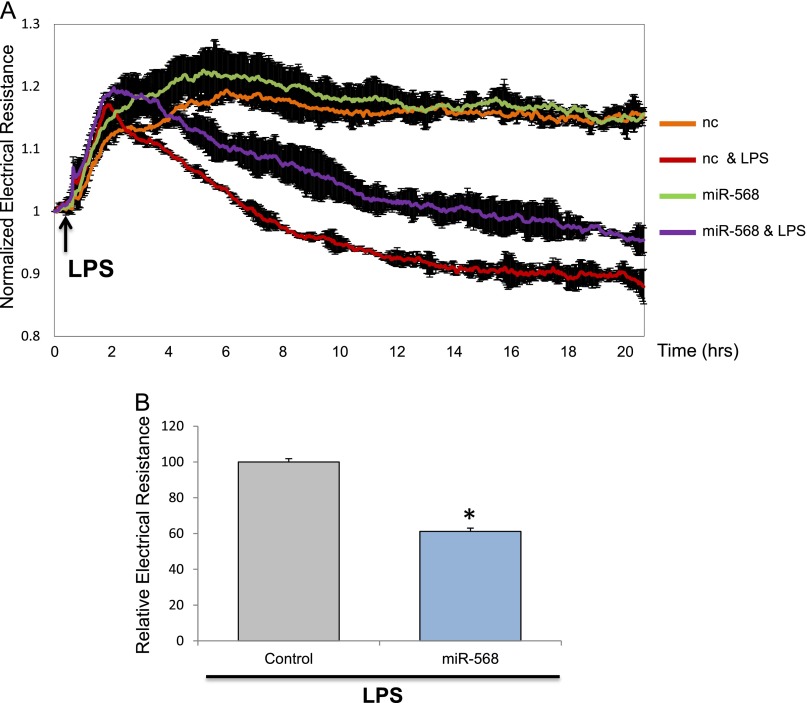
Mimics of miRNAs Attenuate LPS-Induced Human Lung EC Permeability
Our previous in vitro studies demonstrated that PBEF/NAMPT-specific siRNAs (11) and miR-374a (37) abolish PBEF expression and inflammatory agonists’ thrombin-, IL-1β–, and LPS-mediated hyperpermeability (43 ± 2.9% attenuation for miR-374a). Furthermore, intratracheal or intravenous delivery of siRNA (unpublished data) or PBEF/NAMPT neutralizing antibody (9) produce significant reduction in LPS-mediated lung injury and VILI. To evaluate the functional involvement of miR-568 in regulation of PBEF/NAMPT gene expression, we measured changes in LPS-induced lung EC barrier function reflected by increased TER, a highly sensitive in vitro assay of vascular permeability. ECs treated with single miR-568 mimics demonstrate statistically significant attenuation (38.8 ± 1.8%) of LPS-induced hyperpermeability in ECs, reflected by reduced TER (P < 0.01) (Figures 3A and 3B) compared with agonist-stimulated ECs transfected with negative control mimics. These data, together with our previously published data (37), indicate novel roles for miR-374a and miR-568 in mediating LPS-induced lung EC permeability.
Figure 3.
Effect of miR-568 mimic on LPS-induced human lung EC dysfunction. ECs grown in chambers on gold microelectrodes were transfected with miR-568 mimic (A) or treated with nonspecific negative control mimic (nc) as described in Materials and Methods and used for transendothelial electrical resistance (TER) measurements. At time = 0, cells were stimulated with LPS (100 ng/ml) or vehicle control. Shown are pooled TER data of five independent experiments. (B) Maximal value of normalized TER in RCs with nc reagent (control) achieved within 12 hours was taken as 100% ± SE. *Significantly different from cells treated with nc reagent with LPS (P < 0.01).
miRNA Mimics and Antagomirs Alter Inflammatory Agonist-Induced PBEF/NAMPT Expression and 3′-UTR Reporter Activity in Human Lung ECs
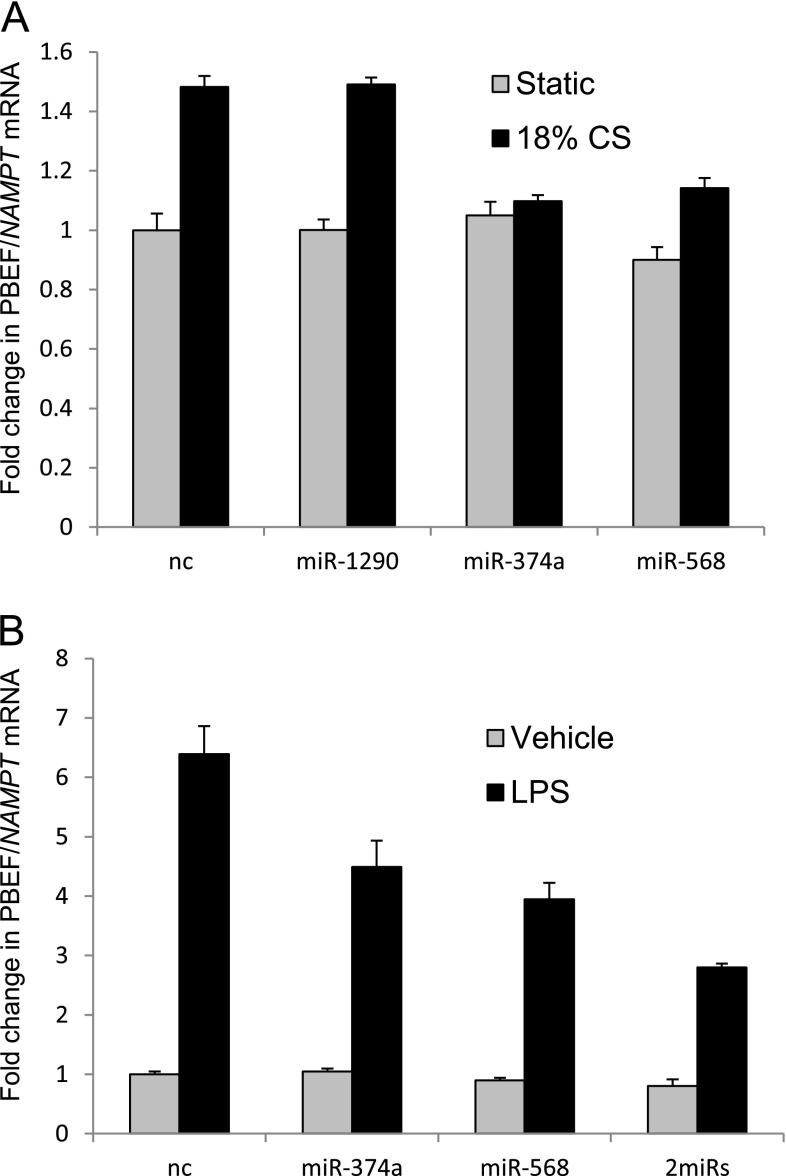
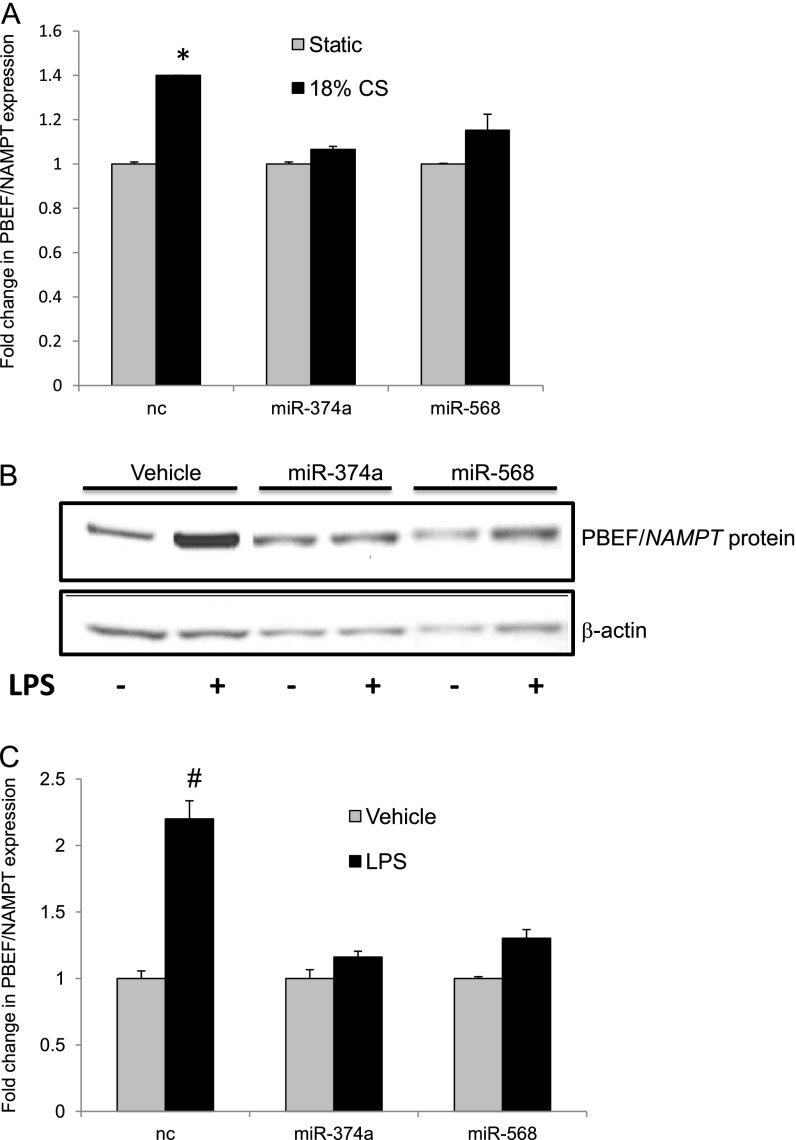
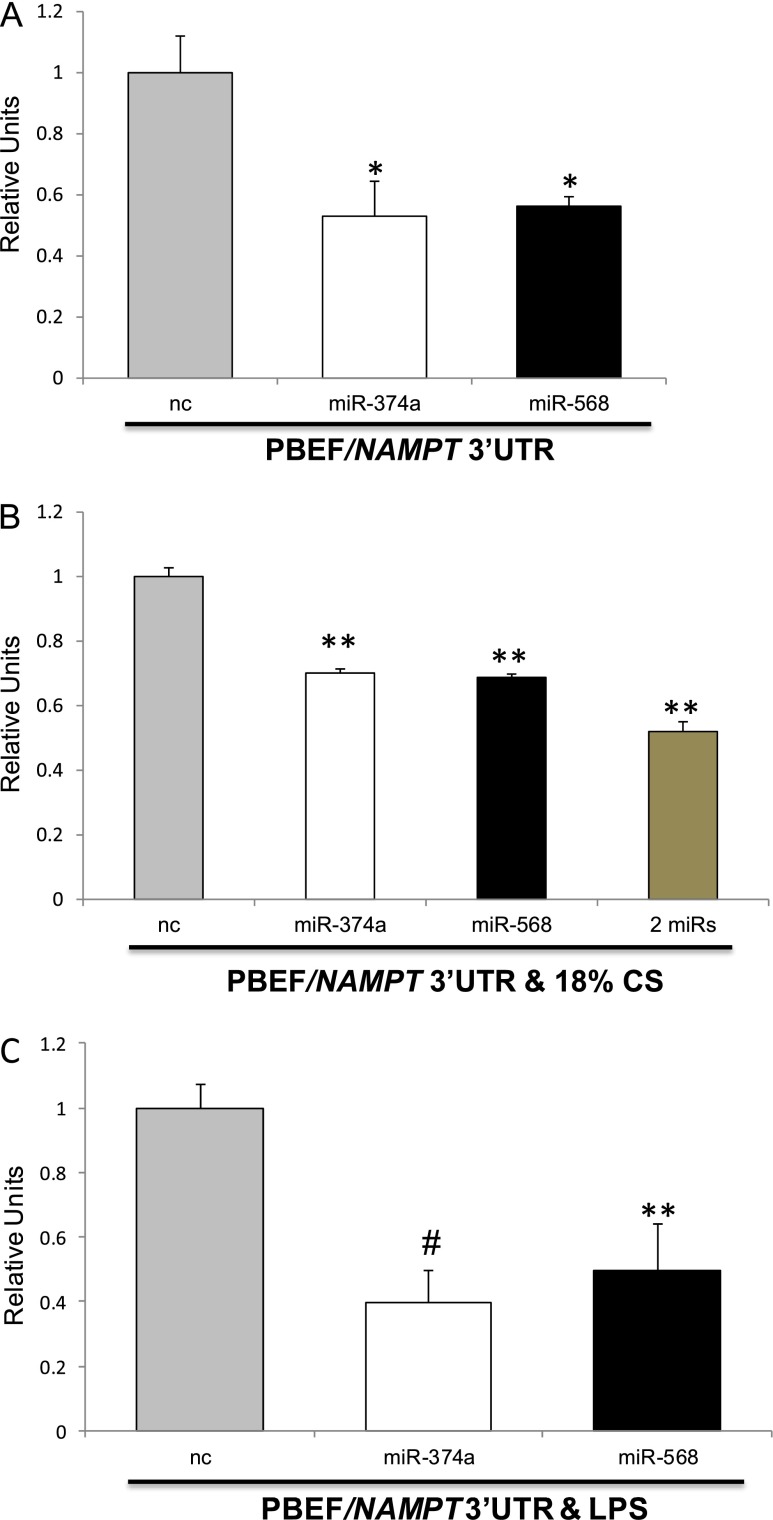
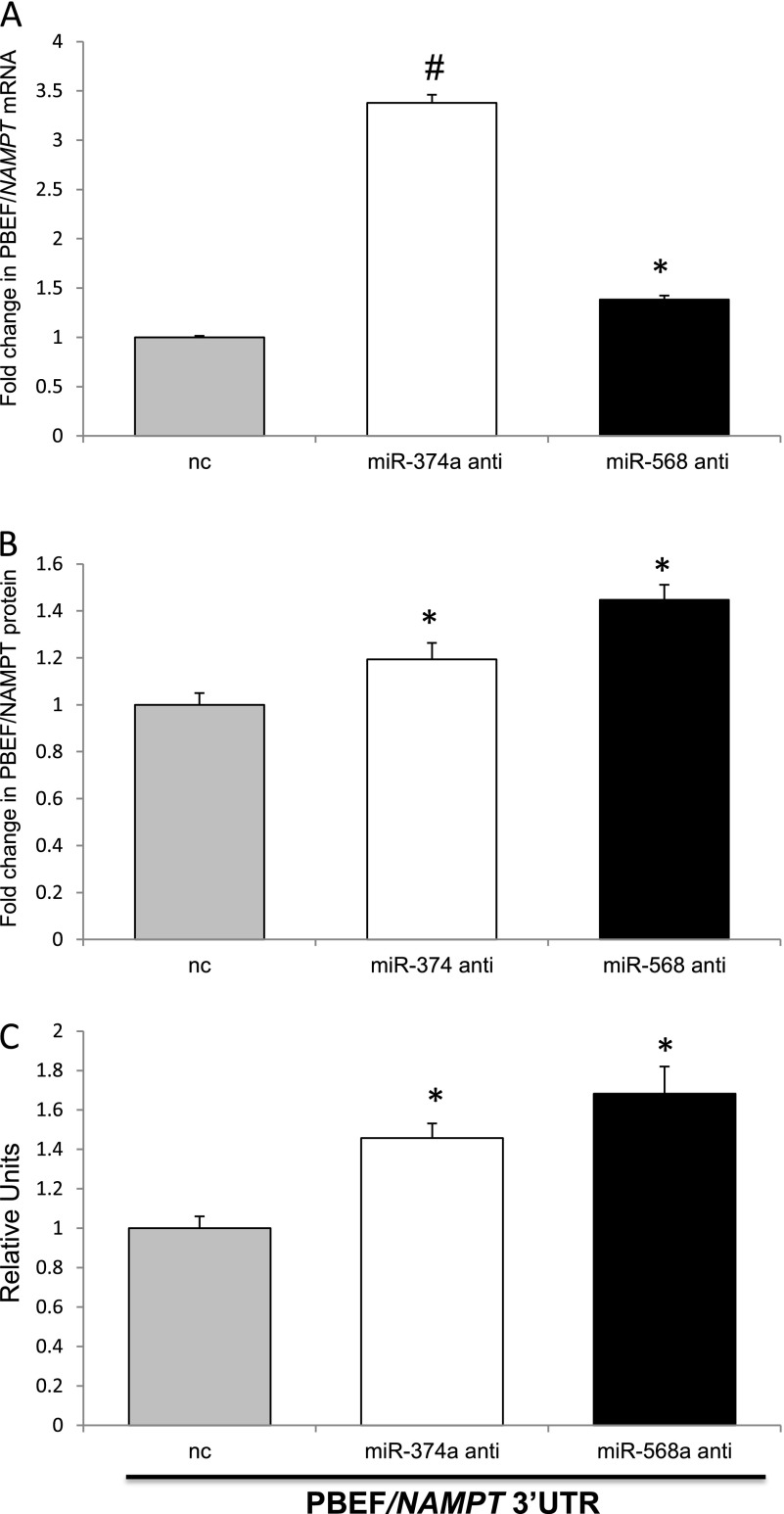
To assess the potential role of miR-374a and miR-568 in 18% CS- or LPS-induced regulation of PBEF/NAMPT expression, we conducted gain- and loss-of-function experiments by transfecting ECs with negative control miRNA mimics or synthetic mimics and/or specific miRNA antagomirs for miR-374a or miR-568. Figures 4A and 4B and Figures 5A–5C depict the significant decreases in PBEF/NAMPT mRNA and protein levels after exposure of ECs to LPS or 18% CS that was produced by miR-374a and miR-568 mimic transfection. However, in cells transfected with miR-374a, miR-568, and with the combination of miR-374a and miR-568 but not exposed to LPS or 18% CS, the basal level of PBEF/NAMPT mRNA not altered significantly (Figures 4A and 4B), suggesting that in static cells the steady-state level of mRNA is due to the saturation of its 3′-UTRs with endogenous miRs. Transfection of ECs with the combination of miR-374a and miR-568 enhanced the attenuation of LPS-induced PBEF/NAMPT transcript levels, suggesting that these miRNAs may have additive or synergistic effects in the setting of LPS-induced EC responses. Consistent with these results, overexpression of miR-374a and miR-568 mimics significantly attenuated basal 3′-UTR reporter activity (Figure 6A) (47 ± 11% and 44 ± 3.1%, respectively, compared with stimulated ECs) as well as 3′-UTR reporter activity after exposure to 18% CS (Figure 6B) (30 ± 1.25% and 31.2 ± 1.0%, respectively) and LPS (60.4 ± 6% and 50.45 ± 4.4%, respectively) (Figure 6C). Combined overexpression of miR-374a and miR-568 mimics enhances the attenuation of 3′-UTR reporter activity after EC exposure to 18% CS (Figure 6B), again suggesting cooperative regulation by these miRNAs. Conversely, Figures 7A and 7B demonstrate that miR-374a and miR-568 antagomirs enhance levels of endogenous PBEF/NAMPT mRNA (3.38 ± 0.08 FI for hsa-miR-374a antagomir; 1.39 ± 0.028 FI for hsa-miR-568 antagomir) and protein levels (1.2 ± 0.13 FI for hsa-miR-374a antagomir; 1.4 ± 0.1 FI for hsa-miR-568 antagomir) in ECs (compared with ECs transfected with negative antagomir control). Furthermore, these antagomirs enhance PBEF/NAMPT 3′-UTR reporter activity in ECs (1.4 ± 0.1 FI for hsa-miR-374a antagomir; 1.8 ± 0.1 FI for hsa-miR-568 antagomir) compared with negative antagomir controls (Figure 7C). Together, these data suggest that miR-374a and miR-568 strongly influence PBEF/NAMPT gene and protein expression.
Figure 4.
Effect of miRNA mimics on inflammatory agonist–induced PBEF/NAMPT transcription in human lung ECs. Total RNA was isolated from ECs, transfected with nc or with the indicated miRNA mimics (48 h) and untreated (A and B), exposed to 18% CS (A, 2 h), or treated with LPS (B, 4 h). PBEF/NAMPT mRNA levels were detected via real-time PCR. Transfection was performed with miR-1290 used as the second negative control. Data are presented as fold change in mRNA level over vehicle-treated control and expressed as means ± SE from four independent experiments.
Figure 5.
Effect of microRNA (miRNA) mimics on inflammatory agonist–induced PBEF/NAMPT expression in human lung ECs. ECs were transfected with nc or with the indicated miRNA mimics (48 h) and exposed to 18% CS (10 h) or LPS (B, 48 h), and endogenous PBEF/NAMPT protein was detected via immunoblots. The bar graphs represent relative densitometry (18% CS [A]; LPS [C]). Data are presented as fold changes in PBEF/NAMPT compared with nc or corresponding miRNA pretreatment without agonist challenge and expressed as means ± SE from three independent experiments. *P < 0.05 versus unstimulated control. #P < 0.01 versus unstimulated control.
Figure 6.
Effect of miRNA mimics on inflammatory agonist–induced PBEF/NAMPT 3′-UTR reporter activity in human lung ECs. ECs were cotransfected with PBEF/NAMPT 3′-UTR reporter together with nc or with the indicated miRNA mimics and phRL-TK, a Renilla luciferase normalization control vector. ECs were untreated and exposed to 18% CS (A) or treated with LPS (C) (24 h) (B), and luciferase activity was measured according the manufacturer’s protocol. Data are presented as relative luciferase units over vehicle-treated control and expressed as means ± SE from four independent experiments. *Significantly different from control cells without stimulation (P < 0.05). **Significantly different from control cells stimulated with 18% CS or LPS (P < 0.05). #Significantly different from control cells stimulated with 18% CS or LPS (P < 0.01).
Figure 7.
Effects of miRNA antagomirs on inflammatory agonist–induced PBEF/NAMPT expression and 3′-UTR reporter activity. Total RNA was isolated from ECs and transfected with nc or with the indicated miRNA. Anti- and PBEF/NAMPT mRNA levels were detected via real-time PCR (A). Data are presented as fold change in mRNA level over control and expressed as means ± SE from four independent experiments. *Significantly different from control cells (P < 0.05). #Significantly different from control cells (P < 0.01). ECs transfected with nc or with the indicated miRNA anti- and endogenous PBEF/NAMPT protein were detected via immunoblot. The bar graph represents relative densitometry (B). Data are presented as fold changes in endogenous PBEF/NAMPT over nc pretreatment and expressed as means ± SE from three independent experiments. *P < 0.05 versus control. ECs were cotransfected with the PBEF/NAMPT 3′-UTR reporter together with phRL-TK, nc, or with the indicated miRNA (C), and luciferase activity was measured according the manufacturer’s protocol. Data are presented as relative luciferase units over control and expressed as means ± SE from four independent experiments. *Significantly different from control cells (P < 0.05).
Discussion
The pulmonary vascular endothelium is a monolayer of ECs and serves as a semiselective barrier between circulating blood and surrounding tissues, with EC integrity being critical to tissue and organ function. EC dysfunction disrupts this vascular barrier and triggers loss of cell–cell adhesion, prooxidation, and an increase in EC permeability and proliferation, a process implicated in inflammatory diseases such as ALI, ARDS, and VILI. The molecular mechanisms that facilitate these phenotypic alterations are only partially understood. In our previous studies (7), PBEF/NAMPT was identified as a novel candidate gene in human inflammatory lung injuries such as VILI and novel biomarker of ARDS and sepsis, with increased PBEF expression in murine, canine, and human ARDS models, which was spatially localized to lung epithelium, leukocytes, and lung vascular endothelium. However, the exact regulatory mechanisms of PBEF/NAMPT expression modulation in the pathogenesis of ARDS and VILI, including epigenetic regulation via the 3′-UTR, are unknown. The 3′-UTR is a versatile region that is enriched in regulatory elements modulating processes such as mRNA stabilization, polyadenylation, transcript degradation, translation, and mRNA localization. Thus, the 3′-UTR is critical for integrated regulation of gene expression. In silico analysis revealed that, compared with the promoter region, 3′-UTR regulatory motifs are preferentially conserved only on one strand, consistent with posttranscriptional impact (42). In addition, 3′-UTRs contain highly conserved sequences that are complementary to miRNA 8-mer motifs, which are believed to represent binding sites for conserved miRNAs, and consequently 3′-UTRs have emerged as target sites for multiple miRNAs (43). The 3′-UTR length is a major determinant in mRNA expression, with longer 3′-UTRs being more likely to possess miRNA-binding sites that inhibit mRNA translation than short 3′-UTRs (43, 44). In this regard, the PBEF/NAMPT gene exhibits an extended 3′-UTR (2,809 base pairs) and led to our speculation that PBEF/NAMPT expression may be influenced by VILI- and ARDS-modulating miRNAs, consistent with the recognition that miRNAs are important modulators of endothelial function in vascular diseases and critical to the regulation of multiple inflammatory processes (45–48). Therefore, miRNAs represent promising therapeutic targets and biomarkers for ALI/ARDS and VILI and facilitate the realization of personalized medicine for individuals with acute inflammatory lung disease. MiRNAs are inhibited by chemically stable complimentary oligonucleotides (or anti-miRs), or their activity is mimicked by miRNA mimics. Overall, the successful studies in rodents and nonhuman primates, as well as the preliminary results on clinical trials, demonstrate that inhibition and overexpression of miRNAs is a promising therapeutic tool (reviewed in Reference 49). MiRNA studies will facilitate the construction of a comprehensive disease model for ALI/ARDS or VILI by applying a systems biology approach that integrates genetic, genomic, epigenetic, proteomic, and environmental information. These speculations do not preclude the contribution of additional regulatory elements such as AU-rich elements, alternative 3′-UTRs, 5′ and 3′ ends of mRNA interaction, 3′-UTR secondary structure, and 3′-UTR binding regulatory proteins in 3′-UTR–mediated control of PBEF/NAMPT gene expression. Further investigation into the regulatory function of the PBEF/NAMPT 3′-UTR is needed.
Because in silico bioinformatic analyses revealed the 3′-UTR of PBEF to contain binding sites for miR-374a and miR-568, we sought to define their participation in the regulation of inflammatory agonist–induced PBEF/NAMPT gene expression (18% CS and LPS). Previously, we indicated that expression of the broadly conserved mature miR-374a (50) is significantly decreased by 18% CS, TNF-α, or LPS (37). We now demonstrate that miR-568 is expressed in ECs with significant down-regulation by 18% CS and LPS (Figure 2). In the present study, we found that PBEF/NAMPT expression in ECs is markedly up-regulated at mRNA and protein levels in response to 18% CS and LPS (Figure 1). Our combined data (37, 39, 51) demonstrate the negative correlation between expression levels of putative miRNA and mRNA/protein and suggest that down-regulation of these miRNAs may contribute to augmented PBEF/NAMPT gene expression in ECs treated with these proinflammatory agonists. To further evaluate whether miR-374a and miR-568 specifically regulate PBEF/NAMPT expression in ECs, transfection with synthetic miRNA mimics and antagomirs was used. We previously reported that targeting PBEF/NAMPT by specific siRNAs (11) or by miR-374a (37) attenuates inflammatory agonist (thrombin, IL-1β, and LPS)-mediated EC hyperpermeability, consistent with the key regulatory role of PBEF in inducing lung inflammation, vascular permeability, and pathobiology (11, 13, 14). Similarly, our data demonstrate that miR-568 mimics attenuate LPS-induced permeability in ECs (Figures 3A and 3B). These mRNAs (miR-374a and miR-568) may modulate LPS-induced EC permeability by targeting the PBEF/NAMPT 3′-UTR, thus altering expression. We found that transfection of ECs with mimics of miR-374a and miR-568 significantly attenuated the 18% CS– and LPS-induced augmented PBEF/NAMPT mRNA and protein levels (Figures 4A and 4B and 5A–5C). Although the exact mechanism by which miR-374a and miR-568 mimics alter PBEF/NAMPT expression is not known, our data support recent evidence that the majority of mammalian miRNAs directly target mRNA down-regulation via cleavage and degradation (52, 53) or accelerated deadenylation of mRNAs (54, 55).
We further investigated the role of miRNAs in the regulation of PBEF/NAMPT expression by using a luciferase 3′-UTR reporter gene system, a sensitive method for measuring miRNA and the 3′-UTR effects on gene regulation. Our data demonstrated that EC exposure to these miRNAs significantly attenuates basal PBEF/NAMPT 3′-UTR reporter activity (Figure 6A) as well as 18% CS- and LPS-induced increases in luciferase activity (Figures 6B and 6C). Because miRNA overexpression produces false-positive results by targeting genes not affected in physiologic conditions (i.e., “off-target effects”), we used the complementary “loss-of-function” approach by inhibiting specific endogenous miRNA function via antagomirs and demonstrated that specific miRNA antagomirs increase PBEF/NAMPT expression (Figures 7A and 7B) and 3′-UTR reporter activity (Figure 7C). Thus, our studies clearly demonstrate that miRNAs miR-374a and miR-568 strongly influence PBEF/NAMPT expression. Our data indicate that these two miRNAs cooperatively regulate PBEF/NAMPT expression in human pulmonary ECs (Figures 4B and 6B).
PBEF/NAMPT is a key participant in VILI pathogenesis and is a critical biomarker of diverse inflammatory pathobiologies such as sepsis, pneumonia, and ARDS (7, 9), potentially via direct effects on innate immunity, apoptosis, and mitochondrial function. Information is limited concerning the possible regulatory mechanisms of PBEF/NAMPT expression via the 5′ and 3′ gene regions; however, our in silico analysis of the 5′ PBEF/NAMPT promoter region by using the Genomatix genome analyzer revealed several putative cis regulatory elements, including sites for binding by transcription activators (e.g., NF-kB, SP1, STAT, and GATA-1) and sequences of homology to antioxidant-, shear stress–, and stretch-responsive elements (unpublished data). In addition, we noted novel CpG islands in the PBEF/NAMPT promoter, suggesting epigenetic regulation of PBEF/NAMPT expression via DNA methylation and 5′ promoter interacting elements. The current study demonstrates that mature expression of miR-374a and miR-568 epigenetically regulates LPS and 18% CS–induced PBEF/NAMPT expression in human pulmonary ECs via 3′-UTR modulation. Future studies are needed to demonstrate whether miRNAs and other regulatory elements synergistically participate in PBEF/NAMPT gene regulation. Targeting of PBEF/NAMPT, a critical inflammatory biomarker in ARDS and VILI, via specific miRNAs is a potentially promising novel therapeutic strategy to reduce lung vascular permeability/edema and inflammation in ARDS and VILI.
Acknowledgments
Acknowledgments
The authors thank Lakshmi Natarajan for providing assistance with the endothelial cell cultures.
Footnotes
This work was supported by National Institutes of Health/Heart Lung Blood Institute grants P01 HL58064, P01 HL98050, and R01 HL94394.
Originally Published in Press as DOI: 10.1165/rcmb.2013-0292OC on September 20, 2013
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Levitt JE, Matthay MA. Treatment of acute lung injury: historical perspective and potential future therapies. Semin Respir Crit Care Med. 2006;27:426–437. doi: 10.1055/s-2006-948296. [DOI] [PubMed] [Google Scholar]
- 2.Leaver SK, Evans TW. Acute respiratory distress syndrome. BMJ. 2007;335:389–394. doi: 10.1136/bmj.39293.624699.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353:1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]
- 4.Ognjanovic S, Bao S, Yamamoto SY, Garibay-Tupas J, Samal B, Bryant-Greenwood GD. Genomic organization of the gene coding for human pre-b-cell colony enhancing factor and expression in human fetal membranes. J Mol Endocrinol. 2001;26:107–117. doi: 10.1677/jme.0.0260107. [DOI] [PubMed] [Google Scholar]
- 5.Rongvaux A, Shea RJ, Mulks MH, Gigot D, Urbain J, Leo O, Andris F. Pre-b-cell colony-enhancing factor, whose expression is up-regulated in activated lymphocytes, is a nicotinamide phosphoribosyltransferase, a cytosolic enzyme involved in NAD biosynthesis. Eur J Immunol. 2002;32:3225–3234. doi: 10.1002/1521-4141(200211)32:11<3225::AID-IMMU3225>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 6.Sommer G, Garten A, Petzold S, Beck-Sickinger AG, Bluher M, Stumvoll M, Fasshauer M. Visfatin/PBEF/Nampt: structure, regulation and potential function of a novel adipokine. Clin Sci (Lond) 2008;115:13–23. doi: 10.1042/CS20070226. [DOI] [PubMed] [Google Scholar]
- 7.Ye SQ, Simon BA, Maloney JP, Zambelli-Weiner A, Gao L, Grant A, Easley RB, McVerry BJ, Tuder RM, Standiford T, et al. Pre-b-cell colony-enhancing factor as a potential novel biomarker in acute lung injury. Am J Respir Crit Care Med. 2005;171:361–370. doi: 10.1164/rccm.200404-563OC. [DOI] [PubMed] [Google Scholar]
- 8.Hug C, Lodish HF. Medicine. Visfatin: a new adipokine. Science. 2005;307:366–367. doi: 10.1126/science.1106933. [DOI] [PubMed] [Google Scholar]
- 9.Hong SB, Huang Y, Moreno-Vinasco L, Sammani S, Moitra J, Barnard JW, Ma SF, Mirzapoiazova T, Evenoski C, Reeves RR, et al. Essential role of pre-b-cell colony enhancing factor in ventilator-induced lung injury. Am J Respir Crit Care Med. 2008;178:605–617. doi: 10.1164/rccm.200712-1822OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bajwa EK, Yu CL, Gong MN, Thompson BT, Christiani DC. Pre-b-cell colony-enhancing factor gene polymorphisms and risk of acute respiratory distress syndrome. Crit Care Med. 2007;35:1290–1295. doi: 10.1097/01.CCM.0000260243.22758.4F. [DOI] [PubMed] [Google Scholar]
- 11.Ye SQ, Zhang LQ, Adyshev D, Usatyuk PV, Garcia AN, Lavoie TL, Verin AD, Natarajan V, Garcia JG. Pre-b-cell-colony-enhancing factor is critically involved in thrombin-induced lung endothelial cell barrier dysregulation. Microvasc Res. 2005;70:142–151. doi: 10.1016/j.mvr.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Jia SH, Li Y, Parodo J, Kapus A, Fan L, Rotstein OD, Marshall JC. Pre-b cell colony-enhancing factor inhibits neutrophil apoptosis in experimental inflammation and clinical sepsis. J Clin Invest. 2004;113:1318–1327. doi: 10.1172/JCI19930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu P, Li H, Cepeda J, Zhang LQ, Cui X, Garcia JG, Ye SQ. Critical role of PBEF expression in pulmonary cell inflammation and permeability. Cell Biol Int. 2009;33:19–30. doi: 10.1016/j.cellbi.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li H, Liu P, Cepeda J, Fang D, Easley RB, Simon BA, Zhang LQ, Ye SQ. Augmentation of pulmonary epithelial cell IL-8 expression and permeability by pre-b-cell colony enhancing factor. J Inflamm (Lond) 2008;5:15. doi: 10.1186/1476-9255-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dahl TB, Yndestad A, Skjelland M, Oie E, Dahl A, Michelsen A, Damas JK, Tunheim SH, Ueland T, Smith C, et al. Increased expression of visfatin in macrophages of human unstable carotid and coronary atherosclerosis: possible role in inflammation and plaque destabilization. Circulation. 2007;115:972–980. doi: 10.1161/CIRCULATIONAHA.106.665893. [DOI] [PubMed] [Google Scholar]
- 16.Tomankova T, Petrek M, Kriegova E. Involvement of microRNAs in physiological and pathological processes in the lung. Respir Res. 2010;11:159. doi: 10.1186/1465-9921-11-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sokolov MV, Panyutin IV, Neumann RD. Unraveling the global microRNAome responses to ionizing radiation in human embryonic stem cells. PLoS ONE. 2012;7:e31028. doi: 10.1371/journal.pone.0031028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ji F, Lv X, Jiao J. The role of micrornas in neural stem cells and neurogenesis. J Genet Genomics. 2013;40:61–66. doi: 10.1016/j.jgg.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 19.Zhou T, Garcia JG, Zhang W. Integrating microRNAs into a system biology approach to acute lung injury. Transl Res. 2011;157:180–190. doi: 10.1016/j.trsl.2011.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ranjha R, Paul J. Micro-RNAs in inflammatory diseases and as a link between inflammation and cancer. Inflamm Res. 2013;62:343–355. doi: 10.1007/s00011-013-0600-9. [DOI] [PubMed] [Google Scholar]
- 21.Kornfeld JW, Baitzel C, Konner AC, Nicholls HT, Vogt MC, Herrmanns K, Scheja L, Haumaitre C, Wolf AM, Knippschild U, et al. Obesity-induced overexpression of miR-802 impairs glucose metabolism through silencing of Hnf1b. Nature. 2013;494:111–115. doi: 10.1038/nature11793. [DOI] [PubMed] [Google Scholar]
- 22.Li N, Zhong X, Lin X, Guo J, Zou L, Tanyi JL, Shao Z, Liang S, Wang LP, Hwang WT, et al. Lin-28 homologue A (LIN28A) promotes cell cycle progression via the regulation of cyclin-dependent kinase 2 (CDK2), cyclin D1 (CCND1), and cell division cycle 25 homolog A (CDC25A) expression in cancer. J Biol Chem. 2012;287:17386–17397. doi: 10.1074/jbc.M111.321158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grosso S, Doyen J, Parks SK, Bertero T, Paye A, Cardinaud B, Gounon P, Lacas-Gervais S, Noel A, Pouyssegur J, et al. MiR-210 promotes a hypoxic phenotype and increases radioresistance in human lung cancer cell lines. Cell Death Dis. 2013;4:e544. doi: 10.1038/cddis.2013.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Creemers EE, Tijsen AJ, Pinto YM. Circulating microRNAs: Novel biomarkers and extracellular communicators in cardiovascular disease? Circ Res. 2012;110:483–495. doi: 10.1161/CIRCRESAHA.111.247452. [DOI] [PubMed] [Google Scholar]
- 25.Kohlstedt K, Trouvain C, Boettger T, Shi L, Fisslthaler B, Fleming I. The AMP-activated protein kinase regulates endothelial cell angiotensin-converting enzyme expression via p53 and the post-transcriptional regulation of microRNA-143/145. Circ Res. 2013;112:1150–1158. doi: 10.1161/CIRCRESAHA.113.301282. [DOI] [PubMed] [Google Scholar]
- 26.Zhao JL, Rao DS, Boldin MP, Taganov KD, O'Connell RM, Baltimore D. NF-kappaB dysregulation in microRNA-146a-deficient mice drives the development of myeloid malignancies. Proc Natl Acad Sci USA. 2011;108:9184–9189. doi: 10.1073/pnas.1105398108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Persengiev SP. MiRNAs at the crossroad between hematopoietic malignancies and autoimmune pathogenesis. Discov Med. 2012;13:211–221. [PubMed] [Google Scholar]
- 28.Liu N, Landreh M, Cao K, Abe M, Hendriks GJ, Kennerdell JR, Zhu Y, Wang LS, Bonini NM. The microRNA miR-34 modulates ageing and neurodegeneration in drosophila. Nature. 2011;482:519–523. doi: 10.1038/nature10810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garcia JG, Liu F, Verin AD, Birukova A, Dechert MA, Gerthoffer WT, Bamburg JR, English D. Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement. J Clin Invest. 2001;108:689–701. doi: 10.1172/JCI12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lewis BP, Burge CB, Bartel DP. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell. 2005;120:15–20. doi: 10.1016/j.cell.2004.12.035. [DOI] [PubMed] [Google Scholar]
- 31.Grimson A, Farh KK, Johnston WK, Garrett-Engele P, Lim LP, Bartel DP. MicroRNA targeting specificity in mammals: determinants beyond seed pairing. Mol Cell. 2007;27:91–105. doi: 10.1016/j.molcel.2007.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Betel D, Wilson M, Gabow A, Marks DS, Sander C. The microRNA.Org resource: targets and expression. Nucleic Acids Res. 2008;36:D149–D153. doi: 10.1093/nar/gkm995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maragkakis M, Reczko M, Simossis VA, Alexiou P, Papadopoulos GL, Dalamagas T, Giannopoulos G, Goumas G, Koukis E, Kourtis K, et al. Diana-micro t web server: elucidating microrna functions through target prediction. Nucleic Acids Res. 2009;37:W273–W276. doi: 10.1093/nar/gkp292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adyshev DM, Moldobaeva NK, Elangovan VR, Garcia JG, Dudek SM. Differential involvement of ezrin/radixin/moesin proteins in sphingosine 1-phosphate-induced human pulmonary endothelial cell barrier enhancement. Cell Signal. 2011;23:2086–2096. doi: 10.1016/j.cellsig.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mitra S, Sammani S, Wang T, Boone DL, Meyer NJ, Dudek SM, Moreno-Vinasco L, Garcia JG, Jacobson JR. Role of growth arrest and DNA damage-inducible alpha in Akt phosphorylation and ubiquitination after mechanical stress-induced vascular injury. Am J Respir Crit Care Med. 2011;184:1030–1040. doi: 10.1164/rccm.201103-0447OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gao L, Grant A, Halder I, Brower R, Sevransky J, Maloney JP, Moss M, Shanholtz C, Yates CR, Meduri GU, et al. Novel polymorphisms in the myosin light chain kinase gene confer risk for acute lung injury. Am J Respir Cell Mol Biol. 2006;34:487–495. doi: 10.1165/rcmb.2005-0404OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adyshev DM, Moldobaeva N, Mapes B, Elangovan V, Garcia JG. MicroRNA regulation of non-muscle myosin light chain kinase (nmmlck) expression in human lung endothelium. Am J Respir Cell Mol Biol. 2013;49:58–66. doi: 10.1165/rcmb.2012-0397OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bartel DP. Micrornas: target recognition and regulatory functions. Cell. 2009;136:215–233. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Witkos TM, Koscianska E, Krzyzosiak WJ. Practical aspects of microRNA target prediction. Curr Mol Med. 2011;11:93–109. doi: 10.2174/156652411794859250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Place RF, Li LC, Pookot D, Noonan EJ, Dahiya R. MicroRNA-373 induces expression of genes with complementary promoter sequences. Proc Natl Acad Sci USA. 2008;105:1608–1613. doi: 10.1073/pnas.0707594105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vasudevan S, Tong Y, Steitz JA. Switching from repression to activation: micrornas can up-regulate translation. Science. 2007;318:1931–1934. doi: 10.1126/science.1149460. [DOI] [PubMed] [Google Scholar]
- 42.Xie X, Lu J, Kulbokas EJ, Golub TR, Mootha V, Lindblad-Toh K, Lander ES, Kellis M. Systematic discovery of regulatory motifs in human promoters and 3′ UTRs by comparison of several mammals. Nature. 2005;434:338–345. doi: 10.1038/nature03441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barrett LW, Fletcher S, Wilton SD. Regulation of eukaryotic gene expression by the untranslated gene regions and other non-coding elements. Cell Mol Life Sci. 2012;69:3613–3634. doi: 10.1007/s00018-012-0990-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stark A, Brennecke J, Bushati N, Russell RB, Cohen SM. Animal MicroRNAs confer robustness to gene expression and have a significant impact on 3′UTR evolution. Cell. 2005;123:1133–1146. doi: 10.1016/j.cell.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 45.Taganov KD, Boldin MP, Chang KJ, Baltimore D. NF-kappaB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc Natl Acad Sci USA. 2006;103:12481–12486. doi: 10.1073/pnas.0605298103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.O'Connell RM, Chaudhuri AA, Rao DS, Baltimore D. Inositol phosphatase SHIP1 is a primary target of miR-155. Proc Natl Acad Sci USA. 2009;106:7113–7118. doi: 10.1073/pnas.0902636106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bazzoni F, Rossato M, Fabbri M, Gaudiosi D, Mirolo M, Mori L, Tamassia N, Mantovani A, Cassatella MA, Locati M. Induction and regulatory function of miR-9 in human monocytes and neutrophils exposed to proinflammatory signals. Proc Natl Acad Sci USA. 2009;106:5282–5287. doi: 10.1073/pnas.0810909106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moschos SA, Williams AE, Perry MM, Birrell MA, Belvisi MG, Lindsay MA. Expression profiling in vivo demonstrates rapid changes in lung microRNA levels following lipopolysaccharide-induced inflammation but not in the anti-inflammatory action of glucocorticoids. BMC Genomics. 2007;8:240. doi: 10.1186/1471-2164-8-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chamorro-Jorganes A, Araldi E, Suarez Y. MicroRNAs as pharmacological targets in endothelial cell function and dysfunction. Pharmacol Res. 2013;75:15–27. doi: 10.1016/j.phrs.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang R, Su B. Small but influential: the role of micrornas on gene regulatory network and 3'utr evolution. J Genet Genomics. 2009;36:1–6. doi: 10.1016/S1673-8527(09)60001-1. [DOI] [PubMed] [Google Scholar]
- 51.Nielsen JA, Lau P, Maric D, Barker JL, Hudson LD. Integrating microRNA and mRNA expression profiles of neuronal progenitors to identify regulatory networks underlying the onset of cortical neurogenesis. BMC Neurosci. 2009;10:98. doi: 10.1186/1471-2202-10-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bagga S, Bracht J, Hunter S, Massirer K, Holtz J, Eachus R, Pasquinelli AE. Regulation by let-7 and lin-4 miRNAs results in target mRNA degradation. Cell. 2005;122:553–563. doi: 10.1016/j.cell.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 53.Liu Z, Wang D, Hu Y, Zhou G, Zhu C, Yu Q, Chi Y, Cao Y, Jia C, Zou Q. MicroRNA-146a negatively regulates PTGS2 expression induced by helicobacter pylori in human gastric epithelial cells. J Gastroenterol. 2013;48:86–92. doi: 10.1007/s00535-012-0609-9. [DOI] [PubMed] [Google Scholar]
- 54.Giraldez AJ, Mishima Y, Rihel J, Grocock RJ, Van Dongen S, Inoue K, Enright AJ, Schier AF. Zebrafish mir-430 promotes deadenylation and clearance of maternal mrnas. Science. 2006;312:75–79. doi: 10.1126/science.1122689. [DOI] [PubMed] [Google Scholar]
- 55.Wu L, Fan J, Belasco JG. MicroRNAs direct rapid deadenylation of mRNA. Proc Natl Acad Sci USA. 2006;103:4034–4039. doi: 10.1073/pnas.0510928103. [DOI] [PMC free article] [PubMed] [Google Scholar]