Abstract
AIM: To evaluate the efficacy of acupuncture for treatment of irritable bowel syndrome (IBS) through meta-analysis of randomized controlled trials.
METHODS: We searched MEDLIINE, PubMed, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials from 1966 to February 2013 for double-blind, placebo-controlled trials investigating the efficacy of acupuncture in the management of IBS. Studies were screened for inclusion based on randomization, controls, and measurable outcomes reported. We used the modified Jadad score for assessing the quality of the articles. STATA 11.0 and Revman 5.0 were used for meta-analysis. Publication bias was assessed by Begg’s and Egger’s tests.
RESULTS: Six randomized, placebo-controlled clinical trials met the criteria and were included in the meta-analysis. The modified Jadad score of the articles was > 3, and five articles were of high quality. We analyzed the heterogeneity and found that these studies did not cause heterogeneity in our meta-analysis. Begg’s test showed P = 0.707 and Egger’s test showed P = 0.334. There was no publication bias in our meta-analysis (Begg’s test, P = 0.707; Egger’s test, P = 0.334). From the forest plot, the diamond was on the right side of the vertical line and did not intersect with the line. The pooled relative risk for clinical improvement with acupuncture was 1.75 (95%CI: 1.24-2.46, P = 0.001). Using the two different systems of STATA 11.0 and Revman 5.0, we confirmed the significant efficacy of acupuncture for treating IBS.
CONCLUSION: Acupuncture exhibits clinically and statistically significant control of IBS symptoms.
Keywords: Irritable bowel syndrome, Functional gastrointestinal disorder, Acupuncture, Meta-analysis
Core tip: Irritable bowel syndrome (IBS) is not life-threatening, but leads to significant impairment of health-related quality of life. There is still no universally accepted satisfactory treatment for IBS. Nowadays, acupuncture is increasingly popular in patients with various diseases. Several studies showed an improvement in quality of life in IBS patients after acupuncture, but other studies showed no improvement. We performed a meta-analysis to establish the therapeutic efficacy of acupuncture for IBS.
INTRODUCTION
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by chronic or recurrent abdominal pain or discomfort, which is associated with disturbed bowel function and feelings of abdominal distention and bloating[1]. It is the most common reason that patients seek medical advice from primary care physicians and gastroenterologists. The prevalence of IBS reaches 7%-10% worldwide depending on the criteria used for diagnosis[2]. It is a common gastrointestinal disorder, affecting 10%-15% of the population in developed countries[3]. IBS is associated with a significant reduction in health-related quality of life[4]. Estimates of annual direct and indirect costs associated with IBS exceed 41 billion dollars in major industrial countries[5].
IBS is caused by multiple factors, although its nosogenesis is not clearly known. The causative factors include intestinal motility and intestinal smooth muscle functional disturbance, visceral paresthesia, alterations in the brain-gut axis, psychological factors, gastrointestinal hormones, and intestinal infection. The pathophysiology of IBS includes alterations in intestinal motility, visceral hypersensitivity, and abnormalities in the processing of visceral information[6]. IBS affects all age groups and it is believed that factors such as familial aggregation, early life events, diet and psychosocial conditions might drive disease development[7]. The disease is not life-threatening, but leads to significant impairment of health-related quality of life, which causes physical role limitations as well as pain and a lower perception of general health[8]. Despite numerous studies targeting treatment of IBS[9,10], there is still no universally accepted satisfactory treatment for this condition. Systematic reviews of conventional medications for IBS have found that the evidence for drug efficacy is weak[11], and that no drug is effective in treating all the symptoms of IBS[12].
Acupuncture has become increasingly popular in patients with various diseases, including IBS[13]. Several recently published studies of acupuncture showed improvement in quality of life, regardless of whether it was traditional or sham acupuncture[14-16]. In patients with IBS, no significant difference in quality of life improvement was observed after treatment with true or sham acupuncture[17,18]. Another study[19] showed that acupuncture for IBS provided an additional benefit over usual care alone. We performed a meta-analysis of randomized controlled trials to assess whether there was any benefit of acupuncture in improving symptoms or health-related quality of life in patients with IBS.
MATERIALS AND METHODS
Search strategy
We searched MEDLINE, PubMed, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials for studies investigating the efficacy of acupuncture for IBS. Data published from 1966 to February 2013 were collected. The search terms were: “acupuncture” or “acupuncture and moxibustion”, and “irritable bowel”, “functional bowel diseases” or “irritable colon”. The search was restricted to English-language literature. We searched the references of reviewed articles for additional articles missed by the computerized database search. All primary and review articles, as well as their references, were reviewed independently in duplicate.
Study selection
All controlled trials investigating the efficacy of acupuncture in patients with IBS were considered. Studies were screened for inclusion, through review of the published article, based on the following criteria: randomization, controls, and measurable outcomes reported. Each article was reviewed in duplicate for inclusion, with substantial inter-rater agreement. Trials were disqualified if they were not controlled or their outcomes did not consider efficacy. Reviewers independently extracted data on country, diagnostic criteria, IBS type, assessment, treatment and time.
Methodology quality assessment
We used the modified Jadad score for assessing the quality of the article. Jadad score, which evaluates studies based on their description of randomization, concealment of allocation, double blinding, and dropouts (withdrawals), was used to assess the methodological quality of the trials. The quality scale ranges from 0 to 7 points with a low quality report of score ≤ 3 and a high quality report of score ≥ 4.
Statistical analysis
All analyses were performed using STATA 11.0 and Revman 5.0. Data from selected studies were extracted into 2 × 2 tables. All included studies were weighted and pooled. Relative risk (OR) and 95%CI were calculated and effect size (weighted mean difference) meta-analysis was performed with STATA 11.0 and Revman 5.0. The event rate in the experimental (intervention) group against the event rate in the control group was calculated using a L’Abbe plot as an aid to explore the heterogeneity of effect estimates. In case of homogeneity, a fixed-effect model was used for meta-analysis; otherwise a random-effect model was applied. Publication bias was assessed by Begg’s and Egger’s tests. P ≥ 0.05 indicated that there was no publication bias.
RESULTS
Article selection
The literature search identified 64 citations involving acupuncture and IBS, six of which met our inclusion criteria[6,17,19-22]. Of the 58 excluded articles, 14 were review articles, 10 were not in English, 13 were observational studies from which we could not extract the results, 15 were experimental studies, two did not study efficacy, and four were meta-analyses (Figure 1).
Figure 1.
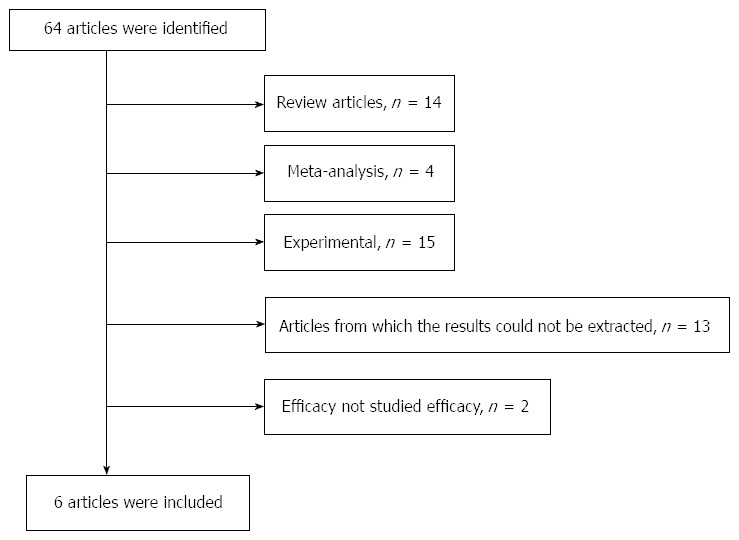
Flow diagram of the study selection process.
Modified Jadad score assessment
The quality of the six articles was assessed by modified Jadad score (Table 1). We found that the score of two articles was > 4, the score of three articles was 4, and one article had a score of 3. Therefore, five articles were of high quality.
Table 1.
Modified Jadad score of the articles
The total number, country, IBS type, diagnostic criteria, assessment mode, time and treatment for each study are reported in Table 2. All subtypes of IBS (diarrhea-predominant, constipation-predominant, and alternating) were incorporated in the included studies. The Rome criteria were used for diagnosis. The control treatment of four studies[6,17,21,22] was sham acupuncture, one[20] was medical treatment, and the other[19] was usual care only. The six studies were conducted in different countries.
Table 2.
Characteristics of papers included in the meta-analysis
| Study | Country | n | Diagnostic criteria | IBS type | Assessment | Time | Acupuncture | Control treatment |
| Macpherson et al[19] | United Kingdom | 233 | Rome criteria | IBS | IBS symptom severity score | 12 wk (every 3 wk) | Offer 10 weekly individualized acupuncture sessions plus usual care | Usual care only |
| Forbes et al[17] | United Kingdom | 59 | Rome I criteria and Manning criteria | IBS | Global symptom score based on patient diary | 13 wk | Individualized 10 sessions over 10 wk | Sham acupuncture at non-acupoints |
| Sun et al[20] | China | 63 | Rome III | IBS-D | Symptom score | 4 wk | Fixed formula; 20 sessions over 4 wk | Pinaverium bromide (50 mg tid) |
| Lembo et al[6] | United States | 230 | Rome II | IBS | IBS adequate relief | 3 wk | Flexible formula; 10 sessions over 3 wk | Sham acupuncture at non-acupoints |
| Lowe et al[22] | Canada | 50 | Rome | IBS | Symptom relief | 4 wk | Fixed formula; 8 sessions over 4 wk | Sham acupuncture - tapping blunt needle on the skin then tapping the needle in place |
| Anastasi et al[21] | United States | 29 | Rome II or Rome III | IBS | Clinical global impression scale | 4 wk (measured 3 wk) | Flexible formula with moxibustion at all points; 8 sessions over 4 wk | Sham acupuncture - superficial needles 2-3 cm |
IBS-D: Irritable bowel syndrome (IBS) with diarrhea.
Heterogeneity test
We performed the heterogeneity test using the χ2 test (χ2 = 3.72, P = 0.59) (Figure 2). We found that the included studies did not cause heterogeneity in our meta-analysis. Therefore, a fixed-effect model was used for meta-analysis.
Figure 2.
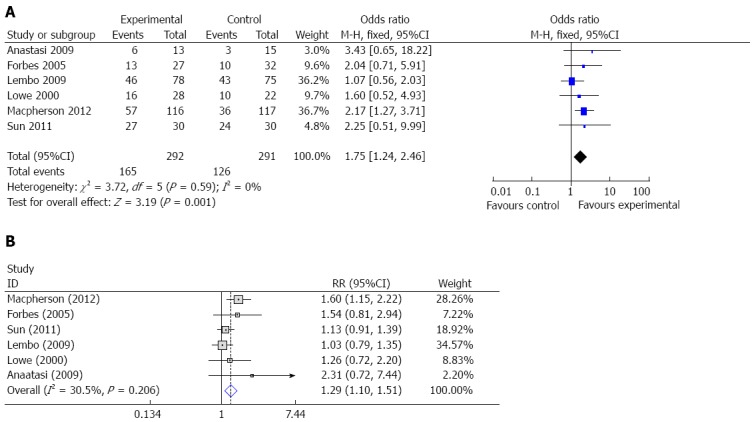
Meta-analysis. A: Meta-analysis of acupuncture for treating Irritable bowel syndrome (IBS) with Revman 5.0; B: Acupuncture for treating IBS with STATA 11.0.
Publication bias assessment
The reason for publication bias was that positive results could be published easily, whereas negative results could not. Or, negative results caused the researchers to abandon their studies, which meant that the negative results were not published, thus affecting the meta-analysis. In our analysis, we performed Begg’s test (Figure 3A) and Egger’s test (Figure 3B), and both the tests indicated that there was no publication bias in our meta-analysis (Begg’s test, P = 0.707; Egger’s test, P = 0.334).
Figure 3.
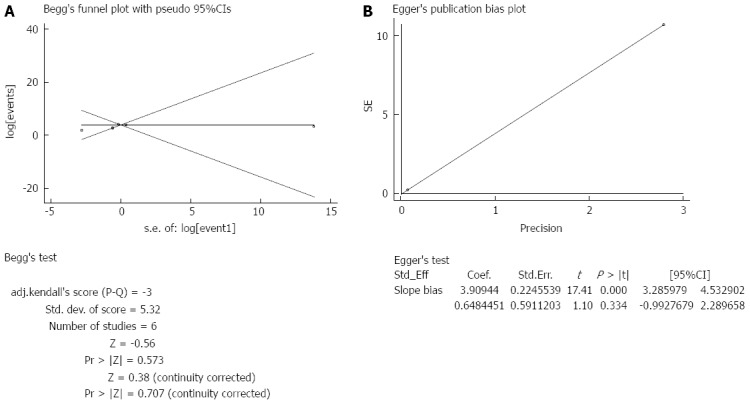
Publication bias. A: Begg’s funnel plot for publication bias; B: Egger’s publication bias plot.
Merging and meta-analysis
The meta-analysis showed that the heterogeneity among the six studies included was not significant (P = 0.59), therefore, we used a fixed-effects model for the meta-analysis. From the forest plot, the diamond was on the right side of the vertical line and did not intersect with the line. From Figure 2A, we found that OR was 1.75 (95%CI: 1.24-2.46, Z = 3.19, P = 0.001) (Figure 2A), which meant that acupuncture had an effect on IBS. However, because the number of included articles was small, further analysis should be done in the future. In order to verify accuracy, we used STATA 11.0 to check the analysis. Figure 2B shows that the diamond was on the right of the vertical line and did not intersect with the line. Therefore, using the two different systems, we confirmed the significant efficacy of acupuncture for treating IBS.
DISCUSSION
IBS is defined as “abdominal pain or discomfort that occurs in association with altered bowel habits over a period of at least 3 mo”[23]. The diagnosis of IBS, a highly prevalent functional gastrointestinal disorder, is currently based on the presence of a characteristic symptom profile (abdominal pain/discomfort, bloating/distension, alterations in defecatory function) in the absence of a demonstrable organic disease of the gastrointestinal tract[24]. The burden of IBS is significant enough to contribute to considerable impairment of quality of life. Patients with IBS have higher healthcare resource utilization than non-IBS patients in terms of more frequent physician visits, more tests, greater medication use, and increased rates of unnecessary surgery[25]. Although IBS is common, its pathophysiology is not completely understood, which poses problems in the search for effective therapeutic approaches.
Although the pathogenesis of IBS is not fully known, a multifactorial involvement of diet, gene mutations, psychosocial factors, and immune-mediated processes is hypothesized[26]. Visceral hypersensitivity and dysregulation of central pain perception in the brain-gut axis are considered to play a pivotal role in the pathophysiology of IBS. One theory regarding the pathophysiology of IBS involves interference of neurotransmission between the central nervous system and the intestines.
IBS can be classified as either diarrhea predominant, constipation predominant, or a mixed form[27]. Due to the wide range of symptoms that may be experienced, the available pharmacological treatments are mainly targeted at symptom reduction. In many studies, we found that pharmacological treatment of IBS varied from antidepressants including tricyclic antidepressants and selective serotonin reuptake inhibitors, to antispasmodics, 5-hydroxytryptamine (5-HT)-3 receptor antagonists, 5-HT4 receptor agonists, antibiotics, probiotics, and melatonin[28]. Effective treatments for IBS are needed to relieve symptoms, improve quality of life, and reduce healthcare utilization. However, acupuncture, a 3000-year-old traditional Chinese medical practice, is receiving increasing acceptance in Western medicine for treating certain medical conditions.
Acupuncture is one of the prominent methods in alternative medicine that has been tried on various disturbances of the digestive tract. It can affect the visceral system by stimulating the somatic system, in accordance with the visceral hyperalgesia theory of the central nervous system[29]. However, previous studies of acupuncture in IBS have not provided conclusive evidence of its efficacy[30]. A Cochrane review of six trials, with a median sample size of 54, found insufficient evidence to determine if acupuncture was an effective treatment for IBS[31]. A systematic review[32] showed unspecific effects of acupuncture for IBS compared with sham acupuncture. Another meta-analysis[33] showed that there was no benefits of acupuncture relative to a credible sham acupuncture control for IBS symptom severity or IBS-related quality of life. A recent study[19] showed that acupuncture for IBS provided an additional benefit. In some studies, acupuncture was believed to alter visceral sensation and motility by stimulating the somatic nervous system and the vagus nerve in IBS[34-36]. Consequently, the real efficacy of acupuncture for IBS is still unclear because the quality of some of the articles included in the systematic review and meta-analysis was poor.
Nevertheless, our meta-analysis of six randomized controlled trials suggests that acupuncture improves the symptoms of IBS, including abdominal pain and distension, sensation of incomplete defecation, times of defecation per day, and state of stool. One study[37] reported that acupuncture might modulate pain in IBS by two actions: (1) modulation of serotonin pathway at insula; and (2) modulation of mood and affection in the higher cortical center via the ascending pathway at the pulvinar and medial nucleus of the thalamus. However, in our analysis, only one article[19] showed a positive effect, so the potential placebo effects of acupuncture should not be dismissed. In our meta-analysis, five of the six articles were of high quality, and there was no publication bias. We used two different operating systems to perform the analysis, and both showed significant differences. No serious adverse events associated with acupuncture were reported in the articles. The mechanism of action of acupuncture for IBS is unclear at present. Most animal experiments on the mechanism of action have been associated with electro-acupuncture. However, one study[38] showed that improvement in pain in IBS was positively associated with increased parasympathetic tone in the acupuncture group.
In our meta-analysis, five articles showed no benefit of acupuncture for IBS, and only one[19] showed a positive effect. However, the meta-analysis showed the benefit of acupuncture. The reason why we obtained a positive end result might have been that the sample size of the positive study was large. The Jadad score of the positive article was 5, and all six included studies were from different countries, therefore, the result was credible. However, the analysis had some limitations. First, the total sample size was not large enough. Second, the treatment mode and the duration were not coincident, thus, we could not confirm how long acupuncture treatment is required to achieve a benefit when treating IBS. Third, because assessment of improvement was not the same and not detailed, it was difficult to assess the effect of acupuncture accurately. Fourth, because the side effects of acupuncture were not recorded in all studies, we could not assess these during treatment of IBS. Fortunately, we did not find any publication bias, which increased the reliability of our meta-analysis. Although our meta-analysis showed that acupuncture was beneficial for IBS patients, we still need further research with larger samples to achieve an accurate result and to explore the functional mechanism of action of acupuncture.
This meta-analysis showed that acupuncture is beneficial for IBS patients. However, this review had some limitations. The data are insufficient to recommend the method as first-line treatment. Moreover, there are insufficient data to establish the long-term results. Therefore, further research is required to assess more accurately the results and mechanism of action of acupuncture for treatment of IBS.
COMMENTS
Background
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by chronic or recurrent abdominal pain or discomfort. IBS can lead to significant impairment of health-related quality of life, which causes physical role limitations as well as pain and a lower perception of general health. There is still no universally accepted satisfactory treatment for this condition.
Research frontiers
Effective treatments for IBS are needed to relieve symptoms, improve quality of life, and reduce healthcare utilization. This study aimed to confirm the efficacy of acupuncture for treatment of IBS. This may help establish the mechanism of action of acupuncture to treat IBS in further research.
Innovations and breakthroughs
It has been found that pharmacological treatment of IBS varied from antidepressants including tricyclic antidepressants and selective serotonin reuptake inhibitors, to antispasmodics, 5-hydroxytryptamine-3 (5-HT3) receptor antagonists, 5-HT4 receptor agonists, antibiotics, probiotics, and melatonin. Despite the numerous studies targeting the treatment of IBS, there is still no universally accepted satisfactory treatment. Nowadays, patients with IBS frequently use complementary medicine including acupuncture. However, the efficacy of acupuncture to treat IBS is still unknown. Some studies of acupuncture treatment of IBS have shown different results. This study was to confirm the effect of acupuncture by meta-analysis.
Applications
The results suggest that acupuncture reduces the symptoms of IBS, without any serious adverse events. The mechanism of action of acupuncture for IBS is unclear.
Terminology
IBS is defined as “abdominal pain or discomfort that occurs in association with altered bowel habits over a period of at least 3 mo.”Acupuncture is one of the prominent methods of alternative medicine that has been tried on various disturbances of the digestive tract. It can affect the visceral system by stimulating the somatic system, in accordance with the visceral hyperalgesia theory of the central nervous system. Jadad score, which evaluates studies based on their description of randomization, concealment of allocation, double blinding, and dropouts (withdrawals), was used to assess the methodological quality of the trials.
Peer review
This is an interesting paper on the effect of acupuncture in IBS. There are few data in this domain. This meta-analysis showed that acupuncture was beneficial for IBS patients. Meta-analysis has some limitations. More research is required so that accurate results can be assessed and the mechanism of action of acupuncture to treat IBS can be confirmed.
Footnotes
Supported by the Youth Fund of National Natural Science Foundation of China, No. 81202828; and the Natural Science Foundation of Zhejiang Province, China, No. LY12H03013; and Academic Climbing Project of the Youth Discipline Leader of Universities in Zhejiang Province (pd2013209)
P- Reviewers: Bonaz BL, Poli-Neto OB, Pehl C S- Editor: Gou SX L- Editor: Wang TQ E- Editor: Liu XM
References
- 1.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 2.Spiegel BM. The burden of IBS: looking at metrics. Curr Gastroenterol Rep. 2009;11:265–269. doi: 10.1007/s11894-009-0039-x. [DOI] [PubMed] [Google Scholar]
- 3.Keszthelyi D, Troost FJ, Masclee AA. Irritable bowel syndrome: methods, mechanisms, and pathophysiology. Methods to assess visceral hypersensitivity in irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2012;303:G141–G154. doi: 10.1152/ajpgi.00060.2012. [DOI] [PubMed] [Google Scholar]
- 4.Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119:654–660. doi: 10.1053/gast.2000.16484. [DOI] [PubMed] [Google Scholar]
- 5.Inadomi JM, Fennerty MB, Bjorkman D. Systematic review: the economic impact of irritable bowel syndrome. Aliment Pharmacol Ther. 2003;18:671–682. doi: 10.1046/j.1365-2036.2003.t01-1-01736.x. [DOI] [PubMed] [Google Scholar]
- 6.Lembo AJ, Conboy L, Kelley JM, Schnyer RS, McManus CA, Quilty MT, Kerr CE, Drossman D, Jacobson EE, Davis RB. A treatment trial of acupuncture in IBS patients. Am J Gastroenterol. 2009;104:1489–1497. doi: 10.1038/ajg.2009.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rey E, Talley NJ. Irritable bowel syndrome: novel views on the epidemiology and potential risk factors. Dig Liver Dis. 2009;41:772–780. doi: 10.1016/j.dld.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 8.Stamuli E, Bloor K, MacPherson H, Tilbrook H, Stuardi T, Brabyn S, Torgerson D. Cost-effectiveness of acupuncture for irritable bowel syndrome: findings from an economic evaluation conducted alongside a pragmatic randomised controlled trial in primary care. BMC Gastroenterol. 2012;12:149. doi: 10.1186/1471-230X-12-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camilleri M. Management of the irritable bowel syndrome. Gastroenterology. 2001;120:652–668. doi: 10.1053/gast.2001.21908. [DOI] [PubMed] [Google Scholar]
- 10.Clouse RE. Managing functional bowel disorders from the top down: lessons from a well-designed treatment trial. Gastroenterology. 2003;125:249–253. doi: 10.1016/s0016-5085(03)00808-4. [DOI] [PubMed] [Google Scholar]
- 11.Akehurst R, Kaltenthaler E. Treatment of irritable bowel syndrome: a review of randomised controlled trials. Gut. 2001;48:272–282. doi: 10.1136/gut.48.2.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quartero AO, Meineche-Schmidt V, Muris J, Rubin G, de Wit N. Bulking agents, antispasmodic and antidepressant medication for the treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2005;(2):CD003460. doi: 10.1002/14651858.CD003460.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Ouyang H, Chen JD. Review article: therapeutic roles of acupuncture in functional gastrointestinal disorders. Aliment Pharmacol Ther. 2004;20:831–841. doi: 10.1111/j.1365-2036.2004.02196.x. [DOI] [PubMed] [Google Scholar]
- 14.Linde K, Jobst K, Panton J. Acupuncture for chronic asthma. Cochrane Database Syst Rev. 2000;(2):CD000008. doi: 10.1002/14651858.CD000008. [DOI] [PubMed] [Google Scholar]
- 15.Linde K, Streng A, Jürgens S, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes MG, Weidenhammer W, et al. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. 2005;293:2118–2125. doi: 10.1001/jama.293.17.2118. [DOI] [PubMed] [Google Scholar]
- 16.Melchart D, Streng A, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes M, Hummelsberger J, Irnich D, et al. Acupuncture in patients with tension-type headache: randomised controlled trial. BMJ. 2005;331:376–382. doi: 10.1136/bmj.38512.405440.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forbes A, Jackson S, Walter C, Quraishi S, Jacyna M, Pitcher M. Acupuncture for irritable bowel syndrome: a blinded placebo-controlled trial. World J Gastroenterol. 2005;11:4040–4044. doi: 10.3748/wjg.v11.i26.4040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schneider A, Enck P, Streitberger K, Weiland C, Bagheri S, Witte S, Friederich HC, Herzog W, Zipfel S. Acupuncture treatment in irritable bowel syndrome. Gut. 2006;55:649–654. doi: 10.1136/gut.2005.074518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacPherson H, Tilbrook H, Bland JM, Bloor K, Brabyn S, Cox H, Kang’ombe AR, Man MS, Stuardi T, Torgerson D, et al. Acupuncture for irritable bowel syndrome: primary care based pragmatic randomised controlled trial. BMC Gastroenterol. 2012;12:150. doi: 10.1186/1471-230X-12-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun JH, Wu XL, Xia C, Xu LZ, Pei LX, Li H, Han GY. Clinical evaluation of Soothing Gan and invigorating Pi acupuncture treatment on diarrhea-predominant irritable bowel syndrome. Chin J Integr Med. 2011;17:780–785. doi: 10.1007/s11655-011-0875-z. [DOI] [PubMed] [Google Scholar]
- 21.Anastasi JK, McMahon DJ, Kim GH. Symptom management for irritable bowel syndrome: a pilot randomized controlled trial of acupuncture/moxibustion. Gastroenterol Nurs. 2009;32:243–255. doi: 10.1097/SGA.0b013e3181b2c920. [DOI] [PubMed] [Google Scholar]
- 22.Lowe C, Depew W, Vanner S. A placebo-controlled, double-blind trial of acupuncture in the treatment of irritable bowel syndrome (IBS) Gastroenterology. 2000;118:A3168. [Google Scholar]
- 23.Brandt LJ, Chey WD, Foxx-Orenstein AE, Schiller LR, Schoenfeld PS, Spiegel BM, Talley NJ, Quigley EM. An evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol. 2009;104 Suppl 1:S1–35. doi: 10.1038/ajg.2008.122. [DOI] [PubMed] [Google Scholar]
- 24.Drossman DA, Dumitrascu DL. Rome III: New standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15:237–241. [PubMed] [Google Scholar]
- 25.Hulisz D. The burden of illness of irritable bowel syndrome: current challenges and hope for the future. J Manag Care Pharm. 2004;10:299–309. doi: 10.18553/jmcp.2004.10.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mathew P, Bhatia SJ. Pathogenesis and management of irritable bowel syndrome. Trop Gastroenterol. 2009;30:19–25. [PubMed] [Google Scholar]
- 27.Cash BD, Chey WD. Diagnosis of irritable bowel syndrome. Gastroenterol Clin North Am. 2005;34:205–220, vi. doi: 10.1016/j.gtc.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 28.Rahimi R, Abdollahi M. Herbal medicines for the management of irritable bowel syndrome: a comprehensive review. World J Gastroenterol. 2012;18:589–600. doi: 10.3748/wjg.v18.i7.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fireman Z, Segal A, Kopelman Y, Sternberg A, Carasso R. Acupuncture treatment for irritable bowel syndrome. A double-blind controlled study. Digestion. 2001;64:100–103. doi: 10.1159/000048847. [DOI] [PubMed] [Google Scholar]
- 30.Sung JJ. Acupuncture for gastrointestinal disorders: myth or magic. Gut. 2002;51:617–619. doi: 10.1136/gut.51.5.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lim B, Manheimer E, Lao L, Ziea E, Wisniewski J, Liu J, Berman B. Acupuncture for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2006;(4):CD005111. doi: 10.1002/14651858.CD005111.pub2. [DOI] [PubMed] [Google Scholar]
- 32.Schneider A, Streitberger K, Joos S. Acupuncture treatment in gastrointestinal diseases: a systematic review. World J Gastroenterol. 2007;13:3417–3424. doi: 10.3748/wjg.v13.i25.3417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Manheimer E, Wieland LS, Cheng K, Li SM, Shen X, Berman BM, Lao L. Acupuncture for irritable bowel syndrome: systematic review and meta-analysis. Am J Gastroenterol. 2012;107:835–847; quiz 848. doi: 10.1038/ajg.2012.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xiao WB, Liu YL. Rectal hypersensitivity reduced by acupoint TENS in patients with diarrhea-predominant irritable bowel syndrome: a pilot study. Dig Dis Sci. 2004;49:312–319. doi: 10.1023/b:ddas.0000017458.55517.33. [DOI] [PubMed] [Google Scholar]
- 35.Cui KM, Li WM, Gao X, Chung K, Chung JM, Wu GC. Electro-acupuncture relieves chronic visceral hyperalgesia in rats. Neurosci Lett. 2005;376:20–23. doi: 10.1016/j.neulet.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 36.Tillisch K. Complementary and alternative medicine for functional gastrointestinal disorders. Gut. 2006;55:593–596. doi: 10.1136/gut.2005.078089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chu WC, Wu JC, Yew DT, Zhang L, Shi L, Yeung DK, Wang D, Tong RK, Chan Y, Lao L, et al. Does acupuncture therapy alter activation of neural pathway for pain perception in irritable bowel syndrome?: a comparative study of true and sham acupuncture using functional magnetic resonance imaging. J Neurogastroenterol Motil. 2012;18:305–316. doi: 10.5056/jnm.2012.18.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schneider A, Weiland C, Enck P, Joos S, Streitberger K, Maser-Gluth C, Zipfel S, Bagheri S, Herzog W, Friederich HC. Neuroendocrinological effects of acupuncture treatment in patients with irritable bowel syndrome. Complement Ther Med. 2007;15:255–263. doi: 10.1016/j.ctim.2006.12.002. [DOI] [PubMed] [Google Scholar]


