Abstract
Background:
We report the functional impact and natural history of cutaneous hypoesthesia after plate internal fixation for mid shaft clavicle fractures with a horizontal skin incision from year 2009 to 2011.
Materials and Methods:
38 patients had complete followup data with an average followup period of 23.2 months (range 8-43 months). The impact of supraclavicular nerve injury was studied by assessment of the incidence, functional impact and natural history of numbness with detailed review of the case records and phone questionnaires.
Results:
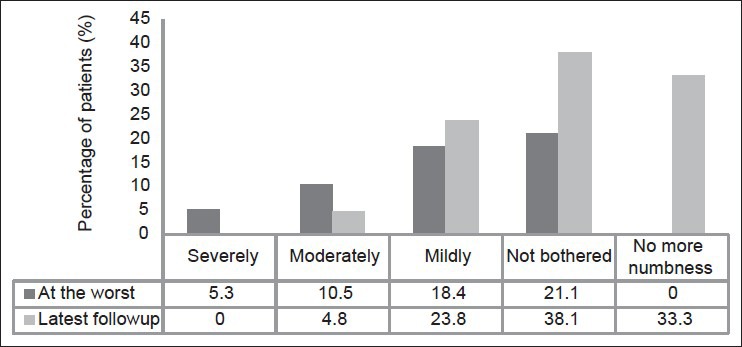
The incidence of postoperative numbness was 55.3% (n = 21). Most patients reported the numbness to be at its worst within the first operative month. At the time of worst numbness, 28.6% (n = 6/21) of patients reported the numbness to be severe while 42.9% (n = 9/21) reported moderate numbness and 28.6% (n = 6/21) reported mild numbness. Fifteen of these patients described increased awareness of numbness during contact with straps or clothes. Two patients were significantly bothered by this numbness; 4 patients stated that it was a moderate bother while 7 patients considered it a mild bother. A total of 8 patients reported that they were not bothered at all by the numbness. An overwhelming majority of affected patients (90.5%, n = 19/21) reported an improvement in the severity of numbness felt over time. At the last followup, the incidence of numbness declined from 55.3% to 36.8% with 7 patients reporting complete resolution of numbness. The numbness however was found to persist in 66.7% of patients. Only 1 patient reported continued severe numbness. The awareness of numbness with straps and clothing was severe in 5 patients. None of the patients were significantly bothered by this numbness.
Conclusions:
Cutaneous sensory loss is a common occurrence following plate fixation of the clavicle and might have been under reported in the literature. The numbness improves in the vast majority, but commonly persists to some degree for up to 2 years and maybe permanent. However, only a small minority eventually considered the numbness a significant “bother” and to affect them while wearing clothing or when in contact with shoulder straps.
Keywords: Clavicle fracture, surgical fixation, cutaneous hypoesthesia, numbness, supraclavicular nerve
INTRODUCTION
Clavicle fractures are common injuries. Plate fixation is a widely performed procedure for significantly displaced fractures.1 Fortunately, major neurological complications after such surgery are rare. Minor neurological deficits; however such as, infraclavicular hypoesthesia secondary to supraclavicular nerve injury is a common complication with reported incidence of 10-29%.1,2 With the expanding surgical indications of clavicle fractures, we expect an increasing number of patients with this complication.1
The supraclavicular nerve is a sensory cutaneous nerve and originates from the C3 and C4 nerve roots of the superficial cervical plexus. Its area of sensory innervation includes the anteromedial shoulder and proximal chest wall inferior to the clavicle. The supraclavicular nerve commonly divides into a medial and lateral branch and in some cases; there may be an additional intermediate branch.3 The medial branch appears to cross at the medial third of the clavicle while the lateral branch tends to cross at the lateral third of the clavicle. The intermediate branch, if present, tends to shows a more variable branching pattern.
Post total knee arthroplasty patients have voiced concerns over persistent numbness and a small proportion of patients consider this numbness to be a significant complication of the procedure.4,5 While there have been several studies documenting this clinical significance in total knee arthroplasties as well as hip arthroplasties,6 there is a little information in the current literature regarding the impact and in particular, the natural history of regional hypoesthesia post plate fixation of clavicle fractures.
In this study, we investigate the incidence of supraclavicular nerve injury post plate fixation of clavicle fractures, its clinical impact on patients’ satisfaction, functional handicap in activities of daily living as well as the natural evolutionary history of the numbness over an average followup period of 23.2 months.
MATERIALS AND METHODS
38 patients who were available for followup and underwent plate internal fixation for displaced midshaft clavicle fractures between January 2009 and December 2011 and were included in the study. All patients underwent surgery by a standard horizontal skin incision. This study was approved by the relevant Ethics Committee Board.
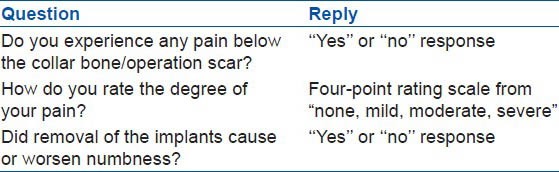
All patients completed the phone questionnaire. The impact of supraclavicular nerve injury was assessed with detailed review of the case records and phone questionnaires at various time points. Specifically, we detailed the presence and functional impact of any numbness at the date of followup with the questions in Table 1. The natural history of this numbness, if present was assessed with the questions in Table 2. Finally, pain below the operative scar and the role of implant removal in the causation of numbness were addressed with the questions in Table 3.
Table 1.
Questionnaire detailing the presence and functional impact of numbness after clavicle surgery, if present, at the date of followup
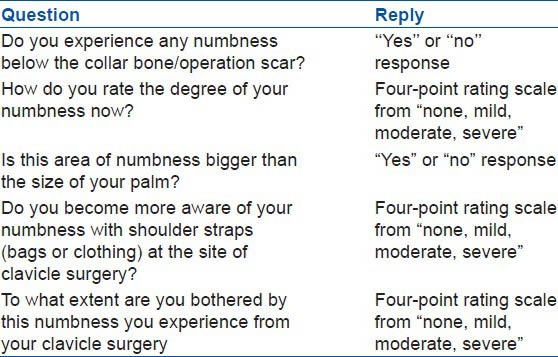
Table 2.
Questionnaire detailing the natural history of numbness after clavicle surgery, if present
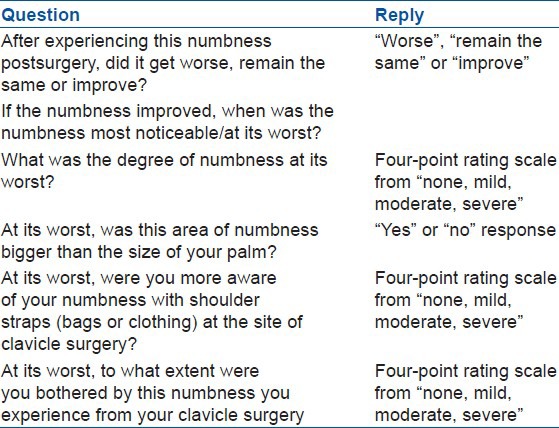
Table 3.
Questionnaire detailing presence of pain after clavicle surgery and the presence of numbness after surgery for implant removal
RESULTS
There were 33 male and 5 female patients. The mean age of the patients was 35.2 years (range 16-68 years, SD 13.9). The average followup time elapsed since the operation was 23.2 months (range 8-43 months, SD 9.5)
The incidence of postoperative numbness was 55.3% with 21 out of 38 patients reporting the development of postoperative numbness. An overwhelming majority of affected patients, 19 out of 21 patients (90.5%), reported an improvement in the numbness severity over time. Only two patients reported constant numbness up to the last followup conducted and none of the patients reported any increased numbness with time. Of the 19 patients who reported an improvement in numbness, 18 reported the numbness to be at its worst within the first operative month and 1 patient reported the numbness to be worst at the 3rd operative month.
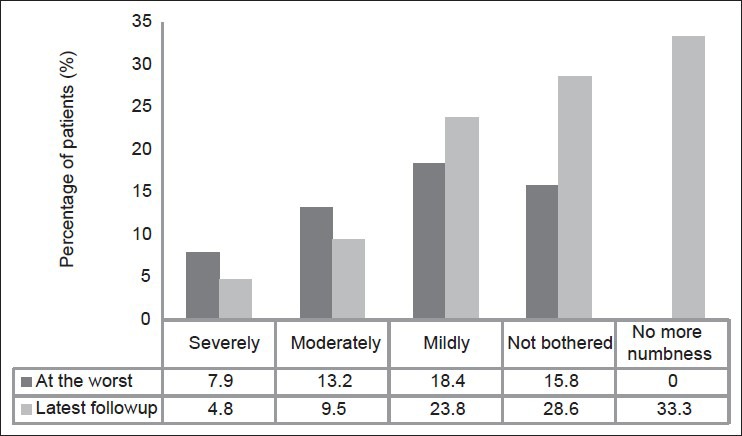
At the time of worst numbness, 28.6% (6/21) of patients reported the numbness to be severe while 42.9% (9/21) reported moderate numbness and 28.6% (6/21) reported mild numbness. At this time point, 52.4% (11/21) of patients had numbness with the size greater than their palm size [Figure 1]. Fifteen of 21 patients (71.4%) described increased awareness of numbness during contact with straps or clothes. The degree of awareness of shoulder straps (bags and clothing) on contact with the surgical site was mild, moderate and severe in 7 patients (33.3%), 5 patients (23.8%) and 3 patients (14.3%) out of 21 patients respectively. Two patients (9.5%) were significantly bothered by this numbness, 4 (19.0%) patients stated that they were moderately bothered while 7 patients (33.3%) considered it a mild bother. A total of 8 patients (38.1%) were not bothered at all by the numbness.
Figure 1.
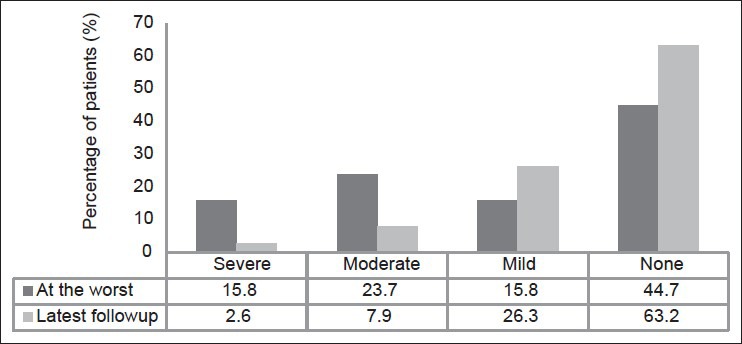
Bar diagram showing natural history of patients’ degree of numbness at the worst against that on the latest followup after plate fixation for clavicle midshaft fractures
At an average of 23.2 months, the incidence of numbness declined from 55.3% (21/38) to 36.8% (14/38) with 7 patients out of 21 reporting resolution of numbness [Figure 2]. The numbness however was found to persist to some degree in 66.7% of patients. Only 7.1% (1/14) of patients reported the numbness to be severe while 21.4% (3/14) reported moderate numbness and 71.4% (10/14) experienced mild numbness. At this time point, 21.4% (3/14) of patients had numbness with the size greater than their palm size. Slightly more than half of patients, (57.1%, 8/14 patients) described increased awareness of numbness during contact with shoulder straps (bags and clothing). The severity of numbness awareness with straps and clothing was mild, moderate and severe in 5 (35.7%), 2 (14.3%) and 1 (7.1%) out of 14 patients respectively [Figure 3]. In terms of “bothersomeness,” none of the patients were significantly affected by this numbness. One (7.1%) patient stated being moderately bothered while 5 patients (35.7%) considered it a mild bother. A total of 8 patients (57.15) reported no bother at all by the numbness [Figure 4].
Figure 2.
Bar diagram showing natural history of patients’ degree of bother by the numbness at the worst against that on the latest followup after plate fixation for clavicle midshaft fractures
Figure 3.
Bar diagram showing natural history of patient's degree of awareness with overlying straps (bags and clothing) at the worst against that on the latest followup after plate fixation for clavicle midshaft fractures
Figure 4.
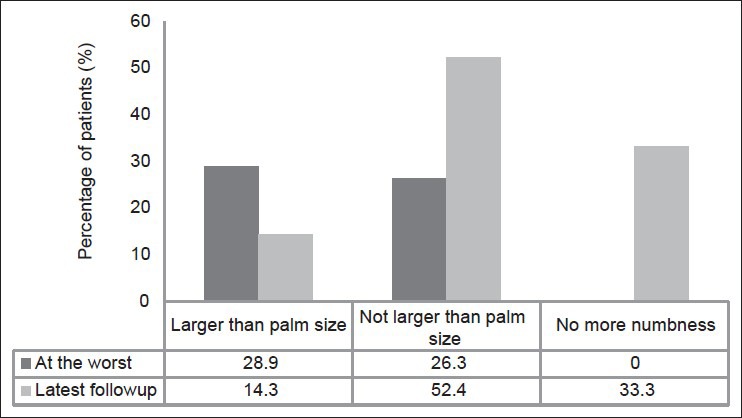
Bar diagram showing natural history of patients’ area of numbness at the worst against that on the latest followup after plate fixation for clavicle midshaft fractures
Only 1 patient (2.6%) reported pain after the surgery, this patient reported moderate pain up to the last followup. Removal of implants was undertaken in 7 out of 38 patients. Two patients felt that removal of the implants worsened the numbness while 5 patients were unaffected in terms of numbness.
DISCUSSION
In current literature, there is to our knowledge only one study that has addressed the impact of clavicle hypoesthesia after plate fixation.3 The authors compared the impact of using vertical versus horizontal incisions and found that vertical incisions for plate fixation of clavicle shaft fractures may be associated with reduced postoperative numbness. The authors felt that vertical incisions may avoid some cases of patient dissatisfaction and recommended that surgeons should consider using this approach in plate fixation of clavicle fractures.
We present new data in the literature and highlight the following points. Firstly, we found incidence of numbness (55.3%) post clavicle plate fixation higher that what was commonly reported in the literature (12-29%).1,2 This is in concordance with the findings recently published by Wang et al.,7 where the authors found overall incidence of 46%. Our findings suggest that this complication may have been under emphasized and unreported in earlier literature. Secondly, the natural history of clavicle hypoesthesia is at its worst almost always declaring itself within the 1st month after the surgery. This is not surprising as postoperatively; patients usually report resolution of pain after fracture stabilization and start to notice the effects of postoperative numbness. Thirdly, at this time point of worst symptomatology (usually at 1 month), this complication is clinically significant. A significant proportion of patients consider the numbness severe (28.6%) with a heightened awareness of numbness with straps and clothing (71.4%). This was a moderate to severe bother in their lives in 28.6% of patients. Moreover, various degrees of numbness persisted in 66.7% of patients at average followup of close to 2 years. Longer term followup studies are required to determine if the numbness dissipates completely over time.
Fortunately, an overwhelming majority of affected patients, 19 out of 21 patients (90.5%), report a subjective diminution in this numbness over time. At the last followup, only 1 patient still had severe numbness while 89.5% (34/38) patients had no or mild numbness. Likewise, the heightened awareness with clothing and straps over the area of numbness was considerably less. Only 1 patient still had severe awareness while 92.1% of patients (35/38) had mild or no awareness.
Patients should be prewarned of cutaneous hypoesthesia before undergoing surgery and counseled that this complication is common and can be persistent. They may feel this numbness to affect their activities of daily living in the initial postoperative period, the discomfort of which seems to peak at 1 month postoperatively. However, they should also be reassured that the vast majority of patients afflicted with numbness encounter marked diminution of the problem functionally at an average of 2 years after the operation and are generally no longer bothered by this issue.
The limitations of this study include the relatively small number of patients treated operatively and the retrospective methodology. Furthermore, outcomes are measured according to the patient's subjective symptomatology and there is a lack of objective quantification of cutaneous hypoesthesia. Objective measures of numbness require a trained neurophysiologist with specialized instruments and tools.
Be that as it may, numbness is more often a subjective complaint than a symptom quantifiable by objective measurement. Hence, we think that the study of self-reported measures is valuable in assessing the functional impact of numbness on the individual. We also believe this study to be the first specific functional assessment of the natural history of clavicle numbness post plate fixation of clavicle shaft fractures. We had complete followup data in all 38 patients, which validates our findings. Future prospective studies addressing risk factors for this complication are required in light of the results of this study where we report a higher than expected incidence of cutaneous sensory loss and one, which seems to persist for up to 2 years.
To conclude, cutaneous sensory loss is a common occurrence following plate fixation of the clavicle and might have been under reported in the literature. The numbness improves in the vast majority, but commonly persists to some degree up to 2 years after the operation and maybe permanent.
All patients should be prewarned about persistent cutaneous numbness before clavicle surgery, but reassured that it almost always improves.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 2.Shen WJ, Liu TJ, Shen YS. Plate fixation of fresh displaced midshaft clavicle fractures. Injury. 1999;30:497–500. doi: 10.1016/s0020-1383(99)00140-0. [DOI] [PubMed] [Google Scholar]
- 3.Nathe T, Tseng S, Yoo B. The anatomy of the supraclavicular nerve during surgical approach to the clavicular shaft. Clin Orthop Relat Res. 2011;469:890–4. doi: 10.1007/s11999-010-1608-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borley NR, Edwards D, Villar RN. Lateral skin flap numbness after total knee arthroplasty. J Arthroplasty. 1995;10:13–4. doi: 10.1016/s0883-5403(05)80095-6. [DOI] [PubMed] [Google Scholar]
- 5.Hopton BP, Tommichan MC, Howell FR. Reducing lateral skin flap numbness after total knee arthroplasty. Knee. 2004;11:289–91. doi: 10.1016/j.knee.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Chatterji U, Fontana A, Villar RN. Posterior skin flap numbness after total hip arthroplasty. J Arthroplasty. 1996;11:853–5. doi: 10.1016/s0883-5403(96)80186-0. [DOI] [PubMed] [Google Scholar]
- 7.Wang K, Dowrick A, Choi J, Rahim R, Edwards E. Postoperative numbness and patient satisfaction following plate fixation of clavicular fractures. Injury. 2010;41:1002–5. doi: 10.1016/j.injury.2010.02.028. [DOI] [PubMed] [Google Scholar]


