Abstract
Background:
Schatzker type V and VI tibial fractures are complex injuries, usually treated with open reduction and internal fixation (ORIF) using dual plates or ring fixators. ORIF has the advantage of not requiring pin tract care, but has a higher infection rate, especially in open fractures. We have combined the advantages of these two methods to treat these difficult fractures.
Materials and Methods:
Ten Schatzker type V and 11 Schatzker type VI fractures were treated between 2006 and 2010. ORIF with dual plates was performed, only if there was marked articular displacement (> 2 mm) in a closed fracture. All other fractures including open fractures and closed fractures with soft tissue compromise or minimal articular displacement were treated with ring fixators. The outcomes were analyzed and documented using the Honkonen and Jarvinen subjective, clinical, functional, and radiological criteria and the Western Ontario and McMaster Universities Arthritis Index (WOMAC).
Results:
Nine closed fractures with marked articular displacement (> 2 mm) were treated with dual plates. Eight closed fractures with minimal articular displacement (< 2 mm) and poor skin condition and four open fractures were treated with ring fixators. The mean follow-up period was 2 ½ years. The mean postoperative knee flexion was 128°. All patients could walk, jump, and climb steps. 90% could squat, though only 50% could duck walk properly. Radiologically, 85% had a plateau tilt of less than 5°, 92% had an articular step of less than 2 mm, and a residual articular widening of less than 5 mm. There were no major infections. Two patients had minor pin tract infections and two requested that their plates be removed subsequently.
Conclusion:
The protocol used to treat Schatzker type V and VI tibial plateau fractures has had excellent results and we suggest that all open fractures be treated with ring fixators and that ORIF should be done only for closed fractures with marked displacement.
Keywords: Tibial plateau fractures, dual plates, ring fixators
INTRODUCTION
The optimal treatment of Schatzker type V and VI tibial plateau fractures is a controversial and challenging. There is no specific and proven treatment protocol yet. Most patients have significant residual dysfunction even after the completion of treatment.1 Though open reduction and internal fixation (ORIF) of these fractures provides good fracture reduction and stability, several authors have reported high rates of complications–deep wound infection, unplanned secondary procedures, and even amputation.1,2,3,4 Lasanianos et al.5 in their biomechanical study comparing intramedullary nailing and compression bolt fixation with single lateral locking plate fixation and dual plating technique in the osteosynthesis of Schatzker type VI fractures showed that the collapse of the medial tibial plateau occurred exclusively in the single lateral locking plate fixation group.5 Though superior to single lateral plate fixation, the dual plating technique is more damaging to the already compromised soft tissues in these high energy injuries and the wound infection rate with dual plating is as high as 20%.1 These problems prompted the development of Ilizarov ring fixation with or without minimal internal fixation as an alternative method for bicondylar fracture treatment. While the Ilizarov fixator seems a reasonable method of fixation of these fractures, there are few problems, including the inconvenience of an external fixator that requires careful maintenance, possibility of pin tract infections and subsequent collapse of the fracture fragments.4 However, it is useful in the treatment of open Schatzker type V and VI tibial plateau fractures, where the incidence of infection has been shown to be relatively high with plating. It may also allow early weight bearing with its attendant benefits.
We managed our cases of Schatzker type V and type VI fractures with such a protocol, which combines the benefits of both systems [Figure 1]. We do not intend to compare the results of dual plating Vs Ilizarov fixation, as both have been used under different circumstances in our study. We analyzed the outcomes of using our protocol in this study.
Figure 1.
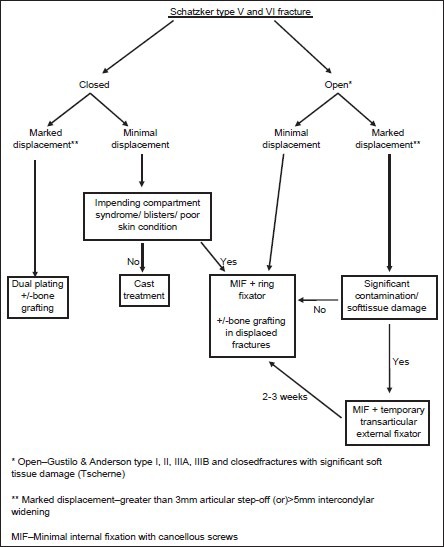
Management protocol for bicondylar tibial plateau fractures
MATERIALS AND METHODS
All patients with Schatzker type V and VI tibial plateau fractures admitted in our institute between 2006 and 2010 were recruited. They were excluded if they had ipsilateral fractures of the femur, any other lower limb fractures, open type 3 C tibial fractures, or severe head injury with permanent neurological deficits. They were evaluated clinically and standard antero-posterior (AP) and lateral radiographs were taken. Computerized tomography (CT) scans were done only in selected patients, who had significant articular depression and comminution on x-rays.
Patients were treated with dual plating or the Ilizarov fixator, based on the above mentioned protocol [Figure 1].
In a closed fracture with minimal articular displacement (< 2 mm), with blisters or if soft tissue injury is significant, such as to preclude cast treatment, even at 1 week of injury, closed reduction and minimal internal fixation with cancellous screws, along with application of the circular frame is done with the leg on a fracture table
In closed fractures with articular displacement > 2 mm, we prefer ORIF with dual plates using two incisions, as reduction of markedly displaced fractures and maintenance of the reduction is better with plates. We use the posteromedial approach as described by Barei et al.,6 along with the standard anterolateral approach. We initially used small fragment reconstruction plates on the medial side, but now prefer locked reconstruction plates. Proximal tibial locking plates are used on the lateral side
Due to the possibility of infection in open fractures, dual plating is not done, even if there is marked displacement. At the time of the initial debridement, articular reduction is obtained and maintained with K wires and screws and a ring fixator is applied. If soft tissue cover is required or if there is significant soft tissue damage to warrant secondary soft tissue procedures, a trans-articular external fixator is applied, as it is difficult to do a flap cover with the ring fixator in situ. Once the soft tissues heal, this is converted to an Ilizarov fixator (usually at 3 weeks)
In open fractures with marked displacement thatrequire bone grafting/substitutes, it is done primarily along with minimal internal fixation and ring fixator application, only if the wound contamination and soft tissue damage are minimal and if surgery is done early, usually within 12 hours of the injury. Else, it is done as a staged procedure
The ring fixator is usually a three ring construct that consists of a proximal ring with two wires, just above the level of the fibular head; with an additional drop-wire if needed, in the proximal fragment. The second ring is placed at the level of the distal shaft fragment, 1 inch below the fracture line. A third ring is placed distally, near the ankle. For severely comminuted and displaced plateau fractures, an additional distal femoral ring with three wires is used for additional stability. This is removed after 4-6 weeks.
Postoperatively, patients were encouraged to start early knee range of movement exercises and quadriceps strengthening exercises. Knee ROM was allowed only after distal femoral ring removal (usually at 6 weeks), in cases where it was used. Partial weight bearing with crutches was allowed in patients with the ring fixator and non-weight bearing crutch walking for patients with dual plating, started after drain removal. The patients were followed up regularly till fracture union. The final outcome measures were assessed at a minimum of 1 year from the date of surgery.
The outcome measures were assessed using the Honkonen and Jarvinen (HJ) Criteria7 – subjective, radiological, clinical, and functional outcome measures and the WOMAC8 - Western Ontario and McMaster Universities Arthritis Index.
RESULTS
Twenty one patients were assessed with a minimum follow up of 1 year. There were 20 males and 1 female in the study group. The mean age of the group was 43.85 years (range 22-61 years). Eleven were Schatzker type V fractures and 10 were Schatzker type VI. Three patients had associated anterior cruciate ligament (ACL) tibial bony avulsion and one patient had patellar tendon avulsion from the tibial tuberosity.
Four patients with type 3A open fractures and eight patients with closed fractures and poor skin condition/minimal articular displacement (n=12) underwent minimal internal fixation and Ilizarov ring fixation, while nine patients underwent dual plating. One of the patients with Ilizarov fixation had fixation of ACL tibial avulsion and another had fixation of the patellar tendon with cancellous screws. Distal femoral ring was used in addition to the three-ring construct in these two patients, and was removed at 6 weeks. The mean duration between the injury and the primary surgery was 5.11 days (range 12 hours-21 days). The mean time of follow up for the outcome assessment from primary surgery was 29 months (range 13-47 months).
All patients were walking without aids at an average period of 5.86 months from surgery (range 4-7 months). Patients with Ilizarov rings walked without any aid at an average of 5.6 months, while the patients who underwent dual plating did so at 6 months.
The average time to return to their job after the injury was 6.66 months (range 3-18 months). Thirteen patients returned to their original job within 6 months from injury, once they were able to walk unassisted. One patient had to change his job due to decreased range of movement of the injured knee.
WOMAC-score
The WOMAC score is primarily used to assess pain, stiffness and physical function in patients with osteoarthritis of the knee and hip. We used the WOMAC score in our study to look for early secondary knee osteoarthritis after tibial plateau fractures. The average WOMAC score in our study was 7.23, which is a good outcome on the scale between 0 [best] and 96 [worst]. Three patients had a WOMAC score of 0. 14 patients had a score of 1-11 and 4 had a score of 12-22. None scored more than 22.
HJ subjective score
The symptoms analyzed include pain during activities, swelling, stiffness, weakness, limping, giving way, and crepitation. The worst grade in the seven symptoms was considered as the final outcome. A score of 1 to 5 was excellent; 6 to 10 good; 11 to 15 fair; and 16 to 25 poor. The subjective score in the study group was excellent for 76.2% of the patients. Sixteen patients were totally pain free during activities and five had mild pain. Of the five, one had a minimally displaced open fracture, one had a markedly displaced closed fracture, and the remaining three were minimally displaced closed fractures. All patients were free of swelling around the knee at follow up. Only two patients had mild stiffness around the knee. Twenty patients did not feel any weakness at the knee. One patient had mild weakness. 20 patients had excellent score for walking without limp. One patient felt occasional giving way at the operated knee, which was of slight importance to him. Twenty patients had an excellent score for crepitation around the knee. Only one patient gave importance to crepitation symptom at the knee.
HJ clinical outcome
The final clinical outcome score was good in 13 patients, fair in 7 patients, and poor in 1 patient. The clinical outcome score has 4 components: Extension lag, range of movement, thigh atrophy and stability at the knee. The worst score among the four was considered as the final outcome score.
None of the patients at follow up had an extension lag. The average knee flexion was 128.09° [Figures 2a, 2b, 3a and 3b]. The range of movement varied from 90° to 145°. There were three patients with a flexion range of less than 110°. Two had markedly displaced closed fractures and one had a minimally displaced open fracture treated with a ring fixator. The average thigh atrophy in the operated side was 1.5 cm (range 1-4 cm) as compared to the contralateral normal thigh. The stability at the knee was excellent in 18 patients. Though three patients had mild anteromedial instability on clinical assessment, only one patient had a sense of occasional giving way at the knee on walking.
Figure 2A.

(a) X-ray of knee joint (anteroposterior and lateral views) showing tibial plateau fracture (b) Anteroposterior radiograph of knee joint showing ilizarov fixator in situ (c) Anteroposterior and lateral radiographs of knee joint of same patient showing followup radiograph after ilizarov removal.
Figure 2B.

Clinical photograph of same patient showing range of motion. Good knee flexion in a patient treated with a circular fixator
Figure 3A.

X-ray anteroposterior and lateral views showing (a) tibial plateau fracture (b) dual plating for tibial plateau fracture
Figure 3B.

Clinical photograph of same patient showing range of motion
HJ functional outcome
19 patients had excellent walking and 2 had good walking function (walking with slight limp). 19 patients had excellent stair climbing function and 2 had mild pain while climbing stairs. Six patients had excellent squatting function and 12 had mild pain while squatting. Three patients were unable to squat well. Two of them had markedly displaced closed fractures and one had minimally displaced closed fracture. The poor squatting function in the 3 patients was due to poor knee range of movement and not due to pain. 12 patients had excellent jumping function. Excellent jumping meant that they were able to jump a distance similar to the uninjured leg, without pain. Nine patients could jump only 50-90% of the opposite normal side. Only three patients were able to do normal duck walking. Six patients were able to duck walk a few steps. Two patients were able to duck walk one step. Ten patients were not able to duck walk.
HJ radiological outcome
Most patients had a “good” radiological score, with only two having a “fair” score. The criteria were extremely stringent. Differences of even 1 degree of plateau tilt from the opposite knee or 1 mm of articular step would classify the result as good and not excellent. A difference of more than 5 degree plateau tilt or a 3 mm articular step was a “fair” result. There were four components in the radiological score and the worst of them was shown as the final radiological score. Figures 4 and 5 show the radiographs of patients treated with the ring fixator and dual plates respectively with good radiological outcome.
Figure 4.
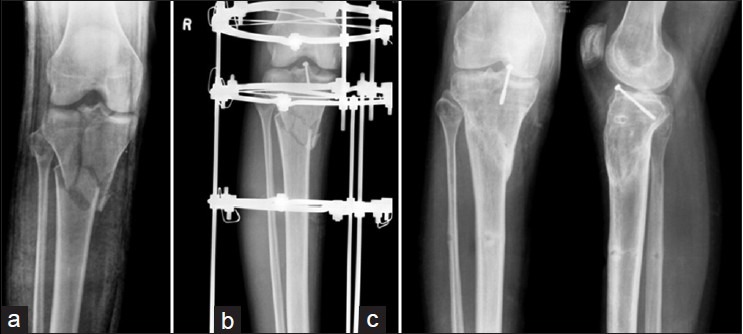
(a) X-ray anteroposterior view of knee joint showing tibial plateau fracture (b) x-ray anteroposterior view treated with minimal internal fixation and a ring fixator (c) X-ray anteroposterior and lateral views showing negligible plateau tilt and articular step
Figure 5.

Anteroposterior and lateral radiographs of a patient showing (a) tibial plateau fracture (b) dual plates/bone grafting and good radiological outcome.
Plateau tilt
Seventeen patients had plateau tilt within 5 degrees from the opposite side and had scored good. Three patients had scored fair (mean tilt-7 degrees) and only one patient had scored poor with a tilt of 11 degrees. This patient had a markedly displaced closed fracture with a preop articular step of 10.54 mm and preoperative intercondylar widening of 13.34 mm. The fracture was fixed using dual plates and postoperatively, there was no intercondylar widening or an articular step; but at years follow-up, there was 11 degrees varus tilt. This was because the posteromedial buttress plate did not provide adequate stability.
Articular step
Seventeen patients did not have any articular step at final follow up based on radiographs. The average pre-operative articular step was 5.34 mm (range 0-10.54 mm). The average articular step postoperatively was 0.42 mm (range 0-2.74 mm). Of the four patients with a mild articular step postoperatively (1-3 mm), three had been treated with the Ilizarov fixator and one with dual plating.
Condylar widening
The average postoperative condylar widening was 3.17 mm (range 0-10 mm). The average preoperative condylar widening was 6.19 mm (range 5-16.97 mm). Six patients did not have any postoperative condylar widening. Fourteen patients scored good (within 5 mm) and one patient scored poor with condylar widening of 10 mm. This patient had a closed fracture treated with minimal internal fixation and Ilizarov ring and had fair final functional score.
Joint space
Four patients did not have any decrease in joint space as compared to the uninjured knee in anteroposterior radiographs. In the remaining 17 patients, the joint space decrease was less than 50%. The mean decrease in joint space was 10.23% at final followup.
Infection Rate
Two patients treated with minimal internal fixation and Ilizarov ring fixation had pin site infection, which did not require wire exchange. One of these patients had an open fracture and the other had a closed, minimally displaced fracture. None of the patients treated with dual plating had wound infections.
DISCUSSION
The optimal treatment of Schatzker type V and VI tibial plateau fractures has remained challenging and controversial, despite the development of various new techniques of fracture reduction, implants for fracture fixation and better techniques of soft tissue handling. The earlier reports of internal fixation with plates by Young and Barrack,2 Moore et al.,3 and Mallik et al.4 had unacceptably high rates of deep wound infection. Uhl et al.9 reported postoperative skin infection and osteomyelitis in 42% and 33% of patients treated with dual plates. The recent randomized controlled trial by the Canadian Orthopedic Trauma Society reported 20% deep wound infection in the patient group treated with open reduction and dual plating.1 They also reported high rates of unplanned secondary procedures which included incision and drainage, soft tissue flaps, redo ORIF, plate removal, knee manipulation, total knee replacement and even above knee amputation.
This prompted several authors to use the ring fixator with or without minimal internal fixation as an alternative method for tibial bicondylar fracture fixation. Kataria et al.10 evaluated 38 high-energy tibial plateau fractures (16 Schatzker type V and 22 type VI fractures) treated with ring fixators. They showed promising results with only two superficial infections and three minor pin site infections. The average knee flexion was 132°. The Canadian Orthopedic Trauma Society study group also had excellent results with the use of ring fixators.
We treated these complex injuries in a more systematic way, utilizing the benefits of both the treatment methods available. The subjective score as scored by the patients themselves regarding various symptoms was excellent in most of the patients. The average postoperative knee flexion in our study was 128.09°, which is better than results in recent literature. The average knee range of movement in the randomized controlled trial by the Canadian Orthopedic Trauma Society was 109° in the dual plating group and 120° in the circular external fixator group.1
In our study, no patient had significant deep infection, requiring implant removal prior to bony union. There were no unplanned secondary procedures prior to bony union. The average wound infection rate in the literature is around 20% in the dual plating group,1 requiring significant number of unplanned secondary procedures. Also, ORIF with dual plates is associated with many complications, especially with open tibial plateau fractures.11 By not performing ORIF in open cases and closed fractures with compromised skin, we have managed to reduce complication rates to a minimum in these complex fractures. All patients except one were able to return to their job at an average of 6.66 months. In other studies, patients with bicondylar tibial fractures have significant residual dysfunction even after completion of treatment.1,12 The Canadian Orthopedic Trauma Society's study showed that only few patients were able to return to their normal pre-injury activities.
To conclude, Schatzker type V and VI tibial plateau fractures when treated using our protocol had good clinical, functional, and radiological outcomes, with low infection rates. However, prospective studies involving larger number of patients are required to establish a protocol for this type of injuries.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Mckee MD, Pirani SP, Stephen DJ. The Canadian Orthopedic Trauma Society, Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Results of a multicenter, prospective, randomized clinical trial. J Bone Joint Surg Am. 2006;88:2613–23. doi: 10.2106/JBJS.E.01416. [DOI] [PubMed] [Google Scholar]
- 2.Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthop Rev. 1994;23:149–54. [PubMed] [Google Scholar]
- 3.Moore TM, Patzakis MJ, Harvey JP. Tibial plateau fractures: Definition, demographics, treatment rationale and long-term results of closed traction management or operative reduction. J Orthop Trauma. 1987;1:97–119. [PubMed] [Google Scholar]
- 4.Mallik AR, Covall DJ, Whitelaw GP. Internal versus external fixation of bicondylar tibial plateau fractures. Orthop Rev. 1992;21:1433–6. [PubMed] [Google Scholar]
- 5.Lasanianos NG, Garnavos C, Magnisalis E, Kourkoulis S, Babis GC. A comparative biomechanical study for complex tibial plateau fractures: Nailing and compression bolts versus modern and traditional plating. Injury. 2013;44:1333–9. doi: 10.1016/j.injury.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 6.Barei DP, Nork SE, Mills WJ, Henley B, Benirschke SK. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two incision technique. J Orthop Trauma. 2004;18:649–57. doi: 10.1097/00005131-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Honkonen SE, Jarvinen MJ. Classification of fractures of the tibial condyles. J Bone Joint Surg Br. 1992;74:840–7. doi: 10.1302/0301-620X.74B6.1447244. [DOI] [PubMed] [Google Scholar]
- 8.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 9.Uhl RL, Goldstock L, Carter AT, Lozman J. New Orleans, Louisiana: Presented at the 61st AAOS meeting; 1994. Hybrid external fixation for bicondylar tibial plateau fractures. [Google Scholar]
- 10.Kataria H, Sharma N, Kanojia RK. Small wire external fixation for high-energy tibial plateau fractures. J Orthop Surg (Hong Kong) 2007;15:137–43. doi: 10.1177/230949900701500202. [DOI] [PubMed] [Google Scholar]
- 11.Subasi M, Kapukaya A, Arslan H, Ozkul E, Cebesoy O. Outcome of open comminuted tibial plateau fractures treated using an external fixator. J Orthop Sci. 2007;12:347–53. doi: 10.1007/s00776-007-1149-7. [DOI] [PubMed] [Google Scholar]
- 12.Buckle R, Blake R, Watson JT, Morandi M, Browner BD. Treatment of the complex tibial plateau fractures with the Ilizarov external fixator. J Orthop Trauma. 1993;7:167–8. [Google Scholar]


