Abstract
Background:
Percutaneous aspiration of abscesses under ultrasonography (USG) and computer tomography (CT) scan has been well described. With recurrence rate reported as high as 66%. The open drainage and percutaneous continuous drainage (PCD) has reduced the recurrence rate. The disadvantage of PCD under CT is radiation hazard and problems of asepsis. Hence a technique of clinically guided percutaneous continuous drainage of the psoas abscess without real-time imaging overcomes these problems. We describe clinically guided PCD of psoas abscess and its outcome.
Materials and Methods:
Twenty-nine patients with dorsolumbar spondylodiscitis without gross neural deficit with psoas abscess of size >5 cm were selected for PCD. It was done as a day care procedure under local anesthesia. Sequentially, aspiration followed by guide pin-guided trocar and catheter insertion was done without image guidance. Culture sensitivity was done and chemotherapy initiated and catheter kept till the drainage was <10 ml for 48 hours. Outcome assessment was done with relief of pain, successful abscess drainage and ODI (Oswestry Disability Index) score at 2 years.
Results:
PCD was successful in all cases. Back and radicular pain improved in all cases. Average procedure time was 24.30 minutes, drain output was 234.40 ml, and the drainage duration was 7.90 days. One patient required surgical stabilisation due to progression of the spondylodiscitis resulting in instability inspite of successful drainage of abscess. Problems with the procedure were noticed in six patients. Multiple attempts (n = 2), persistent discharge (n = 1) for 2 weeks, blocked catheter (n = 2) and catheter pull out (n = 1) occurred with no effect on the outcome. The average ODI score improved from 62.47 to 5.51 at 2 years.
Conclusions:
Clinically guided PCD is an efficient, safe and easy procedure in drainage of psoas abscess.
Keywords: Abscess, percutaneous continuous drainage, psoas, spondylodiscitis, tuberculosis
INTRODUCTION
Iliopsoas abscess, a collection of pus in the iliopsoas compartment, was described by Mynter in 1881.1 Iliopsoas abscess is classified as primary and secondary depending on the presence of underlying disease.2 Many patients with dorsolumbar spondylodiscitis at presentation have preserved neurology without major spinal deformity. They may have variable sized abscesses which may be painful and disabling. There are reports of the abscess getting resolved with chemotherapy alone.3,4 The advocates of surgery recommend that once pus is drained the throbbing pain alleviates because the pressure within the cavity reduces and symptoms relieve immediately.5,6 Conventionally, surgical treatment of abscess has been open drainage through the Pettit's triangle or the Poupart's ligament.7 But it is an extensive procedure with morbidity and chances of sinus formation.8 With the advent of minimal invasive (MIS) techniques, surgical procedures for infected spine are also done less invasively.9
Computer tomography (CT) scan and ultrasonography (USG)- guided percutaneous aspiration of the abscess has been a routine procedure10,11 with recurrence rate reported up to 66%.12 Now open drainage or aspiration has been replaced by PCD which has reduced the recurrence rate.13,14 These procedures have significantly reduced morbidity but have the disadvantages of being expensive, with radiation hazards (CT scan) and also doubtful asepsis.
We describe a clinically guided PCD of the psoas abscess without real-time imaging.
MATERIALS AND METHODS
109 patients of psoas abscess with spondylodiscitis were treated conservatively at our institute from Oct 2003 to Oct 2011. Retrospectively the case records of 29 patients with psoas abscess (coronal length bigger than 5 cm), in which image-based blind PCD had been done, were reviewed. The rest of the cases had smaller abscesses. The 5 cm size was chosen arbitrarily as for sizes smaller than 5 cm the margin of error for drainage would be expectedly high. The patients selected did not have any indication of operative treatment.
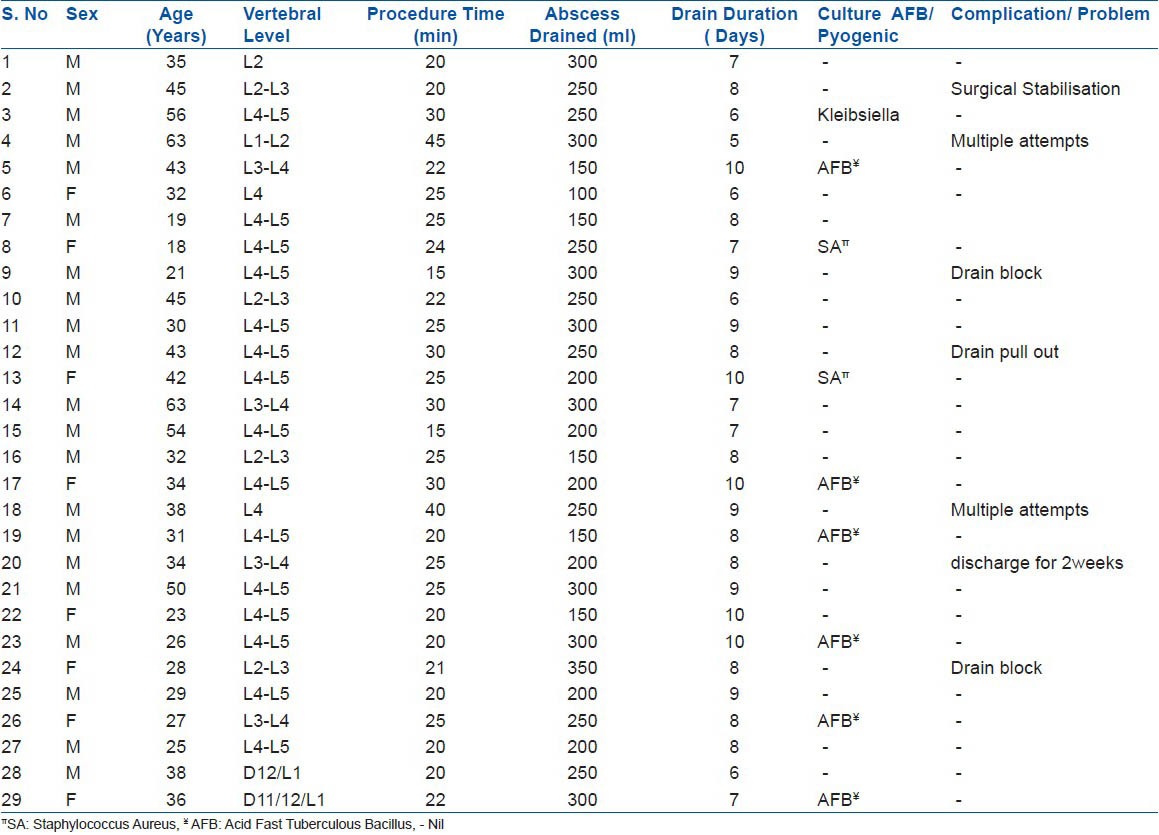
The patients demographic variables were noted with symptomatology and clinical examination [Table 1]. All the patients were initially investigated with radiographs and MRI (standard 1 or 1.5 Tesla) and confirmed the diagnosis of spondylodiscitis of dorsolumbar spine and psoas abscess. The more affected side was planned for drainage. Time taken for the procedure, average drain output, culture and the duration for drainage were noted.
Table 1.
Patient Demography
Preoperatively the Oswestry Disability Index (ODI) score was calculated. The procedure was performed as a day care and patients were followed up.
Estimation of psoas abscess
On MRI T2 axial sequence [Figure 1], measurement of the maximum anteroposterior width of the abscess (dotted black Line) and the distance of this line's posterior skin projection from the midline (white line) is measured. The radiological skin entry point (P) is marked. The distance of point ‘P’ is marked from spinous process. The maximum safe depth measurement (from skin to the anterior abscess wall dotted white line) is calculated. This depth is never violated while putting the needle or cannula. All measurements are done according to the MRI scale markings.
Figure 1.

MRI T2 weighted axial sequence showing measurement of the maximum anteroposterior width of the abscess (black Line 3.4 cm). The distance of this line's posterior skin projection (dotted white line 6.9 cm) from the midline (dotted white line 6.0 cm) is the skin entry point marked “*” Point ‘P’ on the skin denotes entry point.
Procedure
Procedure is performed in the operating room under aseptic precautions under local anaesthesia (LA) [Figure 2]. Patient is put in prone position and bony landmark's are identified to decide the point of entry and the vertebral level. The skin entry point is marked exactly at the distance calculated from the center (mid line) to the side as calculated on the MRI. The needle (16 gauge epidural/spinal 90 mm) is inserted perpendicularly and to a depth already (less than 2 cm) calculated. A loss of resistance is usually well appreciated. Stylet is withdrawn and aspirated to confirm that the needle tip is inside the abscess. Sample is taken for culture and sensitivity. A 0.5 mm long guide wire is threaded into the needle and LA is further given with the spinal needle around the epidural needle. The epidural needle is withdrawn and then over the guide wire the serrated biopsy cannula is inserted into the abscess and pus flow ensured. The guide wire is withdrawn and the 10 FG (French gauge) catheter is threaded through the trocar, so that the catheter coils into the abscess cavity. Drain is secured with sutures to the skin. Catheter is then connected to a suction bag.
Figure 2.

Procedure Illustration (a) The anatomical clinical surface markings with the entry point for the abscess marked patient in prone position. (b) The epidural needle is inserted to a depth less by 2 cm calculated already, then stylet is withdrawn and syringe aspiration done. (c) A 0.5 mm long guide wire is threaded into the needle. (d) The needle is withdrawn and then over the guide wire the serrated biopsy cannula is plunged over the guide wire. (e) The guide wire is withdrawn and the catheter is threaded through the trocar and trocar is then withdrawn. (f) Draining pus flow (arrow). (g) Patient is ambulatory with the PCD
The patients are allowed to go home on the same day. Anti-tuberculosis treatment (ATT) was continued in all the patients and additional antibiotic added if any sensitivity for pyogenic organism was found. Patients were first followed up after 2 days or earlier if the drain bag is full. All catheters were left in place until drainage stopped or was less than 10 ml for 48 hours. On noticing blocked drains/less than expected drain, ultrasound was done before removing the drain. Catheter block with residual significant abscess was managed with withdrawal of the catheter by one inch and again waiting for drainage. Followup ODI score was calculated at 2 years. Patients were followed up regularly in outpatient till treatment completed and at the final follow up of 2 years. Any complications were noted.
Statistical analysis
All demographic data were assessed with calculation of mean ± 2 Standard Deviation, minimum and maximum. A P value for significance of outcome was evaluated. SPSS software was used.
RESULTS
There were 21 males and 8 females in our study the mean age was 36.5 ± 12.7 (range 18-63 years). Fifteen patients had disease at the L4-L5 level and the remaining were of higher lumbar (n = 12) and dorsolumbar (n = 2) levels. The affection was on right side in (n=6), left side in (n=5), and bilateral in (n=18) patients.
Presenting features included back pain (n = 29), radicular pain (n = 6), fever (n = 8), weight loss (n = 15), anorexia (n = 10), walking difficulty (n = 15), spasm (n = 29), range of movement restriction (n = 29), groin mass (n = 5), and pseudo flexion deformity of hip (n = 8). The time taken for the procedure ranged from an average of 24.1 ± 7.4 (range 15-45 minutes). Back pain relief was noted in all patients. Radicular pain was present in 6 patients. Pain disappeared completely in 48 hours of drainage. Average drain output was 224.4 ml ± 74.4 (range 100-350 ml). The average duration for which the drain was used was 7.9 ± 1.4 (range 6-10 days). Positive Pyogenic culture was found in three patients (Staphylococcus aureus = 2, Klebsiella = 1).
The average predrainage ODI score was 62.47 whereas the post treatment ODI score was 5.51 at 2 years followup. Radiographic healing was found in all patients in the form of sclerosis of the body or intervertebral disc space narrowing with fusion.
One patient required surgical stabilization for the spine as subsequent mechanical instability developed inspite of successful drainage of abscess. No major complications were noted. The average time taken for the procedure was 23.88 minutes. Complication was noted in one patient [Table 2]. Multiple attempts were needed in two patients. Persistent discharge was present in one patient for 2 weeks after the removal of the drain. Drain-related complications were found in three patients in the form of blocked catheter (n = 2) and catheter pull out on fourth day (n = 1). Ultrasound was done in these three patients. One patient still had significant collection and was managed with withdrawal of the catheter by one inch which resulted in free flow of pus. Other two had only small residual collection.
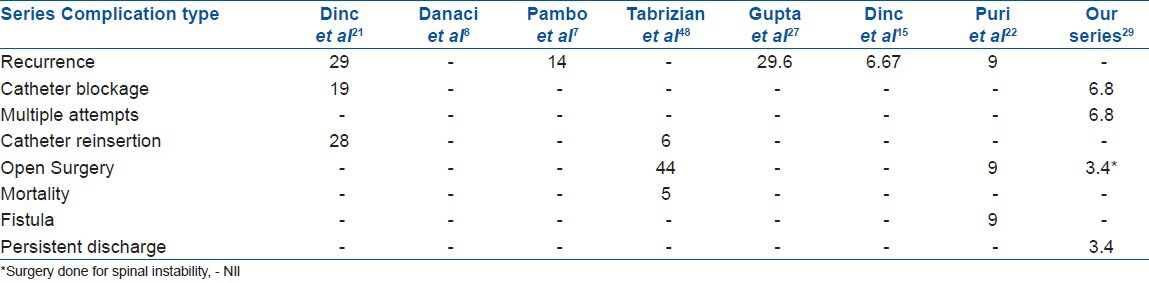
Table 2.
Comparison of complications with other series
DISCUSSION
Iliopsoas abscess is classified on the presence of underlying disease as primary (30% cases) and secondary (70% cases). Primary abscess is pyogenic and is caused by hematogenous or lymphatic spread15,16 usually associated with a predisposing immunosuppression.17 Secondary psoas abscess occurs as a result of local extension from an infective pathology from the adnexa. The most common conditions leading to this are spondylodiscitis (40%) and other conditions (60%) like Crohn's disease, appendicitis, neoplasm, pyonephrosis, etc.18 HIV patients because of immune modulation have tendency to develop more epidural abscess and cord compression.19 Primary psoas abscess are more common in younger patients. In contrast, up to 40% of secondary abscesses mostly occur after the age of 40 years.20 All our cases were secondary psoas abscesses in spondylodiscitis and with no age predilection.
Primary psoas abscess is commonly caused by S. aureus while the secondary psoas abscess is commonly caused by agents like M. tuberculosis, Streptococcus agalactiae, Escherichia coli, Klebsiella, etc.17,20 In areas where tuberculosis is endemic, 5% of dorsolumbar tubercular cases develop a psoas abscess.2 In our series the culture was positive for Mycobacterium tuberculosis (n = 6), S. aureus (n = 2), Klebsiella (n = 1), while no organism was cultured in 20 patients. In spite of getting negative cultures in 20 patients, ATT was continued because tuberculosis is endemic in this part of the world and is a paucibacillary disease hence no organism could be cultured. The chances of getting positive culture in tuberculosis are of the order of 50% to 60%.21,22 All patients were already on ATT since a variable period before presenting to us, thereby decreasing the chances of isolation of the organism. Thus, cultures of appropriate clinical specimens should be obtained prior to starting empirical therapy.23,24
The classical triad of symptoms of a primary psoas abscess include fever, loin pain and groin mass.25 The clinical image can be dominated by peritoneal inflammation expressed by nausea, vomiting and watery stools.17 The presenting signs and symptoms were mixed of the spondylodiscitis and psoas abscess in our study.
The mortality rate in undrained pyogenic psoas abscess is as high as 50% to 100%.17,26 Death is usually due to inadequate or delayed treatment, with mortality close to 100% in patients who do not undergo drainage, most often from sepsis.18 The management of psoas abscess comprises a combination of chemotherapy and open operative drainage, which has been replaced by PCD under USG or CT guidance.10,11,12,13,14 Needle aspiration is frequently not successful and also has high recurrence rates.12,27 CT-guided aspirations/PCD for pelvic and small abscess is recommended.27 Three of our patients (before coming to us) had failed aspirations and two had recurrence.
The original criteria for PCD were limited to well-defined unilocular abscesses and multiple catheters for multilocular abscess.30 Multilocular abscesses can be managed with a single catheter, because the loculi intercommunicate.29 In our series, though there were five multi-loculated abscesses no attempt was made to drain them separately.
PCD is performed with USG, CT and fluoroscopy.7,8,11,14,15,21,22,24,28 But, we are not using any of these modalities. Generally there are two methods for introducing the catheter into the abscess, one by the trocar technique and the other by sequential Seldinger technique.3,28 Though, the single puncture trocar drainage system often saves time, the Seldinger technique allows better control and decreases the complication rate.31 Our technique is principally a combination of Seldinger and trocar technique, as it uses a needle for aspiration and then over the centered guide wire the serrated trocar is inserted. Compare to USG/CT guided technique, our technique is simple and can be done as a day care procedure under LA. Contraindications for percutaneous treatment are uncorrectable coagulopathy, lack of safe access and lack of patient cooperation. Its advantages are avoidance of general anesthesia and stress of surgery and thus indirectly reduced morbidity.15
Abscesses under pressure benefit from the immediate decompression provided through drainage.4,5,6 This was very evident with the significant and quick improvement in low back pain (n = 29) and radicular pain (n = 6). The drainage reduces the bulk of disease rendering it easy for the ATT to work on.32 In spinal osteomyelitis a biopsy can lead to a change in management in 35% of cases.33 Three of our cases who were on empirical ATT came out positive with culture of pyogenic organism. Add-on therapy in 10.34% following culture was required.
In our series average drain output and catheter duration was 224.4 ml and 7.9 days, respectively. Duration of drainage has been reported from 7 to 28 days.27 Longer duration can lead to fistula formation.25 We had one case of long duration discharge but no fistula formation. Followup USG/CT/MRI can be done to check the completeness of drainage and recurrence.27 But we didn’t do it on regular basis except in the one case of drain pullout and two cases of drain block and one case for demonstration [Figure 3].
Figure 3.

(a and b) Anteroposterior and lateral radiograph showing D11-12 paradiscal affection. (c and d) MRI sagittal T1W and T2W showing D11-D12-L1 spondylodiscitis. (e and f) MR Myelogram and T1 coronal section showing the huge abscess extending from L1 to L5, with maximum width at L3 lower border in the right side (yellow arrow). (g) MRI T2 axial image at L 3 lower border. The estimation from this section is used to decide the desired point of aspiration by our technique (details in Figure 1). (h) 3D CT reconstruction image showing the coiled catheter in the abscess. (i) MRI T 2 coronal image showing the collapsed aspirated abscess cavity (white arrow). (j and k) Anteroposterior and lateral radiograph showing healed sclerosed vertebrae at 18 months
Complete cure of the abscesses could be achieved in 28 of 29 abscesses (96.55%). The recurrence rate in other series have been 14% to 29%.6,11,12 There was no recurrence in our series. The high cure rates and low recurrence in our series may be due to the fact that all the patients were on ATT for at least 3 weeks predrainage. There are recommendations to give ATT at least 3-4 weeks prior to PCD or otherwise to keep the drain for longer periods.27 The ODI improvement at 2 years was significant (P < 0.05) and radiographic healing was found in all the patients. The clinico-radiological improvement with no evidence of recurrence at 2 years or more is considered a healed status.34
Our study have many limitations. Ours was a retrospective study. A prospective, randomized controlled study would be advisable. It is unknown whether the alterations in treatment would have resulted in better outcomes. We had no systematic control group for these patients. Outcome studies with controls with non-surgical treatment, aspiration only and open drainage are necessary before we can determine the full clinical value of PCD. Inability to place the tip of a catheter in a gravity-dependent position to facilitate drainage in our blind procedure is a theoretical disadvantage. 29 patients in our study were selected with specific inclusion criterion (size > 5 cm). The results therefore cannot be used to judge the incidence of positive outcomes that can be achieved if this technique were applied to a larger group of patients.
Clinically guided PCD of the psoas abscess is a minimal invasive, efficient and safe procedure.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Mynter H. Acute psoitis. Buffalo Med Surg J. 1881;21:202–210. [PMC free article] [PubMed] [Google Scholar]
- 2.Chawla K, D’Souza A, N SB, Mukhopadhayay C. Primary tubercular psoas abscess: A rare presentation. J Infect Dev Ctries. 2012;6:86–8. [PubMed] [Google Scholar]
- 3.Dinç H, Ahmetoğlu A, Baykal S, Sari A, Sayil O, Gümele HR. Image-guided Percutaneous Drainage of Tuberculous Iliopsoas and Spondylodiskitic Abscesses. Midterm Results Radiology. 2002;225:353–8. doi: 10.1148/radiol.2252011443. [DOI] [PubMed] [Google Scholar]
- 4.Kalpesh JG. Puncture, drainage and irrigation: Is that enough for treating an abscess? Indian J Plast Surg. 2006;39:189–95. [Google Scholar]
- 5.Pieri S, Agresti P, Altieri AM, Ialongo P, Cortese A, Alma MG, et al. Percutaneous management of complications of tuberculous spondylodiscitis: Short- to medium-term results. Radiol Med. 2009;114:984–95. doi: 10.1007/s11547-009-0425-3. [DOI] [PubMed] [Google Scholar]
- 6.Yacoub WN, Sohn HJ, Chan S, Petrosyan M, Vermaire HM, Kelso RL, et al. Psoas abscess rarely requires surgical intervention. Am J Surg. 2008;196:223–7. doi: 10.1016/j.amjsurg.2007.07.032. [DOI] [PubMed] [Google Scholar]
- 7.Wood GW. Campbell's Operative Orthopaedics. In: Canale ST, editor. Chapter 43-Infections of Spine. 12th ed. Philadelphia: Mosby; 2011. pp. 1965–92. [Google Scholar]
- 8.Weinberg JA. The surgical excision of psoas abscesses resulting from spinal tuberculosis. J Bone Joint Surg Am. 1957;39:17–27. [PubMed] [Google Scholar]
- 9.Jain AK, Rajasekaran S. Tuberculosis of the spine. Indian J Ortho. 2012;46:127–9. doi: 10.4103/0019-5413.93671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dahniya MH, Hanna RM, Grexa E, Cherian MJ, Niazy MN, Badr S, et al. Percutaneous drainage of tuberculous iliopsoas abscesses under image guidance. Australas Radiol. 1999;43:444–7. doi: 10.1046/j.1440-1673.1999.00709.x. [DOI] [PubMed] [Google Scholar]
- 11.Kang M, Gupta S, Gulati M, Suri S. Ilio-psoas abscess in the paediatric population: Treatment by us-guided percutaneous drainage. Pediatr Radiol. 1998;28:478–81. doi: 10.1007/s002470050389. [DOI] [PubMed] [Google Scholar]
- 12.Gupta S, Suri S, Gulati M, Singh P. Ilio-psoas abscesses: Percutaneous drainage under image guidance. Clin Radiol. 1997;52:704–7. doi: 10.1016/s0009-9260(97)80036-0. [DOI] [PubMed] [Google Scholar]
- 13.Dinç H, Onder C, Turhan AU, Sari A, Aydin A, Yuluð G, et al. Percutaneous catheter drainage of tuberculous and nontuberculous psoas abscesses. Eur J Radiol. 1996;23:130–4. doi: 10.1016/0720-048x(96)01045-5. [DOI] [PubMed] [Google Scholar]
- 14.Cantasdemir M, Kara B, Cebi D, Selcuk ND, Numan F. Computed tomography-guided percutaneous catheter drainage of primary and secondary iliopsoas abscesses. Clin Radiol. 2003;58:811–5. doi: 10.1016/s0009-9260(03)00274-5. [DOI] [PubMed] [Google Scholar]
- 15.Danaci M, Belet U, Akan H, Selcuk MB, Karaismailoglu TN, Elmail E, et al. Treatment of tuberculous and nontubereulous psoas abscesses with percutaneous catheter drainage. Omu Tlp Dergisi. 1999;16:55–61. [Google Scholar]
- 16.Tuli SM. Relevent surgical anatomy. In: Tuli SM, editor. Tuberculosis of skeletal system. 3rd ed. New Delhi: Jaypee Brothers Medical Publications; 2004. p. 11. [Google Scholar]
- 17.Crisan A, Nicoara E, Bota K, Bordos D. Primary psoas abscess. TMJ. 2004;54:374–6. [Google Scholar]
- 18.Gruenwald I, Abrahamson J, Cohen O. Psoas abscess: Case report and review of the literature. J Urol. 1992;147:1624–6. doi: 10.1016/s0022-5347(17)37650-4. [DOI] [PubMed] [Google Scholar]
- 19.Anley CM, Brandt AD, Dunn R. Magnetic resonance imaging findings in spinal tuberculosis: Comparison of HIV positive and negative patients. Indian J Orthop. 2012;46:186–90. doi: 10.4103/0019-5413.93688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riyad MN, Sallam MA, Nur A. Pyogenic psoas abscess: Discussion of its epidemiology, etiology, bacteriology, diagnosis, treatment and prognosis-case report. Kuwait Med J. 2003;35:44–7. [Google Scholar]
- 21.Levine MJ, Pedlow FX. Spinal infections. In: Garfin SR, Vaccaro AR, editors. Orthopedic knowledge update: Spine. Rosemont: American Academy of Orthopedic Surgeons; 1997. pp. 257–71. [Google Scholar]
- 22.Slucky AV, Eismont FJ. Spinal infections. In: Bridewell KH, Dewald RL, editors. The textbook of spinal surgery. Pheladelphia: Lippincott-Raven; 1997. pp. 2141–83. [Google Scholar]
- 23.Maki DJ. Microbiologic diagnosis of blood culture-negative sepsis by hemofiltration. Crit Care Med. 2004;32:1075–7. doi: 10.1097/01.ccm.0000120048.81149.78. [DOI] [PubMed] [Google Scholar]
- 24.Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003;348:138–50. doi: 10.1056/NEJMra021333. [DOI] [PubMed] [Google Scholar]
- 25.Siu AY, Law KL, Lo CB, Chung CH. Lowback pain: Would it be psoas abscess. Hong Kong J Emerg Med. 2002;9:213–6. [Google Scholar]
- 26.Tomich EB, Della-Giustina D. Bilateral Psoas Abscess in the Emergency Department. West J Emerg Med. 2009;10:288–91. [PMC free article] [PubMed] [Google Scholar]
- 27.Puri SK, Panicker H, Narang P, kumar N, Dhall A, Gupta SB. Percutaneous drainage of tuberculous abcesses. Indian J Radiol Imaging. 2001;11:13–6. [Google Scholar]
- 28.Gervais DA, Connolly SA, Brec SL, Harisinghani MG, Mueller PR. Percutaneous imaging guided abdominal and pelvic abscess drainage in children. Radiographics. 2004;24:737–54. doi: 10.1148/rg.243035107. [DOI] [PubMed] [Google Scholar]
- 29.Yin HP, Tsai YN, Liao SF, Lin PH, Chuang TY. The challenge of diagnosing psoas abscess. Chin Med Assoc. 2004;67:156–9. [PubMed] [Google Scholar]
- 30.Lambiase RE, Deyoe L, Cronan JJ, Dorfman GS. Percutaneous drainage of 355 consecutive abscesses; result of primary drainage with 1 year follow up. Radiology. 1992;184:167–79. doi: 10.1148/radiology.184.1.1376932. [DOI] [PubMed] [Google Scholar]
- 31.VanSonnenberg E, Casola G, Wittich GR, Varney RR, Harker C. Lung abscess: CT guided drainage. Radiology. 1991;178:347–51. doi: 10.1148/radiology.178.2.1987590. [DOI] [PubMed] [Google Scholar]
- 32.Diwanji S, Zaveri G. Posterior inter transeverse approach for drainage of psoas abscess associated with spinal tuberculosis. J Orthopaedics. 2006;3:e10. [Google Scholar]
- 33.Rankine J, Barron D, Robinson P, Millner P, Dickson R. Therapeutic impact of percutaneous spinal biopsy in spinal infection. Postgrad Med J. 2004;80:607–9. doi: 10.1136/pgmj.2003.017863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jain AK. Tuberculosis of spine: A fresh look at an old disease. J Bone Joint Surg Br. 2010;92:905–13. doi: 10.1302/0301-620X.92B7.24668. [DOI] [PubMed] [Google Scholar]


