Abstract
Background:
Discectomy performed open or with an operating microscope remains the standard surgical management. Tubular retractor system is being increasingly used. Potential benefits include less muscle and local damage, better cosmesis, decreased pain and operative time and faster recovery after surgery. We have evaluated the outcome of micro endoscopic discectomy (MED) utilizing tubular retractors in terms of safety and efficacy of the technique.
Materials and Methods:
188 consecutive patients who underwent surgery for herniated disc using the tubular retractors between April 2007 and April 2012 are reported. All patients had a preoperative MRI (Magnetic Resonance Imaging) and were operated by a single surgeon with the METRx system (Medtronic, Sofamor-Danek, Memphis, TN) using 18 and 16 mm ports. All patients were mobilized as soon as pain subsided and discharged within 24-48 hours post surgery. The results were evaluated by using VAS (Visual Analog Scale 0-5) for back and leg pain and ODI (Oswestry Disability Index). Patients were followed up at intervals of 1 week, 6 weeks, 3 months, 6 months, 12 months and 2 years.
Results:
The mean age of patients was 46 years (range 16-78 years) and the sex ratio was 1.5 males to 1 female. The mean followup was 22 months (range 8-69 months). The mean VAS scale for leg pain improved from 4.14 to 0.76 (P < 0.05) and the mean VAS scale for back pain improved from 4.1 to 0.9 (P < 0.05). The mean ODI changed from 59.5 to 22.6 (P < 0.05). The mean operative time per level was about 50 minutes (range 20-90 minutes). Dural punctures occurred in 11 (5%) cases. Average blood loss was 30 ml (range 10-500 ml). A wrong level was identified and later corrected in a case of revision discectomy. Four patients with residual disc-herniation had revision MED and three patients with recurrent disc herniation later underwent fusion. One patient had wound infection which needed a debridement.
Conclusion:
MED for herniated discs effectively achieves the goals of surgery with minimal access. The advantages of the procedure are cosmesis, early postoperative recovery and minimal postoperative morbidity.
Keywords: Herniated nucleus pulposus (HNP), micro endoscopic discectomy, minimal invasive spine surgery
INTRODUCTION
Discectomy first reported by Mixter and Barr1 (1934) has changed the management of lumbar disc herniations. Kambin and Savitz2 (1973) introduced the concept of endoscopic lumbar discectomy. Caspar3 (1977), Yasargil4 (1977) and Williams5 (1978) added refinements in approach with the use of microsurgical technique. Foley and Smith6 (1997) introduced an operative endoscope with the tubular system terming it “Endoscopic Discectomy”. As an alternative to the endoscope, Foley et al. (2003) modified the tubular retractors to include a microscope, which is termed “Micro Endoscopic Discectomy” (MED). The term is used interchangeably for describing the discectomy procedure utilizing tubular retractors either with an endoscope or a microscope.7 Recent prospective randomized control trials (RCTs) have found a benefit of surgery for patients when conservative therapies fail.8,9,10,11 Discectomy performed open or with an operating microscope remains the standard surgical management.12,13,14 Tubular retractor system15,16,17 is being increasingly used now. The potential benefits of to this technique include less muscle and local damage, better cosmesis,18,19,20 decreased pain and operative time and faster recovery after surgery.21,22 On the other hand, open surgery includes extensive retraction and dissection of paraspinal muscles, longer operative time, longer incisions and bone resection.23,24 Many surgeons have been reluctant to use these techniques due to significant learning curve.
In India, Ranjan et al.,25 Jayaswal et al.,26 and Jhala et al.,27 have reported the use of METRx tubular system for discectomy with an endoscope. Kaushal et al.28 have reported results of the Destandau endoscopic technique. We report our experience using the METRx tubular retractor system with a microscope. To the best of our knowledge this is the first study from India where a combination of METRx system and microscope has been used in a large series [Figure 1a].
Figure 1.
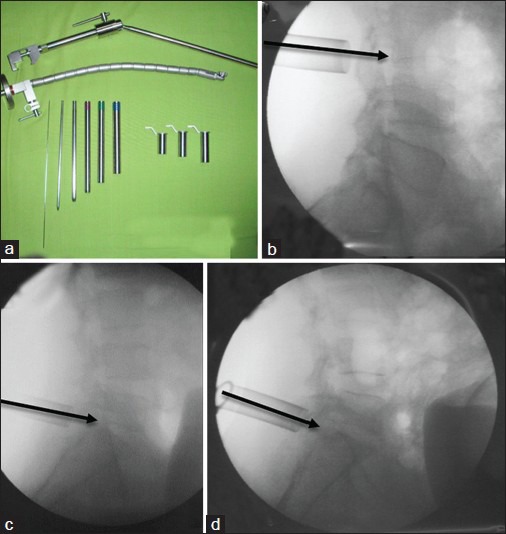
(a) Image showing flexible docking arm with serial dilators and tubular retractor of different sizes. (b) Intraoperative fluoroscopic image showing superior angulation in superior migrated disc herniation. (c) Intraoperative fluoroscopic image showing angulation in disc herniation with no migration. (d) Intraoperative fluoroscopic image showing inferior angulation in inferior migrated disc herniation
MATERIALS AND METHODS
188 consecutive patients who underwent surgery for herniated disc using the tubular retractor were prospectively evaluated between April 2007 and April 2012. Patients with at least 6 weeks of conservative treatment with positive nerve root tension signs, radicular pain and correlating MRI findings were included. Exclusions were patients with large central disc herniations, chronic discogenic pain, discitis, previous instrumentation, multilevel fusions or presence of instability. There was no control group. All patients had preoperative standing x-rays and MRI and were operated by a single surgeon with the METRx™ system (Medtronics Sofamor-Danek, Memphis, TN, USA) using the 18 and 16 mm ports.
Operative procedure
The patient was positioned on a radiolucent table in prone position with bolsters below the chest and the iliac crest keeping the abdomen free, head end raised and pressure points well padded. The surgeon stands on the side of the herniation. Using lateral fluoroscopy imaging on ipsilateral side, a 20 G spinal needle was inserted at the level of the involved disc space. The needle was inserted 1.2 cm lateral to the midline. The needle should be either targeted superiorly, at the disc level or inferiorly, depending upon the anatomy of the herniation or sequestration [Figure 1b–d]. A 20 mm incision was then made centered over the needle and wafs deepened till the fascia. The incision was 18 mm if a 16 mm-diameter tube was used. The blunt end of the guide wire was then inserted under fluoroscopic guidance. The sharp end should be avoided as it can cause a dural tear. The target site was the inferior lamina of the superior vertebrae that was the junction of lamina and medial facet. The initial dilator was then inserted over the guide wire and the wire was removed. The initial dilator was used to sweep off the para-spinal muscle mass and palpate the bony landmarks. Sequential dilators were then inserted while confirming the target site under fluoroscopy [Figure 2a]. The marking on the final dilator at the level of skin provides the depth of the tubular retractor. If the marking is between 4 and 5 then a number 5 tubular retractor should be used. The final tubular retractor, which was 18 or 16 mm in diameter, was then docked with the flexible arm as the final working channel [Figure 2b]. The 18 mm tube was most commonly used in this series. The 16 mm tube was utilized in cases where the disc herniation was small and restricted to the disc space without any migration. In cases of extra-foraminal disc herniations the incision was taken just lateral to the facet joint under fluoroscopic guidance and the tube was docked just lateral to the facet joint directly over the fragment. The operating microscope was then brought into the field [Figure 2b].
Figure 2.
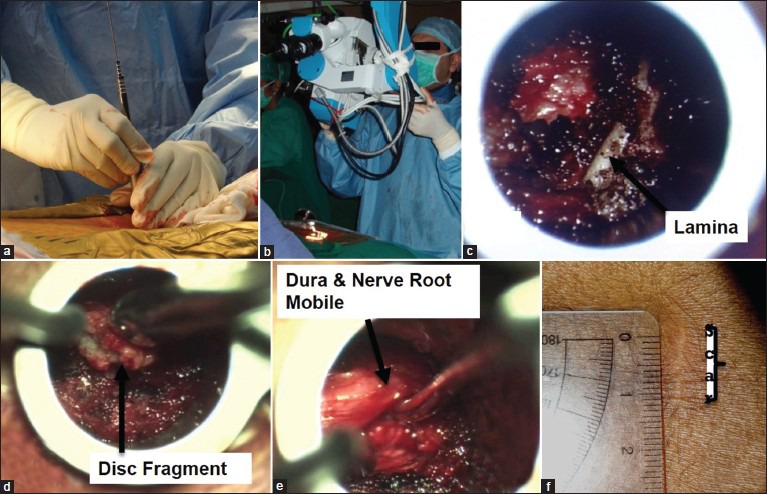
(a) Intraoperative image showing serial dilators being introduced. (b) Intraoperative image showing docked tubular retractor with the flexible arm as the final working channel. (c) Intraoperative microscope camera image showing lamina after soft tissue is removed. (d) Intraoperative microscope camera image showing extraction of herniated disc fragment. (e) Intra-operative microscope camera image showing mobile dura and nerve root. (f) Post-operative image showing length of surgery scar after healing
The soft tissue was separated using a long cautery tip till the lamina could be visualized [Figure 2c]. Then, laminotomy was done using a 4 mm high speed burr, till the junction of the inner cortex and ligamentum flavum was encountered. A cleft was created in the ligamentum flavum with a no. 4 Penfield dissector. The flavum was then excised medially and laterally using a no. 2 Kerrison rongeur to get a good visualization of the dural sac and nerve root. It was important to determine preoperatively on the MRI, whether the location of the disc was in the axilla or the shoulder of the nerve root. An inferiorly migrated disc was generally in the axilla of the nerve root. In case of a shoulder disc the nerve root once identified, can be retracted medially using a nerve root retractor. The disc was then identified. The bulge in a contained disc can be well appreciated under the microscope. Then, an annulotomy was done with a no. 15 blade on a bayonet handle in cruciate manner or the annular tear if present can be probed with a nerve hook. The disc was then probed using a nerve hook and the herniated fragment was delivered out of the annulus. The fragment was then removed with a disc forceps [Figure 2d]. Multiple attempts were made to seek hidden disc fragments with a nerve hook till adequate nerve root decompression was performed. A pulsatile central dural sac and nerve root that was mobile was considered an adequate decompression surgery [Figure 2e]. The epidural bleeding was controlled using a combination of bipolar cautery, bone wax and Gelfoam®. The thoracolumbar fascia and subcutaneous tissue were closed using 2-0 Vicryl (Ethicon, Johnson and Johnson). The skin was closed using 3-0 Monocryl (Johnson and Johnson Int.).
A single dose of intravenous antibiotic was given on the same night as a standard protocol. Postoperatively, all patients were mobilized as soon as the pain subsides and and were discharged within 24-48 hours post-surgery. The patients were allowed to go back to work after 3 weeks. A gradual back-strengthening program was started after 6 weeks.”
Only one dose of intravenous antibiotic was given on the same night as a standard protocol. Postoperatively, all patients were mobilized as soon as the pain subsided and discharged within 24-48 hours post-surgery. Patients were allowed to go back to work after 3 weeks. A gradual back-strengthening program was started after 6 weeks.
The patients were followed up at intervals of 1 week, 6 weeks, 3 months, 6 months and 12 months and 2 years and were evaluated for technical problems like tube docking issues, complications and overall results by VAS (Visual Analogue Scale) for back and leg pain and ODI questionnaire (Oswestry Disability Index). Paired samples t-tests were used for comparisons of continuous variables like VAS and ODI. All statistical analyses were performed using IBM® SPSS® software version 15.0. A probability value of P < 0.05 was considered statistically significant.
RESULTS
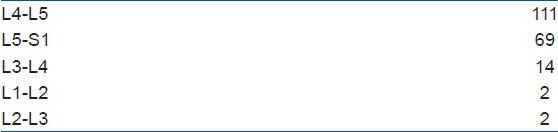
The mean age of patients was 46 years (range 16-78 Years) and the male to female ratio was 1.5:1. The mean followup was 27 months (range 8-69 months). 94% of patients had paracentral disc [Figure 3]. Eight patients (4%) also had associated stenosis. Out of 198 total levels operated, L4-5 (n = 111, 56%) and L5-S1 (n = 69, 35%) were the most commonly involved [Table 1]. A 18 mm tube was used in 160 (85%) patients and 16 mm tube was used in 28 (15%) patients.
Figure 3.
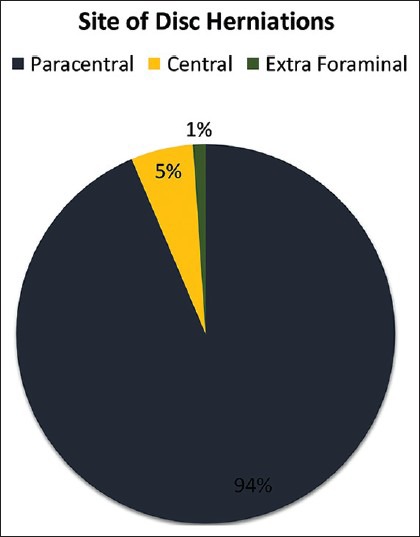
Pie chart diagram depicting frequency of disc herniations based on morphology
Table 1.
Levels operated in our study (n=198)
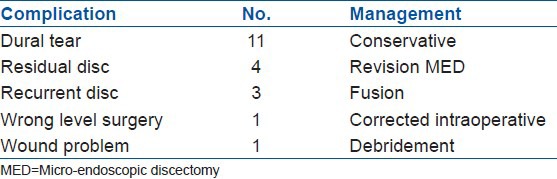
The mean operative time per level was about 50 minutes (range 20-90 minutes). Some of the cases done early in the study took a longer time that is up to 90 minutes, however after gaining experience the average time taken for surgery was less than the mean average. The average blood loss was 30 ml (range 10-500 ml). There was only one patient who bled close to 500 ml of blood. This was secondary to unexpected bleeding from the cancellous bony surfaces as a result of osteoporosis as well as disproportionate epidural bleeding. Dural punctures in our study occurred in 11 cases (5%) [Table 2]. The first three cases were managed with fibrin glue injection was used over the tear and the other tears were treated conservatively with masterly inactivity. No delayed cerebrospinal fluid leaks or pseudomeningoceles developed. One wrong level (0.5%) was identified and later corrected in a case of revision discectomy. There were four patients (2.1%) with residual disc-herniation; all had a successful revision MED. There were three patients (1.5%) with recurrent disc-herniation who later underwent fusion. These occurred at 1 month, 3 months and 4 months after the primary MED. One patient (0.5%) had wound infectious. The patient needed debridement, antibiotics and dressings and recovered without further complications.
Table 2.
Complications (n=188)
The mean VAS scale for leg pain improved significantly from a preoperative value of 4.14 to 0.76 (P < 0.05) postoperatively. The mean VAS scale for back pain changed significantly from a preoperative value of 4.1 to 0.9 (P < 0.05) postoperatively. The mean ODI changed significantly from 59.5 to 22.6 (P < 0.05) till last followup.
DISCUSSION
Lumbar disc herniations causing significant or new neurological deficit, cauda equina syndrome, or those refractory to conservative treatment are dealt surgically.3,4,5,6 A proper technique should lead to satisfactory outcomes, minimal morbidity and good cosmesis. It should be cost effective, able to adjust to patient factors like obesity, ethnicity, etc., The percutaneous systems such as chemonucleolysis,29 percutaneous lumbar discectomy (manual30 and automated31), nucleoplasty and percutaneous laser-assisted discectomy32 cannot deal with disc fragment extrusions and associated bony and ligamentous compression. The results of these procedures have been very variable and speculative ranging from 29% to 92% success rates.16
Open discectomy (OD) and microdiscectomy remain the current standard of surgical treatment.12,13,14 Several recent prospective RCTs have compared OD to tubular retractor-based MED33,34,35,36 and success rates have been found to be similar. Our results are comparable to results of MED by Wu et al.,37 in which the mean VAS scale changes were significant and ODI changed from 48% to 23%. In our series, there was one wound infection at a rate of 0.5%, discitis rate of 0% and a durotomy rate of 5%. These rates compared favorably with those reported by Ebling et al.,38 (3.3%, 0.8% and 3.9%, respectively), Caspar et al.,39 (0.7, 0.7 and 6.7% respectively), Williams et al.,14 (0, 0 and 0% respectively) and Pappas et al.,40 (7.2, 0.5 and 1%, respectively). Our re-operation rate was 4.2% while the reoperation rate in MED series by Wu et al.37 was 2.4%. A higher rate in our case could be attributed to two peaks in the learning curve: One at the beginning with the use of the 18 mm tube and the other at the beginning with the 16 mm tube. The complications occurred during the initial cases of using the respective tubes. As the authors performed more cases, gaining experience the learning curve was negotiated and in subsequent cases, the complication rates were negligible. The aforementioned authors14,38,39,40 reported reoperation rates in OD ranging from 3% to 14%. In our series there were 11 cases (5%) of dural tears. The fibrin glue injection was used over the dorsal tear. Due to inherent quality of technique there is no dead space to encourage the collection of CSF as the paraspinal muscles, thoracolumbar fascia, subcutaneous soft tissues, and skin fall into place causing a tamponade-effect once the tube is retracted. There were three cases of recurrent disc herniations. The patients chose a fusion procedure over a revision discectomy and underwent a successful fusion.41
The advantages of MED over OD include small incision, better cosmesis, early ambulation, less postoperative pain, less blood loss, short hospital stay, less analgesics, short time to return to work and thus less cost of treatment.20,42,43,44 In our study skin incision was 1.8-2 cm in length initially which after shrinkage [Figure 2f] (which accompanies healing), became shorter leading to better cosmesis. If one would compare microdiscectomy and MED, it is but natural that if both the procedures have the same overall outcome, then the procedure with lesser tissue invasion, lesser length of incision, lesser use of postoperative analgesics with an early return to work becomes the procedure of choice.13 This was the conclusion drawn by Katayama et al.,13 while comparing microdiscectomy against macrodiscectomy.
Minimal tissue damage has been proven by studies comparing measurements of pre-operative and postoperative cross-sectional area (by MRI or CT) of paraspinal muscles, intraoperative EMG, serum biochemical markers (CRP, CPKMM and IL) and histological evidence, which show MED causes less local damage than microdiscectomy and OD.19,45,46,47 It was found to be more effective in obese patients and in extraforaminal HNPs. These patients need more soft tissue dissection in OD for visualization thereby improving outcomes and decreasing complications.
Another measure of success of this technique is reflected by the patient's ability to return early to the previous job. Bookwalter et al.44 reported that 40% of their patients returned to work in fewer than 5 weeks proving its cost-effectiveness. Caspar et al.39 reported a mean return-to-work time of 18.6 weeks and Foley and Smith15 reported a mean return-to-work time of 17.6 days. Our protocol is to allow patients to resume work after 2 weeks following surgery.
Majority of patients in the two most recently published RCTs comparing OD and MED expressed a preference for MED.48,49 METRx™ can be used with both a microscope and an endoscope. The microscope system allows both hands free and therefore two separate instruments can be used simultaneously as dissection is performed with clear visualization of structures under a microscope.41 This is the advantage of this system over Destandau system, wherein the surgeon has to hold the tube while performing the procedure with one hand only. While with an endoscope, there is problem of fogging of the camera secondary to cautery smoke as well as contamination by blood in the field, which requires repeated withdrawal and cleaning of the camera lens. The limitations of MED include a learning curve, specialized equipment and specific training. A study on lumbar MED by a single surgeon states that approximately 30 cases are required to overcome the learning curve and before the operative time and complications reduce.50 METRx™ tubular system is a highly versatile system. It can be used for doing advanced procedures like decompression of central canal and lateral recess stenosis, cervical foraminotomies, tumor removal and minimally invasive fusions (TLIF (transforaminal lumbar interbody fusion)), etc., There is a growing interest in this technique in the subcontinent with increasing number of authors reporting its successful usage in the management of disc herniations.25,26,27
To conclude microendoscopic surgery for herniated discs effectively achieves the goals of surgery with minimal access. There is a learning curve associated with the procedure to reach an adequate level of expertise. Adequate training of surgeons and effective utilization of the technique can harness the benefits of this procedure and make it a gold standard in management of prolapsed lumbar discs.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:210–5. [Google Scholar]
- 2.Kambin P, Savitz MH. Arthroscopic microdiscectomy: An alternative to open disc surgery. Mt Sinai J Med. 2000;67:283–7. [PubMed] [Google Scholar]
- 3.Caspar W. A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach. In: Wullenweber R, Brock M, Hamer J, editors. Advances in Neurosurgery. Berlin: Springer-Verlag; 1977. pp. 74–7. [Google Scholar]
- 4.Yasargil MG. Microsurgical operation for herniated disc. In: Wullenweber R, Brock M, Hamer J, Klinger M, Spoerri O, editors. Advances in Neurosurgery. Berlin: Springer-Verlag; 1977. p. 81. [Google Scholar]
- 5.Williams RW. Microlumbar discectomy: A conservative surgical approach to the virgin herniated lumbar disc. Spine (Phila Pa 1976) 1978;3:175–82. [PubMed] [Google Scholar]
- 6.Foley KT, Smith MM. Microendoscopic discectomy. Techniques in Neurosurgery. 1997;3:301–7. [Google Scholar]
- 7.Kulkarni AG, Dhruv AN, Bassi AJ. Microendoscopic Excision of C2 osteoid osteoma: A Technical Report. Spine (Phila Pa 1976) 2008;38:E1231–4. doi: 10.1097/BRS.0b013e31829cbf5e. [DOI] [PubMed] [Google Scholar]
- 8.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Longterm outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the Maine lumbar spine study. Spine (Phila Pa 1976) 2005;30:927–35. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 9.Pearson AM, Blood EA, Frymoyer JW, Herkowitz H, Abdu WA, Woodward R, et al. SPORT lumbar intervertebral disk herniation and back pain: Does treatment, location, or morphology matter? Spine (Phila Pa 1976) 2008;33:428–35. doi: 10.1097/BRS.0b013e31816469de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356:2245–56. doi: 10.1056/NEJMoa064039. [DOI] [PubMed] [Google Scholar]
- 11.Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse: Updated Cochrane Review. Spine (PhilaPa 1976) 2007;32:1735–47. doi: 10.1097/BRS.0b013e3180bc2431. [DOI] [PubMed] [Google Scholar]
- 12.Tait MJ, Levy J, Nowell M, Pocock C, Petrik V, Bell BA, et al. Improved outcome after lumbar microdiscectomy in patients shown their excised disc fragments: A prospective, double blind, randomised, controlled trial. J NeurolNeurosurg Psychiatry. 2009;80:1044–6. doi: 10.1136/jnnp.2008.156356. [DOI] [PubMed] [Google Scholar]
- 13.Katayama Y, Matsuyama Y, Yoshihara H, Sakai Y, Nakamura H, Nakashima S, et al. Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: A prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech. 2006;19:344–7. doi: 10.1097/01.bsd.0000211201.93125.1c. [DOI] [PubMed] [Google Scholar]
- 14.McGirt MJ, Ambrossi GL, Datoo G, Sciubba DM, Witham TF, Wolinsky JP, et al. Recurrent disc herniation and long term back pain after primary lumbar discectomy: Review of outcomes reported for limited versus aggressive disc removal. Neurosurgery. 2009;64:338–45. doi: 10.1227/01.NEU.0000337574.58662.E2. [DOI] [PubMed] [Google Scholar]
- 15.Freudenstein D, Duffner F, Bauer T. Novel retractor for endoscopic and microsurgical spinal interventions. Minim Invasive Neurosurg. 2004;47:190–5. doi: 10.1055/s-2004-818487. [DOI] [PubMed] [Google Scholar]
- 16.Husain M, Jha DK, Agrawal S, Husain N, Gupta RK. Conical working tube: A special device for endoscopic surgery of herniated lumbar discs. J Neurosurg Spine. 2005;2:265–70. doi: 10.3171/spi.2005.2.3.0265. [DOI] [PubMed] [Google Scholar]
- 17.Isaacs RE, Podichetty V, Fessler RG. Microendoscopic discectomy for recurrent disc herniations. Neurosurg Focus. 2003;15:E11. doi: 10.3171/foc.2003.15.3.11. [DOI] [PubMed] [Google Scholar]
- 18.Schick U, Döhnert J, Richter A, König A, Vitzthum HE. Microendoscopic lumbar discectomy versus open surgery: An intraoperative EMG study. Eur Spine J. 2002;11:20–6. doi: 10.1007/s005860100315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shin DA, Kim KN, Shin HC, Yoon H. The efficacy of Microendoscopic discectomy in reducing iatrogenic muscle injury. J Neurosurg Spine. 2008;8:39–43. doi: 10.3171/SPI-08/01/039. [DOI] [PubMed] [Google Scholar]
- 20.Kotil K, Tunckale T, Tatar Z, Koldas M, Kural A, Bilge T. Serum creatine phosphokinase activity and histological changes in the multifidus muscle: A prospective randomized controlled comparative study of discectomy with or without retraction. J Neurosurg Spine. 2007;6:121–5. doi: 10.3171/spi.2007.6.2.121. [DOI] [PubMed] [Google Scholar]
- 21.Harrington JF, French P. Open versus minimally invasive lumbar microdiscectomy: Comparison of operative times, length of hospital stay, narcotic use and complications. Minim Invasive Neurosurg. 2008;51:30–5. doi: 10.1055/s-2007-1004543. [DOI] [PubMed] [Google Scholar]
- 22.Yeung AT, Yeung CA. Minimally invasive techniques for the management of lumbar disc herniation. Orthop Clin North Am. 2007;38:363–72. doi: 10.1016/j.ocl.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 23.Mayer HM, Brock M. Percutaneous endoscopic discectomy: Surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216–25. doi: 10.3171/jns.1993.78.2.0216. [DOI] [PubMed] [Google Scholar]
- 24.Ditsworth DA. Endoscopic transforaminal lumbar discectomy and reconfiguration: A postero-lateral approach into the spinal canal. SurgNeurol. 1998;49:588–98. doi: 10.1016/s0090-3019(98)00004-4. [DOI] [PubMed] [Google Scholar]
- 25.Ranjan A, Lath R. Microendoscopic discectomy for prolapsed lumbar intervertebral disc. Neurol India. 2006;54:190–4. [PubMed] [Google Scholar]
- 26.Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus open discectomy for lumbar disc herniation: A prospective randomised study. J Orthop Surg (Hong Kong) 2011;19:30–4. doi: 10.1177/230949901101900107. [DOI] [PubMed] [Google Scholar]
- 27.Jhala A, Mistry M. Endoscopic lumbar discectomy: Experience of first 100 cases. Indian J Orthop. 2010;44:184–90. doi: 10.4103/0019-5413.62051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaushal M, Sen R. Posterior endoscopic discectomy: Results in 300 patients. Indian J Orthop. 2012;46:81–5. doi: 10.4103/0019-5413.91640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith L, Brown JE. Treatment of lumbar intervertebral disc lesion by direct injection of chymopapain. J Bone Joint Surg Br. 1967;49:502–19. [PubMed] [Google Scholar]
- 30.Hijikata S. Percutaneous nucleotomy. A new concept technique and 12 years’ experience. Clin Orthop Relat Res. 1989;238:9–23. [PubMed] [Google Scholar]
- 31.Onik G, Helms CA, Ginsberg L, Hoaglund FT, Morris J. Percutaneous lumbar diskectomy using a new aspiration probe. Am J Roentgenol. 1985;144:1137–40. doi: 10.2214/ajr.144.6.1137. [DOI] [PubMed] [Google Scholar]
- 32.Choy DS, Ascher PW, Ranu HS, Saddekni S, Alkaitis D, Liebler W, et al. Percutaneous laser disc decompressions: A new therapeutic modality. Spine (Phila Pa 1976) 1992;17:949–56. doi: 10.1097/00007632-199208000-00014. [DOI] [PubMed] [Google Scholar]
- 33.Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RH, Tan WF, et al. Tubular diskectomy vs conventional microdiscectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery. 2011;69:135–44. doi: 10.1227/NEU.0b013e318214a98c. [DOI] [PubMed] [Google Scholar]
- 34.Härtl R. Comment to the article: “Tubular diskectomy vs conventional microdiskectomy for sciatica: A randomized controlled trial”. Minim Invasive Neurosurg. 2010;53:95–6. doi: 10.1055/s-0030-1263198. [DOI] [PubMed] [Google Scholar]
- 35.Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: Results of a randomized controlled trial. Neurosurgery. 2007;61:545–9. doi: 10.1227/01.NEU.0000290901.00320.F5. [DOI] [PubMed] [Google Scholar]
- 36.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine (PhilaPa 1976) 2008;33:931–9. doi: 10.1097/BRS.0b013e31816c8af7. [DOI] [PubMed] [Google Scholar]
- 37.Wu X, Zhuang S, Mao Z, Chen H. Microendoscopic discectomy for lumbar disc herniation: Surgical technique and outcome in 873 consecutive cases. Spine (Phila Pa 1976) 2006;31:2689–94. doi: 10.1097/01.brs.0000244615.43199.07. [DOI] [PubMed] [Google Scholar]
- 38.Ebling U, Reichenberg W, Reulen HJ. Results of microsurgical lumbar discectomy. Review on 485 patients. ActaNeurochir. 1986;81:45–52. doi: 10.1007/BF01456264. [DOI] [PubMed] [Google Scholar]
- 39.Caspar W, Campbell B, Barbier DD, Kretschmmer R, Gotfried Y. The Caspar microsurgical discectomy and comparison with a conventional standard lumbar disc procedure. Neurosurgery. 1991;28:78–87. doi: 10.1097/00006123-199101000-00013. [DOI] [PubMed] [Google Scholar]
- 40.Pappas CT, Harrington T, Sonntag VK. Outcome analysis in 654 surgical treated lumbar disc herniations. Neurosurgery. 1992;30:862–6. doi: 10.1227/00006123-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Chen Z, Zhao J, Liu A, Yuan J, Li Z. Surgical treatment of recurrent lumbar disc herniation by transforaminal lumbar interbody fusion. Int Orthop. 2009;33:197–201. doi: 10.1007/s00264-008-0531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tullberg T, Isacson J, Weidenhielm L. Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Result of a one-year randomized study. Spine (Phila Pa 1976) 1993;18:24–7. doi: 10.1097/00007632-199301000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Perez-Cruet MJ, Foley KT, Isaacs RE, Rice-Wyllie L, Wellington R, Smith MM, et al. Microendoscopic Lumbar Discectomy: Technical Note. Neurosurgery. 2002;51:S129–36. [PubMed] [Google Scholar]
- 44.Nakagawa H, Kamimura M, Uchiyama S, Takahara K, Itsubo T, Miyasaka T. Microendoscopic discectomy (MED) for lumbar disc prolapse. J Clin Neurosci. 2003;10:231–5. doi: 10.1016/s0967-5868(02)00337-5. [DOI] [PubMed] [Google Scholar]
- 45.Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RH, Peul WC. Tubular diskectomy vs conventional microdiskectomy for sciatica: A randomized controlled trial. JAMA. 2009;302:149–58. doi: 10.1001/jama.2009.972. [DOI] [PubMed] [Google Scholar]
- 46.Muramatsu K, Hachiya Y, Morita C. Postoperative magnetic resonance imaging of lumbar disc herniation: Comparison of microendoscopic discectomy and Love's method. Spine (Phila Pa 1976) 2001;26:1599–605. doi: 10.1097/00007632-200107150-00022. [DOI] [PubMed] [Google Scholar]
- 47.Schizas C, Tsiridis E, Saksena J. Microendoscopic discectomy compared with standard microsurgical discectomy for treatment of uncontained or large contained disc herniations. Neurosurgery. 2005;57(4 Suppl):357–60. doi: 10.1227/01.neu.00000176650.71193.f5. [DOI] [PubMed] [Google Scholar]
- 48.Bookwalter JW, III, Busch MD, Nicely D. Ambulatory surgery is safe and effective in radicular disc disease. Spine (Phila Pa 1976) 1994;19:526–30. doi: 10.1097/00007632-199403000-00006. [DOI] [PubMed] [Google Scholar]
- 49.Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010;19:443–50. doi: 10.1007/s00586-010-1290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nowitzke A. Assessment of the learning curve for Lumbar Microendoscopic Discectomy. Neurosurgery. 2005;56:755–62. doi: 10.1227/01.neu.0000156470.79032.7b. [DOI] [PubMed] [Google Scholar]


