Abstract
Oral diseases continue to be a major health problem world-wide. Oral health is integral to general well-being and relates to the quality-of-life that extends beyond the functions of the craniofacial complex. The standard Western medicine has had only limited success in the prevention of periodontal disease and in the treatment of a variety of oral diseases. Hence, the search for alternative products continues and natural phytochemicals isolated from plants used in traditional medicine are considered to be good alternatives to synthetic chemicals. The botanicals in the Ayurvedic material medica have been proven to be safe and effective, through several hundred to several thousand years of use. The exploration of botanicals used in traditional medicine may lead to the development of novel preventive or therapeutic strategies for oral health. The present scientific evidence based review is focused on the possible role of Ayurveda in the management of various orofacial disorders.
Keywords: Ayurveda, dentistry, oral health, orofacial disorders
INTRODUCTION
Oral diseases continue to be a major health problem world-wide.[1] Dental caries and periodontal diseases are among the most important global oral health problems, although other conditions like oral and pharyngeal cancers and oral tissue lesions are also of significant concern.[2] Oral health is integral to general well-being and relates to the quality-of-life that extends beyond the functions of the craniofacial complex. The link between oral diseases and the activities of microbial species that form part of the micro biota of the oral cavity is well-established.[3] The global need for alternative prevention and treatment options and products for oral diseases that are safe, effective and economical comes from the rise in disease incidence (particularly in developing countries), increased resistance by pathogenic bacteria to currently used antibiotics and chemotherapeutics, opportunistic infections in immunocompromised individuals and financial considerations in developing countries.[4,5] Despite several chemical agents being commercially available, these can alter oral micro biota and have undesirable side-effects such as vomiting, diarrhea and tooth staining.[6,7] Furthermore, the standard Western medicine has had only limited success in the prevention of periodontal disease and in the treatment of a variety of oral diseases. Hence, the search for alternative products continues and natural phytochemicals isolated from plants used in traditional medicine are considered as good alternatives to synthetic chemicals.[8]
Ayurveda is the ancient Indian system of health-care and longevity. It involves a holistic view of man, his health and illness. Ayurvedic treatment is aimed at patient as an organic whole and treatment consists of salubrious use of drugs, diets and certain practices.[9] Currently, Ayurveda is widely practiced in the Hindustan peninsula (India and the neighboring countries) and in recent years, has attracted much attention in economically developed countries such as those in Europe and in the United States and Japan.[10] There are approximately 1250 Indian medicinal plants[11] that are used in formulating beneficial measures according to Ayurvedic or other ethnicity. This 5000-year-old system of medicine recommends treatments with specific herbs and minerals to cure various diseases. The botanicals in the Ayurvedic material medica have been proven to be safe and effective, through several hundred to several thousand years of use.[12] The exploration of botanicals used in traditional medicine, may lead to the development of novel preventive or therapeutic strategies for oral health.[13] As most of the oral diseases are due to bacterial infections and it has been well-documented that medicinal plants confer considerable anti-bacterial activity against various microorganisms including bacteria's responsible for dental caries.[14]
The dentist needs to be more informed regarding the use, safety and effectiveness of the various traditional medicines and over-the-counter products. As this is hardly explored part for the field of dentistry, there is a need for integration of professional dental treatment modalities and complementary alternative medical (CAM) systems to provide the best and unique from each system to patients as a complementary therapy and an alternative choice of treatment.[15] Considering the importance of various traditional or CAM systems, the present scientific evidence based review of literature is focused on the possible role of Ayurveda in the management of various orofacial disorders.
MATERIALS AND METHODS
In this review of the literature, we only considered those studies that include individual plants or mixtures of plants consistent with the philosophy of Ayurveda. The databases searched for the current review were Medline, Natural Products Alert Database, and related databases, such as AYUSH Research Portal, National Library of Ayurveda Medicine, Systematic Reviews in Ayurveda, Ayurveda Database, Web of Science, Indus Medicus and Google Scholar; by consulting existing bibliographies; by using both forward and backward reference chaining techniques; and by tracking recent activities in the field of Ayurveda, which is primarily concerned with prevention and management of orofacial disorders. In addition, we also collected literature on traditional medicine and searched some Indian journals not included in Medline. References that were primarily anecdotal or that were only peripherally related to the topic were excluded.
Ayurveda and the concept of health
Sushruta Samhita, the surgical compendium of Ayurveda, defines health as “the equilibrium of the three biological humors (doshas), the seven body tissues (dhatus), proper digestion and a state of pleasure or happiness of the soul, senses and the mind.”[16]
A balance among the three doshas is necessary for health. Together, the three doshas govern all metabolic activities. When their actions in our mind-body constitution are balanced, we experience psychological and physical wellness. When they go slightly out of balance, we may feel uneasy. When they are more obviously unbalanced, symptoms of sickness can be observed and experienced.[17,18]
Ayurveda and orofacial diseases
According to the Shalyatantra and Shalakyatantra (one of the branches of Ayurveda), 65 varieties of oral diseases can arise in seven anatomic locations-eight on the lips, 15 on the alveolar margin, eight in connection with the teeth, five on the tongue, nine on the palate, 17 in the oropharynx and three in a generalized form.[19]
For the treatment of these diseases Ayurveda advocates procedures such as oral cleansing, extractions, excisions, flap surgeries etc., Along with the treatment of orofacial diseases, Ayurveda recommends some daily use therapeutic procedures for the prevention of and maintenance of oral health. These include: Dant Dhavani (Brushing), Jivha Lekhana (Tongue scrapping) and Gandoosha (gargling) or oil pulling and tissue regeneration therapies. Some of the scientifically proven beneficial effects of these procedures are described below:
Dant Dhavani (brushing): Avurveda recommends chewing sticks in the morning as well as after every meal to prevent diseases. Ayurveda insists on the use of herbal brushes, approximately nine inches long and the thickness of one's little finger. These herb sticks should be either “kashaya” (astringent), “katu” (acrid) or “tikta” (bitter) in taste. The method of use is to crush one end, chew it and eat it slowly.[20] The neem (margosa or Azadirachta indica) is a famous herbal chewing stick. Fresh stems of liquorice (Glycyrrhiza glabra), black catechu or the cutch tree (Acacia Catechu Linn.),[21] Arjuna tree (Termmalia arjuna), fever nut (Caesalipinia bouduc) and milkweed plant (Calotropis procera)[22] can also be used for brushing. Chewing on these stems is believed to cause attrition and leveling of biting surfaces, facilitate salivary secretion and possibly, help in plaque control while some stems have an anti-bacterial action.[22] Present-day research has shown that all the chewing sticks described in ancient Avurveda texts (Circa 200 BC) have medicinal and anti-cariogenic properties.[23]
Jivha Lekhana (tongue scrapping): It is ideal to use gold, silver, copper, stainless steel for the scrapping of the tongue. Tongue scrapping stimulates the reflex points of the tongue. Removes bad odor (halitosis). Improves the sense of taste, stimulate the secretion of digestive enzymes. Removes millions of bacteria growth (approximately 500 varieties) Clinical evidence also shows that use of tongue scrapers on a regular basis, has a significant Improvement on eliminating anaerobic bacteria and decreases bad odor.[24]
Gandusha (gargling) or oil pulling: Oil pulling is an ancient Ayurveda procedure that involves swishing oil in the mouth for oral and systemic health benefits. It is mentioned in the Avurvedic text Charaka Samhita where it is called Kavala or Gandusha and is claimed to cure about 30 systemic diseases ranging from headache, migraine to diabetes and asthma. Oil pulling has been used extensively as a traditional Indian folk remedy for many years to prevent decay, oral malodor, bleeding gums, dryness of throat, cracked lips and for strengthening teeth, gums and the jaw.[25,26] Oil pulling therapy can be done using oils like sunflower oil or sesame oil.[27] Oil pulling therapy is very effective against plaque induced gingivitis both in the clinical and microbiological assessment.[28,29]
Tissue regeneration therapies: In Avurveda, the well-known herb, Amla (Phyllanthus emblica) is considered a general rebuilder of oral health. Amla works well as a mouth rinse as a decoction. One to two grams per day can be taken orally in capsules for the long-term benefit to the teeth and gums. Amla supports the healing and development of connective tissue when taken internally.[30] Regular use of Bilberry and hawthorn berry fruits stabilize collagen and strengthens the gum tissue.[31] Liquorice root promotes anti-cavity action, reduces plaque and has an anti-bacterial effect.[30] Herbs such as yellow dock root, alfalfa leaf, cinnamon bark and turmeric root are taken internally to strengthen Astidharu, for example, the skeleton and the joints, have proven to be good for long term health of teeth.[31]
Ayurvedic herbs with various oral health related properties
Ayurvedic medications have stood the test of time and since time immemorial been used for various ailments. Recently, there is renewed interest in use of various Ayurvedic drugs for oral and dental health. Various plants and natural products have been used for their pharmacological applications viz. antiulcer genic, wound healing, anti-inflammatory, antimicrobial, antioxidant properties etc.[31,32,33] In this section, we have tried to review the recent studies undertaken to use of natural products for oral diseases and also have looked into the multitude prospects and perspectives of Ayurveda in the management of orofacial diseases. Various clinical implications of commonly used Ayurvedic herbs in the management of orofacial diseases are summarized in Table 1.
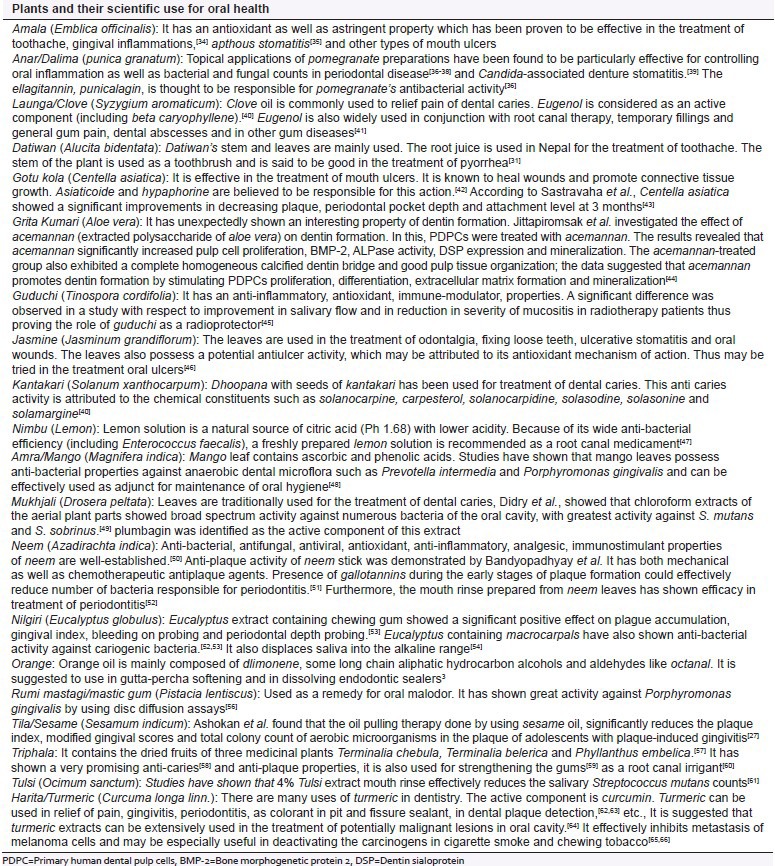
Table 1.
Plants with their oral health related indications
CONCLUSION
Oral diseases are one of the most important problems in public health and are on the rise in developing countries. Most of the oral diseases are caused due to the bacterial infections. The anti-bacterial activity of medicinal plants are due to the presence of potential bioactive compounds, which help to reduce bacterial load in the oral cavity and thus prevent the formation of plaque, dental caries and ulcers. Use of indigenous plants in oral health and hygiene has a long history in different parts of the world. Therefore, this knowledge is likely to vanish soon as many of these ethno-phytotherapeutic remedies are followed only by a few in rural areas. New generation is ignorant of this traditional knowledge. Because of younger generation's lack of knowledge on the identification, collection, preservation and processing of the plant species for medicinal use it is therefore very crucial to conserve these ethno-cultural practices before they are lost definitively.[66]
In this paper, an attempt has been made to review various herbal plants mentioned in Ayurveda that can be used as an adjunct for the maintenance of oral health. The literature showed that there are numerous Ayurvedic drugs, which can be used in prevention as well as management of oral diseases. Many Ayurvedic herbal plants, which are reviewed, possess antimicrobial, anti-inflammatory, analgesic, antiulcer genic activities when screened according to the modern parameters. However, among them very negligible amount of herbals extracts are used in clinical practice and the rest of others are not practiced because of their unknown toxicological effects. The clinical studies should be encouraged to assess the efficacy as well as toxicity of herbal drugs.
The traditional knowledge of Ayurveda should be integrated with the modern dentistry. For this, the active principles of plants should be incorporated into modern oral health-care practices and dentists should be encouraged to use natural remedies in various oral health treatments. This will make dentistry much safer, affordable and more accessible for the lower socio-economic groups in society.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83:661–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Petersen PE. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century: The approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2003;31(Suppl 1):3–23. doi: 10.1046/j..2003.com122.x. [DOI] [PubMed] [Google Scholar]
- 3.Jenkinson HF, Lamont RJ. Oral microbial communities in sickness and in health. Trends Microbiol. 2005;13:589–95. doi: 10.1016/j.tim.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Tichy J, Novak J. Extraction, assay, and analysis of antimicrobials from plants with activity against dental pathogens (Streptococcus sp. ) J Altern Complement Med. 1998;4:39–45. doi: 10.1089/acm.1998.4.1-39. [DOI] [PubMed] [Google Scholar]
- 5.Badria FA, Zidan OA. Natural products for dental caries prevention. J Med Food. 2004;7:381–4. doi: 10.1089/jmf.2004.7.381. [DOI] [PubMed] [Google Scholar]
- 6.Park KM, You JS, Lee HY, Baek NI, Hwang JK. Kuwanon G: An antibacterial agent from the root bark of Morus alba against oral pathogens. J Ethnopharmacol. 2003;84:181–5. doi: 10.1016/s0378-8741(02)00318-5. [DOI] [PubMed] [Google Scholar]
- 7.Chung JY, Choo JH, Lee MH, Hwang JK. Anticariogenic activity of macelignan isolated from Myristica fragrans (nutmeg) against Streptococcus mutans. Phytomedicine. 2006;13:261–6. doi: 10.1016/j.phymed.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Prabu GR, Gnanamani A, Sadulla S. Guaijaverin: A plant flavonoid as potential antiplaque agent against Streptococcus mutans. J Appl Microbiol. 2006;101:487–95. doi: 10.1111/j.1365-2672.2006.02912.x. [DOI] [PubMed] [Google Scholar]
- 9.Sharma S. Ayurveda and health. In: Sharma PS, editor. Realms of Ayurveda. 1st ed. New Delhi: Arnold-Heineman Publishers; 1979. pp. 117–34. [Google Scholar]
- 10.Hartzell JF, Zysk KG. Health, science, and the spirit: Veda and Ayurveda in the Western world. J Altern Complement Med. 1995;1:297–301. [Google Scholar]
- 11.Chatterjee A, Pakrashi S. History of Indian medicine. In: Chatterjee A, editor. The Treatise on Indian Medicinal Plants. 1st ed. Vol. 1. New Delhi: National Inst. Science Communication and Information Resources; 1991. pp. 221–4. [Google Scholar]
- 12.Kosta S, Tiwari A. A fusion of ancient medicinal plants with modern conventional therapies on its multifaceted anti diabetic properties. Pharmacol. 2009;1:64–77. [Google Scholar]
- 13.Borchers AT. Traditional Asian medicine and oral health. J Tradit Med. 2004;21:17–26. [Google Scholar]
- 14.Kelmanson JE, Jäger AK, van Staden J. Zulu medicinal plants with antibacterial activity. J Ethnopharmacol. 2000;69:241–6. doi: 10.1016/s0378-8741(99)00147-6. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein BH. Unconventional dentistry: Part I. Introduction. J Can Dent Assoc. 2000;66:323–6. [PubMed] [Google Scholar]
- 16.Samhita S. 1st ed. Ch 21, Stanza 9. New Delhi, India: Motilal Banarasidas Publishers; 1983. Sutrasthanam; pp. 335–6. [Google Scholar]
- 17.Sharma PV. In: Charaka Samhita: Sutrasthanam. 23rd ed. Ch. 20, Stanzas 11-13. Sharma P, editor. Varanasi, India: Chaukambha Orientalia; 1981. pp. 112–4. [Google Scholar]
- 18.Sharma PV, Sharma P. Charaka Samhita: Vimanasthanam. 23rd ed. Ch 5. Varanasi, India: Chaukambha Orientalia; 1981. pp. 226–40. [Google Scholar]
- 19.Chakravorty RC. Head and neck diseases in an ancient Indian surgical text (The Sushruta-samhita) Med Hist. 1971;15:393–6. doi: 10.1017/s002572730001694x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Telles S, Naveen KV, Balkrishna A. Use of Ayurveda in promoting dental health and preventing dental caries. Indian J Dent Res. 2009;20:246. doi: 10.4103/0970-9290.52877. [DOI] [PubMed] [Google Scholar]
- 21.Athavale VB. Dant rogas. In: Athavale VB, editor. Dentistry in Ayurveda. 1st ed. New Delhi: Chaukhamba Sanskrit Pratishthan; 1999. pp. 7–11. [Google Scholar]
- 22.Naik GH, Priyadarsini KI, Satav JG, Banavalikar MM, Sohoni DP, Biyani MK, et al. Comparative antioxidant activity of individual herbal components used in Ayurvedic medicine. Phytochemistry. 2003;63:97–104. doi: 10.1016/s0031-9422(02)00754-9. [DOI] [PubMed] [Google Scholar]
- 23.Venugopal T, Kulkarni VS, Nerurker RA, Damle SG, Patnekar PN. Epidemiological study of dental caries. Indian J Pediatr. 1998;65:883–9. doi: 10.1007/BF02831355. [DOI] [PubMed] [Google Scholar]
- 24.Kadam A, Prasad BS, Bagadia D, Hiremath VR. Effect of Ayurvedic herbs on control of plaque and gingivitis: A randomized controlled trial. Ayu. 2011;32:532–5. doi: 10.4103/0974-8520.96128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bethesda M. A closer look at Ayurvedic medicine. Focus on complementary and alternative medicine. National Center for Complementary and Alternative Medicine (NCCAM). US National Institutes of Health (NIH) 2006;12:123–39. [Google Scholar]
- 26.Hebbar A, Keuskar V, Shetti A. Oil pulling: Unraveling the path to mystic cure. J Int Oral Health. 2010;2:11–4. [Google Scholar]
- 27.Asokan S. Oil pulling therapy. Indian J Dent Res. 2008;19:169. doi: 10.4103/0970-9290.40476. [DOI] [PubMed] [Google Scholar]
- 28.Amith HV, Ankola AV, Nagesh L. Effect of oil pulling on plaque and gingivitis. J Oral Health Community Dent. 2007;1:12–8. [Google Scholar]
- 29.Asokan S, Emmadi P, Chamundeswari R. Effect of oil pulling on plaque induced gingivitis: A randomized, controlled, triple-blind study. Indian J Dent Res. 2009;20:47–51. doi: 10.4103/0970-9290.49067. [DOI] [PubMed] [Google Scholar]
- 30.Singh A, Purohit B. Tooth brushing, oil pulling and tissue regeneration: A review of holistic approaches to oral health. J Ayurveda Integr Med. 2011;2:64–8. doi: 10.4103/0975-9476.82525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amruthesh S. Dentistry and Ayurveda-V: An evidence based approach. Indian J Dent Res. 2011;2:3–9. [Google Scholar]
- 32.Cowan MM. Plant products as antimicrobial agents. Clin Microbiol Rev. 1999;12:564–82. doi: 10.1128/cmr.12.4.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahmad I, Beg AZ. Antimicrobial and phytochemical studies on 45 Indian medicinal plants against multi-drug resistant human pathogens. J Ethnopharmacol. 2001;74:113–23. doi: 10.1016/s0378-8741(00)00335-4. [DOI] [PubMed] [Google Scholar]
- 34.Treadway L. Amla traditional food and medicine. Herbalgram. 1994;31:26. [Google Scholar]
- 35.Nadkarni KM, Nadkarni AK. Vegetable kingdom. In: Nadkarni K, editor. Indian Materia Medica with Ayurvedic, Unani-Tibbi, Siddha, Allopathic, Homeopathic, Naturopathic and Home remedies. 3rd ed. Vol. 1. Bombay, India: Popular Prakashan Private Ltd; 1999. p. 46. [Google Scholar]
- 36.Menezes SM, Cordeiro LN, Viana GS. Punica granatum (pomegranate) extract is active against dental plaque. J Herb Pharmacother. 2006;6:79–92. [PubMed] [Google Scholar]
- 37.Vasconcelos LC, Sampaio FC, Sampaio MC, Pereira Mdo S, Higino JS, Peixoto MH. Minimum inhibitory concentration of adherence of Punica granatum Linn (pomegranate) gel against S. mutans, S. mitis and C. albicans. Braz Dent J. 2006;17:223–7. doi: 10.1590/s0103-64402006000300009. [DOI] [PubMed] [Google Scholar]
- 38.Jurenka JS. Therapeutic applications of pomegranate (Punica granatum L.): A review. Altern Med Rev. 2008;13:128–44. [PubMed] [Google Scholar]
- 39.Vasconcelos LC, Sampaio MC, Sampaio FC, Higino JS. Use of Punica granatum as an antifungal agent against candidosis associated with denture stomatitis. Mycoses. 2003;46:192–6. doi: 10.1046/j.1439-0507.2003.00884.x. [DOI] [PubMed] [Google Scholar]
- 40.Amruthesh S. Dentistry and Ayurveda-IV: Classification and management of common oral diseases. Indian J Dent Res. 2008;19:52–61. doi: 10.4103/0970-9290.38933. [DOI] [PubMed] [Google Scholar]
- 41.Sinha AR, Bajaj VK, Singh P, Shekhawat S, Singh K. Phytochemical estimation and antimicrobial activity of aqueous and methanolic extract of Ocimum sanctum L. J Nat Prod Plant Resour. 2013;3:51–8. [Google Scholar]
- 42.Maquart FX, Bellon G, Gillery P, Wegrowski Y, Borel JP. Stimulation of collagen synthesis in fibroblast cultures by a triterpene extracted from Centella asiatica. Connect Tissue Res. 1990;24:107–20. doi: 10.3109/03008209009152427. [DOI] [PubMed] [Google Scholar]
- 43.Sastravaha G, Yotnuengnit P, Booncong P, Sangtherapitikul P. Adjunctive periodontal treatment with Centella asiatica and Punica granatum extracts. A preliminary study. J Int Acad Periodontol. 2003;5:106–15. [PubMed] [Google Scholar]
- 44.Jittapiromsak N, Sahawat D, Banlunara W, Sangvanich P, Thunyakitpisal P. Acemannan, an extracted product from Aloe vera, stimulates dental pulp cell proliferation, differentiation, mineralization, and dentin formation. Tissue Eng Part A. 2010;16:1997–2006. doi: 10.1089/ten.TEA.2009.0593. [DOI] [PubMed] [Google Scholar]
- 45.Amruthesh S, Mubeen, Pramod KP, Venkatesh BA, Ramesh C. Evaluation of radio protective effects of Tinospor acordifolia in patients on radiotherapy for squamous cell carcinoma of head and neck-Pilot study. Int J Contemp Dent. 2010;1:24–30. [Google Scholar]
- 46.Umamaheswari M, Asokkumar K, Rathidevi R, Sivashanmugam AT, Subhadradevi V, Ravi TK. Antiulcer and in vitro antioxidant activities of Jasminum grandiflorum L. J Ethnopharmacol. 2007;110:464–70. doi: 10.1016/j.jep.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 47.Abuzied ST, Eissa SA. Comparative study on antibacterial activities of two natural plants versus three different intra canal medicaments (Online article) [Last accessed on 2012 Feb 12]. Available from: http://www.kau.edu.sa/Files/165/Researches/19240_Comparative%20Study%20On.pdf .
- 48.Bairy I, Reeja S, Siddharth, Rao PS, Bhat M, Shivananda PG. Evaluation of antibacterial activity of Mangifera indica on anaerobic dental microglora based on in vivo studies. Indian J Pathol Microbiol. 2002;45:307–10. [PubMed] [Google Scholar]
- 49.Didry N, Dubreuil L, Trotin F, Pinkas M. Antimicrobial activity of aerial parts of Drosera peltata Smith on oral bacteria. J Ethnopharmacol. 1998;60:91–6. doi: 10.1016/s0378-8741(97)00129-3. [DOI] [PubMed] [Google Scholar]
- 50.Bandyopadhyay U, Biswas K, Chatterjee R, Bandyopadhyay D, Chattopadhyay I, Ganguly CK, et al. Gastroprotective effect of Neem (Azadirachta indica) bark extract: Possible involvement of H(+)-K(+)-ATPase inhibition and scavenging of hydroxyl radical. Life Sci. 2002;71:2845–65. doi: 10.1016/s0024-3205(02)02143-4. [DOI] [PubMed] [Google Scholar]
- 51.Wolinsky LE, Mania S, Nachnani S, Ling S. The inhibiting effect of aqueous Azadirachta indica (Neem) extract upon bacterial properties influencing in vitro plaque formation. J Dent Res. 1996;75:816–22. doi: 10.1177/00220345960750021301. [DOI] [PubMed] [Google Scholar]
- 52.Botelho MA, dos Santos RA. Efficacy of a mouth rinse based on leaves of the neem tree (Azadirachta indica) in the treatment of patients with chronic gingivitis: A double-blind, randomized, controlled trial. J Med Plants Res. 2008;2:341–6. [Google Scholar]
- 53.Nagata H, Inagaki Y, Tanaka M, Ojima M, Kataoka K, Kuboniwa M, et al. Effect of eucalyptus extract chewing gum on periodontal health: A double-masked, randomized trial. J Periodontol. 2008;79:1378–85. doi: 10.1902/jop.2008.070622. [DOI] [PubMed] [Google Scholar]
- 54.Pistorius A, Willershausen B, Steinmeier EM, Kreislert M. Efficacy of subgingival irrigation using herbal extracts on gingival inflammation. J Periodontol. 2003;74:616–22. doi: 10.1902/jop.2003.74.5.616. [DOI] [PubMed] [Google Scholar]
- 55.Bauer K, Garbe D, Surburg H. 4th ed. Weinheim: Wiley VCH; 2001. Common Fragrance and Flavor Materials; p. 189. [Google Scholar]
- 56.Sterer N. Antimicrobial effect of mastic gum methanolic extract against Porphyromonas gingivalis. J Med Food. 2006;9:290–2. doi: 10.1089/jmf.2006.9.290. [DOI] [PubMed] [Google Scholar]
- 57.Wohlmuth H. Triphala-A short review. Inf Res Bot Med. 2007;16:2. [Google Scholar]
- 58.Tandon S, Gupta K, Rao S, Malagi KJ. Effect of Triphala mouthwash on the caries status. Int J Ayurveda Res. 2010;1:93–9. doi: 10.4103/0974-7788.64413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Date BB, Kulkarni PH. Assessment of Rasa danti in various oral disorders. Ayurveda Res Pap. 1995;2:175–97. [Google Scholar]
- 60.Biradar YS, Jagatap S, Khandelwal KR, Singhania SS. Exploring of antimicrobial activity of triphala mashi-An Ayurvedic formulation. Evid Based Complement Alternat Med. 2008;5:107–13. doi: 10.1093/ecam/nem002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Agarwal P, Nagesh L. Comparative evaluation of efficacy of 0.2% Chlorhexidine, Listerine and Tulsi extract mouth rinses on salivary Streptococcus mutans count of high school children – RCT. Contemp Clin Trials. 2011;32:802–8. doi: 10.1016/j.cct.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 62.Chaturvedi TP. Uses of turmeric in dentistry: An update. Indian J Dent Res. 2009;20:107–9. doi: 10.4103/0970-9290.49065. [DOI] [PubMed] [Google Scholar]
- 63.Bhowmik D, Chiranjib B, Sampath Kumar KP, Chandira M, Jayakar B. Turmeric: A herbal and traditional medicine. Arch Appl Sci Res. 2009;1:86–108. [Google Scholar]
- 64.Kawamori T, Lubet R, Steele VE, Kelloff GJ, Kaskey RB, Rao CV, et al. Chemopreventive effect of curcumin, a naturally occurring anti-inflammatory agent, during the promotion/progression stages of colon cancer. Cancer Res. 1999;59:597–601. [PubMed] [Google Scholar]
- 65.Mehta K, Pantazis P, McQueen T, Aggarwal BB. Antiproliferative effect of curcumin (diferuloylmethane) against human breast tumor cell lines. Anticancer Drugs. 1997;8:470–81. doi: 10.1097/00001813-199706000-00010. [DOI] [PubMed] [Google Scholar]
- 66.Menon LG, Kuttan R, Kuttan G. Anti-metastatic activity of curcumin and catechin. Cancer Lett. 1999;141:159–65. doi: 10.1016/s0304-3835(99)00098-1. [DOI] [PubMed] [Google Scholar]


