Abstract
Aims:
The purpose of this study was to demonstrate the factors influencing nurse-patient communication in cancer care in Iran.
Materials and Methods:
This study was conducted with a qualitative conventional content analysis approach in oncology wards of hospitals in Tabriz. Data was collected through purposive sampling by semi-structured deep interviews with nine patients, three family members and five nurses and analyzed simultaneously. Robustness of data analysis was evaluated by the participants and external control.
Results:
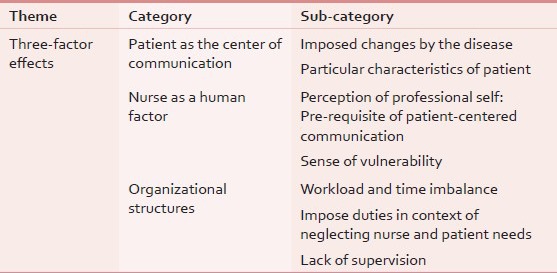
The main theme of the research emerged as “three-factor effects” that demonstrates all the factors related to the patient, nurse, and the organization and includes three categories of “Patient as the center of communication”, “Nurse as a human factor”, and “Organizational structures”. The first category consists of two sub-categories of “Imposed changes by the disease” and the “patient's particular characteristics”. The second category includes sub-categories of “sense of vulnerability” and “perception of professional self: Pre-requisite of patient-centered communication”. The third category consists of the sub-categories of “workload and time imbalance”, “lack of supervision”, and “impose duties in context of neglecting nurse and patient needs”. Characteristics of the patients, nurses, and care environment seemed to be the influential factors on the communication.
Conclusions:
In order to communicate with cancer patients effectively, changes in philosophy and culture of the care environment are essential. Nurses must receive proper trainings which meet their needs and which focus on holistic and patient-centered approach.
Keywords: Cancer, Effective factors, Nurse-patient communication, Oncology
INTRODUCTION
Relationship with the patient is the major component of nursing care. In fact, along with other organizational factors, it would help to build a positive relationship between nurse and patient. Furthermore, it helps in providing quality nursing care. Researches on nursing care often complain about poor relationship,[1,2,3,4,5] and patients often feel health care personnel do not meet all their communicative needs. According to the Research Center for Quality Care, 10.8% of patients believe that caregivers sometimes or never listened to them carefully, do not explain things clearly, they do not respect what patients say, and do not spend enough time with them.[6] Because of asking questions or expressing their concerns, some patients have to face with inappropriate behavioral reactions of caregivers. Gaps in communication between caregivers and patients result in decreased quality of care, poor outcomes, and dissatisfaction with health care system.[7]
Nurses play a major role in cancer care, because cancer nursing not only focuses on the biological and medical aspects of care, but also on the emotional aspects. Therefore, such care requires a comprehensive understanding of the patient.[8] As cancer care is affected by factors related to the patient and organizational factors,[9] this leads to many communicative problems experienced by nurses that consequently leads to excluding patients from sharing their concerns with them.[10] In other words, the roles of patients and caregivers in influencing communication processes are equally important.[11] Moreover, factors such as the competence of nurses in communication skills, training programs to improve the nurse-patient relationship, task-oriented view, insufficient skills in providing psychological aspects of care for patients who are living in difficult emotional situations, seeking information by patients and having a role in caring themselves and that they do not want to talk about the disease and their feelings in such cases have been mentioned.[12]
Studies show that nurses often fear from situations when patients express emotions that they are unable to manage. Therefore, through changing discussions, they prevent patients from expressing their concerns. In most cases, the emotional issues are not being selected as the main topic; instead, they tend to provide information and practical care. In fact, these barriers lead to inadequate emotional support for patients.[5,12,13] Fakhr-Movahedi et al. studied the nurse - patient relationship in Iran and showed that factors such as organizational factors, culture and tradition, expectations from nurses, and heavy workloads can limit the time allocated to communicate with patients and reduce the effectiveness of communication.[4]
In addition, although nurses’ communication behavior, including friendly personality, kindness, quick response, and timely attending to the needs of patients, allocating sufficient time to provide care could improve communication with the patient, heavy workload and shortage of nurses, are common problems that are prevalent in the training hospitals of Iran, which could potentially affect this behavior.[14] On one hand, it should be noted that facilities for palliative care in cancer in Iran are currently limited to only a few centers in major cities, and as a result, referring patients with a variety of needs and concerns increases the workload in oncology units.[15] On the other hand, the number of nurses in the country has not reached the standard that it can influence the quality of nursing care and effectiveness of communication with patients.[16] Cancer care system is based on the biomedical model and the unwillingness to allocate authority to the patient for clinical decision making affects the patients, share in nursing care. Moreover, increasing level of education, patient's expectations, and more familiarity with his/her rights causes the patients to demand more authority and effectiveness in their communications with the caregivers. Communication gap is one of the reasons for the dissatisfaction of patients in the country.[17]
To improve health care and reduce patients’ dissatisfaction, the factors that affect communication between nurses and patients must be identified and taken into account, also response to all communication needs of patients should be provided.[18] Therefore, this study was conducted with the aim of exploring the factors influencing the communication between cancer patients and their nurses.
MATERIALS AND METHODS
In this study, in order to explore participants’ experiences of factors influencing communication, qualitative content analysis approach was used. Participants (nine patients, three family members, and five nurses) were chosen based on purposive sampling and saturation principles using the following inclusion criteria for patients: 1) They should be at least 20 years old, and 2) they should not be suffering from mental disorders according to their records. The inclusion criteria for family members were: 1) They should be at least 20 years old, and 2) they should have experience of accompanying patient during hospitalization; the criteria for nurses were: 1) At least one year of nursing experience in oncology unit, and 2) a minimum of a bachelor's degree in nursing. This study was conducted in two main oncology centers in Tabriz that include Ali-Nasab Hospital and Shahid Ayatollah Qazi Tabatabaee hospital.
The data were collected during the months of May to December 2012 using semi-structured and in-depth individual interviews. All interviews were audiotape-recorded. In-depth individual interviews were performed in an isolated room for the participants’ comfort. The interviews that lasted between one and two hours started with general questions but progressively, questions became more detailed pertinent to the study. For example, “What experience do you have in communication with cancer patients? What are your experiences of nurses’ communication with you? How nurses act for you?” In case of need, the researcher, with follow-up questions, asked participants to express experiences, memories, and more description of their understandings of what they say. Natural behaviors and patient-nurse interactions were observed in the environment, and field notes were prepared in the same environment as well. It means that notes recorded interaction of nurses with patients during nursing care, chemotherapy, or bone marrow biopsy.
The researcher transcribed the interviews and field notes verbatim and read them all several times to obtain full understanding of the data. Whole interviews and field notes were contemplated as units of analysis. Words, sentences, and paragraphs considered as the meaning units were condensed according to their content and context. The condensed meaning units were abstracted and labeled with codes. Codes were sorted into subcategories and categories based on comparisons regarding their similarities and differences. Finally, a theme was formulated as the expression of the latent content of the text.[19]
The Research Council and Ethics Committee affiliated to Kerman University of Medical Sciences approved the study proposal (with No K.91.125). The aims of the study were explained in detail to the participants. The following information was given to the participants: The voluntary nature of the participation, their right to privacy, anonymity, and confidentiality as well as right to withdraw from the study at any time without any penalty. The participants then signed an informed consent form. During observation sessions, informed consent was obtained dynamically and continuously from both nurse and patient.
To increase the validity of the data, the codes were compared, and the differences were discussed and re-evaluated in group research, until shared codes and categories were created. In addition, parts of two interviews that converted to text had been sent to two expert researchers in the qualitative research on cancer. The agreement between the external coders with codes of researchers was measured using Holsti method,[20] which was an average of 78%.
RESULTS
All the nurses participating in the study had a bachelor degree, and their work experiences in oncology unit ranged from a year and half to 29 years. There was just one male. Two of them were head nurses. The patients’ age ranged between 20 and 59 years, and there were three females. The patients were diagnosed with and were being treated for leukemia, breast cancer, colon, lymphoma, sarcoma, stomach, and liver cancer.
Data analysis resulted in the emergence of the “three-factor effects” theme. This theme suggests that despite the desire of nurses and patients to establish a patient-centered communication regarding a particular condition of the patient and the caregiver, always this kind of communication was being affected strongly by three factors that were related to the condition of patient, the nurse, and the organization. In this theme, the three categories which emerged affect communicative performance of nurses were: Patient as the center of communication, nurse as a human factor, and organizational structures [Table 1]. These categories explain the underlying psychosocial and cultural factors influencing nurse–patient communication in oncology care environment.
Table 1.
Categories and sub-categories in theme of three-factor effects
The patient as the center of the communication
This category refers to the particular characteristics of the patient and the changes that the disease and its long-term treatment impose on the patient and his/her family. These changes made communication with patients particularly important.
Changes imposed by the disease
Cancer and treatments such as mastectomy and chemotherapy cause severe appearance changes in patients. In addition, change of patients’ self-image has more effect on mood in young patients, particularly females. In such circumstances, it is essential that nurses consider gender differences, needs, and problems of patients in communication. These changes cause the patient to be deprived of the support of his/her family or his/her spouse.
“Participant 2 (nurse): Females have different problems; we saw that when their appearances change, their husbands avoid them….they do not contact easily, they become apathetic to our recommendations….”
The change in appearance was much stressful for patients, which caused an increase in their emotional needs. In other words, preparing the patients by the nurse before the onset of these changes would be helpful.
“Participant 4 (patient): The first time of chemotherapy, I had a great fear, the mouth sores, hair shedding,… the nurse who had given me drugs talked to keep me calm, but I was still afraid of serum in the foil.”
Sometimes patients showed reactions such as anger and aggression in communication with nurses.
“Participant 10 (nurse): When a number of periods pass and they see there is no improvement, they become depressed, which makes it hard to communicate with them. Because he/she thought that whatever had been done by you or the doctor was useless…”
This condition caused nurses to limit verbal communication with them and just to leave them alone in their world not to be met with negative reactions of patients.
“Participant 13 (nurse): In some patients, because they were not in the mood, we tried to make the least verbal communication with them…when insisting on communication, they turned aggressive.”
Emotional need of families of end-stage patients substantially increased, that they showed severe psychological reactions. Nurses tried to support them spiritually and emotionally to prepare them for the upcoming eventuality.
“Participant 13 (nurse): When a patient is ill or close to death, his/her family showed violent reactions… cried, made noise, I let them express their feelings. I consoled them to trust in God…”
The particular characteristics of the patient
Patients with higher education level asked more questions. In addition, with increased awareness, adherence to self-care recommendations became more.
“Participant 11 (nurse): Patients are not the same in terms of awareness and knowledge. Even for patients with high levels of education, they don’t get convinced with our trainings and take the Internet to search for information. We consider these situations to give appropriate trainings. For those with low-level education, we try to provide them with simple information about the disease and its complications.”
Another particular characteristic is the stage of the disease. Patients after passing the denial stage are more active in terms of communication with nurses. However, when they reach close to end stages, they often become depressed. According to a number of participants, in the beginning stage, when patients became aware of the diagnosis and in the end stages as well, they had greater need for nurses and for their support.
“Participant 9 (nurse): In the active phase, patient tries to communicate with the nurse, he/she always asks questions and requires information, but when they get discouraged of the treatment, they seek less information than before. In this phase, they should be supported emotionally more.”
Difference in languages is another effective characteristic that plays a preventive role in communication. In such cases, using a third person who is familiar with the language of the patient and of the nurse was the only possible solution to break the language barrier in nurse - patient communication.
“Participant 6 (relative): Well, my mother speaks Kurdish. Moreover, she is illiterate. Therefore, nurses cannot explain to her what they mean. When I am here, I translate what nurses say to her into Kurdish.”
In terms of participants, another effective characteristic was gender differences. In fact, male participants mention it as a major barrier in communication. Our study showed that unmarried young female nurses have difficulty in communicating in a friendly manner with male patients.
“Participant 11 (unmarried female nurse) in this regard stated that: There have been times when I communicate comfortably with a male patient and it brings problems. To me, communication is for facilitating curing, but the patient thinks something else. I try to limit contact with young males.”
Nurse as a human factor
This category deals with the personal, cognitive, emotional, and professional characteristics processed by nurses, which affect the nurse-patient communication.
Perception of professional self: Pre-requisite of patient-centered communication
To work and communicate effectively with patients in oncology, nurses should have three characteristics as follows: Self-confidence, holistic view, and expert knowledge. In fact, the presence of these characteristics leads to the “perception of professional self” in nurse that is effective in nurse-patient communication.
Self-confidence in nurses shows extent to which they are familiar with their roles and its influence in the consequences of cancer and its treatment. Some nurses in the present study had the view that doctors have towards caring. In other words, they measure the effectiveness of the work of a nurse by an increase in the patient's longevity; they believed that because their work could not be effective in curing the disease, then it doesn’t matter how they communicate with the patient. Lack of confidence caused them to make technical aspects important and ignore the effectiveness of nurse-patient communication in improving the patient's conditions.
“Participant 9 (nurse): I believe that whether the nurse sympathizes with the patient or not, is kind or not, and so on, he/she would get chemotherapy and eventually will die. I could not postpone the patient's death …”
Holistic approach as a professional characteristic in nurses demands that they consider comprehensive roles for themselves. In the present study, nurses mostly focus on care roles regardless the intellectual and emotional context which care is provide.
“Participant 6 (relative): Well, nurses emphasize more on routine works; most of them just gave medications, check blood pressure. Even during chemotherapy, they did not say anything or ask any questions…”
Expert knowledge of nurses is essential to identify, to solve problems, and to enable patients through information. In fact, the knowledge processed by a nurse leads the patient to develop trust in the nurse.
“Participant 11 (nurse): For effective communication with the patient, we should have more information. When a patient sees that I have rich information and I answer whatever he/she asks, then he/she feels can trust me.”
Sense of vulnerability
Nurses described this characteristic as the feeling of exposure to physical and psychological harm during care and communication with patients with cancer. This feeling stems from three beliefs including the impalpable effects of chemotherapy drugs on the health of nurses, transmission of depressed mood, and grief after death of patient. In light of this sense, their relationship was more of a superficial and non-intimate communication, in which emotional issues were not being exchanged between the nurse and the patient.
Nurses think that preparing chemotherapy drugs, close contact with people undergoing chemotherapy could affect them with drug complications in future.
“Participant 9 (nurse): In the oncology unit, nurses are much afraid of the side-effects of chemotherapy, which in turn increases job dissatisfaction. In addition, it makes the nurse to limit his/her communication with the patient.”
Nurses suffer from a sense of grief that afflicts them following the death of patients. Long-term relationships with their patients have brought up friendship and familiarity, while the death of patient cuts friendship between the patient and the nurse. Because of the fear of being in a situation like this, nurses limit friendly and intimate relationship with patients.
“Participant 9 (nurse): Due to prolonged hospitalization of patients when he/she died, it was hard for you to take him/her out of your mind.… When a patient died, it was just like that a friend has been dead. Because of this, some nurses try not to be involved with patients emotionally.”
Organizational structures
These factors in organizational context lead to reduction in quantity and quality of nurse-patient communication and include the three sub-categories.
Workload and time imbalance
The large number of patients, the unstable condition of the patients as well as shortage of nurses would lead to imbalance between the workload and time for nurses that caused extreme stress to the nurses and minimized the time of interacting with patients and supporting them emotionally.
“Participant 10 (nurse): Workload of oncology is horrible. Due to the high workload, communications with patient become less, often routine care is a priority, and there isn’t an opportunity to support the patient.”
Impose duties in context of neglecting nurse and patient needs
Nurses participating in the study felt they were imposed in oncology and had to tolerate conditions that result from organizational culture and lack of attention to the personal and professional needs of them. However, nurse managers acknowledge the hard work in oncology, but in conditions of overcrowding of patients, they impose additional shifts to nurses. In this situation, there is a reduction in the quality of care and communication with patients, and the conflict between work and personal life increases job dissatisfaction.
“Participant 2 (nurse): Irritated behavior with patients, especially in nurses who had been given forced extra shifts, is more common… Concern for her child… problems with her husband… she is dissatisfied with her job… working with cancer patient has been regular for her/his…”
One of the impositions was compulsory education, and it was inconsistent with the nurses’ need. Nurses believed that the trainings provided do not prepare them to communicate with the patients with cancer.
“Participant 9 (nurse): Here, managers hold courses about communication with patient, but is communication really the same in oncology and general units?”
The dominant culture among oncology nurses is routine-oriented; it means that nurses due to the high workload, limited time, and incomplete understanding of their professional roles, provide task-oriented care rather than holistic care.
“Participant 1 (relative): High workload does not justify neglect of patients… They can communicate with patient and listen to him/her during care… His spirit is more important than his/her body, but they just take care of his/her body.”
Lack of supervision
Patients expect the system have not supervision over work and communication of nurses. Surprisingly, nurses believed that the system does not demand them to increase their ability in communication with patients. In fact, it demands them to pass their shifts and to do their tasks that caused nurses to be inclined to do dictated tasks that were ordered by doctors.
“Participant 1 (relative): The system should provide more supervision on the nurse's behavior with the patients. The system should ask the nurse to strengthen his/her communication with the patients…”
DISCUSSION
This study aims to explore the factors affecting the communication between patients with cancer and nurses. This study indicates that the triangle of patient, nurse, and organization can play a decisive role in the effectiveness of this communication. Problems related to these three factors have been stated in various studies.[1,4,5,10,12,21,22]
Our participants explain that the impacts of the disease on the body, mind, and social life bring difficulties for them. In fact, paying comprehensive attention to these problems by nurses would facilitate communication process. The result of McCabe's study showed that considering the needs and problems of patients is a fundamental key in patient-centered communication.[5] The findings indicated the complexity of communication in end-stage patients. Perhaps, so the literature indicates, in this stage of cancer, patients are faced with unpleasant feelings and thoughts of death, and focus of health care providers must be shifted to the relief of emotional distress.[9,21,23,24] Moreover, our results showed that the appearance changes resulting from the disease and its treatment lead to weakening the patient's mood, which make it difficult to communicate with them. Understanding these changes and preparation of patient and family for dealing with these changes could reduce the severity of the patient's emotional distress. In patients with cancer, return to previous life is a dream, but when they realize that this would not happen, they are depressed. This situation could disrupt interactions with caregivers.[9]
Characteristics of the patients seemed to be an important influential factor on the communication, and the results of the present research showed that information-seeking differed from patient to patient depending on their educational level and the disease stage and patients with different conditions in terms of education level and stage of the disease demand different information and nurses can provide appropriate information consistent with the patient preferences and perception to gain the trust. Owen and Jeffrey pointed out that the need and demand for information differs in patients and depends on the patient's understanding of the issues and of his/her health literacy.[9] Fakhr- Movahedi et al. showed that information provision to patient influences on the nurse-patient communication and leads to building confidence in patients.[4]
In our study, more female patients mentioned different emotional needs than male patients. Moreover, the need for emotional support was more expressed by young females. The study of Wessels et al. also showed that among the factors related to patient, gender is the most influential factor on patients’ preferences.[25] Studies showed that females more than males prefer to receive psychosocial support during communication.[26,27,28] This is not restricted to only patients, but family members are also affected by the disease. The need to support family members especially increases in the end stages of the disease, and if the family members were not supported in this situation, negative psychological reactions of relatives such as stress, tension, and worry will be transferred to the patient. This finding is not consistent with results of Fakhr-Movahedi et al., to be precise; they mentioned that presence of family members in the wards prevents nurse-patient communication.[4] Perhaps, this difference is related to the setting of their study, which was restricted to medical-surgical wards, where emotional support to patients was not as important as it is in oncology wards. In contrast, Park and Song found that for nurses, the absence of a family member as caregiver is the most important barrier in communication with patient.[29]
The other characteristic influencing in our results was language as the difference in language played a deterrent role in communication. A number of literatures,[1,4,29,30] support our findings. In addition, gender differences between patient and nurse prevents friendly relationship, which was expressed mostly by female nurses and male patients participating in the research. In studies, patients’ preference for receiving care from a nurse of the same gender was referred as a cultural issue.[1,4] From the perspective of the people and health system managers, gender differences between patient and care providers is an important cultural challenge in Iran because it's a custom in Iran that nurses are prohibited from touching or gazing at patients of the opposite sex,[1] and the government has approved a plan to fit sex of health care providers with patients in 1998, but the shortage of nurses, especially male nurses has prevented its implementation.[31] Although in the current study, it was found that unmarried female nurses try to limit conversation with young male patients in interactions with them, other studies have not mentioned about this finding that we found in religious background of Iran as a Muslim country.
Professional and psychological characteristics of the nurses were other influential factors on the nurse-patient communication. According to our findings, the lack holistic perspective among nurses inclined them towards doing physician orders and physical care. Biomedical perspective in nurses obstructs emotional support for the patient and holistic care in clinical situations. This perspective was reflected in more attention of nurses to the technical aspects of the caring and meeting physical needs of patients. Study of Zamanzadeh et al. showed that patients with cancer and their nurses perceive physical aspects of care more valuable than other aspects.[32] Sivesind et al. study also indicated that nurses have less self-confidence in resolving non-physical problems and responding to emotional needs of patients.[33] These results show that nurses have not yet moved toward a holistic view in practice because a holistic nurse will be sensitive to the patient's whole spectrum of needs.[34] Papathanasiou et al. mentioned that ineffective communication through health systems is mostly derived from the biomedical view that has a negative effect on nursing care provision. This problem is rooted in the fact that the majority of nurses were graduated from educational systems, which focus only on practical skills.[35]
In addition, our study showed that nurses who have communication skills and knowledge gain the trust of patients in communication process. Systematic review of Rchaidia et al. indicated according to the patients perception that good nurses are characterized by professional and trained skills, specific nursing and non-nursing knowledge, and support provision.[36] Such nurses increase confidence, hope, comfort, and safety in their patients.[36,37]
For the nurses participating in the current study, psychological pressure of caring of patients who are suffering from cancer was perceived as a factor influencing on the nurse-patient communication. They mentioned the sense of vulnerability as an effective factor on communication that could be understood through a long-term and friendly relationship with patient. Owen and Jeffrey believed that in long-term care of patients with cancer, nurses who share to patients’ distress in a close emotional connection with them, resulting in the emotional involvement of nurses that is harmful for them.[9] Rassouli et al. showed that fatigue in nurses working in oncology units is more related to emotional factors.[38] Aycock and Boyle define this phenomenon as compassion fatigue in oncology.[39] In addition, Anselm et al. claim that under such psychological tension, caregivers are unable to communicate effectively.[40] According to the experiences of nurses participating in the study, traumatic nature of work in oncology is related to death of patients that occurs frequently. Other studies referred to the fear of death in oncology and its impact on communication with patient.[9,10,12]
Our research showed that in organizational dimension, factors such as time, workload, and imbalance between these two minimizes communication with patients. Furthermore, Maguire et al. noted that crowded conditions increase pressure for caregivers and waiting time for patients. In such situations, nurses do not have enough time to discover concerns of patients.[41] This finding is consistent with other studies that showed lack of time, heavy workload, work in extra shifts, and fatigue in nurses hindered nurse–patient communication.[4,42] In contrast, the study of Chan et al. showed that nurses with integrating communication within the routines that they tend to do, in practice prove that not only extra time is not needed to communicate with the patients but also good communication is possible without wasting their time.[43]
According to the present research, imposed caring duties in task-oriented organizational context reduce the communication with patients. Nurses participating in the study believe that if their managers meet the need of nurses, request them to do their all roles and monitor their work, all needs of the patients will be attended by the nurses. Other studies have showed that task-oriented approach results in regarding of many of the needs and problems of patients during communication.[1,5] Our findings demonstrated that nurses’ tendency to perform dependent tasks, the shadow of bio-medical paradigm over care, and physician-centered system hindered patient-centered communication. Study results indicated that nurses often focus on the physicians orders instead of the patient's needs and problems,[4,13] and causes the patients to feel that the nurses’ duties and physician orders have more importance than patients.[5] Our findings indicated that the lack of monitoring on communication processes by nursing managers influences on the nurse-patient communication. In a task-oriented structure, in which nursing managers do not emphasize on the communication with patient, reduction of communication is expectable.[5,10] In order to confirm this issue, Anoosheh et al. found that lack of nursing manager appreciation of communication behaviors of nurses decreases communication with patient.[1]
Systematic review of Gysels et al. indicated the moderate effectiveness of training courses in increasing the communication skills and facilitator attitudes. In addition, it emphasizes that the effectiveness of courses is relevant to long-term courses, integrating theory, and practical exercises and getting feedback from colleagues.[44,45] Our research suggested that nurses perceived the type and the quality of training courses as insufficient in improving their communication skills. They requested the kind of education, which is consistent with their communications needs in oncology. Study of Wilkinson et al. showed that communication skill training for nurses can change communication skills and the level of confidence in them to communicate with patients.[10]
CONCLUSION
Understanding the factors influencing the communication could be the first step to solve communication problems. In fact, it can be said that a satisfactory communication is impossible without sufficient and comprehensive understanding of the views of nurses and patients. In the present research, in the context of nurse-patient communication, routine and task-oriented approach reduced quality and quantity of care. Changes in the culture of the nursing care systems are essential in order for the patients to feel that their individuality is more regarded than the nurses’ works. Nurses must feel that they receive proper training for care and communication with patients. These trainings should promote nurses’ perception of their various roles for providing support to the patients with cancer. Managers must support nurses emotionally considering nurses’ personal and professional problems. Furthermore, they must prevent burnout by balancing the workload and staffing. This research was conducted based on the experiences of Iranian patients with cancer, their family members and the nurses, and according to a few studies in this area, it is necessary that factors influencing nurse-patient communication in other life-threatening chronic conditions has to be researched.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009;56:243–9. doi: 10.1111/j.1466-7657.2008.00697.x. [DOI] [PubMed] [Google Scholar]
- 2.Baile WF, Lenzi R, Kudelka AP, Maguire P, Novack D, Goldstein M, et al. Improving physician-patient communication in cancer care: Outcome of a workshop for oncologists. J Cancer Educ. 1997;12:166–73. doi: 10.1080/08858199709528481. [DOI] [PubMed] [Google Scholar]
- 3.Bakker DA, Fitch MI, Gray R, Reed E, Bennett J. Patient-health care provider communication during chemotherapy treatment: The perspectives of women with breast cancer. Patient Educ Couns. 2001;43:61–71. doi: 10.1016/s0738-3991(00)00147-6. [DOI] [PubMed] [Google Scholar]
- 4.Fakhr-Movahedi A, Salsali M, Negharandeh R, Rahnavard Z. A qualitative content analysis of nurse-patient communication in Iranian nursing. Int Nurs Rev. 2011;58:171–80. doi: 10.1111/j.1466-7657.2010.00861.x. [DOI] [PubMed] [Google Scholar]
- 5.McCabe C. Nurse-patient communication: An exploration of patients’ experiences. J Clin Nurs. 2004;13:41–9. doi: 10.1111/j.1365-2702.2004.00817.x. [DOI] [PubMed] [Google Scholar]
- 6.Washington, DC: S.S. Department of Health and Human Services; 2005a. [Last accessed on 2012 Aug 25]. Agency for Healthcare Research and Quality (AHRQ). National healthcare disparities report. http://archive.ahrq.gov/qual/nhdr05/nhdr05.pdf . [Google Scholar]
- 7.Bonds DE, Zaccaro DJ, Karter AJ, Selby JV, Saad M, Goff DC., Jr Ethnic and racial differences in diabetes care: The insulin resistance atherosclerosis study. Diabetes Care. 2003;26:1040–6. doi: 10.2337/diacare.26.4.1040. [DOI] [PubMed] [Google Scholar]
- 8.Skilbeck J, Payne S. Emotional support and the role of clinical nurse specialists in palliative care. J Adv Nurs. 2003;43:521–30. doi: 10.1046/j.1365-2648.2003.02749.x. [DOI] [PubMed] [Google Scholar]
- 9.Owen R, Jeffrey D. Communication: Common challenging scenarios in cancer care. Eur J Cancer. 2008;44:1163–8. doi: 10.1016/j.ejca.2008.02.029. [DOI] [PubMed] [Google Scholar]
- 10.Wilkinson S. Factors which influence how nurses communicate with cancer patients. J Adv Nurs. 1991;16:677–88. doi: 10.1111/j.1365-2648.1991.tb01726.x. [DOI] [PubMed] [Google Scholar]
- 11.Sherman SR. Closing the communication gap in cancer care. Calif Med. 1972;116:76–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Tay LH, Hegney D, Ang E. Factors affecting effective communication between registered nurses and adult cancer patients in an inpatient setting: A systematic review. Int J Evid Based Healthc. 2011;9:151–64. doi: 10.1111/j.1744-1609.2011.00212.x. [DOI] [PubMed] [Google Scholar]
- 13.Naish J. The route to effective nurse-patient communication. Nurs Times. 1996;92:27–30. [PubMed] [Google Scholar]
- 14.Rafii F, Hajinezhad ME, Haghani H. Nurse caring in Iran and its relationship with patient satisfaction. Aust J Adv Nurs. 2007;26:75–84. [Google Scholar]
- 15.Tehran: Cancer Research Center, Cancer Institute of Iran; 2012. [Last accessed on 2012 Nov 27]. National Network for Cancer Research. Comprehensive program for supportive and palliative care of cancer in Iran. crc.tums.ac.ir/Portals/6/mostanadat/scoping.docx . [Google Scholar]
- 16.Sharifi-Moghaddam M. The number of Iranian nurses is the third of international standard. 2011. [Last accessed on 2012 Aug 13]. http://daneshju.ir/forum/f873/t77050.html .
- 17.Kattel S. Bangladesh: Master in public policy and governance program thesis, North South University; 2010. [Last accessed on 2013 Jan 12]. Doctor patient communication in health care service delivery: A case of Tribhuvan University Teaching Hospital, Kathmandu. http://mppg-nsu.org/attachments/119_Final%20Thesis%20_Sarbani%20Kattel_.pdf . [Google Scholar]
- 18.Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, et al. Closing the loop: Physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 19.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–12. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Rourke L. Methodological issues in the content analysis of computer conference transcripts. Int J Artif Intell Educ. 2001;12:8–22. [Google Scholar]
- 21.Iranmanesh S, Axelsson K, Sävenstedt S, Häggström T. A caring relationship with people who have cancer. J Adv Nurs. 2009;65:1300–8. doi: 10.1111/j.1365-2648.2009.04992.x. [DOI] [PubMed] [Google Scholar]
- 22.Rodin G, Mackay JA, Zimmermann C, Mayer C, Howell D, Katz M, et al. Clinician-patient communication: A systematic review. Support Care Cancer. 2009;17:627–44. doi: 10.1007/s00520-009-0601-y. [DOI] [PubMed] [Google Scholar]
- 23.Iranmanesh S, Abbaszadeh A, Dargahi H, Cheraghi MA. Caring for people at the end of life: Iranian oncology nurses’ experiences. Indian J Palliat Care. 2009;15:141–7. doi: 10.4103/0973-1075.58461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slort W, Schweitzer BP, Blankenstein AH, Abarshi EA, Riphagen II, Echteld MA, et al. Perceived barriers and facilitators for general practitioner-patient communication in palliative care: A systematic review. Palliat Med. 2011;25:613–29. doi: 10.1177/0269216310395987. [DOI] [PubMed] [Google Scholar]
- 25.Wessels H, de Graeff A, Wynia K, de Heus M, Kruitwagen CL, Woltjer GT, et al. Gender-related needs and preferences in cancer care indicate the need for an individualized approach to cancer patients. Oncologist. 2010;15:648–55. doi: 10.1634/theoncologist.2009-0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clarke SA, Booth L, Velikova G, Hewison J. Social support: Gender differences in cancer patients in the United Kingdom. Cancer Nurs. 2006;29:66–72. doi: 10.1097/00002820-200601000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer. 2000;88:226–37. doi: 10.1002/(sici)1097-0142(20000101)88:1<226::aid-cncr30>3.3.co;2-g. [DOI] [PubMed] [Google Scholar]
- 28.Volkers N. In coping with cancer, gender matters. J Natl Cancer Inst. 1999;91:1712–4. doi: 10.1093/jnci/91.20.1712. [DOI] [PubMed] [Google Scholar]
- 29.Park EK, Song M. Communication barriers perceived by older patients and nurses. Int J Nurs Stud. 2005;42:159–66. doi: 10.1016/j.ijnurstu.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Magnusdottir H. Overcoming strangeness and communication barriers: A phenomenological study of becoming a foreign nurse. Int Nurs Rev. 2005;52:263–9. doi: 10.1111/j.1466-7657.2005.00421.x. [DOI] [PubMed] [Google Scholar]
- 31.Reflections of fit plan of administrative and technical design standards of medical institutions with sacred religion. J Women's Rights. 1998;3:16–9. [Google Scholar]
- 32.Zamanzadeh V, Azimzadeh R, Rahmani A, Valizadeh L. Oncology patients’ and professional nurses’ perceptions of important nurse caring behaviors. BMC Nurs. 2010;9:10. doi: 10.1186/1472-6955-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sivesind D, Parker PA, Cohen L, Demoor C, Bumbaugh M, Throckmorton T, et al. Communicating with patients in cancer care; What areas do nurses find most challenging? J Cancer Educ. 2003;18:202–9. doi: 10.1207/s15430154jce1804_7. [DOI] [PubMed] [Google Scholar]
- 34.Lai HL, Hsieh ML. Alternative nursing interventions for facilitating holistic nursing based on eastern philosophy. Tzu Chi Nurs J. 2003;2:13–9. [Google Scholar]
- 35.Papathanasiou I, Sklavou M, Kourkouta L. Holistic nursing care: Theories and perspectives. American Journal of Nursing Science. 2013;2:1–5. [Google Scholar]
- 36.Rchaidia L, Dierckx de Casterlé B, De Blaeser L, Gastmans C. Cancer patients’ perceptions of the good nurse: A literature review. Nurs Ethics. 2009;16:528–42. doi: 10.1177/0969733009106647. [DOI] [PubMed] [Google Scholar]
- 37.Berterö C, Eriksson BE, Ek AC. Demanding interaction-given routines: An observational study on leukaemia patients and their nursing staff. Int J Nurs Pract. 1996;2:201–8. [Google Scholar]
- 38.Rassouli M, Zandiye S, Noorian M, Zayeri F. Fatigue and its related factors in pediatric and adult oncology nurses. Iran J Nurs. 2011;24:37–47. [Google Scholar]
- 39.Aycock N, Boyle D. Interventions to manage compassion fatigue in oncology nursing. Clin J Oncol Nurs. 2009;13:183–91. doi: 10.1188/09.CJON.183-191. [DOI] [PubMed] [Google Scholar]
- 40.Anselm AH, Palda V, Guest CB, McLean RF, Vachon ML, Kelner M, et al. Barriers to communication regarding end-of-life care: Perspectives of care providers. J Crit Care. 2005;20:214–23. doi: 10.1016/j.jcrc.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 41.Maguire P, Faulkner A, Booth K, Elliott C, Hillier V. Helping cancer patients disclose their concerns. Eur J Cancer. 1996;32A:78–81. doi: 10.1016/0959-8049(95)00527-7. [DOI] [PubMed] [Google Scholar]
- 42.Cleary M, Edwards C, Meehan T. Factors influencing nurse-patient interaction in the acute psychiatric setting: An exploratory investigation. Aust N Z J Ment Health Nurs. 1999;8:109–16. doi: 10.1046/j.1440-0979.1999.00141.x. [DOI] [PubMed] [Google Scholar]
- 43.Chan EA, Jones A, Fung S, Wu SC. Nurses’ perception of time availability in patient communication in Hong Kong. J Clin Nurs. 2012;21:1168–77. doi: 10.1111/j.1365-2702.2011.03841.x. [DOI] [PubMed] [Google Scholar]
- 44.Gysels M, Richardson A, Higginson IJ. Communication training for health professionals who care for patients with cancer: A systematic review of effectiveness. Support Care Cancer. 2004;12:692–700. doi: 10.1007/s00520-004-0666-6. [DOI] [PubMed] [Google Scholar]
- 45.Gysels M, Richardson A, Higginson IJ. Communication training for health professionals who care for patients with cancer: A systematic review of training methods. Support Care Cancer. 2005;13:356–66. doi: 10.1007/s00520-004-0732-0. [DOI] [PubMed] [Google Scholar]


