Abstract
Context:
Attention deficit hyperactivity disorder (ADHD) is common in the general population, and many individuals with this condition participate in sports activity at all competition levels.
Evidence Acquisition:
Related studies were selected through literature searches of PubMed, MEDLINE, and Cochrane databases for the years 1991 to 2011. Key search terms were ADD, ADHD, sports, athletes, athletics, guidelines, NCAA, WADA, IOC, college, concussion, diagnosis, management, treatment, evaluation, return-to-play, pharmacotherapy, adult, adolescent, student, screening, injury, risk, neuropsychiatry, TBI, traumatic brain injury, and epidemiology.
Study Design:
Literature review.
Level of Evidence:
Level 4.
Results:
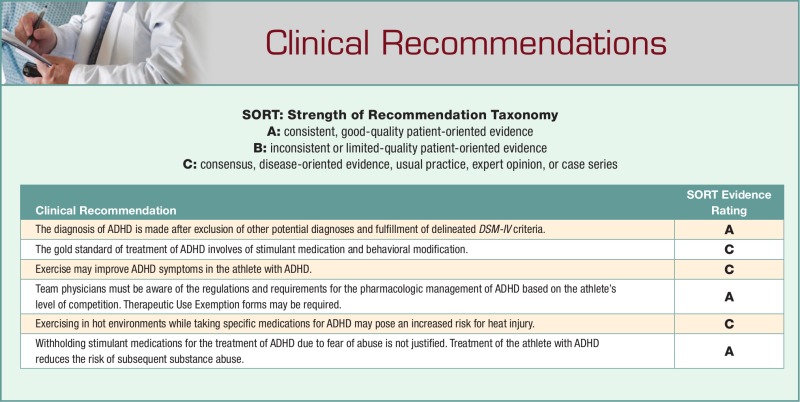
ADHD usually has an early onset, with delayed diagnosis in some patients due to heterogeneous presentations. Suspected cases can be evaluated with available diagnostic tools and confirmed clinically. Athletes with ADHD may participate at all competition levels.
Conclusion:
Athletes with ADHD are able to participate at all competition levels by following published guidelines and requirements. Exercise benefits many athletes with ADHD. The relationship between ADHD and concussion syndromes is currently under investigation.
Keywords: attention deficit, hyperactivity disorder, athletes
Attention deficit hyperactivity disorder (ADHD) is common in our society and now approaches 10% of children.25 While some patients stabilize over time, many individuals require treatment into adolescence and adulthood. Interventional therapy often benefits patients, including athletes. With proper management, athletes with ADHD may participate in sports at all competitive levels.
ADHD is a disorder of chronic and impairing behavioral patterns that results in abnormal levels of inattention, hyperactivity, or their combination.4,5 ADHD is a deficit in behavioral inhibition.12 ADHD is usually diagnosed in childhood, but some cases persist into adulthood or are diagnosed later.3,23,42,92
Proper diagnosis of ADHD in adults is based on a detailed patient history and assessment of current behavior and level of functioning using the same Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), criteria in adults and children. The criteria stipulate that symptoms must be present before 7 years of age. However, many adults do not recall early symptoms or did not have a diagnosis of ADHD made in childhood, often making the diagnosis of ADHD in adults less of a consideration.57,58
Attention Deficit Hyperactivity Disorder
Epidemiology
ADHD is one of the most common neuropsychiatric disorders of childhood, and its classification has been debated.6,11,13,28,72,73,75,83 According to the Centers for Disease Control and Prevention, rates of ADHD in US children continue to trend upward. Akinbami et al1 reported that the percentage of American children diagnosed with ADHD increased from 6.9% in 1998 to 2000 to 9.0% in 2007 to 2009.1,14,64,74,94 During this study time interval, the prevalence was higher among boys than girls. For boys, ADHD prevalence increased from 9.9% in the study period 1998 to 2000 to 12.3% in the study interval 2007 to 2009, and for girls from 3.6% to 5.5% during the same study period. In this group and time frame, prevalence varied by race and ethnicity, but the differences between most groups narrowed. Although some of the symptoms of ADHD diminish or disappear with maturation, 60% to 85% of children with ADHD continue to meet DSM-IV criteria as teenagers or young adults.2,3,18,19,28,49,92 ADHD may persist into adulthood in 30% of patients.15,47,52,61,63,80
Clinical Presentation
The causes and risk factors are unknown, but genetic factors seem to play a role.16,18,19,20 ADHD comprises inattentive and impulsive-hyperactive subtypes. The symptoms include poor attention span; difficulty with waiting one’s turn, managing time, organizational skills, and initiating or completing tasks; and increased risk-taking behaviors.67 Common comorbidities include anxiety, depression, disruptive behavior, learning disorders, substance abuse, and psychotic disorders.45,54 ADHD can present in a heterogeneous symptom pattern that is compounded by the variable presence of comorbid conditions including affective and substance use disorders.54
Diagnosis
ADHD is a clinical diagnosis supported by laboratory results, imaging tests, and careful clinical evaluation.46,74 Accurate patient evaluation requires gathering pertinent information from not only the patient and parent but also from others who interact with the patient, for example, teachers. This is especially important since children and adolescents may not be good historians of overall function. Several tools are available to assist with diagnosis and monitoring of those with ADHD, including the Connors Questionnaire, NICQH Vanderbilt Assessment Tool, DMS-5 criteria, Special Needs Assessment Profile (SNAP), SNAP-IV (Teacher and Parent Rating scale), SNAP-IV-C (condensed version), and Swanson, Kotkin, Angler, M-Flynn, and Pelham (SKAMP) Scale.30,34-36,70,80,81,87,90-92
Treatment
Outcomes for individuals with ADHD are as variable as the diverse patterns of behavior presentations.56,66 Ideally, early indicators of poor outcomes should be identified so that appropriate resources can be allocated for support.55,56
Several long-acting medications have been approved specifically for use in adolescents.24 These include extended-release dexmethylphenidate, transdermal methylphenidate, osmotic-release oral system methylphenidate, extended-release mixed amphetamine salts, lisdexamfetamine, and the nonstimulants atomoxetine, extended-release guanfacine, and extended-release clonidine.68
Athlete with ADHD
Level of Competition
Young Athletes
Young athletes (children and adolescents) may experience problems with specific movement required in competitive sports and may manifest problems with balance or coordinated activity.8 At the same time, exercise may decrease lack of attention or impulsive behavior.44 One study demonstrated improvement in anxiety/depression symptoms in those who participated in sports.28,53 Thus, competitive sports may benefit those with ADHD.32
Middle School/High School Athletes
The coaching staff and team physician should be aware of and note common potential side effects experienced with prescribed specific medications both during practice and in competition, with careful attention paid to the environment (eg, ambient temperature, humidity, wind, direct sunlight), the fatigue level of the athlete, and the athlete’s performance.60,65 In particular, athletes treated with amphetamines (which increase heat production) or tricyclics (which decrease sweat production) require careful monitoring.65,84 Young athletes may not recognize medication side effects such as decreased appetite, sleep problems, stomachache, or headache.39
Collegiate Athletes
As of August 1, 2009, collegiate athletes who are diagnosed with ADHD and receive stimulant medication must supply documentation of diagnosis and treatment for National Collegiate Athletic Association (NCAA) competition (participation) prior to initiation of the sport activity. This required documentation must provide evidence (1) that the athlete has undergone clinical evaluation to diagnose the disorder, (2) is being monitored routinely for use of the stimulant medication, and (3) has a current prescription on file.69 This often requires documentation from outside or previous health care providers. If documentation is no longer available, a current comprehensive evaluation must be completed. Furthermore, the NCAA requires yearly clinical evaluation and documentation with the sports medicine staff and the athletic department.69,74 This documentation requires (1) description of the assessment, evaluation tools, or procedures; (2) statement of diagnosis; (3) history of previous and current ADHD treatment; (4) statement that a nonbanned ADHD alternative medication has been considered if a stimulant medication is prescribed; and (5) plan for follow-up and monitoring visits.15,69,74
The NCAA requires that physicians consider nonstimulant medications before prescribing stimulants.16,18,71 In addition, team physicians should educate NCAA athletes about proper use of medications in the treatment of ADHD. It is crucial that the team physician explain to the athlete that while stimulant medications are allowed in the management of ADHD, certain rules do apply.
Olympic Athletes
Athletes competing at the Olympic level may participate and continue medical treatment with prohibited drugs for their ADHD as governed by the International Olympic Competition (IOC) and World Anti-Drug Agency (WADA).50,96 Many athletes may compete simultaneously at both the NCAA and Olympic levels but must be aware of specific guidelines for each organization.
Olympic-level athletes must submit a therapeutic use exemption (TUE) form to the Therapeutic Use Exemption Committees detailing the symptoms, diagnosis, and testing criteria utilized in forming the diagnosis of ADHD.50,95 These criteria often include the Connors scale, SNAP, or other DSM-IV tools.6,27,33,44,65,69 The diagnosis is then confirmed clinically.
Athletes maintained on continued therapy must undergo annual review. In the case of a well-documented, long-standing diagnosis, a TUE can be granted for up to 4 years. However, yearly reviews by an experienced clinician are still recommended.74,95
ADHD Effect on Performance
ADHD can manifest in many ways, including lack of focus and concentration, oppositional behavior in team sports, argumentative attitude, frustration, poor self-esteem, and mood lability.89 In addition, anxiety, depression, substance abuse, and psychotic disorders may coexist,89 each of which directly affects team sports and participant interaction. Academic difficulties may also arise that could threaten the student athlete’s qualification to participate in sports. For these reasons, athletes with ADHD often perform better with medical treatment in both the classroom and the sporting venue.
Treatment
The treatment of ADHD in sports requires a combination of behavioral, psychosocial, and medication modalities.80 The coordinated treatment often involves all members of the medical and athletic staff. With a coordinated effort, the abnormal, disruptive behavior can often be controlled.
Medication
Medications are often central to the treatment of ADHD (Table 1). Stimulants (amphetamines) and nonstimulants (atomoxetine and bupropion) are commonly used.32 While tricyclic antidepressants may be useful in select patients, they are not first-line agents.38 Many agents can potentially mitigate symptoms in patients with ADHD.
Table 1.
ADHD medications67
| Generic Name | Trade Name | Chemical Class | Comments | Side Effects | |
|---|---|---|---|---|---|
| Stimulants | Methylphenidate | Concerta, Ritalin, Metadate | Amphetamine | MOA: release and/or inhibit reuptake of D and NE Increased attentiveness, decreased disruptiveness |
Decreased appetite, nervousness, weight loss, sleep difficulties, irritability, hypertension, tachycardia |
| Mixed dextroamphetamine- amphetamine salts | Adderall | Amphetamine | MOA: release and/or inhibit reuptake of D and NE | Decreased appetite, nervousness, weight loss, sleep difficulties, irritability, hypertension, tachycardia | |
| Dextroamphetamine | Dexedrin, Dextrostat (labeled Adderall in Canada) | Amphetamine | Not commonly used | Decreased appetite, nervousness, weight loss, sleep difficulties, irritability, hypertension, tachycardia | |
| Modafinil (“cognitive enhancer”) | Provigil | Wakefulness-promoting agent | MOA: possible alpha-1 agonist and inhibition of GABA release centrally Indicated for sleep apnea, narcolepsy, fatigue due to multiple sclerosis Caution in those with cardiac disease, liver or renal insufficiency, psychosis |
Hypertension, arrhythmias, tachycardia, syncope, nausea, diarrhea, headache, insomnia, nervousness | |
| Nonstimulants | Atomoxetine HCL | Strattera | Selective NE reuptake inhibitor | MOA: selective inhibition of the presynaptic NE transporter Reduce symptoms of ADHD and anxiety Must increase dose slowly |
Upset GI, sedation, fatigue, dry mouth, increased sweating, hypertension, rarely hepatotoxic, increased suicidality |
| Bupropion | Wellbutrin, Zyban | Aminoketon | MOA: D and NE reuptake inhibitor Reduce irritability, impulsivity, and improve attention dysfunction Not commonly used as monotherapy but may be useful as adjuvant |
Drowsiness, anorexia, tics, potential seizures | |
| Antidepressants 1. Imipramine 2. Nortriptyline 3. Amitriptyline 4. Desipramine |
1. Tofranil 2. Pamelor 3. Elavil 4. Nopramin |
Tricyclic | MOA: block reuptake of D and NE Usually not recommended for competitive athletes due to side effect profile FDA “Black Box” warning for use in adolescents |
Anticholinergic effects (eg, dry mouth, sweating abnormalities), ECG changes, drowsiness/sedation, increased suicidality | |
| Clonidine | Catapres | Alpha-2 agonist | MOA: alpha-2 agonists Not commonly used as monotherapy but may be useful as adjuvant Consider patch for smooth drug release |
Sedating postural hypotension, dry mouth, fatigue, dizziness, aggravation of preexisting cardiac arrhythmias, profound withdrawal effects |
MOA, mechanism of action; D, dopamine; NE, norepinephrine; GABA, γ-aminobutyric acid; HCL, hydrochloric acid; FDA, Food and Drug Administration; ECG, electrocardiogram.
Adapted with permission from the American Medical Society of Sports Medicine.67
Performance Effects
Stimulant medications are beneficial to patients with ADHD and constitute the first treatment option selected.38 These effective medications are ergogenic in athletes but are approved by the NCAA, WADA, and IOC with proper documentation. Potential performance enhancement includes a subjective sense of euphoria, improved concentration, increased aggression, and decreased pain.22 Consequently, these agents may improve athletic performance.
Other medications less commonly utilized in athletes with ADHD include tricyclic antidepressants, bupropion, and clonidine, which are effective in treating ADHD but show increased side effects such as drowsiness, anorexia, and heat injury.
Side Effects
Two particular areas of concern are the risk for heat injury and cardiac arrhythmias. While the potential for both problems exists, occurrence in older, mature athletes is very low. Habel’s43 study in athletes up to age 64 years revealed a 1- to 3-mmHg increase in diastolic blood pressure and a 2- to 5-mmHg increase in diastolic blood pressure overall with no increased incidence of complications. Careful monitoring of the athlete’s weight, observing for possible heat-related illnesses, and checking for extreme fatigue is paramount.
The risk for cardiac arrhythmias is not increased compared with patients not receiving these medications.43,77,85,86 The greatest risk lies in younger athletes with symptoms of cardiovascular disease, an underlying structural heart defect, or preexisting heart disease.29,35,43 Team physicians should not prescribe stimulants to these patients.36,43
Schelleman et al explored cardiovascular risks of stimulant treatment in adolescents.77,78,84 The rate of sudden death or ventricular arrhythmia was no greater for children receiving medications compared with those who were not. Recent studies also suggest no increased risk of serious cardiovascular events.29,32
Careful history and examination should be performed prior to initiation of these agents. Electrocardiogram (ECG) testing is controversial.3,4,42,71,74,88 The team physician should assess the athlete’s blood pressure, heart rate, and exertional symptoms prior to initiating ADHD therapy and monitor these parameters periodically.
The specific side effects of medical treatment vary with the chemical class of agents. Many of the side effects can adversely affect the athlete’s performance (Table 1).
Concussion and ADHD
Concussion is defined by the Zurich Consensus Statement as a complex pathophysiologic process affecting the brain induced by traumatic biomechanical forces.62 Common symptoms include headache, dizziness, fatigue, irritability, insomnia, poor concentration, difficulty with memory, intolerance of stress, and emotional lability.26 The cognitive symptoms of impaired attention and memory and the behavioral symptoms that arise after a concussion can mirror those of a patient with ADHD.
Traumatic brain injury (TBI) in children can worsen ADHD symptoms.57 A study comparing children (5-15 years of age) with mild, moderate, and severe TBI showed that children with pre-injury ADHD had more significant and longer lasting symptoms of inattention and hyperactivity after TBI than controls.57 The symptoms of ADHD can worsen, and it may be more difficult to treat ADHD after a concussion.21 College football players with learning disabilities had a prolonged return to baseline function on neuropsychologic testing after concussion.31 Asplund et al9 examined factors associated with prolonged return to play. Athletes with a history of learning disorders or ADHD did not have a difference in outcome or prolonged return to play.9 The Zurich Consensus Statement does list learning disorders and ADHD as modifying factors in return to play after concussion.62 Individuals with a modifying factor such as ADHD may need additional management and a multidisciplinary approach rather than a standard return-to-play protocol.62 At this time, it seems reasonable to take a cautious approach with return to play in athletes with a prior diagnosis of ADHD.
Increased Risk of Injury or Prolonged Symptoms
Children with ADHD are more likely to be injured than children without ADHD in free play activities.37 The underlying problem of injury risk in children with ADHD is that they anticipate fewer negative consequences, expect less severe injury, and report greater likelihood of participating in risky behavior even though they recognize hazards at similar levels compared with control children.41 Five- to 14-year-old children with ADHD were more likely to have severe head injuries than children without ADHD. However, children with ADHD had fewer sports-related injuries.37 However, Clendenin et al29 showed a positive correlation between ADHD and sports-related injury in children 5 to 13 years of age. Currently, it is unclear whether ADHD predisposes children to sports-related injuries.
At this time no studies demonstrate patients with ADHD are at an increased risk of suffering from a sports-related concussion. However, individuals with low attention levels may be more prone to participate in fast-paced, unpredictable sports, therefore increasing the opportunity for head injury.40 Because of the common symptoms of ADHD and concussion, good baseline assessment of cognitive factors should be conducted to assist in making return-to-play decisions for an athlete with ADHD after concussion.
Secondary ADHD in Traumatic Brain Injury
Secondary ADHD (SADHD) develops after TBI. SADHD can follow severe TBI but has only been seen after moderate TBI in patients with pre-injury ADHD traits.59 There are no conclusive studies that demonstrate brain injury following mild TBI as the primary factor for SADHD.59
Utility of Neuropsychologic Testing
Individuals with ADHD show deficits in executive functions (cognitive processes that maintain an appropriate problem-solving set to attain a future goal).10 There are differences in pen-and-paper neuropsychologic testing results when comparing individuals with TBI and ADHD.7,82 To differentiate neuropsychiatric findings in TBI and ADHD patients, neuropsychologic evaluations were used with 90 children.82 Thirty children (mean age, 10.7 years) after moderate to severe TBI had significantly lower focus factor scores, while 30 children with ADHD (mean age, 10.6 years) had lower sustained scores. Both groups had lower encode factor (attention, concentration, and numeric reasoning) scores than controls (mean age, 11 years).
Adults with TBI or ADHD had more difficulty with attention tasks than controls.7 Those with mild TBI had slower responses while those with ADHD had higher levels of impulsivity.7 Based on these studies, differences do exist between moderate TBI and ADHD on neuropsychologic testing, but there are no studies examining patients with mild TBI or concussion versus patients with ADHD.
Neurocognitive testing was computerized to make neuropsychologic testing more widely available. Adolescents (ages 13-19 years) with self-reported ADHD tested lower on visual memory, processing speed, and right-left orientation and inhibition than controls without ADHD on Immediate Post-concussion Assessment and Cognitive Testing (ImPACT).51 There was no significant difference for verbal memory or reaction time.42,51 Baseline ImPACT testing showed a difference in symptoms, verbal memory, motor, and reaction time in Division I collegiate athletes with self-reported ADHD compared with normal controls.48,76 However, computer-based neuropsychologic tests should not be used to diagnose a learning disability or ADHD. If the results of baseline testing cause suspicion of a learning disability, referral to a neuropsychologist may be needed.56 Since normative data may not apply to those with ADHD, having a quality baseline evaluation to compare with postinjury testing may be best for treating athletes with ADHD after a head injury.14
Conclusion
Many athletes with ADHD can participate at all levels of competition while undergoing treatment. The team physician should be current on the diagnosis and proper medical management and aware of the potential side effects of effective treatment. The relationship between ADHD and concussion injuries is currently unknown.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Akinbami LJ, Xiang L, Pastor PN, et al. Attention deficit hyperactivity disorder among children aged 5-19 years in the United States. 1998-2009. CDC–NCHS Data Brief. 2011;70:1-5 [PubMed] [Google Scholar]
- 2. American Academy of Child and Adolescent Psychiatry, Work Group on Quality Issues Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:894-921 [DOI] [PubMed] [Google Scholar]
- 3. American Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Attention-Deficit/Hyperactivity Disorder Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics. 2000;105:1158-1170 [DOI] [PubMed] [Google Scholar]
- 4. American Academy of Pediatrics, Subcommittee on Attention-Deficit/Hyperactivity Disorder and Committee on Quality Improvement Clinical practice guideline: treatment of school-aged child with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108:1033-1044 [DOI] [PubMed] [Google Scholar]
- 5. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000 [Google Scholar]
- 6. American Psychiatric Association DSM-5 development. http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=383 Accessed June 2, 2012
- 7. Aracia E, Gualtieri CT. Neurobehavioral performance of adults with closed-head injury, adults with attention deficit, and controls. Brain Injury. 1994;8:395-404 [DOI] [PubMed] [Google Scholar]
- 8. Archer T, Kostrzewa RM. Physical exercise alleviates ADHD symptoms: regional deficits and development trajectory. Neurotox Res. 2012;21:195-209 [DOI] [PubMed] [Google Scholar]
- 9. Asplund CA, McKeag DB, Olsen CH. Sport-related concussion factors associated with prolonged return to play. Clin J Sport Med. 2004;14:339-343 [DOI] [PubMed] [Google Scholar]
- 10. Atkins JJ, Atkins MS, Pelham WE, Licht MH. A comparison of objective classroom measures and teacher ratings of attention deficit disorder. J Abnorm Child Psychol. 1985;13:155-167 [DOI] [PubMed] [Google Scholar]
- 11. Barbaresi WJ, Katusic SK, Colligan RC, et al. How common is attention-deficit/hyperactivity disorder? Incidence in a population-based birth cohort in Rochester Minn. Arch Pediatr Adolesc Med. 2002;156:217-224 [DOI] [PubMed] [Google Scholar]
- 12. Barkley RA. Behavioral inhibition, sustained attention, and executive function: constructing a unified theory of ADHD. Psychol Bull. 1997;121:65-94 [DOI] [PubMed] [Google Scholar]
- 13. Barkley RA, Cook EH, Diamond A, et al. International Consensus Statement on ADHD. Clinical Child Family Psychol Rev. 2002;5:89-111 [DOI] [PubMed] [Google Scholar]
- 14.Baseline Data/Immediate Post Concussive Assessment and Cognitive Testing. [Accessed January 10, 2013]. http://impacttest.com/publications/normative
- 15. Bidwell LC, McClernon FJ, Kollins SH. Cognitive enhancers for the treatment of ADHD. Pharmacol Biochem Behav. 2011;99:262-274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Biederman J. Attention-deficit/hyperactivity disorder: a life-span perspective. J Clin Psychiatry. 1998;59(suppl 7):4-16 [PubMed] [Google Scholar]
- 17. Biederman J, Farone SV. Current concepts on the neurobiology of attention-deficit/hyperactivity disorder. J Attention Disorders. 2002;6(suppl 1): S7-S16 [DOI] [PubMed] [Google Scholar]
- 18. Biederman J, Faraone S, Milberger S, et al. A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Arch Gen Psychiatry. 1996;53:437-446 [DOI] [PubMed] [Google Scholar]
- 19. Biederman J, Monteaux MC, Mick E, et al. Young adult outcome of attention deficit hyperactivity disorder: a controlled 10 year prospective follow-up study. Psychol Med. 2006;36:167-179 [DOI] [PubMed] [Google Scholar]
- 20. Biederman J, Spencer T. Attention-deficit/hyperactivity disorder (adhd) as a noradrenergic disorder. Biol Psychiatry. 1999:46:1234-1242 [DOI] [PubMed] [Google Scholar]
- 21. Boschert S. Experts discuss psychiatric effects of concussion. Family Practice News. 2011;July:36 [Google Scholar]
- 22. Bouchard R, Weber AR, Geiger JD. Informed decision-making on sympathomimetic use in sport and health. Clin J Sport Med. 2002;12:209-224 [DOI] [PubMed] [Google Scholar]
- 23. Brown RT, Amler RW, Freeman WS, et al. Treatment of attention-deficit/hyperactive disorder: overview of the evidence. Pediatrics. 2005;115:e749-e757 [DOI] [PubMed] [Google Scholar]
- 24. Cascade E, Kalali AH, Weisler RH. Short-acting versus long-acting medications for the treatment of ADHD. Psychiatry. 2008;5:24-27 [PMC free article] [PubMed] [Google Scholar]
- 25. CDC-ADHD. Data and Statistics—NCBDDD. [Accessed April 18, 2013]; http://www.cdc.gov/ncbddd/adhd/data.html
- 26. Centers for Disease Control and Prevention; Injury Prevention & Control: Traumatic Brain Injury. Concussion. http://www.cdc.gov/concussion/signs_symptoms.html Accessed April 18, 2013
- 27.CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder) [Accessed April 18, 2013]. http://www.chadd.org/Understanding-ADHD/Adults-with-ADHD/Symptoms-and-Causes.aspx
- 28. Claude D, Firestone P. The development of ADHD boys: a 12 year follow up. Can J Behav Sci. 1995;27:226-249 [Google Scholar]
- 29. Clendenin AA, Businell MS, Kelley ML. Screening ADHD problems in the sports behavior checklist: factor structure, convergent and divergent validity and group differences. J Atten Disord. 2005;8:79-87 [DOI] [PubMed] [Google Scholar]
- 30. Collett BR, Jeneva LO, Meyers KM. Ten-year review of rating scales V. Scales assessing attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2003;42:1015-1037 [DOI] [PubMed] [Google Scholar]
- 31. Collins MW, Lovell MR, McKeag DB. Relationship between concussion and neuropsychological performance in college football players. JAMA. 1999;282:964-970 [DOI] [PubMed] [Google Scholar]
- 32. Conant-Norville DO, Tofler IR. Attention deficit/hyperactivity disorder and psychopharmacologic treatments in the athlete. Clin Sports Med. 2005;24:829-843 [DOI] [PubMed] [Google Scholar]
- 33. Conners C. A teacher rating scale for use in drug studies with children. Am J Psychiatry. 1969;126:884-888 [DOI] [PubMed] [Google Scholar]
- 34. Conners CK. Manual for Conners’ Rating Scales. Conners Rating Scales-Revised. 3rd ed. North Tonawanda, NY: Multi-Health Systems; 2010 [Google Scholar]
- 35. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365:1896-1904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Diagnostic and Statistical Manual of Mental Disorders (DSM). 3rd ed. Washington, DC: American Psychiatric Association; 1980 [Google Scholar]
- 37. DiScala C, Lescohier I, Barthel M, Li G. Injuries to children with attention deficit hyperactivity disorder. Pediatrics. 1998;102:1415-1421 [DOI] [PubMed] [Google Scholar]
- 38. Dulcan MK, Benson RS. AACAP official action. Summary of the practice parameters for the assessment and treatment of children, adolescents, and adults with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1997;36:1311-1317 [DOI] [PubMed] [Google Scholar]
- 39. Dulk-Jacobs V. AD/HD medications for children. http://www.nimh.nih.gov/health/publications/mental-health-medications/complete-index.shtml#pub8 Accessed June 10, 2012
- 40. Esfandiari A, Broshek DK, Freeman JR. Psychiatric and neurological issues in sports medicine. Clin Sports Med. 2011;30:611-627 [DOI] [PubMed] [Google Scholar]
- 41. Farmer JE, Peterson L. Injury risk factors in children with attention deficit hyperactivity disorder. Health Psychol. 1995;14:325-332 [DOI] [PubMed] [Google Scholar]
- 42. Greydanus DE, Pratt HD, Patel DR. Attention deficit hyperactivity disorder across the lifespan: the child, adolescent, and adult. Dis Mon. 2007;53:70-131 [DOI] [PubMed] [Google Scholar]
- 43. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306:2673-2683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Halperin JM, Healey DM. The influences of environmental enrichment, cognitive enhancement, and physical exercise on brain development: can we alter the development trajectory of ADHD? Neurosci Biohav Rev. 2011;35:621-634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hamilton SS, Armando J. Oppositional defiant disorder. Am Fam Physician. 2008;78:861-866 [PubMed] [Google Scholar]
- 46. Harel EH, Brown WD. Attention deficit hyperactivity disorder in elementary school children in Rhode Island: associated psychosocial factors and medications used. Clin Pediatr. 2003;42:497-503 [DOI] [PubMed] [Google Scholar]
- 47. Hechtman L. Long-term outcome in attention deficit hyperactivity disorder. Psychiatr Clin North Am. 1992;1:553-565 [Google Scholar]
- 48. Hunt TN, McCamey KL, Beisner AJ. Relationship between ADHD and concussion history on neuropsychiatric test scores in collegiate athletes. Med Sci Sports Exerc. 2010;42:114 [Google Scholar]
- 49. Ingram S, Hechtman L, Morgenstern G. Outcome issues in ADHD: adolescent and adult long-term outcome. Ment Retard Dev Disabil Res Rev. 1999;5:243-250 [Google Scholar]
- 50.International Olympic Committee. The International Olympic Committee Anti-Doping Rules applicable to the Games of the XXX Olympiad, London. 2012. [Accessed May 25, 2012]. http://www.olympic.org/Documents/Games_London_2012/Anti-doping/IOC_Anti-Doping_Rules_London%20_2012-eng.pdf
- 51. Iverson GL, Strangway CL. Computerized neuropsychological screening of adolescents with ADHD. Paper presented at: National Association of School Psychologists; April 1, 2004; Dallas, Texas [Google Scholar]
- 52. Kessler RC, Adler LA, Barkley R, et al. Patterns and predictors of ADHD persistence into adulthood: results from the National Comorbidity Survey Replication. Biol Psychiatry. 2005:57:1442-1451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kiluk BD, Weden S. Sport participation and anxiety in children with ADHD. J Atten Disord. 2009;12:499-506 [DOI] [PubMed] [Google Scholar]
- 54. Kitchen REC. Disorders that are comorbid with ADHD. http://www.healthguideinfo.com/adult-add/p96967/ Accessed June 5, 2012
- 55. Klein RG, Biederman J. ADHD long-term outcomes; comorbidity, secondary conditions, and health risk behaviours. http://www.cdc.gov/ncbddd/adhd/workshops/outcomes.html Accessed June 14, 2012
- 56. Kutcher JS, Eckner JT. At-risk populations in sports-related concussion. Curr Sports Med Rep. 2010;9:16-20 [DOI] [PubMed] [Google Scholar]
- 57. Levin H, Hanten G, Max F, et al. Symptoms of attention-deficit/hyperactivity disorder following traumatic brain injury in children. J Dev Behav Pediatr. 2007;28:108-118 [DOI] [PubMed] [Google Scholar]
- 58. Max JE. Children and adolescents. In: Silver JM, McAllister TW, Yudofsky SC, eds. Textbook of Traumatic Brain Injury. 2nd ed. Arlington, VA: American Psychiatric Publishing; 2011:442-443 [Google Scholar]
- 59. Max JE, Lansing AE, Koele SL, et al. Attention deficit hyperactivity disorder in children and adolescents following traumatic brain injury. Dev Neuropsychol. 2004;25:159-177 [DOI] [PubMed] [Google Scholar]
- 60. Mayo Clinic Heatstroke risk factors. http://www.mayoclinic.com/health/heat-stroke/ds01025/dsection=risk-factors Accessed May 25, 2012
- 61. McCann BS, Royu-Byrne P. Attention-deficit/hyperactivity disorder and learning disabilities in adults. Semin Clin Neuropsychiatry. 2000;5:191-197 [DOI] [PubMed] [Google Scholar]
- 62. McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on Concussion in Sport 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clin J Sport Med 2009;19:185-200 [DOI] [PubMed] [Google Scholar]
- 63. McGee R, Partridge F, Williams S, et al. A twelve-year follow-up of preschool hyperactive children. J Am Acad Child Adolesc Psychiatry. 1991;30:224-232 [DOI] [PubMed] [Google Scholar]
- 64. National Center for Health Statistics Data Brief. 2011:70 [Google Scholar]
- 65. National Federation of State High School Associations Sports Medicine Handbook. 4th ed. http://www.nmact.org/pages/for_parents/HeatRelatedIllness.pdf Published May 2011. Accessed May 23, 2012
- 66. National Initiative for Children’s Healthcare Quality Caring for children with ADHD; a resource toolkit for clinicians. http://www.hichq.org/NICHQ/Topics/ChronicConditions/ADHD/Tools/ADHD.html Accessed June 25, 2012
- 67. National Institutes of Mental Health Attention deficit hyperactivity disorder (ADHD). http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder/complete-index.shtml Accessed June 12, 2012
- 68. National Institutes of Mental Health Attention deficit hyperactivity disorder (ADHD): medications. http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder/medications.shtml Accessed June 10, 2012
- 69.NCAA banned drugs and medical exceptions policy guidelines. [Accessed October 25, 2011]. http://www.ncaa.org/wps/wcm/connect/public/NCAA/Health+and+Safety/Drug+Testing/Resources/Medical+Exceptions+for+Banned+Substances
- 70. Office of Mental Health, New York State Scoring instrument for the SNAP IV-C-C rating scale. http://www.omh.ny.gov/omhweb/ebt/resources/snap_instructions.html Accessed June 2, 2012
- 71. Perrin JM, Friedman RA, Knilans TK, et al. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008;122:451-453 [DOI] [PubMed] [Google Scholar]
- 72. Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADH: a systematic review and meta-regression analyses. Am J Psychiatry. 1996;53:437-446 [Google Scholar]
- 73. Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psych. 2007;164:942-948 [DOI] [PubMed] [Google Scholar]
- 74. Putakian M, Kreher JB, Coppeo DB, Glazer JL, McKeag DB, White RD. Attention deficit hyperactivity disorder (ADHD) and the team physician: an American Medical Society for Sports Medicine Position Statement. Clin J Sport Med. 2011;21:392-401 [DOI] [PubMed] [Google Scholar]
- 75. Rowland AS, Lesesne CA, Abramovwitz AJ. The epidemiology of attention-deficit/hyperactivity disorder (ADHD): a public health view. Ment Retard Dev Disabil Res Rev. 2002;8:162-170 [DOI] [PubMed] [Google Scholar]
- 76. Schatz P, Zillmer E. Computer-based assessment of sports-related concussion. Appl Neuropsychol. 2003;10:42-47 [DOI] [PubMed] [Google Scholar]
- 77. Schelleman H, Bilker WB, Strom BL, et al. Cardiovascular events and death in children exposed and unexposed to ADHD agents. Pediatrics. 2011;127:1102-1110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Silva RR, Skimming JW, Muniz R. Cardiovascular safety of stimulant medications for pediatric attention deficit hyperactivity disorder. Clin Pediatr. 2010;49:840-851 [DOI] [PubMed] [Google Scholar]
- 79. Spencer T, Biederman J, Wilens T. Nonstimulant treatment of adult attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2008;367-384 [DOI] [PubMed] [Google Scholar]
- 80. Spencer T, Biederman J, Wilens T, et al. Adults with attention-deficit/hyperactivity disorder: a controversial diagnosis. J Clin Psychiatry. 1998;59(suppl 7):59-68 [PubMed] [Google Scholar]
- 81. Swanson N. and Pelham Rating Scale fourth edition James Swanson, PhD. Child Development Center, 19262 Jamboree Blvd, University of California; Irvine, CA: 92717. [Google Scholar]
- 82. Thaler ST, Allen DN, Park BS, McMurry JC, Mayfield J. Attention processing abnormalities in children with traumatic brain injury and attention-deficit/hyperactivity disorder: difference impairment of component processes. J Clin Exp Neuropsychol. 2010;32:929-936 [DOI] [PubMed] [Google Scholar]
- 83. Timini S, Taylor E. ADHD is best understood as a cultural construct. Brit J Psychiatry. 2004;184:8-9 [DOI] [PubMed] [Google Scholar]
- 84. US Department of Health & Human Resources, U.S. Food and Drug Administration. FDA Drug DrugFacts: stimulant ADHD medications—methylphenidate and amphetamines. http://www.drugabuse.gov/publications/drugfacts/stimulant-adhd-medications-methylphenidate-amphetamines Accessed May 25, 2012
- 85. US Department of Health & Human Resources, U.S. Food and Drug Administration FDA drug safety communication: safety review update of medications used to treat attention-deficit/hyperactivity disorder (ADHD) in children and young adults. www.fda.gov/Drugs/DrugSafety/ucm277770.htm Accessed May 12, 2012
- 86. US Food and Drug Administration, Drug Safety and Risk Management Advisory Committee Meeting. [Accessed October 25, 2011];2006 http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4202_00_TOC.htm
- 87. Vanderbilt AD/HD Diagnostic Teaching Rating Scale Nashville, TN: Vanderbilt University [Google Scholar]
- 88. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation. 2008;17:2407-2423 [DOI] [PubMed] [Google Scholar]
- 89. WebMD ADHD in teens. http://www.webmd.com/add-adhd/guide/adhd-teens Accessed May 22, 2012
- 90. Wigal SB, Gupta S, Guinta D, et al. Reliability and validity of the SKAMP rating scale in a laboratory setting. Psychopharmacol Bull. 1998;34:47-53 [PubMed] [Google Scholar]
- 91. Wigal SB, Gupta S, Guinta D, et al. Reliability and validity of the SKAMP rating scale in a laboratory setting. Psychopharmacol Bull. 1998;34:65-69 [PubMed] [Google Scholar]
- 92. Wolraich ML, Feurer ID, Hannah JN, et al. Obtaining systematic teacher reports of disruptive behavior disorders utilizing DSM-IV. J Abnorm Child Psychol. 1998;26:141-152 [DOI] [PubMed] [Google Scholar]
- 93. Wolraich ML, Wibbelsman CJ, Brown TE, et al. Attention deficit/hyperactivity disorder among adolescents: a review of the diagnosis, treatment, and clinical implications. Pediatrics. 2005;115:1734-1746 [DOI] [PubMed] [Google Scholar]
- 94. Woodruff TJ, Axelrad DA, Kyle AD, et al. Trends in environmentally related childhood illnesses. Pediatrics. 2004;113:1133-1140 [PubMed] [Google Scholar]
- 95. World Anti-Doping Agency (WADA) Medical information to support the decisions of TUECs: ADHD; Version 2.0; May 2011. http://www.wada-ama.org/Documents/Science_Medicine/Medical_info_to_support_TUECs/WADA_Medical_info_ADHD_2.0_EN.pdf Accessed October 25, 2011
- 96. World Anti-Doping Agency World Anti-Doping code. http://www.wada-ama.org/en/World-Anti-Doping-Program/Sports-and-Anti-Doping-Organizations/The-Code/ Accessed June 14, 2012