Abstract
Background:
As injury rates rise in the later stages of sporting activities, a better understanding of lower extremity biomechanics in the later phases of gamelike situations may improve training and injury prevention programs.
Hypothesis:
Lower extremity biomechanics of a drop-jump task (extracted from a principal components analysis) would reveal factors associated with risk of anterior cruciate ligament injury during a 90-minute individualized intermittent exercise protocol (IEP) and for 1 hour following the IEP.
Study Design:
Controlled laboratory study.
Level of Evidence:
Level 4.
Methods:
Fifty-nine athletes (29 women, 30 men) completed 3 sessions. The first session assessed fitness for an IEP designed to simulate the demands of a soccer match. An experimental session assessed drop-jump biomechanics, after a dynamic warm-up, every 15 minutes during the 90-minute IEP, and for 1 hour following the IEP. A control session with no exercise assessed drop-jump performance at the same intervals.
Results:
Two biomechanical factors early in the first half (hip flexion at initial contact and hip loading; ankle loading and knee shear force) decreased at the end of the IEP and into the 60-minute recovery period, while a third factor (knee loading) decreased only during the recovery period (P ≤ 0.05).
Conclusion:
The individualized sport-specific IEP may have more subtle effects on landing biomechanics when compared with short-term, exhaustive fatigue protocols.
Clinical Relevance:
Potentially injurious landing biomechanics may not occur until the later stages of soccer activity.
Keywords: principal components, drop landing, soccer, anterior cruciate ligament
Landing tasks place mechanical demands on the lower extremities and are commonly used in research settings to assess biomechanical risk factors for anterior cruciate ligament (ACL) injury. Changes in fatigue-related processes during extended sporting activity leading to altered landing biomechanics have been implicated as reasons for increased injury risk.23 As injury rates rise in the later portions of sporting activities,15,29 an improved understanding of lower extremity biomechanics in the later phases of gamelike situations may better inform the development of ACL screening and injury prevention programs.
Repetitive exercise may alter lower extremity biomechanics during double-leg landing tasks.3,17,18,22,24 A systematic review of fatigue exercise on single-limb landing biomechanics33 revealed that vertical ground reaction forces and hip and knee moments were reduced when fatigued. The reduction in vertical ground reaction forces and the corresponding reduction in hip and knee moments may be attributed to an adaptive strategy to ensure a safe landing.41 Collectively, it appears that repetitive exercise does affect landing biomechanics. However, the majority of these landing biomechanics studies have used relatively short-term, high-intensity exercise models3,5,8,11,17,18,22,24,28,42 that do not mimic the extended physiologic and biomechanical demands encountered during common court and field sporting activities that incorporate intermittent exercise. The biomechanical changes accompanying these fatiguing conditions may not represent those conditions occurring during more intermittent, sport-specific activity. Exercise protocols have been developed to simulate the extended demands of a soccer match using a treadmill10,12,14,25,30 and overground running protocols.4,39
The purposes of this study were (1) to identify lower extremity biomechanical factors of a drop-jump task (as extracted from a principal components analysis [PCA]) during a 90-minute individualized intermittent exercise protocol (IEP) designed to simulate a soccer match and (2) to examine how such factors change during the course of, as well as 1 hour following, the IEP. We hypothesized that we would be able to identify biomechanical factors comprising correlated variables and that factors which include landing biomechanics commonly associated with being high risk for ACL injury would become more apparent during the latter stages of an IEP, relative to a control session.
Methods
Before participation, participants were informed of study risks and signed a consent form approved by the university’s Institutional Review Board. Participants included 30 men (mean age, 20.3 ± 2.0 years; mean height, 1.79 ± 0.05 m; mean weight, 75.2 ± 7.2 kg) and 29 women (mean age, 20.5 ± 2.3 years; mean height, 1.67 ± 0.08 m; mean weight, 61.8 ± 9.0 kg), all intercollegiate and club sport athletes who participated in a larger study examining performance, biomechanical, and knee laxity changes during an IEP designed to simulate a soccer match.37,38 All participants consistently engaged in competitive sport activities that included running, cutting, and landing maneuvers for the past 5 years; were currently active a minimum of 6 hours per week; were injury-free for the past 6 months; and had no known coexisting medical conditions affecting connective tissue, no vestibular or balance disorders, and no history of knee injury involving the osteochondral surface, ligaments, tendons, capsule, or menisci (Table 1). The preferred stance limb in kicking (left leg for all participants) was utilized for biomechanical analyses. For the 48 hours before testing days, participants were instructed to (1) avoid moderate to strenuous activity, (2) maintain common dietary habits, and (3) avoid consuming alcohol. On test days, they were asked to refrain from exercise before testing. All testing for women was completed during the first 10 days of their menstrual cycle.
Table 1.
Participants’ sporting backgrounds and testing results
| Women |
Men |
|||
|---|---|---|---|---|
| Sport | No. | YYIR1, m | No. | YYIR1, m |
| Basketball | 7 | 760 ± 226 | 8 | 1340 ± 555 |
| Football | 0 | 1 | 960 | |
| Lacrosse | 0 | 4 | 1110 ± 182 | |
| Rugby | 1 | 520 | 1 | 1160 |
| Soccer | 16 | 992.5 ± 318 | 10 | 1600 ± 376 |
| Tennis | 2 | 480 ± 56 | 1 | 1840 |
| Ultimate Frisbee | 2 | 640 ± 0 | 3 | 1253 ± 260.3 |
| Volleyball | 1 | 600 | 2 | 1460 ± 380 |
YYIR1, Yo-Yo Intermittent Recovery Test–Level 1.
Testing Protocol
Participants first attended a familiarization session and completed a 15-minute dynamic flexibility warm-up, followed by performance of the Yo-Yo Intermittent Recovery Test–Level 1 (YYIR1).20 The YYIR1 was used to assess fitness level and prescribe submaximal IEP running speeds (Table 1). Following the YYIR1, participants were familiarized to all study procedures, including their prescribed running speeds. They were scheduled for control and experimental test sessions (order counterbalanced equally among men and women), spaced 3 to 4 days apart at the same time of day.
On the experimental day, participants were first instrumented using a cluster technique with 3 optical LED markers (PhaseSpace, San Leandro, California) on the left foot, left shank, left thigh, and sacrum. The knee joint center was calculated as the center of the medial and lateral femoral epicondyles.36 The ankle joint center was calculated as the center of the medial and lateral malleoli.36 The hip center was calculated using the rotational method.21 The foot, shank, and thigh local coordinate systems were defined by first creating a long axis (Y) of each segment, as established through the previously defined joint centers (foot distal point defined as the end of second ray). While in anatomical position, 2 axes orthogonal to the long axis were established: one parallel to the anterior-posterior plane (X) and another parallel to the medial-lateral planes (Z). The pelvic coordinate system was created by first defining the long axis (Y) as the vector that points directly downward in the global reference frame when the person is standing in the anatomic position, with the remaining 2 defined similarly to the other segments.
Once instrumented, participants completed the same dynamic warm-up, followed by the IEP. The IEP was designed to simulate the physiologic and biomechanical demands of a soccer match (an intermittent exercise sport) with two 45-minute halves and a 20-minute halftime intermission.4 The IEP was performed as an intermittent shuttle run consisting of alternating 6-second intervals of submaximal running at randomized, varying intensities (standing, walking, jogging, low-intensity running, moderate-intensity running, high-intensity running, and sprinting), followed by 6 seconds of walking and standing. The varying intensities were accomplished by increasing or decreasing the distances covered in each 6-second interval. The relative distances covered in each interval were based on performance of the YYIR1. Investigators were present for all interval running to ensure that the appropriate distances were covered in each 6-second interval. Each 15-minute exercise segment included 2 consecutive sets of a 6-minute submaximal down-and-back shuttle run, plus 2 maximal 505 agility sprint trials (1 off each leg),9 which were followed by 2 countermovement jumps, 3 drop-jump landings,36 and 4 single-leg perturbation trials.34 Knee laxity testing then followed each 15-minute exercise segment (approximately 90 seconds). With the exception of the laxity measures, all functional testing activities were integrated into the IEP to mimic the stretch-shortening cycle work characteristic of field- and court-based sports. Following each 15-minute segment, ratings of perceived exertion were acquired to ensure a high level of effort was achieved. Prior validation of the IEP (Division I soccer) ranked it on a scale from 0 (nothing like a match) to 10 (exactly like a match).5 A subjective rating of 8.7 ± 0.6 suggested that the IEP effectively replicated the demands of a soccer match.5
Lower extremity biomechanics were assessed during the bilateral drop-jump landings from a height of 0.45 m. Participants began with their hands held at shoulder level and their toes aligned along the leading edge of the platform. Then they dropped down, landed evenly on both feet (left foot centered on the force plate), and immediately performed a maximal-effort double-leg vertical jump upon landing. Data from the larger project regarding laxity were reported previously.37,38 Testing time to complete all functional and laxity testing from the end of the 505 sprint trials to the start of the next running block was recorded (5 minutes, 3 seconds ± 1 minute, 1 second). An 8-camera optical system (PhaseSpace) captured DJ kinematics (240 Hz), while force-plate data (type 4060-130; Bertec Corporation, Columbus, Ohio) were simultaneously obtained at 1000 Hz on the testing limb.
A total of 12 testing time points assessed landing biomechanics from post-warm-up (0:00) to every 15 minutes during the IEP (0:15, 0:30, 0:45, posthalf, 0:60, 0:75, 0:90) and every 15 minutes for 1 hour following the IEP (0:15r, 0:30r, 0:45r, 0:60r). During the 1-hour recovery period, participants rested quietly in a seated position between testing segments. To assess potential migration of kinematic markers, measurement consistency and precision of the kinematic model derived from LED markers were tested by having 52 participants actively assume a neutral stance after the warm-up and at completion of the 90-minute exercise challenge. Neutral stance hip, knee, and ankle joint angles were calculated at each time point.
The control day consisted of the same instrumentation and biomechanical methods as the experimental session. Participants were again instrumented and digitized before the dynamic flexibility warm-up. During each 12-minute segment, where intermittent running took place during the experimental session, participants were seated at a table in the laboratory. Otherwise, all testing procedures, with the exception of 505 sprints (because of the potential risk of injury in performing a maximal sprint with no prior activity or active warming), were identical to what was utilized during the experimental testing session.
Data Reduction
Drop-jump biomechanical data were processed and modeled with Motion Monitor software (Innovative Sports Training, Chicago, Illinois). All biomechanical drop-jump data were calculated from foot contact to peak center of mass displacement and then averaged over the 3 trials. Kinematic and kinetic data were processed using a fourth-order, zero-lag, 12-Hz low-pass Butterworth filter. The reference system used for kinematic data was established for each segment, with the positive Z-axis defined as the left-to-right axis, the positive Y-axis defined as the distal-to-proximal vertical axis, and the positive X-axis defined as the posterior-anterior axis. Sagittal, frontal, and transverse hip and knee and sagittal ankle angles (initial, peak, and excursion) were calculated using Euler angle definitions with a rotational sequence of Z Y′ X′′. Peak vertical ground reaction force was normalized to body weight (%BW). Sagittal, frontal, and transverse hip and knee and sagittal ankle peak internal moments (Nm × BW-1 × Ht-1) were calculated using inverse dynamics solutions in a distal segment reference frame from foot contact to peak center of mass displacement. Hip, knee, and ankle negative sagittal powers were calculated and subsequently integrated to calculate energy absorption (J × BW-1 × Ht-1). Hip, knee, and ankle sagittal stiffness were calculated by peak moment divided by excursion (Nm × deg-1). Peak anterior knee shear force was normalized to body weight (%BW). For all analyses, moments, energy absorption, and stiffness were normalized to body weight (N) × height (m). A total of 40 lower biomechanical variables were calculated.
Statistical Analyses
Intraclass correlation coefficient 2,1 and standard error of measurement were calculated from hip, knee, and ankle kinematic neutral stance data from 0:00 to 0:90. A PCA using the covariance matrix was performed (SPSS 20; IBM, Armonk, New York) on the biomechanical dependent variables obtained from the drop jumps for all time points on the experimental test day. The purpose of the PCA was to reduce a relatively large number of correlated biomechanical variables into a smaller number of independent factors31 to more efficiently characterize exercise-related changes in landing biomechanics within each person. With an Oblimin rotation, the original loading pattern matrix was rotated to aid in interpretation. The number of principal components in the pattern matrix extracted by the PCA was chosen to account for approximately 80% of the variance while considering the interpretation of each component. To help identify coherent factor structure, only the loadings of individual biomechanical variables that were relatively larger for each factor were interpreted. The same factors were then extracted from the biomechanical drop-jump data collected during the control session.
We examined changes in each biomechanical factor extracted from the PCA during and following the IEP using a multivariate analysis of variance: condition (experimental/control) × sex (women/men) × time (12 time points). Given the widespread understanding of sex differences in landing biomechanics, we included sex in the model to determine if there were sex-specific changes in biomechanics during the IEP. Where the analysis was significant (used initially to control for type I error), univariate tests for each biomechanical factor were explored. Tukey post hoc tests were used, and statistical significance was set at P ≤ 0.05.
Results
Neutral-stance hip, knee, and ankle kinematic intraclass correlation coefficient 2,1 ranged from 0.61 to 0.87 (mean, 0.76), while standard error of measurement ranged from 1.4° to 4.4° (mean, 2.4°). Participants reported ratings of perceived exertion of 13.8 ± 2.1 and 14.9 ± 2.3 at the end of the first and second halves, respectively. The PCA resulted in a logical factor structure that grouped dependent variables into 11 factors that in total explained 75.2% of the total variance (Table 2). Factors 1 to 6 were specific to sagittal plane variables, whereas factors 7 to 11 were specific to frontal and transverse plane variables.
Table 2.
Extracted factors from principal components analysis, including the relevant discrete biomechanical variables, loading weight, descriptive data, and factor descriptiona
| Factor | Variables | Overall Mean ± SD | Loading Weight | Factor Description |
|---|---|---|---|---|
| 1 | HFpk | 43.6 ± 13.9° | 0.180 | More hip flexion motion and energy absorption |
| HFex | 35.2 ± 10.7° | 0.270 | ||
| Hwa | 0.01 ± 0.01, J × BW-1 × Ht-1 × 10-3 | 0.431 | ||
| 2 | Hfin | 8.5 ± 7.7° | 0.188 | Greater initial hip flexion and hip loading |
| HFmom | 0.10 ± 0.03, Nm × BW | 0.219 | ||
| Hk | 3.1 ± 1.5, Nm × BW | 0.347 | ||
| 3 | KFpk | 87.1 ± 10.8° | 0.235 | More knee and ankle flexion with more knee energy absorption |
| KFex | 75.0 ± 10.6° | 0.288 | ||
| AFpk | 17.2 ± 5.1° | 0.332 | ||
| Kwa | 0.09 ± 0.02, J × BW-1 × Ht-1 | 0.220 | ||
| 4 | AKSF | 0.72 ± 0.12, BW | 0.343 | Greater knee loading |
| GRF | 1.51 ± 0.23, BW | 0.256 | ||
| KFmom | 0.11 ± 0.02, Nm × BW-1 × Ht-1 | 0.432 | ||
| Kwa | 0.09 ± 0.02, J × BW-1 × Ht-1 | 0.232 | ||
| Kk | 1.6 ± 0.4, Nm × BW-1 × Ht-1 × deg-1 | 0.386 | ||
| 5 | Afin | 42.1 ± 7.0° | 0.433 | More flexed ankle position |
| AFex | 59.3 ± 6.9° | –0.393 | ||
| 6 | AKSF | 0.72 ± 0.12, BW | 0.222 | Greater ankle loading and knee shear |
| AFmom | 0.06 ± 0.02, Nm × BW-1 × Ht-1 | 0.323 | ||
| Awa | –0.03 ± 0.01, J × BW-1 × Ht-1 | 0.253 | ||
| Ak | 1.1 ± 0.4, Nm × BW-1 × Ht-1 × deg-1 × 10-3 | 0.289 | ||
| 7 | HERin | 1.6 ± 5.4° | 0.264 | More initial hip external rotation, knee valgus, and internal rotation with less transverse plane knee motion |
| KVALin | –0.4 ± 5.1° | 0.216 | ||
| KVALpk | 1.8 ± 8.1° | 0.213 | ||
| KERin | 10.2 ± 8.6 | –0.346 | ||
| KERpk | 11.4 ± 8.2° | –0.330 | ||
| KIRex | –19.5 ± 8.9° | 0.282 | ||
| 8 | HADex | −1.6 ± 2.8° | −0.183 | More relative hip adduction and knee valgus motion with less relative hip internal rotation |
| HIRpk | 5.8 ± 7.8° | 0.260 | ||
| HIRex | –7.4 ± 5.8° | 0.264 | ||
| KVARpk | –12.6 ± 9.6° | 0.236 | ||
| KVARex | –12.3 ± 8.2° | 0.324 | ||
| KVALex | 2.1 ± 3.8° | 0.208 | ||
| 9 | KIRpk | −9.3 ± 8.3° | −0.299 | More knee internal rotation motion |
| KIRex | –19.5 ± 8.9° | –0.229 | ||
| 10 | KERex | 1.2 ± 2.0° | 0.694 | More knee external rotation motion |
| 11 | HADmom | −0.03 ± 0.02, Nm × BW-1 × Ht-1 | 0.315 | Less frontal and transverse plane hip and knee loading |
| HERmom | 0.01 ± 0.001, Nm × BW-1 × Ht-1 | –0.225 | ||
| KVARmom | –0.02 ± 0.01, Nm × BW-1 × Ht-1 | 0.411 | ||
| KIRmom | –0.01 ± 0.01, Nm × BW-1 × Ht-1 | 0.251 |
H, hip; K, knee; A, ankle; AD, adduction (–); VAL, valgus (+); VAR, varus (–); ER, external rotation (+); IR, internal rotation (–); F, flexion; in, initial angle; pk, peak angle; ex, excursion; mom, moment; k, stiffness; wa, work absorption; AKSF, anterior knee shear force; GRF, ground reaction force.
All sagittal plane flexion angles, extensor moments, stiffness, and work absorption values are positive (+).
The multivariate analysis of variance revealed a significant condition × time interaction (P ≤ 0.001) when all biomechanical factors were combined. The corresponding condition × time univariate analyses revealed changes in factors 1, 2, 4, and 6. There were decreases in hip motion and work absorption (factor 1) (P = 0.004) for only the control condition from post-warm-up (0:00) to 30 minutes in the first half through all remaining time points (0:30-0:60r) (Figure 1). Initial hip flexion and hip loading (factor 2) decreased (P = 0.003) from the beginning of the first half (0:00-0:15) to the end of the second half through the 60-minute recovery (0:90-0:60r) and decreased from the latter stages of the first half (0:30-0:45) to the 60-minute recovery (0:15r-0:60r), with no changes during the control condition (Figure 2). Knee loading (factor 4) decreased (P ≤ 0.001) during the experimental condition from the first half (0:15-0:30) to the 60-minute recovery period (0:15r-0:60r), with no changes occurring during the control condition (Figure 3). Finally, ankle loading and knee shear forces (factor 6) decreased (P = 0.013) from 0:00 to 0:90 and 0:15r in the experimental condition, with no changes during the control condition (Figure 4). There were no significant interactions involving condition and sex (condition × sex, P = 0.449; condition × sex × time, P = 0.089), nor was there a main effect for condition (P = 0.449).
Figure 1.
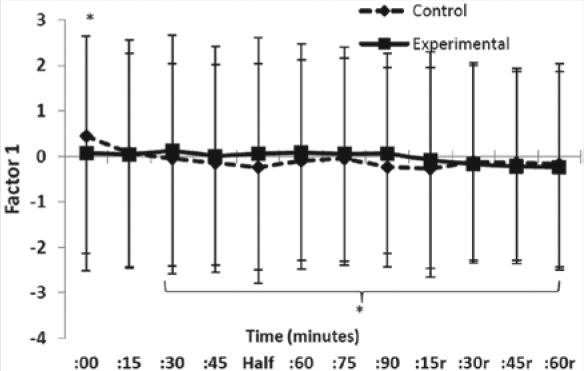
Factor 1 (greater hip flexion motion and corresponding hip energy absorption). Mean ± standard deviation across conditions and time. *In control, 0:00 > 0:30-0:60r, with no change in the experimental condition (P = 0.004).
Figure 2.
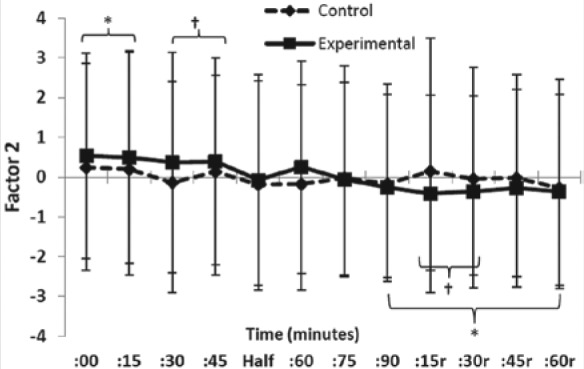
Factor 2 (greater initial hip flexion and greater hip loading). Mean ± standard deviation across conditions and time. *In experimental, 0:00 and 0:15 > 0:90-0:60r; †0:30 and 0:45 > 0:15r and 0:90r, with no change in control (P = 0.003).
Figure 3.
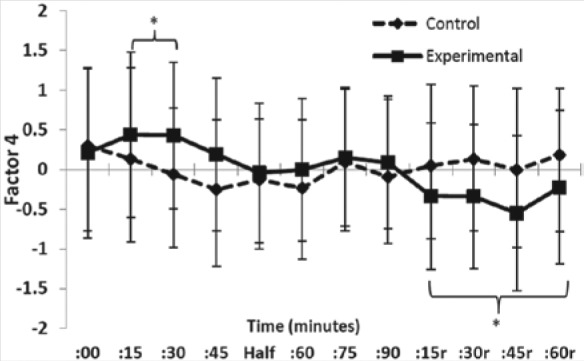
Factor 4 (greater knee loading factor). Mean ± standard deviation across conditions and time. *In experimental, 0:15-0:30 > 0:15r-60r, with no change in control (P ≤ 0.001).
Figure 4.
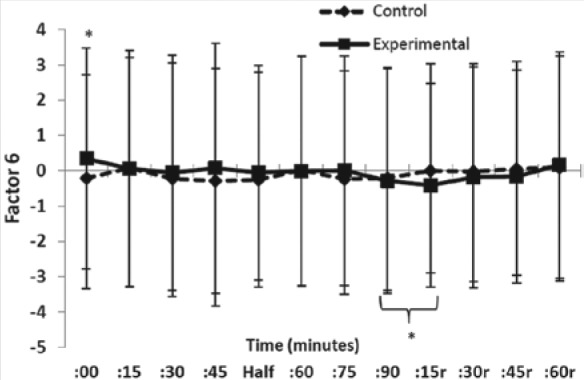
Factor 6 (greater ankle loading and knee shear). Mean ± standard deviation across conditions and time. *In experimental, 0:00 > 0:90 and 0:15r, with no change in control (P = 0.013).
Discussion
Collectively, current results suggest that during an IEP the proximal lower extremity is in a more upright position, in an attempt to decrease the demands placed on the hip, knee, and ankle extensors. Upright landing styles have been associated with ACL injury mechanisms1 and have been characterized as a reduction in shock-attenuating ability of the lower extremity and greater relative quadriceps activation.35 Although it might be posited that landing kinetics would increase in the later stages of activity, a more extended joint position would likely result in a reduction of external force moment arms relative to the joint, thus decreasing peak net extensor internal moment demands.6 While it is still unknown exactly how fatigue directly affects injury mechanisms, there may be a potential that the body attempts to create a more upright landing style to reduce the external joint moments and forces, as previously suggested.41 But if for some reason the body fails to implement this biomechanical strategy because of potentially diminished neuromuscular feedback mechanisms experienced during fatigue,13 there may be a possibility of injury when the body is placed in a potentially injurious position to which it cannot adequately respond. It is acknowledged that recovery testing periods occurred with no warm-up before drop-jump testing. It is possible that, along with recovering from the IEP, the lack of activity during the recovery testing intervals may have affected the drop-jump performance with recovery processes, as warm-up activities are known to positively influence lower extremity power.27
The decrease in hip flexion motion and hip energy absorption in only the control condition may be a function of the dynamic warm-up. A recent systematic review suggested that long-term implementation of dynamic warm-ups can reduce lower extremity injury.16 Greater hip contributions during landing are beneficial with respect to reducing loads on the knee joint,40 and there is potential that the dynamic warm-up in the current study had a beneficial effect on hip function that diminished rapidly when activity ceased.
Comparisons to previous research assessing lower extremity biomechanics during and following sport-specific intermittent exercise are quite limited. A previous study utilizing the same IEP as the current investigation demonstrated that although there were no changes in overall vertical leg spring stiffness (load/displacement before rebound activity) and impedance (load/displacement during landing only) in single-leg jumping and landing tasks, respectively, there were subjective changes in peak vertical ground reaction force and center of mass displacement, respectively.4 A 60-minute shuttle run that was not individually prescribed resulted in changes in cutting kinematics with a more externally rotated hip, knee, and ankle at initial contact as well as greater knee internal rotation during stance phase.32 However, it is difficult to draw direct comparisons between this previous work and the current study due to biomechanical task demands.19,26
The IEP used in the current study differed from the majority of previous exercise protocols that have investigated changes in landing mechanics.3,5,8,11,17,18,22,24,28,42 Our goal was to elicit individualized submaximal fatigue congruous with most sporting situations. Participants perceived the work to be “hard” on the “ratings of perceived exertion” scale; these values are consistent with those of young, elite soccer players following matches and training sessions (14.4 ± 1.2).2 We did not observe significant changes until well into the IEP. The only changes relative to the start of the IEP during the 90 minutes of exercise were decreases in hip loading and hip flexion at initial contact (factor 2) and plantar flexor loading and knee shear force (factor 6), both of which did not occur until the end of the IEP. Previous studies demonstrating changes in double-leg landing biomechanics have used Wingate tests,8 repetitive squatting,18 shuttle exercise including 30-meter sprints and alternating vertical jumps,3 vertical jumping,11,17 step and bounding drills,22 and treadmill running24 as mechanisms to induce neuromuscular fatigue. Consistently, these types of exercise/fatigue models generally took less than 10 to 15 minutes to complete and required exercise intensities in which participants exercised to the point of failure, as defined by predetermined criteria. Thus, the external validity of such protocols must be considered. Given the increase in injury risk with game or practice duration,15,29 gaining a more realistic understanding of biomechanical changes during sport-specific exercise may aid our ability to better understand how ACL injuries occur. It is difficult to compare changes in landing biomechanics experienced during extended intermittent exercise common in a soccer match to relatively short-term exhaustive fatigue protocols.
While previous investigations have reported changes in nonsagittal plane variables in double-leg landing tasks following repetitive exercise,3,5,18,22,28 none of the current factors associated with frontal or transverse plane variables changed during the course of the IEP. This may be once again due to the individualized intensity along with the sport specificity and duration of exercise protocol along with the tested biomechanical task. It is possible that the short-term, relatively high-intensity exercise most commonly used in the fatigue and landing biomechanics literature may have differential planar effects on lower extremity biomechanics. While the current investigation did not demonstrate changes in frontal and transverse plane biomechanics during the IEP, it is important to note that these are average effects. Given the relatively large sample size and large range of factor scores, as evidenced by the standard deviations associated with our factor scores, it is possible that individuals may use different strategies to complete the drop-jump task.
The current findings of decreased hip flexion at initial contact along with decreased hip and knee loading that are still apparent 60 minutes following the exercise protocol may have implications on the timing of subsequent activity, such as 2-a-day practices or a tournament where multiple games are played in a single day.
Of the 59 participants in the current study, 33 participated in intermittent sports other than soccer (Table 1). Participants may have been affected differentially by the IEP based on experience. Such concerns are minimized given that the IEP was individualized per the YYIR1 performance. This study is limited by the lack of data with regard to core body temperature and hydration level, as such variables can confound landing assessment.7 Also, the pelvic anatomic coordinate system used determined the long axis of the pelvis as vertical to the global axis, which does not allow for individual differences in pelvic orientation. However, given the within-subject, repeated-measures design of the current study, such concerns are minimized. While there was also potential for marker cluster movement during the course of the study, our reported neutral-stance reliability and precision across the IEP suggest a satisfactory degree of marker cluster security.
Clinical Relevance
Sagittal plane lower extremity joint biomechanics from a drop jump are altered toward the end of a 90-minute IEP designed to simulate a soccer match, as well as during the 1-hour recovery period. When attempting to best assess potentially injurious mechanisms associated with extended intermittent exercise common to a sport such as soccer, potentially injurious landing biomechanics may not occur until the later stages of activity. Appropriately designing and utilizing an exercise protocol that accounts for the demands of real-world field and court activity may allow for a better understanding of lower extremity biomechanics in the later phases of gamelike situations and may better inform training and injury prevention programs.
Acknowledgments
This study was supported by a grant from the National Football League Medical Charities.
Footnotes
The following authors declared potential conflicts of interest: Randy J. Schmitz, PhD, ATC, John C. Cone, PhD, CSCS, Amanda J. Tritsch, PhD, ATC, Michele L. Pye, MS, ATC, Melissa M. Montgomery, PhD, ATC, and Robert A. Henson, PhD, received funding from a grant from the National Football League Medical Charities; Sandra J. Shultz, PhD, ATC, received a grant from the National Football League Medical Charities.
References
- 1. Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573-578 [DOI] [PubMed] [Google Scholar]
- 2. Brink MS, Nederhof E, Visscher C, Schmikli SL, Lemmink KA. Monitoring load, recovery, and performance in young elite soccer players. J Strength Cond Res. 2010;24:597-603 [DOI] [PubMed] [Google Scholar]
- 3. Chappell JD, Herman DC, Knight BS, Kirkendall DT, Garrett WE, Yu B. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2005;33:1022-1029 [DOI] [PubMed] [Google Scholar]
- 4. Cone JR, Berry NT, Goldfarb AH, et al. Effects of an individualized soccer match simulation on vertical stiffness and impedance. J Strength Cond Res. 2012;26:2027-2036 [DOI] [PubMed] [Google Scholar]
- 5. Cortes N, Quammen D, Lucci S, Greska E, Onate J. A functional agility short-term fatigue protocol changes lower extremity mechanics. J Sports Sci. 2012;30:797-805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Derrick TR. The effects of knee contact angle on impact forces and accelerations. Med Sci Sports Exerc. 2004;36:832-837 [DOI] [PubMed] [Google Scholar]
- 7. Distefano LJ, Casa DJ, Vansumeren MM, et al. Hypohydration and hyperthermia impair neuromuscular control after exercise. Med Sci Sports Exerc. 2013;45:1166-1173 [DOI] [PubMed] [Google Scholar]
- 8. Dominguese DJ, Seegmiller J, Krause BA. Alterations in peak ground-reaction force during 60-cm drop landings caused by a single session of repeated Wingate anaerobic tests. J Sport Rehabil. 2012;21:306-312 [DOI] [PubMed] [Google Scholar]
- 9. Draper JA, Lancaster MG. The 505 test: a test for agility in the horizontal plane. Austr J Sci Med Sport. 1985;17:15-18 [Google Scholar]
- 10. Edwards S, Steele JR, Cook JL, Purdam CR, McGhee DE, Munro BJ. Characterizing patellar tendon loading during the landing phases of a stop-jump task. Scand J Med Sci Sports. 2012;22:2-11 [DOI] [PubMed] [Google Scholar]
- 11. Edwards S, Steele JR, McGhee DE. Does a drop landing represent a whole skill landing and is this moderated by fatigue? Scand J Med Sci Sports. 2010;20:516-523 [DOI] [PubMed] [Google Scholar]
- 12. Gleeson NP, Reilly T, Mercer TH, Rakowski S, Rees D. Influence of acute endurance activity on leg neuromuscular and musculoskeletal performance. Med Sci Sports Exerc. 1998;30:596-608 [DOI] [PubMed] [Google Scholar]
- 13. Gollhofer A, Komi PV, Fujitsuka N, Miyashita M. Fatigue during stretch-shortening cycle exercises: II. Changes in neuromuscular activation patterns of human skeletal muscle. Int J Sports Med. 1987;8(suppl 1):38-47 [PubMed] [Google Scholar]
- 14. Greig MP, McNaughton LR, Lovell RJ. Physiological and mechanical response to soccer-specific intermittent activity and steady-state activity. Res Sports Med. 2006;14:29-52 [DOI] [PubMed] [Google Scholar]
- 15. Hawkins RD, Hulse MA, Wilkinson C, Hodson A, Gibson M. The association football medical research programme: an audit of injuries in professional football. Br J Sports Med. 2001;35:43-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Herman K, Barton C, Malliaras P, Morrissey D. The effectiveness of neuromuscular warm-up strategies, that require no additional equipment, for preventing lower limb injuries during sports participation: a systematic review. BMC Med. 2012;10:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. James CR, Dufek JS, Bates BT. Effects of stretch shortening cycle exercise fatigue on stress fracture injury risk during landing. Res Q Exerc Sport. 2006;77:1-13 [DOI] [PubMed] [Google Scholar]
- 18. Kernozek TW, Torry MR, Iwasaki M. Gender differences in lower extremity landing mechanics caused by neuromuscular fatigue. Am J Sports Med. 2008;36:554-565 [DOI] [PubMed] [Google Scholar]
- 19. Kristianslund E, Krosshaug T. Comparison of drop jumps and sport-specific sidestep cutting: implications for anterior cruciate ligament injury risk screening. Am J Sports Med. 2013;41:684-688 [DOI] [PubMed] [Google Scholar]
- 20. Krustrup P, Mohr M, Amstrup T, et al. The Yo-Yo Intermittent Recovery Test: physiological response, reliability, and validity. Med Sci Sports Exerc. 2003;35:697-705 [DOI] [PubMed] [Google Scholar]
- 21. Leardini A, Cappozzo A, Catani F, et al. Validation of a functional method for the estimation of hip joint centre location. J Biomech. 1999;32:99-103 [DOI] [PubMed] [Google Scholar]
- 22. McLean SG, Fellin RE, Suedekum N, Calabrese G, Passerallo A, Joy S. Impact of fatigue on gender-based high-risk landing strategies. Med Sci Sports Exerc. 2007;39:502-514 [DOI] [PubMed] [Google Scholar]
- 23. McLean SG, Samorezov JE. Fatigue-induced ACL injury risk stems from a degradation in central control. Med Sci Sports Exerc. 2009;41:1661-1672 [DOI] [PubMed] [Google Scholar]
- 24. Moran KA, Marshall BM. Effect of fatigue on tibial impact accelerations and knee kinematics in drop jumps. Med Sci Sports Exerc. 2006;38:1836-1842 [DOI] [PubMed] [Google Scholar]
- 25. Oliver JL, Armstrong N, Williams CA. Reliability and validity of a soccer-specific test of prolonged repeated-sprint ability. Int J Sports Physiol Perform. 2007;2:137-149 [DOI] [PubMed] [Google Scholar]
- 26. Pappas E, Hagins M, Sheikhzadeh A, Nordin M, Rose D. Biomechanical differences between unilateral and bilateral landings from a jump: gender differences. Clin J Sport Med. 2007;17:263-268 [DOI] [PubMed] [Google Scholar]
- 27. Perrier ET, Pavol MJ, Hoffman MA. The acute effects of a warm-up including static or dynamic stretching on countermovement jump height, reaction time, and flexibility. J Strength Cond Res. 2011;25:1925-1931 [DOI] [PubMed] [Google Scholar]
- 28. Quammen D, Cortes N, Van Lunen BL, Lucci S, Ringleb SI, Onate J. Two different fatigue protocols and lower extremity motion patterns during a stop-jump task. J Athl Train. 2012;47:32-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rahnama N, Reilly T, Lees A. Injury risk associated with playing actions during competitive soccer. Br J Sports Med. 2002;36:354-359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rahnama N, Reilly T, Lees A, Graham-Smith P. Muscle fatigue induced by exercise simulating the work rate of competitive soccer. J Sports Sci. 2003;21:933-942 [DOI] [PubMed] [Google Scholar]
- 31. Salaj S, Markovic G. Specificity of jumping, sprinting, and quick change-of-direction motor abilities. J Strength Cond Res. 2011;25:1249-1255 [DOI] [PubMed] [Google Scholar]
- 32. Sanna G, O’Connor KM. Fatigue-related changes in stance leg mechanics during sidestep cutting maneuvers. Clin Biomech (Bristol, Avon). 2008;23:946-954 [DOI] [PubMed] [Google Scholar]
- 33. Santamaria LJ, Webster KE. The effect of fatigue on lower-limb biomechanics during single-limb landings: a systematic review. J Orthop Sports Phys Ther. 2010;40:464-473 [DOI] [PubMed] [Google Scholar]
- 34. Schmitz RJ, Shultz SJ, Kulas AS, Windley TC, Perrin DH. Kinematic analysis of functional lower body perturbations. Clin Biomech (Bristol, Avon). 2004;19:1032-1039 [DOI] [PubMed] [Google Scholar]
- 35. Shimokochi Y, Ambegaonkar JP, Meyer EG, Lee SY, Shultz SJ. Changing sagittal plane body position during single-leg landings influences the risk of non-contact anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2013;21:888-897 [DOI] [PubMed] [Google Scholar]
- 36. Shultz SJ, Nguyen AD, Leonard MD, Schmitz RJ. Thigh strength and activation as predictors of knee biomechanics during a drop jump task. Med Sci Sports Exerc. 2009;41:857-866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Shultz SJ, Schmitz RJ, Cone JR, et al. Changes in multi-planar knee laxity during intermittent exercise influence landing biomechanics. In Review. 2013 [Google Scholar]
- 38. Shultz SJ, Schmitz RJ, Cone JR, et al. Multiplanar knee laxity increases during a 90-min intermittent exercise protocol. Med Sci Sports Exerc. 2013;45:1553-1561 [DOI] [PubMed] [Google Scholar]
- 39. Small K, McNaughton LR, Greig M, Lohkamp M, Lovell R. Soccer fatigue, sprinting and hamstring injury risk. Int J Sports Med. 2009;30:573-578 [DOI] [PubMed] [Google Scholar]
- 40. Tsai LC, Powers CM. Increased hip and knee flexion during landing decreases tibiofemoral compressive forces in women who have undergone anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:423-429 [DOI] [PubMed] [Google Scholar]
- 41. Webster KE, Santamaria LJ, McClelland JA, Feller JA. Effect of fatigue on landing biomechanics after anterior cruciate ligament reconstruction surgery. Med Sci Sports Exerc. 2012;44:910-916 [DOI] [PubMed] [Google Scholar]
- 42. Weinhandl JT, Smith JD, Dugan EL. The effects of repetitive drop jumps on impact phase joint kinematics and kinetics. J Appl Biomech. 2011;27:108-115 [DOI] [PubMed] [Google Scholar]


