Abstract
Background:
Two of the most common causes of groin pain in athletes are femoroacetabular impingement (FAI) and athletic pubalgia. An association between the 2 is apparent, but the prevalence of radiographic signs of FAI in patients undergoing athletic pubalgia surgery remains unknown. The purpose of this study was to determine the prevalence of radiologic signs of FAI in patients with athletic pubalgia.
Hypothesis:
We hypothesized that patients with athletic pubalgia would have a high prevalence of underlying FAI.
Study Design:
Case series.
Level of Evidence:
Level 4.
Methods:
A retrospective review of all patients evaluated at our institution with athletic pubalgia who underwent surgical treatment (ie, for sports hernia) from 1999 to 2011 was performed. The radiographs of patients with athletic pubalgia were reviewed for radiographic signs of FAI. Alpha angles were measured using frog-leg lateral radiographs. Pincer lesions were identified by measuring the lateral center-edge angle and identifying the presence of a “crossover” sign on anteroposterior radiographs. Phone follow-up was performed 2 years or more after the initial sports hernia surgery to evaluate recurrent symptoms.
Results:
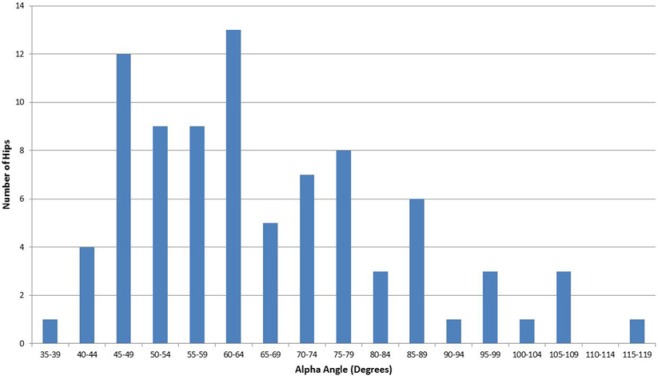
Forty-three patients underwent 56 athletic pubalgia surgeries. Radiographic evidence of FAI was identified in at least 1 hip in 37 of 43 patients (86%). Cam lesions were identified in 83.7% of the population; the alpha angle averaged 66.7° ± 17.9° for all hips. Pincer lesions were present in 28% of the hips. Eight patients had recurrent groin pain, 3 patients had revision athletic pubalgia surgery, and 1 had hip arthroscopy.
Conclusion:
The study demonstrates a high prevalence of radiographic FAI in patients with athletic pubalgia.
Clinical Relevance:
Underlying FAI may be a cause of continued groin pain after athletic pubalgia surgery. Patients with athletic pubalgia should be evaluated closely for FAI.
Keywords: sports hernia, femoroacetabular impingement, athletic pubalgia, alpha angle, center-edge angle
Chronic groin pain in high-level athletes is one of the most difficult problems that a sports physician faces. Groin injuries account for up to 6% of all athletic injuries.1,7,8,15,24 The diagnosis of groin injuries in athletes is difficult because of the multiple anatomic structures that can generate pain. One of the most common causes of groin pain in the athlete is athletic pubalgia. Athletes participating in sports requiring rapid acceleration and deceleration movements and repetitive high-speed twisting and cutting motions, as in soccer, rugby, and ice hockey, are more prone to developing athletic pubalgia.1,13,17,22,24 The incidence of athletic pubalgia in male soccer players ranges from 10% to 18%.18 The cause of athletic pubalgia is not well understood but is often linked to overuse injuries.1,10 Muscle imbalance between the hip adductor and rectus abdominus muscles leading to increased shear stress at the pubic symphysis can cause chronic groin pain and athletic pubalgia.1,10,17,19
Another common cause of groin pain in athletes is femoral acetabular impingement (FAI).6,21 Like athletic pubalgia, FAI has commonly been found in sports that require cutting, pivoting, and accelerating, as in soccer and football.9,24 FAI consists of 2 primary forms: pincer and cam lesions. Pincer lesions represent overcoverage of the femoral head by the acetabulum. This leads to abnormal contact between the femoral neck and the acetabular rim during activities. A cam lesion is an osteochondral bump present at the femoral head-neck junction leading to loss of normal femoral head-neck offset. The most common location for a cam lesion is the anterolateral aspect of the femoral head-neck junction. Cam lesions affect the anterosuperior chondrolabral junction, causing chondrolabral separation and often adjacent acetabular chondral delamination.4 In the setting of a pincer lesion, the labrum is often injured, and cartilage injury is usually limited to a small strip of the cartilage adjacent to the labrum. Although both types of lesions may be present, cam lesions are seen more frequently in young male athletes.4 In the past, athletic pubalgia and FAI were considered 2 independent problems causing groin pain in the athlete. Recent literature has shown that athletic pubalgia and FAI frequently coexist in athletes with chronic hip and groin pain.16,20 Recent studies have shown radiographic signs of FAI to be highly prevalent in high-level athletes.9,12 Although an association between the 2 conditions has been mentioned, no study has specifically determined the radiographic prevalence of FAI in patients treated for athletic pubalgia. The purpose of this study was to determine the prevalence of radiographic signs of FAI in patients with surgically proven athletic pubalgia to help build a foundation in understanding the relationship between FAI and athletic pubalgia.
Methods
Participant Selection
A retrospective review of all patients followed at our institution after athletic pubalgia surgical repair between 1999 and 2011 was performed. Internal review board approval from our institutional review committee was obtained for this study. Each patient’s record was reviewed to identify demographic information and determine the available imaging studies. Patients were included if they had undergone athletic pubalgia surgery and had appropriate imaging that allowed us to evaluate radiographic evidence of FAI. In addition, the patient’s preoperative physical examination was reviewed for signs of impingement, including decreased hip internal rotation with the hip flexed and adducted.
Radiographic Evaluation
Cam lesions were identified by measuring the alpha angle on the frog-leg lateral radiographs.5 The alpha angle on the frog-leg lateral films was measured by drawing a best-fit circle around the femoral head. The point where the femoral head deviated away from this best-fit circle was marked, and a line was drawn from the center of the circle to this point on the perfect circle. The angle was measured between the longitudinal axis of the femoral neck and the line connecting the center of the circle to the point where the head deviates from the best-fit circle (Figure 1). An alpha angle measuring 55° or greater was considered radiographic evidence of a cam FAI.2,3 Acetabular overcoverage was determined by measuring the lateral center-edge angle (CEA) and identifying a “crossover” sign on plain anteroposterior views of the hip. The lateral CEA was formed by a line connecting the lateral edge of the acetabulum with the center of the femoral head and a line perpendicular to that connecting the ischial tuberosities (Figure 2). A lateral CEA of 40° or more was consistent with a pincer lesion and, therefore, FAI.25 A crossover sign was also identified on the anteroposterior radiographs. The anterior and posterior acetabular walls were outlined (Figure 3). The crossover sign, consistent with a pincer lesion, is the extension of the anterior wall lateral to the posterior wall.
Figure 1.

Frog-leg lateral radiograph of a patient with a cam lesion. The alpha angle is measured by drawing a perfect circle around the femoral head and identifying the point where the contour of the femoral head leaves this circle. A line is drawn down the center of the femoral neck and through the center of the perfect circle. A second line is drawn through the center of the circle and through the point where the femoral head leaves the perfect circle. The angle between these 2 lines represents the alpha angle. An angle greater than 55° was considered radiographic evidence of a cam lesion.
Figure 2.

Anteroposterior radiograph of a male athlete with elevated lateral center-edge angle. The lateral center-edge angle was formed by a line connecting the lateral edge of the acetabulum with the center of the femoral head and a line perpendicular to that connecting the ischial tuberosities. A lateral center-edge angle of greater than 40° is typically considered to represent acetabular overcoverage consistent with a pincer lesion.
Figure 3.

Anteroposterior view of a left hip in a patient with a crossover sign. The anterior wall of the acetabulum is outlined in red, while the posterior acetabular wall is outlined in blue. In a hip with typical anteversion, the outline of the anterior wall will remain medial to the outline of the posterior wall. In this patient with acetabular retroversion, the outline of the posterior wall crosses medial to the outline of the anterior wall. This is referred to as the crossover sign.
Telephone Follow-up
Two years or more after athletic pubalgia surgery, patients underwent a phone interview. The data collected from the phone follow-up included current visual analog scale and Tegner activity scores, ability to return to sport, time to return to sport and work, time to feeling “normal,” and recurrent symptoms.
Statistical Analysis
The data are presented as means and standard deviations. Data that were normally distributed were tested using the unpaired Student t test and analysis of variance. For data not normally distributed, a Mann-Whitney U test was used to compare the 2 surgical groups. The chi-square test was used to compare binary data. A test was considered statistically significant if the P value was 0.05 or less.
Results
Demographics
Fifty-three patients underwent surgical treatment for their athletic pubalgia and were followed at our institution from 1999 to 2011. A total of 43 patients (81%) with 56 sports hernias had appropriate imaging to evaluate for FAI and were included in the study. The 10 patients excluded from the study did not have imaging available to review (4 patients) nor had imaging limited to sonography of the groin (6 patients) that did not allow evaluation of FAI. Anteroposterior and frog-leg lateral radiographs were available for all included patients. The study consisted of 42 male patients and 1 female patient. The mean age was 22.3 years (range, 17-46 years). The study included 34 collegiate athletes, 3 high school athletes, 2 competitive club athletes, 3 recreational athletes, and 1 collegiate soccer coach who was a former player (Table 1).
Table 1.
Demographics of study participants
| Patients | ||
|---|---|---|
| No. | % | |
| Athletic pubalgia surgery | ||
| Right | 24 | |
| Left | 32 | |
| Bilateral | 13 | |
| Sport | ||
| Soccer | 15 | 34.8 |
| Football | 6 | 14 |
| Basketball | 6 | 14 |
| Lacrosse | 4 | 9.3 |
| Track | 4 | 9.3 |
| Runner | 3 | 7 |
| Volleyball | 1 | 2.3 |
| Tennis | 1 | 2.3 |
| Ice skating | 1 | 2.3 |
| Hockey | 1 | 2.3 |
| Baseball | 1 | 2.3 |
| Level | ||
| Collegiate | 34 | 79.1 |
| High school | 3 | 7 |
| Recreational | 3 | 7 |
| Club | 2 | 4.7 |
| Coach | 1 | 2.3 |
Radiographic Findings
At least 1 radiographic sign of FAI was identified in 37 of 43 patients (86%) (Figure 4). The mean lateral CEA of the hips was 35.2° ± 7.6°. A lateral CEA of greater than 40° was present in 4 patients (9%) (Table 2).
Figure 4.
Alpha angle of each hip in the study. Thirteen patients had alpha angles between 60° and 64°, making this range the most common in our study.
Table 2.
Radiographic findings of the study group
| Mean ± SD | No. (%) | |
|---|---|---|
| Cam lesions | ||
| Average alpha angle | 66.7° ± 17.9° | |
| Right hip alpha angle | 66.9° ± 17° | |
| Left hip alpha angle | 66.5° ± 18.9° | |
| +Cam lesiona | 33 (76.7) | |
| Bilateral cam lesion | 25 (58.1) | |
| Pincer lesions | ||
| +Pincer lesiona | 12 (27.9) | |
| Isolated pincer | 4 (9.3) | |
| Combined cam and pincer | 8 (18.6) | |
| Average center-edge angle | 35.2° ± 7.6° | |
| Right hip center-edge angle | 34.2° ± 7.9° | |
| Left hip center-edge angle | 36.3° ± 7.4° | |
| Elevated center-edge angle (>40°) | 4 (9.3) | |
| “Crossover” sign | 12 (27.9) |
+, positive for.
Clinical Outcome
Of the 43 patients, 28 (65%) were 2 or more years from their primary athletic pubalgia surgery and underwent telephone follow-up, performed at an average of 40 months (range, 24-119 months) from surgery. Of the 28 patients interviewed, 27 (96%) had occasional groin pain that was not present on a daily basis. One patient reported on-and-off groin pain, but his pain did not occur on a daily basis. No patients were taking pain medications to control groin pain. Of the 28 patients available, 22 (79%) were able to return to sports after their surgery. The average time to return to sports was 9.9 ± 6.8 weeks. At the time of follow-up, the average visual analog scale score was 1.3 (range, 0-6). Eighty-six percent (24 of 28) of patients were satisfied with their surgery at the time of follow-up.
Eight patients developed recurrent groin pain in the ipsilateral groin following surgery. Three patients had revision athletic pubalgia surgery on the ipsilateral side because of recurrent pain. Seven of the 8 patients had pelvic MRI available for review. Six of 7 patients had chondrolabral separation (85%). Three patients had labral tears (43%). One developed symptomatic hip pain on the same side as his previous athletic pubalgia surgery. He underwent intra-articular injection to the hip, which resolved his pain, and he elected to undergo hip arthroscopy with pincer resection, labral repair, and femoral osteochondroplasty; his pain resolved following arthroscopy.
The average alpha angle of patients with recurrent groin pain after athletic pubalgia surgery was 75.2° ± 18.5°, while the average alpha angle in patients without recurrent groin pain was 64.7° ± 17.3° (P = 0.03). Six of the 8 patients (75%) with recurrent groin pain had pincer lesions, while 6 of the 35 patients (17%) without recurrent groin pain had pincer lesions (P = 0.02). Sixty-three percent (5 of 8) of patients with recurrent groin pain after surgery had preoperative impingement signs, compared with 31% (11 of 35) of patients without recurrent groin pain (P = 0.15).
Discussion
Eighty-six percent of patients in this cohort with athletic pubalgia had at least 1 radiographic sign of FAI. FAI is associated with groin pain. Ninety-four percent of a patient population with long-standing adductor-related groin pain had radiographic evidence of FAI.24 There is also an association between decreased hip range of motion and chronic groin pain.22,23 This study describes the prevalence of radiographic FAI in patients with surgically proven athletic pubalgia.
The prevalence of radiographic FAI in this study is consistent with the rate of radiographic FAI in high-level athletes.9,12 In 67 Division I football players, the prevalence of FAI based on anteroposterior and frog-leg lateral radiographs was 95% of the 134 hips with a cam or pincer impingement or 77% with 2 or more radiographic findings of FAI.12 In elite male professional soccer players, FAI was found in 72%.9 Cam lesions were present in 68%, while pincer lesions were present in 27%. These findings were similar to our findings of 77% with cam lesions and 30% with pincer lesions in our cohort of athletes treated for sports hernias.
Thirty-seven percent of the patients in this study had preoperative findings of FAI. In these patients, the athletic pubalgia was treated surgically since the symptoms of pain with coughing or sneezing and resisted sit-up with the Valsalva maneuver were the primary complaint. As expected, cam lesions and pincer lesions were both significantly associated with the presence of preoperative impingement signs, with P values of 0.02 and <0.01, respectively (Table 3). Although it did not reach statistical significance, 63% of patients with recurrent symptoms had preoperative signs of anterior impingement, compared with 31% of patients without signs of impingement. The reason for the lack of significance was probably related to the small sample size of 16 patients with preoperative signs of impingement. Of the 5 patients with preoperative impingement signs and recurrent groin pain, 2 had revision hernia repair, and 1 underwent arthroscopic pincer resection, labral repair, and cam resection. In the group without preoperative impingement symptoms, only 3 (11%) developed recurrent symptoms, with 1 of these patients undergoing revision athletic pubalgia surgery. An association was also found between radiographic signs of FAI and the development of recurrent symptoms after athletic pubalgia surgery. The mean alpha angle of patients with recurrent groin pain was 75.2°, which was significantly greater than that of patients without recurrent groin pain, which measured 64.7°. The presence of a pincer lesion was also associated with the development of recurrent groin pain after athletic pubalgia surgery. Pincer lesions were present in 75% of patients with recurrent groin pain after athletic pubalgia surgery, compared with 17% of patients without recurrent pain having pincer lesions. In the 8 patients with recurrent groin pain after athletic pubalgia surgery, 7 had MRI available for review. Intra-articular pathology was identified in each patient, including 6 with chondral-labral separation and 3 with labral tears. These intra-articular lesions could be the source of recurrent pain after the index athletic pubalgia surgery. Only 1 patient had enough pain to undergo intra-articular injection, which did resolve the patient’s pain for several weeks.
Table 3.
Radiographic findings comparing patients with and without preoperative findings of impingement, No. (%)
| Preoperative Anterior Impingement Signs | |||
|---|---|---|---|
| With (n = 16) | Without (n = 27) | P | |
| Average alpha anglea | 71.8° ± 18.4° | 63.6° ± 16.9° | 0.03* |
| +Cam lesionb | 16 (100) | 20 (74.1) | 0.02* |
| Bilateral cam lesions | 9 (56.3) | 16 (59.3) | 0.85 |
| +Pincer lesionsb | 9 (56.3) | 3 (11.1) | < 0.01* |
| Average center-edge anglea | 38° ± 7.9° | 33.1° ± 6.8° | < 0.01* |
| +Center-edge angle (>45°)b | 2 (12.5) | 2 (7.4) | 0.59 |
| “Crossover” sign | 9 (56.3) | 3 (11.1) | 0.01* |
| Combined cam and pincer | 6 (37.5) | 2 (7.4) | < 0.01* |
Mean ± standard deviation.
+, positive for.
P ≤ 0.05.
Larson et al reviewed 37 hips in 31 patients presenting with both intra-articular injuries (eg, labral tears and/or chondral injuries) and athletic pubalgia.16 Sixteen patients were initially treated with athletic pubalgia surgery. Four (25%) were able to return to sports, while 11 eventually required hip arthroscopy for continued intra-articular pain. Alternatively, 8 patients underwent hip arthroscopy as an index procedure, with 4 (50%) returning to sports uninhibited by pain. Thirteen patients underwent hip arthroscopy and athletic pubalgia surgery concomitantly. Of 13 patients undergoing concomitant surgery, 11 were able to return to sports without continued pain. Concurrent or eventual hip arthroscopy and athletic pubalgia surgery improved outcome scores and unrestricted return to sport in 89% of hips with associated intra-articular pathology and athletic pubalgia. Preoperative impingement signs may be a predictor of poor outcome after sports hernia repair alone.
The correlation between sports hernias and FAI points toward a relationship between cam lesions and the kinematics of the hip and pelvis.14 This study found a significantly lower peak hip abduction, frontal plane range of motion, and attenuated pelvic frontal range of motion in patients with cam lesions. There is an association between decreased hip range of motion and adductor injuries in soccer players.11 The decreased range of motion of the hip may lead to increased demand on extra-articular structures, such as the pubic symphysis. Repetitive loading of the pubic symphysis may cause breakdown of the pubic symphysis, leading to reduced mechanical stability and pelvic instability.8 The decreased pelvic stability may stress the surrounding musculature and tear the tendinous insertions.
The major limitation of this review is its retrospective nature. The clinical diagnosis of FAI was made by the patients’ subjective complaints and physical examinations recorded in their records. Another limitation was that the radiographs were reviewed by only 1 orthopaedic surgeon, which limits interobserver reliability.
Conclusion
The prevalence of FAI radiographic signs in athletes treated surgically for athletic pubalgia was 86%. Athletes with underlying FAI may be more prone to develop chronic groin pain and athletic pubalgia. Preoperative signs of impingement are a predictor for poor outcome after surgical repair of athletic pubalgia. FAI may be a cause of continued groin pain after surgery for athletic pubalgia. Patients with athletic pubalgia should be evaluated closely for the presence of FAI.
Footnotes
The authors declared no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533 [DOI] [PubMed] [Google Scholar]
- 2. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012-1018 [DOI] [PubMed] [Google Scholar]
- 3. Bedi A, Chen N, Robertson W, Kelly BT. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24:1135-1145 [DOI] [PubMed] [Google Scholar]
- 4. Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39:7S-13S [DOI] [PubMed] [Google Scholar]
- 5. Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115-121 [DOI] [PubMed] [Google Scholar]
- 6. Fabricant PD, Heyworth BE, Kelly BT. Hip arthroscopy improves symptoms associated with FAI in selected adolescent athletes. Clin Orthop Relat Res. 2012;470:261-269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fon LJ, Spence RA. Sportsman’s hernia. Br J Surg. 2000;87:545-552 [DOI] [PubMed] [Google Scholar]
- 8. Garvey JF, Read JW, Turner A. Sportsman hernia: what can we do? Hernia. 2010;14:17-25 [DOI] [PubMed] [Google Scholar]
- 9. Gerhardt MB, Romero AA, Silvers HJ, Harris DJ, Watanabe D, Mandelbaum BR. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med. 2012;40:584-588 [DOI] [PubMed] [Google Scholar]
- 10. Hackney RG. The sports hernia: a cause of chronic groin pain. Br J Sports Med. 1993;27:58-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ibrahim A, Murrell GA, Knapman P. Adductor strain and hip range of movement in male professional soccer players. J Orthop Surg (Hong Kong). 2007;15:46-49 [DOI] [PubMed] [Google Scholar]
- 12. Kapron AL, Anderson AE, Aoki SK, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS exhibit selection. J Bone Joint Surg Am. 2011;93:e111(1-10). [DOI] [PubMed] [Google Scholar]
- 13. Kavanagh EC, Koulouris G, Ford S, McMahon P, Johnson C, Eustace SJ. MR imaging of groin pain in the athlete. Semin Musculoskelet Radiol. 2006;10:197-207 [DOI] [PubMed] [Google Scholar]
- 14. Kennedy MJ, Lamontagne M, Beaule PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait walking biomechanics of FAI. Gait Posture. 2009;30:41-44 [DOI] [PubMed] [Google Scholar]
- 15. Kluin J, den Hoed PT, van Linschoten R, IJzerman JC, van Steensel CJ. Endoscopic evaluation and treatment of groin pain in the athlete. Am J Sports Med. 2004;32:944-949 [DOI] [PubMed] [Google Scholar]
- 16. Larson CM, Pierce BR, Giveans MR. Treatment of athletes with symptomatic intra-articular hip pathology and athletic pubalgia/sports hernia: a case series. Arthroscopy. 2011;27:768-775 [DOI] [PubMed] [Google Scholar]
- 17. LeBlanc KE, LeBlanc KA. Groin pain in athletes. Hernia. 2003;7:68-71 [DOI] [PubMed] [Google Scholar]
- 18. Minnich JM, Hanks JB, Muschaweck U, Brunt LM, Diduch DR. Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med. 2011;39:1341-1349 [DOI] [PubMed] [Google Scholar]
- 19. Morales-Conde S, Socas M, Barranco A. Sportsmen hernia: what do we know? Hernia. 2010;14:5-15 [DOI] [PubMed] [Google Scholar]
- 20. Nepple JJ, Brophy RH, Matava MJ, Wright RW, Clohisy JC. Radiographic findings of femoroacetabular impingement in National Football League Combine athletes undergoing radiographs for previous hip or groin pain. Arthroscopy. 2012;28:1396-1403 [DOI] [PubMed] [Google Scholar]
- 21. Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38:99-104 [DOI] [PubMed] [Google Scholar]
- 22. Verrall GM, Slavotinek JP, Barnes PG, Esterman A, Oakeshott RD, Spriggins AJ. Hip joint range of motion restriction precedes athletic chronic groin injury. J Sci Med Sport. 2007;10:463-466 [DOI] [PubMed] [Google Scholar]
- 23. Verrall GM, Slavotinek JP, Fon GT, Barnes PG. Outcome of conservative management of athletic chronic groin injury diagnosed as pubic bone stress injury. Am J Sports Med. 2007;35:467-474 [DOI] [PubMed] [Google Scholar]
- 24. Weir A, de Vos RJ, Moen M, Holmich P, Tol JL. Prevalence of radiological signs of femoroacetabular impingement in patients presenting with long-standing adductor-related groin pain. Br J Sports Med. 2011;45:6-9 [DOI] [PubMed] [Google Scholar]
- 25. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand. 1939;(suppl 58):83 [Google Scholar]