Abstract
Context:
In active individuals with femoroacetabular impingement (FAI), the resultant reduction in functional range of motion leads to high impaction loads at terminal ranges. These increased forces result in compensatory effects on bony and soft tissue structures within the hip joint and hemipelvis. An algorithm is useful in evaluating athletes with pre-arthritic, mechanical hip pain and associated compensatory disorders.
Evidence Acquisition:
A literature search was performed by a review of PubMed articles published from 1976 to 2013.
Level of Evidence:
Level 4.
Results:
Increased stresses across the bony hemipelvis result when athletes with FAI attempt to achieve supraphysiologic, terminal ranges of motion (ROM) through the hip joint required for athletic competition. This can manifest as pain within the pubic joint (osteitis pubis), sacroiliac joint, and lumbosacral spine. Subclinical posterior hip instability may result when attempts to increase hip flexion and internal rotation are not compensated for by increased motion through the hemipelvis. Prominence of the anterior inferior iliac spine (AIIS) at the level of the acetabular rim can result in impingement of the anterior hip joint capsule or iliocapsularis muscle origin against the femoral head-neck junction, resulting in a distinct form of mechanical hip impingement (AIIS subspine impingement). Iliopsoas impingement (IPI) has also been described as an etiology for anterior hip pain. IPI results in a typical 3-o’clock labral tear as well as an inflamed capsule in close proximity to the overlying iliopsoas tendon. Injury in athletic pubalgia occurs during high-energy twisting activities in which abnormal hip ROM and resultant pelvic motion lead to shearing across the pubic symphysis.
Conclusion:
Failure to recognize and address concomitant compensatory injury patterns associated with intra-articular hip pathology can result in significant disability and persistent symptoms in athletes with pre-arthritic, mechanical hip pain.
Strength-of-Recommendation Taxonomy (SORT):
B
Keywords: femoroacetabular impingement, compensatory injury, hip, athletic pubalgia, iliopsoas impingement
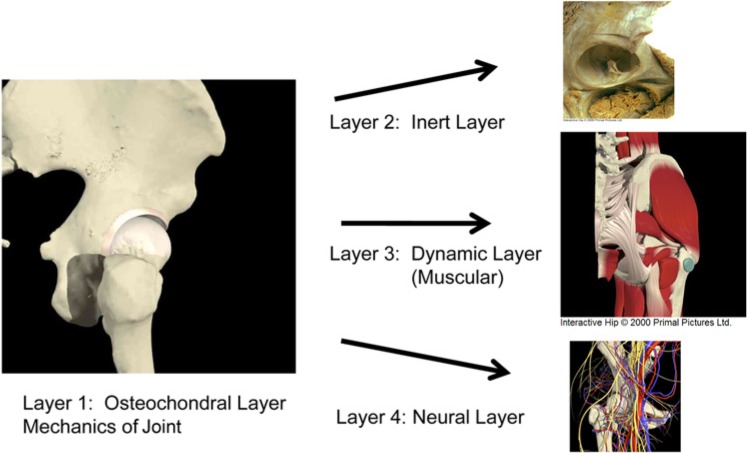
A Layered Approach to Evaluation and Treatment
An algorithmic approach is useful in evaluating the painful hip and associated compensatory disorders in a comprehensive and systematic way (Figure 1). It is termed the “layered approach” to understanding the underlying etiologic factors contributing to pain around the hip joint and associated hemipelvis. It begins with layer 1, which is the osteochondral layer. The structures within this layer are the femur, pelvis, and acetabulum. In the normal hip, these structures provide joint congruence and normal joint kinematics. Abnormalities within this layer can be subdivided into 3 distinct categories: (1) static overload, (2) dynamic impingement, and (3) dynamic instability. Structural variations resulting in static overload include lateral or anterior acetabular undercoverage/dysplasia, femoral anteversion, and femoral valgus. These structural mechanics lead to abnormal stress and asymmetric loads between the femoral head and acetabular socket in the axially loaded position (ie, standing). Dynamic factors may contribute to hip pain as abnormal stress and contact between the femoral head and acetabular rim occur with hip motion. Different morphologies within layer 1 that may contribute to dynamic impingement include femoroacetabular impingement (FAI; cam and rim impingement), femoral retroversion, and femoral varus. When the functional range of motion (ROM) required to compete in sports is greater than the physiologic motion allowed by the hip, a compensatory increase in motion may be provided through layer 1. This involves increased motion and resultant stresses through the sacroiliac (SI) joint, pubic symphysis, and lumbar spine. When functional ROM requirements are greater than physiologic motion limits, forceful anterior contact occurring at the end range of internal rotation may lead to dynamic instability in the form of subtle posterior hip subluxation, which occurs as the femoral head levers out of the hip socket (Krych AJ, Larson CM, Byrd TW, Warren RF, Kelly BT. “Low energy posterior wall fractures in athletes: evidence of cam induced posterio hip subluxation.” Presented at the NFL Combine Physicians Society Meeting, 2011).
Figure 1.
Layered, anatomic approach to the hip.
These mechanical stresses lead to reactive hip pain related to insufficient congruency or impingement between the head and socket, leading to asymmetric wear of the chondral surfaces of the acetabulum and femoral head with or without associated instability of the hip. Thus, layer 1 has a direct effect on the inert layer of the hip, or layer 2. Structures within the inert layer include the labrum, joint capsule, ligamentous complex, and ligamentum teres. These structures contribute to static stability of the hip joint. When abnormal mechanical stresses are applied to the hip joint secondary to underlying abnormalities within layer 1, pathologies such as labral injury, ligamentum teres tear, capsular instability, and various ligament tears can result. Direct injury to layer 2 structures can be predicted based on the underlying structural morphology and mechanics of layer 1, combined with the forces that are generated through the joint and ROM requirements of the joint that are specific to the activities and demands of the individual athlete.
Layer 3 is the contractile layer of the hip and hemipelvis. It includes all musculature around the hemipelvis, including the lumbosacral and pelvic floor. This layer is responsible for the dynamic stability and muscular balance of the hip, pelvis, and trunk. Abnormal mechanics within layer 1 can lead to increased stresses of the SI joint, pubic symphysis, and ischium and secondary increases in the strains imparted to the muscles that attach to these pelvic structures. Enthesopathies and/or tendinopathies can result in a variety of peri-articular muscular structures and can be subcategorized based on their position relative to the hip joint (anterior, medial, posterior, and lateral). Anterior enthesopathy includes hip flexor and psoas impingement and strains. Medial enthesopathy encompasses adductor and rectus tendinopathies, which are often included in “sports hernia” or athletic pubalgia. Posterior enthesopathies include mainly proximal hamstring strains. Injuries to the short external rotators, including the piriformis, may involve a constellation of pain patterns called “deep gluteal syndrome,” involving posterior soft tissue injury and irritation or compression of the sciatic nerve. Lateral enthesopathies involve the peritrochanteric space and injuries to the gluteus medius and minimus tendons. Specific patterns of pathology exist, with layer 1 morphologic abnormalities associated with specific compensatory injury patterns within layer 3. One example is the classic male FAI pattern with large cam lesion and decreased internal rotation. The constellation of symptoms seen with this common FAI pattern include: decreased functional ROM of the hip in flexion and internal rotation (layer 1), direct injury to the labrum and transition zone cartilage within the acetabulum (layer 2), and adductor enthesopathy and athletic pubalgia (medial enthesopathy, layer 3).
Layer 4 is the neurokinetic layer, including the thoracolumbosacral plexus, lumbopelvic tissue, and lower extremity structures. This layer serves as the link and functional control of the entire segment. Compensatory injuries within this layer include nerve compression and pain syndromes, neuromuscular dysfunction, and spine referral patterns. Commonly involved nerves include the ilioinguinal, iliohypogastric, genitofemoral, and pudendal nerves.4,34,37,39,44,50,73
Compensatory Disorders of the Hemipelvis-Osseous Structures
Femoroacetabular impingement results in reduced functional ROM of the hip. With this reduction, achieving the supraphysiologic, terminal ROM required for athletic competition can lead to increased stresses across the entire hemipelvis. These increased forces seen through the pubis, SI joint, and lumbosacral spine lead to compensatory pain disorders. Attempts to increase hip flexion and internal rotation not compensated for by the increased motion through the hemipelvis may also result in subclinical posterior hip instability as the femoral head is levered secondary to anterior engagement between a cam lesion and the anterior acetabulum, resulting in “contra-coup injury” (Figure 2).43
Figure 2.
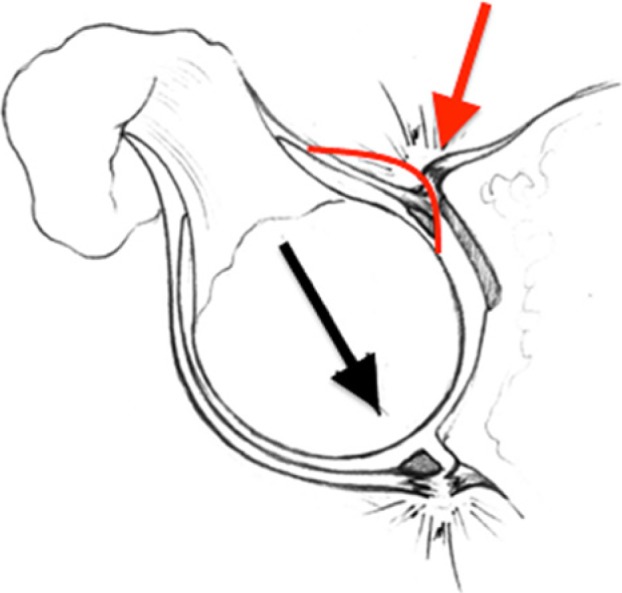
Schematic drawing illustrating typical findings in posterior hip instability in the setting of mechanical impingement from cam lesion (red line) in flexion and internal rotation, including anterior labral injury (red arrow) and posterior capsulolabral lesion (black arrow).
Osteitis Pubis
In athletes, osteitis pubis is an overuse injury to the anterior pelvis.59 It occurs most commonly in twisting, kicking, and pivoting sports such as soccer, Australian-rules football, rugby, ice hockey, and American football.53,59,63,67 The adductor muscles insert at the pubic tubercle and have been implicated in the etiology of the injury.53,59,63,67 Moreover, limited ROM and dysmorphology of the hip joint have been detected in athletes with osteitis pubis as well as in athletes with pubic bone stress injury.66,70
Several investigators have explored the idea that decreases in hip joint ROM may lead to increased biomechanical stress at the pubic symphysis and that these repetitive biomechanical stresses may lead to an overuse injury at the pubic symphysis. In 1978, Williams70 published a study postulating that reduced internal rotation of the hip joint led to shearing stress in the pelvis, which in turn led to anteroposterior movement of 1 hemipelvis in relation to the other during extension, and proximodistal movement in flexion. There is also a significant association between osteitis pubis and the loss of both external and internal ROM in athletes.66
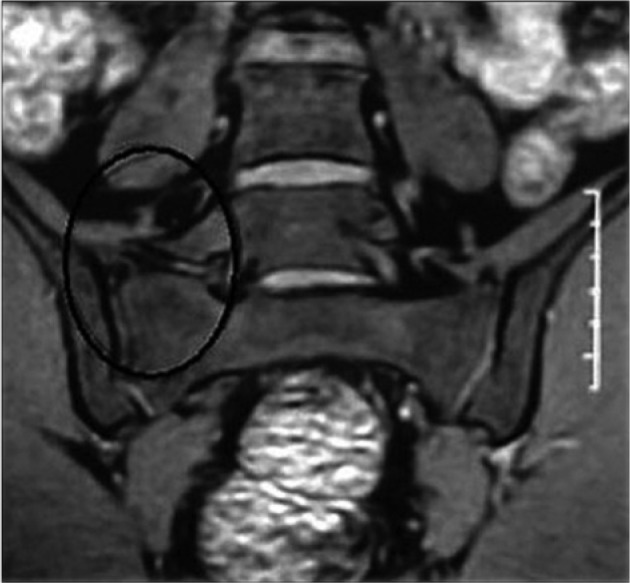
Patients most commonly complain of an insidious onset of unilateral or bilateral pain in the pubic symphysis that may radiate to the groin, lower abdomen, or perineum. Pain can be reproduced with palpation of the pubic symphysis and resisted hip adduction.53,59,63 Radiographs are often normal in the acute setting. Chronic cases may display sclerosis or cystic changes.59 Bone marrow edema at the symphysis can be seen on magnetic resonance imaging (MRI), although its utility in diagnosis has been questioned.53,59,63 In a study of the MRI findings associated with osteitis pubis, bone marrow edema was found in 100% of patients surgically treated, 88% of those treated nonoperatively, and 65% of asymptomatic athletes (Figure 3).53
Figure 3.
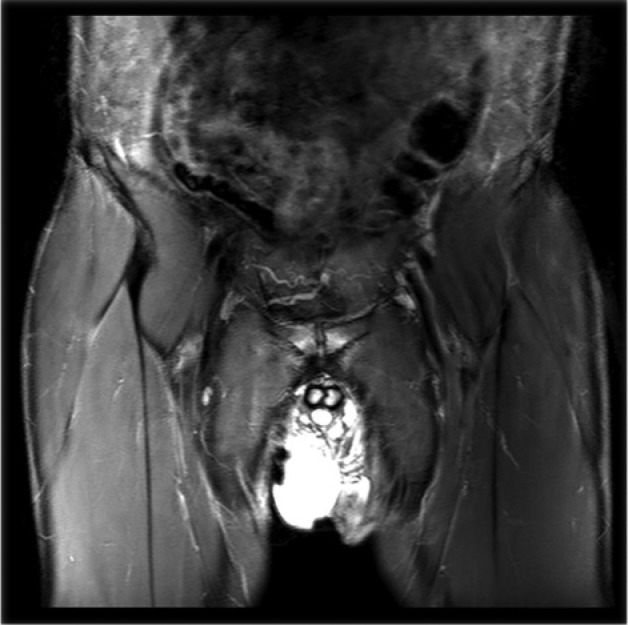
Coronal magnetic resonance imaging STIR (short inversion time inversion recovery) sequence demonstrating edema at the pubic symphysis and findings consistent with osteitis pubis. This 30-year-old man presented with left groin and central pubic pain secondary to femoroacetabular impingement and compensatory motion at the pubic symphysis.
Nonoperative treatment includes nonsteroidal anti-inflammatory drugs, core strengthening, hip ROM therapy, and activity modifications. Local steroid injections may be a diagnostic and therapeutic tool.53,59,63 When conservative measures have failed, surgical treatment has had success.59 An extraperitoneal endoscopic mesh placed behind the symphysis allowed 7 of 8 athletes (88%) to return to sport at 2 months.53 In 23 athletes who underwent open curettage of the pubic symphysis, 21 returned to pain-free running by 3 months, and 78% felt their symptoms were better.59
Sacroiliac Joint
The SI joint is synovial surrounded by a thin capsule, and it is stabilized primarily by thick anterior and posterior ligaments (Figure 4).19 Pain in the SI joint may result from degenerative or inflammatory arthritis, infection, ankylosis, stress fractures, and either hyper- or hypomobility.19 The SI joint is supported by the gluteus maximus and medius, erector spinae, biceps femoris, psoas, piriformis, and oblique and transversus abdominis muscles, transmitting muscular forces from the spine and lower extremities to the pelvis.19 Abnormal motion in the lumbar spine, pubic symphysis, and hip can all lead to increased stress at the SI joint and discomfort. A cross-sectional study of limited hip joint ROM in patients with low back pain and SI joint dysfunction10 showed SI joint dysfunction had significantly more unilateral external hip rotation than internal rotation.
Figure 4.
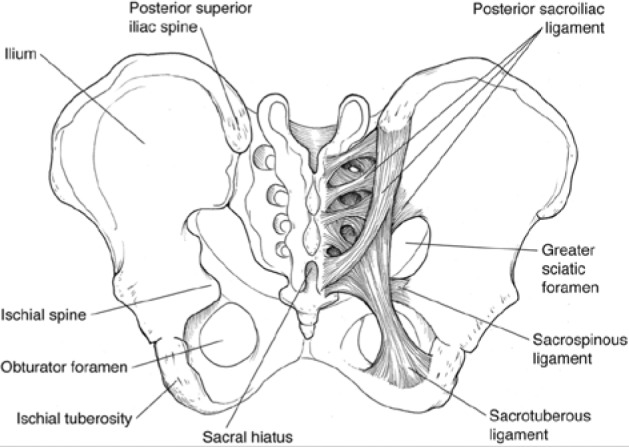
The sacroiliac joint and ligamentous anatomy. Reprinted with permission from the American Academy of Orthopaedic Surgeons.19
Patients commonly complain of pain near the posterior inferior iliac spine, the buttocks, groin, and occasionally radiating into the thigh. It is important to rule out the lumbar spine as the source of pathology. On examination, palpation of the posterior SI joint may elicit pain. Provocative tests involving rotation of the ipsilateral hip may reproduce symptoms,19,65 further reinforcing the concept that functional ROM of the hip beyond the anatomic constraints can lead to increased stresses across the entire hemipelvis and through the SI joint.
Treatment consists of physical therapy focusing on posture, core muscle strength, and ROM. Oral anti-inflammatory medications and corticosteroid injections may be both diagnostic and therapeutic when other modalities have failed.63 Arthrodesis of the SI joint has been described in only very refractory cases of severe joint dysfunction and degeneration.19,63,65
Lumbar Spine
Low back pain in the athlete is common and often difficult to diagnose and treat.42,65 Athletes with prior low back injuries have a 3 to 6 times greater risk of sustaining further low back injury relative to other athletes.26 Additional risk factors for lumbar spine pain in the athlete include decreased lumbar spine ROM, poor conditioning, excessive or repetitive loading, improper technique, and abrupt increases in training.42 Muscle strain is the most common cause of back pain in athletes, but this diagnosis should be made only after other sources have been excluded. When motion of the hemipelvis is limited, increased strain may occur on the lower back as a source of motion for the extremity. Furthermore, limitations in hip internal rotation are associated with symptomatic lumbar spine pain.12 Stress reactions in the pars interarticularis and posterior facet pain may result and are implicating factors as pain generators.48,61 Posterior element pain is common in twisting and hyperextension sports, such as gymnastics, diving, and football (lineman). Limited motion of the hip may also trigger or exacerbate symptoms from Bertolotti’s syndrome, which is partial sacralization of a transitional fifth lumbar vertebrae. The transitional vertebra transverse process will partially articulate with the sacrum or illium and may become symptomatic with compensatory increases in motion of the hemipelvis in the setting of FAI (Figure 5).16
Figure 5.
Coronal T2-weighted magnetic resonance image of the lumbosacral region demonstrating contact of the right L5 transverse process with the sacrum. Image adapted with permission from the Associação Arquivos de Neuro-Psiquiatria Dr Oswaldo Lange.16
On physical examination, pain is exacerbated with hyperextension of the spine. Diagnostic imaging should be targeted17: standing radiographs, oblique views of the pars interarticularis, and flexion and extension radiographs for dynamic instability.
Posterior Hip Subluxation and Femoroacetabular Impingement
The spectrum of posterior hip instability ranges from subluxation to frank dislocation. The most common traumatic mechanism of injury in athletic competition is a fall on a flexed and adducted hip with a posteriorly directed force.21,49,58 Atraumatic and lower energy mechanisms of hip instability have been reported in American football, skiing, rugby, gymnastics, jogging, basketball, biking, and soccer.2,15,33,55,62,64,69 Laxity in capsular tissue or abnormal bony morphology may predispose the athlete to hip instability (Krych AJ, Larson CM, Byrd TW, Warren RF, Kelly BT. Low energy posterior wall fractures in athletes: evidence of cam induced posterio hip subluxation; 2011.).2,55,58,62,69
In the athlete with FAI, functional ROM required in athletic competition is often greater than the limited physiologic motion allowed by the cam and/or rim impingement lesions. Attempts to increase flexion and internal rotation in competition may result in anterior engagement between the cam lesion and the anterior acetabulum and levering of the femoral head posteriorly, with posterior acetabular rim fracture and posterior capsulolabral tear, analogous to a posterior bony Bankart lesion of the shoulder (Figures 2 and 6).6 Anterior labral tears occur after posterior hip subluxation or dislocation (Krych AJ, Larson CM, Byrd TW, Warren RF, Kelly BT. Low energy posterior wall fractures in athletes: evidence of cam induced posterio hip subluxation; 2011.).21 A labral crush injury can occur where the cam lesion engages the anterior acetabulum and labrum. In certain cases, a posterior hip subluxation or dislocation event may be the first manifestation of occult FAI in competitive athletes.24 In chronic FAI, particularly with a focal rim lesion creating cephalad retroversion (Figure 7), the anterosuperior labrum is typically degenerated, and an associated “contra-coup” pattern of cartilage loss in the posterior capsular-labral junction develops secondary to a distraction force from the femoral head levering out of the hip socket with continued hip flexion.57,72 Increased levering forces during athletic competition could result in a subluxation episode.
Figure 6.
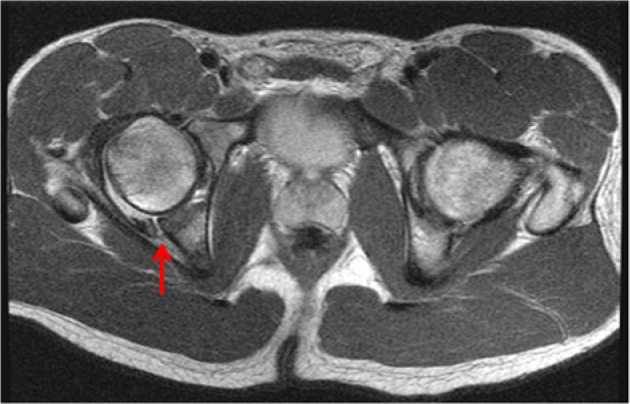
T1-weighted axial image of the pelvis. The anterior loss of femoral offset and mechanical impingement in flexion and internal rotation may predispose to a “levering effect,” resulting in posterior capsulolabral injury (arrow) and secondary instability.
Figure 7.

Anteroposterior radiograph of the hip demonstrating a focal rim lesion (arrow) creating cephalad retroversion.
Patients present with painful limitation of hip motion, often having discomfort in the hip at rest. A high index of suspicion is critical to avoid missing this injury, which is often misdiagnosed as a muscle strain (Krych AJ, Larson CM, Byrd TW, Warren RF, Kelly BT. Low energy posterior wall fractures in athletes: evidence of cam induced posterio hip subluxation; 2011.).2,21,49,55,58,62,69 Posterior subluxation of the hip can be a potentially devastating injury to an athlete and result in avascular necrosis if unrecognized.14
The classic triad after posterior hip subluxation in 8 American football players is hemarthrosis, iliofemoral ligament disruption, and posterior acetabular lip fracture.49 In a series of 22 athletes with a low-energy posterior acetabular rim fracture from a posterior hip instability episode, 18 athletes had underlying FAI (Krych AJ, Larson CM, Byrd TW, Warren RF, Kelly BT. Low energy posterior wall fractures in athletes: evidence of cam induced posterio hip subluxation; 2011.). The most common pathologies were a posterior bony Bankart lesion, anterior labral injury, chondral injury to the femoral head with loose bodies, and ligamentum teres avulsion. In a series of 14 athletes who sustained traumatic hip dislocation, 9 had FAI at arthroscopy.58 Labral tears, ligamentum teres avulsion, and chondral defects were found.58 Five patients (36%) sustained posterior acetabular rim fractures; however, none required arthroscopic repair.
Anterior Inferior Iliac Spine “Subspine” Impingement
Prominence of the anterior inferior iliac spine (AIIS) at the acetabular rim can result in mechanical hip impingement but is entirely distinct from typical cam and focal rim impingement lesions.40 This abnormal morphology of the AIIS may result in decreased space available for soft tissue at the level of the acetabular rim during hip flexion. The result is impingement of anterior tissue (anterior capsule or iliocapsularis muscle origin) against the femoral head-neck junction (Figure 8).
Figure 8.
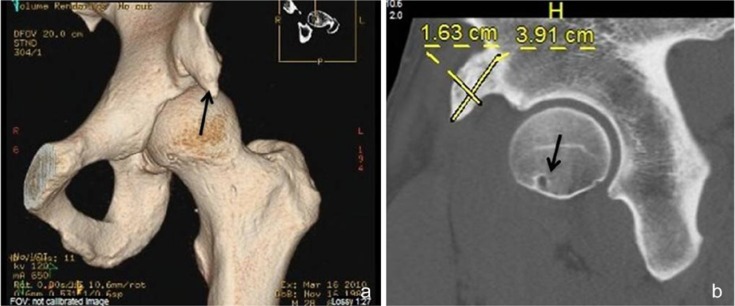
(a) Three-dimensional computed tomography (CT) scan demonstrating prominent anterior inferior iliac spine (AIIS) resulting in subspine impingement and restriction in hip flexion. (b) Sagittal CT image demonstrating AIIS dimensions and point of pathologic contact on the femoral neck (arrow) with terminal flexion and rotation of the hip.
The treatment of AIIS impingement was initially described in a case report of a 30-year-old man presenting with anterior hip pain and limited hip motion nonresponsive to conservative treatment.56 Imaging revealed impingement between the femoral head-neck junction and a prominent AIIS. Surgical resection of the hypertrophic AIIS resulted in resolution of pain and hip function.56
Clinical findings of AIIS “subspine” impingement may mimic a hip flexor strain. Pain is often insidious in onset and exacerbated by deep hip flexion. A bony fragment of the AIIS from a traumatic hip flexor avulsion may displace at or below the level of the acetabulum and ossify in continuity to the pelvis over time. With significant bony impingement from a low-lying AIIS, limitation in hip flexion may be noted. Using computed tomography scans with 3-dimensional reconstructions, the morphology of the AIIS and its location relevant to the superior acetabular rim can be determined.28 Surgical decompression of the AIIS area in patients with signs of FAI and significant AIIS subspine impingement may result in improvement of anterior impingement symptoms.
Associated and Compensatory Peri-Articular Soft Tissue Injury
Hip Flexor Strain
The quadriceps muscle, specifically the rectus femoris, is a common site for muscle strain and avulsion.25,27 The most common site of injury is at the musculotendinous junction.5,27 MRI studies show that the indirect head is the most commonly injured site of the muscle origin.25,52
Avulsion of the rectus femoris is common in the adolescent, skeletally immature population.22,30,45,56 These injuries occur in football, soccer, lacrosse, gymnastics, hockey, dance, and track and field.22,30 Proximal avulsions of the rectus in the adult, skeletally mature population are a less common entity. Several studies have reported the occurrence of proximal rectus avulsions in both professional football and soccer athletes.9,31,68 Muscle-tendon injuries of the lower extremity are common in National Football League (NFL) kickers.9 Eleven proximal rectus femoris avulsions were reported in a study of the NFL Injury Surveillance System.25 Frequently, rectus femoris avulsions in adults or apophyseal avulsions in skeletally immature patients are associated with clinical findings suspicious for underlying FAI.
Hip flexor strains commonly occur as a noncontact injury during either eccentric contraction of the muscle or during high-velocity hip flexion, like the kicking motion.5,27 Athletes often report an acute “pop” and immediate pain in the anterior hip. Ecchymosis and swelling often result. Clinical suspicion is confirmed by tenderness to palpation over the hip flexor origin, occasional step-off, and weakness and/or pain with resisted hip flexion. Assessment of hip rotation and impingement maneuvers provides clues to the involvement of FAI. The association with FAI is based on a protective eccentric contraction of the hip flexor group occurring as the hip ROM exceeds physiologic capacity determined by the mechanical structure.
Treatment of proximal rectus avulsions is almost uniformly conservative, with gradual return to sport as symptoms allow. In the setting of American professional football, proximal avulsions of the rectus femoris can be treated nonoperatively with a high degree of predictability for return to full unrestricted participation.25 Surgical treatment is rarely indicated. In adolescents with a bony apophyseal avulsion, surgical intervention may be warranted for prolonged disability despite rehabilitation or when there is significant displacement of the bony fragment.22,30,31,45,56 In the adult population, surgery may be indicated in the chronic setting where a symptomatic bony exostosis has formed and excision is necessary.
Iliopsoas Impingement and Strain
The iliopsoas muscle acts as one of the main flexors of the hip joint.60 In addition, it prevents hyperextension of the hip during standing. Recent studies also suggest that the iliopsoas contributes to internal rotation at 0° and external rotation at 90° of hip flexion.17
When the hip is in full flexion, the iliopsoas tendon shifts laterally in relation to the center of the femoral head as it crosses the iliopectineal eminence.60 Subsequently, with extension of the hip, the iliopsoas tendon moves medially over the femoral head. This shift of the iliopsoas over the iliopectineal eminence or at the base of the AIIS and femoral head may be the source of internal coxa saltans in many patients.60
Recently, a distinct clinical entity, termed iliopsoas impingement (IPI) has been described as an etiology for anterior hip pain.18,29 IPI is based on the close proximity of the iliopsoas tendon to the capsule and anterior labrum just distal to the iliopectineal eminence. It has been previously described in total hip arthroplasty, where either anterior extrusion of cement or anterior overhang of the acetabular component results in irritation of the iliopsoas tendon.38
In the native hip with IPI, the labral tear occurs at the 3-o’clock position on the acetabulum rather than the typical 12- or 1-o’clock positions seen in classic FAI.18,29 An inflamed capsule and iliopsoas tendon can be visualized during arthroscopy directly overlying the injured labrum (Figure 9).32,38
Figure 9.
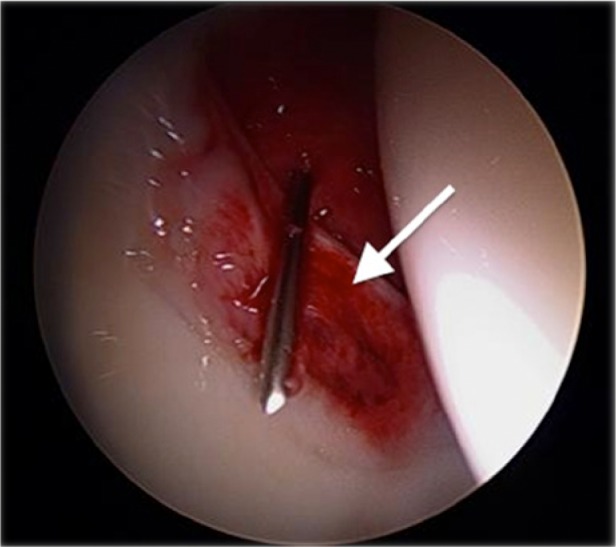
Arthroscopic image demonstrating the iliopsoas impingement sign with inflammation of the capsule and labrum (arrow) in the 3-o’clock position on the acetabulum.
Iliopsoas impingement is a compensatory injury pattern.18,29 Iliopsoas impingement may occur on the anterior labrum during hip motion. The iliopsoas makes an obtuse angle around the iliopectineal eminence and femoral head that increases in hip extension. The resultant pressure and friction exerted on the femoral head and anterior labrum during hip motion may lead to the 3-o’clock labral injury.71 A tight or spastic iliopsoas increases contact pressures beneath the tendon, resulting in IPI.17,18
A second theory involves scarring or adhesion of the iliopsoas to the anterior capsule and labrum resulting in a repetitive traction injury. The normal iliopsoas loses contact with the femoral head at 14° of flexion and the iliopectineal eminence at 54°.17 A chronically inflamed iliopsoas tendon and/or bursa in internal coxa saltans may result in scarring of the tendon to the anterior capsule. This adherence may prevent lift-off from the capsule and lead to a reverse obtuse angle of the tendon in flexion. The adherent tendon would pull on the anterior capsulolabral complex, with contraction of the iliopsoas muscle resulting in the characteristic 3-o’clock tear.
The third theory involves the iliocapsularis muscle that originates on the anterior joint capsule and iliopectineal eminence and inserts slightly distal to the lesser trochanter (Figure 10). Hypertrophy or spasticity of the iliocapsularis may represent an alternative cause of repetitive traction injury on the anterior capsulolabral complex.18,29 The iliocapsularis and iliopsoas are adjacent to one another, and it is possible that the tendon overlying a percentage of the labral injuries seen was that of the iliocapsularis.
Figure 10.
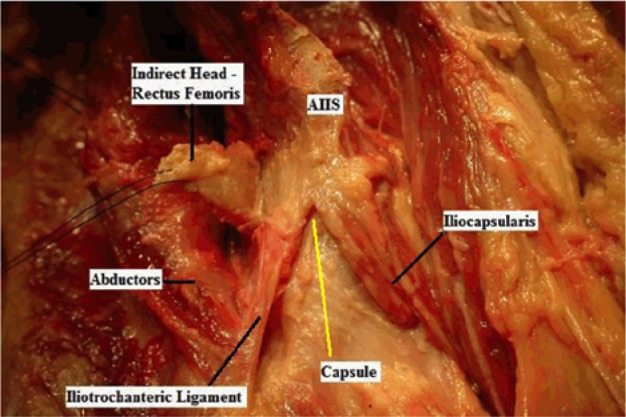
The iliocapsularis muscle, which originates on the anterior joint capsule and iliopectineal eminence and inserts slightly distal to the lesser trochanter. Reprinted with permission from Bedi et al.7
The clinical presentation of IPI is more insidious than that of a rectus femoris injury. Patients often complain of discomfort with repetitive twisting or hip flexion activities. On occasion, the report of a sudden pop in the anterior hip via a noncontact mechanism may occur. Mechanical symptoms may be present as the iliopsoas snaps over the labrum or the torn labrum incarcerates into the joint.
On physical examination, nearly all patients have a positive flexion-adduction–internal rotation (FADIR) impingement test.18 In addition, most patients have focal tenderness over the iliopsoas at the level of the anterior joint line. Focal tenderness, however, is a nonspecific finding and should not be independently used as a diagnostic criterion for IPI.18 Anteroposterior pelvis and elongated neck lateral radiographs are recommended in all patients in addition to an MRI. Initial treatment is uniformly conservative. Physical therapy is recommended for at least 3 to 6 months to focus on hip ROM, strength, and iliopsoas stretching. Selective use of intra-articular and iliopsoas bursa injections provides variable relief.
Hip arthroscopy is considered when conservative measures have failed.10 An ideal surgical candidate has responded well to an iliopsoas injection, has a documented labral tear on MRI, and shows evidence of anterior capsule thickening where the psoas tendon crosses the acetabulum. Labral tears are typically debrided. Occasionally, repair with suture anchors is required. The iliopsoas is lengthened through its tendinous portion (Figure 11).3,18,28 In patients with increased femoral anteversion, the psoas may compress the anterior labrum as it stabilizes the hip joint in external rotation. Fractional lengthening of the iliopsoas in patients with increased femoral anteversion may further destabilize the hip joint.
Figure 11.
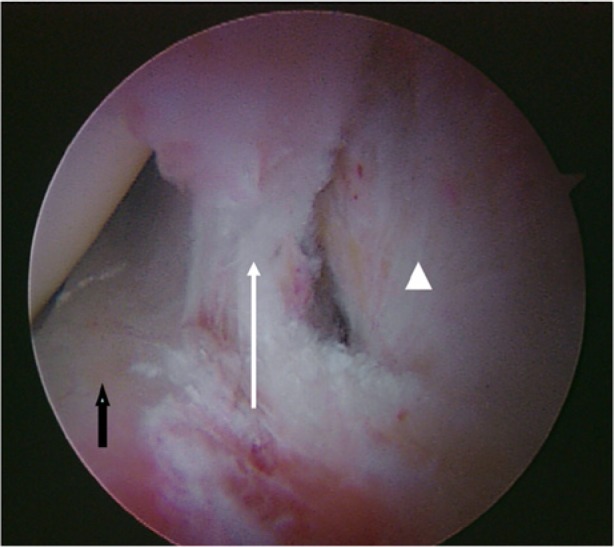
To address a symptomatic iliopsoas tendon via a transcapsular approach, an anterior capsulotomy approximately 1 cm in length is made directly anterior to the labral injury (dark arrow) using the beaver blade or radiofrequency ablation device. Through this capsular window (white arrow), the tendinous portion of the iliopsoas (arrowhead) can be visualized and lengthened.
Proximal Hamstring Syndrome
Posterior mechanical hip pain can result from morphologic bony abnormalities, resulting in bony impingement; abnormal mechanics across the hip joint leading to increased stresses with chronic; symptomatic tendinopathy of the proximal hamstring, as well as from sciatic nerve entrapment.
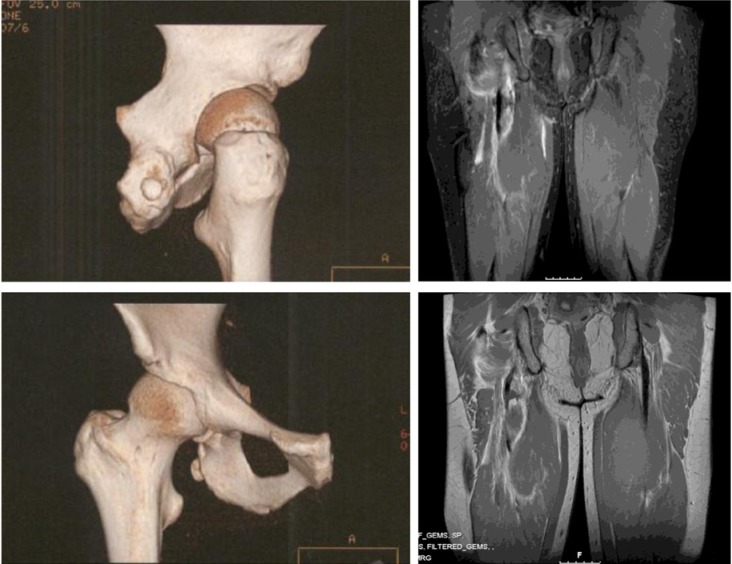
Proximal hamstring tendinopathy, previously reported as hamstring syndrome, is an overuse injury with lower gluteal pain, especially during sports,19,42,54,65 and occurs in athletes in various sports, but especially in sprinters and middle- and long-distance runners.19,42,65 Abnormal bony morphology within the realm of FAI may be implicated in exacerbating proximal hamstring muscle problems in athletes.8,13,23,26,48,61 This compensatory injury pattern is more commonly seen in female patients with a predominant rim impingement morphology. In an attempt to decrease anterior impingement, these patients will develop a compensatory posterior tilt of the pelvis, which leads to chronic hamstring shortening and ultimately predisposing them to chronic hamstring tendinopathy (Figure 12). Surgery may be indicated for the treatment of recalcitrant proximal hamstring tendonitis.8,13,26,48,61
Figure 12.
Posterior pubalgia: proximal hamstring syndrome. Patients with symptomatic femoroacetabular impingement (FAI) and restricted internal rotation may develop a compensatory posterior tilt of the pelvis, which leads to chronic hamstring shortening and predisposition to chronic hamstring tendinopathy. Computed tomography images (left) of the right hip demonstrate FAI and a proximal hamstring avulsion fracture. Coronal magnetic resonance images (right) demonstrate a complete proximal hamstring avulsion with retraction and adjacent hematoma.
Athletic Pubalgia and Adductor Muscle Injury
Athletic pubalgia (AP) is a weakness or tear of the posterior inguinal wall without a clinically recognizable hernia.20 AP pathology may include attenuation of the conjoined tendon, injury at the insertion of the rectus abdominis muscle, avulsion of part of the internal oblique muscle fibers at the pubic tubercle, tearing within the internal oblique muscle fibers at the pubic tubercle, tearing within the internal oblique musculature, or an abnormality in the external oblique aponeurosis.20,46
Athletic pubalgia injury occurs during high-energy twisting activities in which abnormal hip ROM and resultant pelvic motion lead to shearing across the pubic symphysis.20,21,47 The force often comes from trunk hyperextension and thigh hyperabduction in athletes with strong adductor muscles and relatively weak lower abdominal muscles. Pain usually develops insidiously with increasing activity and resolves with rest. Symptoms are exacerbated by sit-ups, kicking, running, and coughing. On examination, pain may be reproduced with resisted hip adduction, a sit-up, or the Valsalva.20,47 No palpable hernia is detected, and tenderness is elicited around the pubic tubercle or posterior inguinal canal. MRI may confirm the diagnosis and other sources of groin pain.
Initial treatment is conservative. When nonoperative measures fail and the athlete is unable to return to sport, open and laparoscopic repairs are available with and without the use of mesh.1,20,35,47 Up to 95% of the athletes who underwent athletic pubalgia operations in one series were able to return to full play within 3 months of surgery.47
Patients with FAI may adopt an alternative motion strategy, recruiting different muscles, with an alteration in hip and pelvic biomechanics during gait as well as competitive play.36 During level gait, cam FAI causes a decrease in peak hip abduction and total frontal ROM, slight reduction in sagittal hip ROM, and attenuated pelvic mobility in the frontal plane.36 It seems unlikely that these altered motions result from mechanical limitations or bony contact at the extremes of motion. This is suggestive of a soft tissue component to FAI that is adaptive in nature to reduce hip pain during ambulation.36 Limited sagittal pelvic ROM occurs in patients with FAI; moreover, patientswith FAI had limited squatting ability.56 Compensatory or adaptive changes in pelvic motion and peri-articular musculature secondary to FAI may precipitate athletic pubalgia symptoms.
In the high-performance athlete, restriction of terminal flexion and internal rotation at the hip joint (as in FAI) results in secondary abnormal motion of the hemipelvis. This motion may be responsible for secondary strain/injury to the central pubic musculature.47 Four of 29 Australian-rules football players developed chronic groin injury (defined by at least 6 weeks of groin pain and missing match playing time) over 2 playing seasons.67 In these 4 athletes, reduced total hip joint ROM(P = 0.03) was associated, suggesting that limitations in hip motion are associated with later development of chronic groin injury and may be a risk factor.
Muscle strain, contusion, intra-articular injury, and sprain are the most common types of hip injuries in the NFL.21 Although these injuries may occur in isolation, a “sports hip triad” (labral tear, adductor strain, and rectus strain) has been detected.21 Thus, intra-articular pathology, such as in FAI, may exacerbate muscle injuries around the pelvis in athletes. Proximal hamstring tendonitis, rectus femoris avulsions, and psoas tendonitis are other causes of groin pain that may have a similar association with FAI.3,11,21,51
A series of athletes (37 hips; mean age, 25 years) treated for symptomatic intra-articular hip pathology and athletic pubalgia illustrates the association of these injuries.41 Hip arthroscopy was performed in 32 hips (30 cases of FAI treatment, 1 traumatic labral tear, and 1 borderline dysplasia). Of 16 hips that had AP surgery as the index procedure, 4 (25%) returned to sports without limitations and 11 (69%) subsequently had hip arthroscopy at a mean 20 months after pubalgia surgery. Of 8 hips managed initially with hip arthroscopy alone, 4 (50%) returned to sports without limitations and 3 (43%) had subsequent pubalgia surgery at a mean of 6 months after hip arthroscopy. Thirteen hips had AP surgery and concurrent hip arthroscopy at a single setting. Concurrent or eventual surgical treatment of both disorders led to improved postoperative outcomes scores (P < 0.05) and an unrestricted return to sporting activity in 89% of hips (24 of 27).
Conclusion
Failure to recognize and address concomitant compensatory injury patterns associated with intra-articular hip pathology can result in significant disability and persistent symptoms in athletes with pre-arthritic, mechanical hip pain. Recognition of the etiology of both intra- and extra-articular hip pain is critical to effectively and comprehensively treat patients for dysfunction of the hip joint, hemipelvis, and surrounding musculature associated with FAI.
Footnotes
The following authors declared potential conflicts of interest: Asheesh Bedi, MD, is an education consultant for Smith & Nephew.
References
- 1. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55:393-396 [DOI] [PubMed] [Google Scholar]
- 2. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533 [DOI] [PubMed] [Google Scholar]
- 3. Anderson SA, Keene JS. Results of arthroscopic iliopsoas tendon release in competitive and recreational athletes. Am J Sports Med. 2008;36:2363-2371 [DOI] [PubMed] [Google Scholar]
- 4. Antolak SJ, Jr, Hough DM, Pawlina W, Spinner RJ. Anatomical basis of chronic pelvic pain syndrome: the ischial spine and pudendal nerve entrapment. Med Hypotheses. 2002;59:349-353 [DOI] [PubMed] [Google Scholar]
- 5. Armfield DR, Kim DH, Towers JD, Bradley JP, Robertson DD. Sports-related muscle injury in the lower extremity. Clin Sports Med. 2006;25:803-842 [DOI] [PubMed] [Google Scholar]
- 6. Bankart ASB. The pathology and treatment of recurrent dislocation of the shoulder joint. Br J Surg. 1938;26:23-29 [Google Scholar]
- 7. Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscpy: from femeroacetabular impingement to instability. Arthroscopy. 2011;21:1720-1731 [DOI] [PubMed] [Google Scholar]
- 8. Benson ER, Schutzer SF. Posttraumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am. 1999;81:941-949 [PubMed] [Google Scholar]
- 9. Brophy RH, Wright RW, Powell JW, Matava MJ. Injuries to kickers in American football: the National Football League experience. Am J Sports Med. 2010;38:1166-1173 [DOI] [PubMed] [Google Scholar]
- 10. Byrd JW. Evaluation and management of the snapping iliopsoas tendon. Instr Course Lect. 2006;55:347-355 [PubMed] [Google Scholar]
- 11. Caudill P, Nyland J, Smith C, Yerasimides J, Lach J. Sports hernias: a systematic literature review. Br J Sports Med. 2008;42:954-964 [DOI] [PubMed] [Google Scholar]
- 12. Cibulka MT, Sinacore DR, Cromer GS, Delitto A. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine (Phila Pa 1976). 1998;23:1009-1015 [DOI] [PubMed] [Google Scholar]
- 13. Clemente C. Gray’s Anatomy: Anatomy of the Human Body. 13th ed. Baltimore, MD: Williams & Wilkins; 1985 [Google Scholar]
- 14. Cooper DE, Warren RF, Barnes R. Traumatic subluxation of the hip resulting in aseptic necrosis and chondrolysis in a professional football player. Am J Sports Med. 1991;19:322-324 [DOI] [PubMed] [Google Scholar]
- 15. Cross MB, Shindle MK, Kelly BT. Arthroscopic anterior and posterior labral repair after traumatic hip dislocation: case report and review of the literature. HSS J. 2010;6:223-227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. de Almeida DB, Mattei TA, Sória MG, et al. Transitional lumbosacral vertebrae and low back pain: diagnostic pitfalls and management of Bertolotti’s syndrome. Arq Neuropsiquiatr. 2009;67:268-272 [DOI] [PubMed] [Google Scholar]
- 17. Delp SL, Hess WE, Hungerford DS, Jones LC. Variation of rotation moment arms with hip flexion. J Biomech. 1999;32:493-501 [DOI] [PubMed] [Google Scholar]
- 18. Domb BG, Shindle MK, McArthur B, Voos JE, Magennis E, Kelly BT. Iliopsoas impingement: a newly identified cause of labral pathology in the hip. HSS J. 2011;7:1-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dreyfuss P, Dreyer SJ, Cole A, Mayo K. Sacroiliac joint pain. J Am Acad Orthop Surg. 2004;12:255-265 [DOI] [PubMed] [Google Scholar]
- 20. Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15:507-514 [DOI] [PubMed] [Google Scholar]
- 21. Feeley BT, Powell JW, Muller MS, Barnes RP, Warren RF, Kelly BT. Hip injuries and labral tears in the National Football League. Am J Sports Med. 2008;36:2187-2195 [DOI] [PubMed] [Google Scholar]
- 22. Frank JB, Jarit GJ, Bravman JT, Rosen JE. Lower extremity injuries in the skeletally immature athlete. J Am Acad Orthop Surg. 2007;15:356-366 [DOI] [PubMed] [Google Scholar]
- 23. Fredericson M, Moore W, Guillet M, Beaulieu C. High hamstring tendinopathy in runners: meeting the challenges of diagnosis, treatment, and rehabilitation. Phys Sportsmed. 2005;33(5):32-43 [DOI] [PubMed] [Google Scholar]
- 24. Freiberg AH. Sciatic pain and its relief by operations on muscle and fascia. Arch Surg. 1937;34:337-350 [Google Scholar]
- 25. Gamradt SC, Brophy RH, Barnes R, Warren RF, Byrd JW, Kelly BT. Nonoperative treatment for proximal avulsion of the rectus femoris in professional American football. Am J Sports Med. 2009;37:1370-1374 [DOI] [PubMed] [Google Scholar]
- 26. Greene HS, Cholewicki J, Galloway MT, Nguyen CV, Radebold A. A history of low back injury is a risk factor for recurrent back injuries in varsity athletes. Am J Sports Med. 2001;29:795-800 [DOI] [PubMed] [Google Scholar]
- 27. Hasselman CT, Best TM, Hughes CT, Martinez S, Garrett WE., Jr An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med. 1995;23:493-499 [DOI] [PubMed] [Google Scholar]
- 28. Hetsroni I, Poultsides L, Bedi A, Larson CM, Kelly BT. Anterior inferior iliac spine morphology correlates with hip range of motion: a classification system and dynamic model. Clin Orthop Relat Res. 2013;471:2497-2503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Heyworth BE, MacArthur BA, Kelly BT. Anterior hip muscle injuries. In: Guanche CA, ed. Hip and Pelvis Injuries in Sports Medicine. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2010:192-199 [Google Scholar]
- 30. Heyworth BE, Voos JE, Metzl JD. Hip injuries in the adolescent athlete. Pediatr Ann. 2007;36:713-718 [DOI] [PubMed] [Google Scholar]
- 31. Hsu JC, Fischer DA, Wright RW. Proximal rectus femoris avulsions in National Football League kickers: a report of 2 cases. Am J Sports Med. 2005;33:1085-1087 [DOI] [PubMed] [Google Scholar]
- 32. Ilizaliturri VM, Jr, Camacho-Galindo J. Endoscopic treatment of snapping hips, iliotibial band, and iliopsoas tendon. Sports Med Arthrosc. 2010;18:120-127 [DOI] [PubMed] [Google Scholar]
- 33. Ilizaliturri VM, Jr, Gonzalez-Gutierrez B, Gonzalez-Ugalde H, Camacho-Galindo J. Hip arthroscopy after traumatic hip dislocation. Am J Sports Med. 2011;39(suppl):50S-57S [DOI] [PubMed] [Google Scholar]
- 34. Irshad K, Feldman LS, Lavoie C, Lacroix VJ, Mulder DS, Brown RA. Operative management of “hockey groin syndrome”: 12 years of experience in National Hockey League players. Surgery. 2001;130:759-764 [DOI] [PubMed] [Google Scholar]
- 35. Kachingwe AF, Grech S. Proposed algorithm for the management of athletes with athletic pubalgia (sports hernia): a case series. J Orthop Sports Phys Ther. 2008;38:768-781 [DOI] [PubMed] [Google Scholar]
- 36. Kennedy MJ, Lamontagne M, Beaulé PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait: walking biomechanics of FAI. Gait Posture. 2009;30:41-44 [DOI] [PubMed] [Google Scholar]
- 37. Knockaert DC, D’Heygere FG, Bobbaers HJ. Ilioinguinal nerve entrapment: a little-known cause of iliac fossa pain. Postgrad Med J. 1989;65:632-635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lachiewicz PF, Kauk JR. Anterior iliopsoas impingement and tendinitis after total hip arthroplasty. J Am Acad Orthop Surg. 2009;17:337-344 [DOI] [PubMed] [Google Scholar]
- 39. Lacroix VJ, Kinnear DG, Mulder DS, Brown RA. Lower abdominal pain syndrome in national hockey league players: a report of 11 cases. Clin J Sport Med. 1998;8:5-9 [DOI] [PubMed] [Google Scholar]
- 40. Lamontagne M, Kennedy MJ, Beaule PE. The effect of cam FAI on hip and pelvic motion during maximum squat. Clin Orthop Relat Res. 2009;467:645-650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Larson CM, Pierce BR, Giveans MR. Treatment of athletes with symptomatic intra-articular hip pathology and athletic pubalgia/sports hernia: a case series. Arthroscopy. 2011;27:768-775 [DOI] [PubMed] [Google Scholar]
- 42. Lawrence JP, Greene HS, Grauer JN. Back pain in athletes. J Am Acad Orthop Surg. 2006;14:726-735 [DOI] [PubMed] [Google Scholar]
- 43. Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616-622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Martin HD, Shears SA, Johnson JC, Smathers AM, Palmer IJ. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 2011;27:172-181 [DOI] [PubMed] [Google Scholar]
- 45. Metzmaker JN, Pappas AM. Avulsion fractures of the pelvis. Am J Sports Med. 1985;13:349-358 [DOI] [PubMed] [Google Scholar]
- 46. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28:2-8 [DOI] [PubMed] [Google Scholar]
- 47. Meyers WC, McKechnie A, Philippon MJ, Horner MA, Zoga AC, Devon ON. Experience with “sports hernia” spanning two decades. Ann Surg. 2008;248:656-665 [DOI] [PubMed] [Google Scholar]
- 48. Miller SF, Congeni J, Swanson K. Long-term functional and anatomical follow-up of early detected spondylolysis in young athletes. Am J Sports Med. 2004;32:928-933 [DOI] [PubMed] [Google Scholar]
- 49. Moorman CT, 3rd, Warren RF, Hershman EB, et al. Traumatic posterior hip subluxation in American football. J Bone Joint Surg Am. 2003;85:1190-1196 [DOI] [PubMed] [Google Scholar]
- 50. Murata Y, Ogata S, Ikeda Y, Yamagata M. An unusual cause of sciatic pain as a result of the dynamic motion of the obturator internus muscle. Spine J. 2009;9:e16-e18 [DOI] [PubMed] [Google Scholar]
- 51. Nelson EN, Kassarjian A, Palmer WE. MR imaging of sports-related groin pain. Magn Reson Imaging Clin N Am. 2005;13:727-742 [DOI] [PubMed] [Google Scholar]
- 52. Ouellette H, Thomas BJ, Nelson E, Torriani M. MR imaging of rectus femoris origin injuries. Skeletal Radiol. 2006;35:665-672 [DOI] [PubMed] [Google Scholar]
- 53. Paajanen H, Hermunen H, Karonen J. Pubic magnetic resonance imaging findings in surgically and conservatively treated athletes with osteitis pubis compared to asymptomatic athletes during heavy training. Am J Sports Med. 2008;36:117-121 [DOI] [PubMed] [Google Scholar]
- 54. Pace JB, Nagle D. Piriform syndrome. West J Med. 1976;124:435-439 [PMC free article] [PubMed] [Google Scholar]
- 55. Pallia CS, Scott RE, Chao DJ. Traumatic hip dislocation in athletes. Curr Sports Med Rep. 2002;1:338-345 [DOI] [PubMed] [Google Scholar]
- 56. Pan H, Kawanabe K, Akiyama H, Goto K, Onishi E, Nakamura T. Operative treatment of hip impingement caused by hypertrophy of the anterior inferior iliac spine. J Bone Joint Surg Br. 2008;90:677-679 [DOI] [PubMed] [Google Scholar]
- 57. Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778-785 [DOI] [PubMed] [Google Scholar]
- 58. Philippon MJ, Kuppersmith DA, Wolff AB, Briggs KK. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25:169-174 [DOI] [PubMed] [Google Scholar]
- 59. Radic R, Annear P. Use of pubic symphysis curettage for treatment-resistant osteitis pubis in athletes. Am J Sports Med. 2008;36:122-128 [DOI] [PubMed] [Google Scholar]
- 60. Rajasekhar C, Kumar KS, Bhamra MS. Avulsion fractures of the anterior inferior iliac spine: the case for surgical intervention. Int Orthop. 2001;24:364-365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Sairyo K, Katoh S, Sasa T, et al. Athletes with unilateral spondylolysis are at risk of stress fracture at the contralateral pedicle and pars interarticularis: a clinical and biomechanical study. Am J Sports Med. 2005;33:583-590 [DOI] [PubMed] [Google Scholar]
- 62. Shindle MK, Voos JE, Heyworth BE, et al. Hip arthroscopy in the athletic patient: current techniques and spectrum of disease. J Bone Joint Surg Am. 2007;89(suppl 3):29-43 [DOI] [PubMed] [Google Scholar]
- 63. Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24:1407-1421 [DOI] [PubMed] [Google Scholar]
- 64. Tortolani PJ, Carbone JJ, Quartararo LG. Greater trochanteric pain syndrome in patients referred to orthopedic spine specialists. Spine J. 2002;2:251-254 [DOI] [PubMed] [Google Scholar]
- 65. van der Wurff P, Hagmeijer RH, Meyne W. Clinical tests of the sacroiliac joint. A systematic methodological review. Part 1: reliability. Man Ther. 2000;5:30-36 [DOI] [PubMed] [Google Scholar]
- 66. Verrall GM, Hamilton IA, Slavotinek JP, et al. Hip joint range of motion reduction in sports-related chronic groin injury diagnosed as pubic bone stress injury. J Sci Med Sport. 2005;8:77-84 [DOI] [PubMed] [Google Scholar]
- 67. Verrall GM, Slavotinek JP, Barnes PG, Esterman A, Oakeshott RD, Spriggins AJ. Hip joint range of motion restriction precedes athletic chronic groin injury. J Sci Med Sport. 2007;10:463-466 [DOI] [PubMed] [Google Scholar]
- 68. Waters PM, Millis MB. Hip and pelvic injuries in the young athlete. Clin Sports Med. 1988;7:513-526 [PubMed] [Google Scholar]
- 69. Weber M, Ganz R. Recurrent traumatic dislocation of the hip: report of a case and review of the literature. J Orthop Trauma. 1997;11:382-385 [DOI] [PubMed] [Google Scholar]
- 70. Williams JG. Limitation of hip joint movement as a factor in traumatic osteitis pubis. Br J Sports Med. 1978;12:129-133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Yoshio M, Murakami G, Sato T, Sato S, Noriyasu S. The function of the psoas major muscle: passive kinetics and morphological studies using donated cadavers. J Orthop Sci. 2002;7:199-207 [DOI] [PubMed] [Google Scholar]
- 72. Zebala LP, Schoenecker PL, Clohisy JC. Anterior femoroacetabular impingement: a diverse disease with evolving treatment options. Iowa Orthop J. 2007;27:71-81 [PMC free article] [PubMed] [Google Scholar]
- 73. Ziprin P, Williams P, Foster ME. External oblique aponeurosis nerve entrapment as a cause of groin pain in the athlete. Br J Surg. 1999;86:566-568 [DOI] [PubMed] [Google Scholar]