Leveraging computers and mobile devices to understand one’s health, support self-management, and interact with providers is associated with favorable diabetes outcomes (1,2). However, not everyone uses these technologies, potentially limiting broad benefit. We examined whether patient race and health literacy (HL) status are associated with technology use.
We analyzed data from a cross-sectional study of adults (age ≥18 years) with type 2 diabetes from a federally qualified health center in Nashville, TN. Research assistants worked with clinic personnel to recruit eligible patients arriving for appointments. Research assistants conducted in-person interviews to collect self-reported information on demographics and technology access and use (Table 1), administered the Short Test of Functional Health Literacy in Adults (3), and reviewed medical charts. All participants received a point-of-care (POC) A1C test on the day of participation (4). Only 38% had a chart-reviewed A1C that same day (with POC, ρ = 0.87, P < 0.001), requiring use of POC. We used SAS version 9.3 to limit the analysis to non-Hispanic white (NHW) and African American/black (AA/black) participants, and conducted t tests and χ2 tests to make comparisons by race and, separately, by HL status (limited [inadequate/marginal] vs. adequate).
Table 1.
Participant characteristics and differences by race and health literacy status
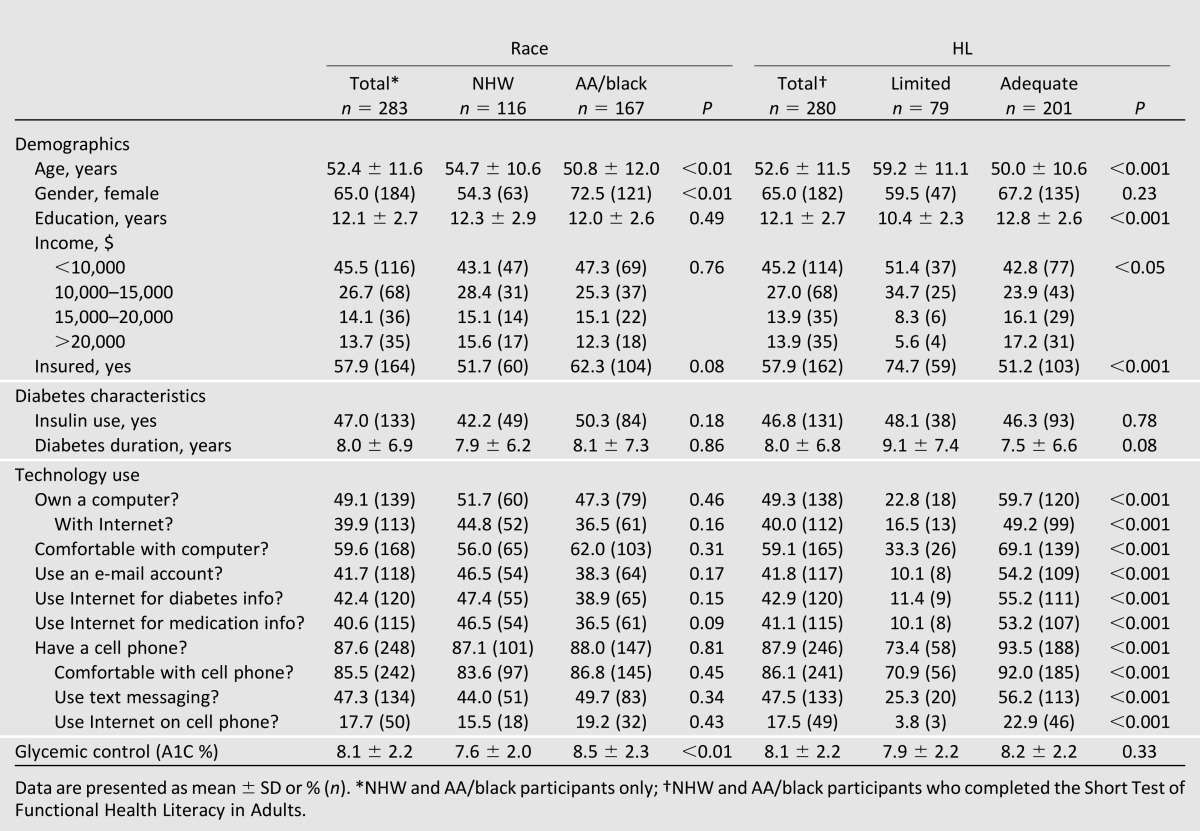
Research assistants approached 86.2% of the 588 type 2 diabetic patients who had a clinic appointment during the study period. Of those eligible (372), 84% participated (n = 314); 283 were NHW or AA/black (Table 1). Race was not associated with HL status as a categorical or continuous variable. Participants with limited HL were less likely than participants with adequate HL to own a computer or a cell phone, be comfortable with or use the Internet on either device, have an e-mail account, send text messages, or use the Internet to get information about diabetes or medications (all P < 0.001) (Table 1). AA/blacks were as likely as NHWs to access and use technologies, but AA/blacks had worse glycemic control than NHWs. HL status was not associated with A1C (P = 0.33).
The “digital divide” may be narrowing by race, but not by HL, which mirrors recent increases in technology use by racial and ethnic minorities (5). There were no differences in A1C by HL status despite differences in technology use. In contrast, AA/blacks had worse glycemic control than NHWs despite similarities in having access and using technologies. Other patient factors (e.g., treatment regimen) may be more strongly related to A1C, contribute to disparities in A1C despite equity in technology use (e.g., medication noncompliance), and explain the association between technology use and outcomes (e.g., age). Future research should explore these questions using a cohort study design to evaluate the impact of technology use on A1C over time. In addition to the cross-sectional design limitation, other limitations include sampling from one clinic, reliance on self-report measures, and not assessing the use of health information technologies (e.g., patient portals), which have the sole purpose of communicating health information.
Increased reliance on technology to promote patient health may have limited value if certain groups lack access and/or the skills to leverage these tools. Efforts are needed to engage individuals with limited HL in the development of technology-based interventions that they would use.
Article Information
Acknowledgments. The authors would like to thank Cecilia C. Quintero, Sahbina Ebba, Karen Calderon, Leo Cortes, Anne Crook, Carmen Mekhail, the Vine Hill Community Clinic personnel, and the participants for their contributions to this research.
Funding. This work was funded with support from the Vanderbilt Clinical Translational Scientist Award (UL1TR000445) from the National Center for Advancing Translational Sciences. C.Y.O. was supported by a Career Development Award (K01DK087894) from the National Institute of Diabetes and Digestive and Kidney Diseases.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. R.J.C. and C.Y.O. managed data, conducted analyses, and interpreted the data. R.J.C. wrote the manuscript. S.K., D.G.S., and T.A.E. reviewed and edited the manuscript. C.Y.O. designed the parent study; supervised all aspects of data collection, cleaning, and management; guided the analyses; interpreted the data; and reviewed and edited the manuscript. All authors approved the final version before it was submitted for publication. C.Y.O. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the National Institutes of Health.
References
- 1.Mulvaney SA, Ritterband LM, Bosslet L. Mobile intervention design in diabetes: review and recommendations. Curr Diab Rep 2011;11:486–493 [DOI] [PubMed] [Google Scholar]
- 2.Osborn CY, Mayberry LS, Mulvaney SA, Hess R. Patient web portals to improve diabetes outcomes: a systematic review. Curr Diab Rep 2010;10:422–435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns 1999;38:33–42 [DOI] [PubMed] [Google Scholar]
- 4.Kennedy L, Herman WH, GOAL A1C Study Team Glycated hemoglobin assessment in clinical practice: comparison of the A1cNow point-of-care device with central laboratory testing (GOAL A1C Study). Diabetes Technol Ther 2005;7:907–912 [DOI] [PubMed] [Google Scholar]
- 5.Zickuhr K, Smith A. Digital Differences. Washington, DC, Pew Internet and American Life Project, 2012. Available from http://pewinternet.org/Reports/2012/Digital-differences.aspx. Accessed 1 February 2013 [Google Scholar]


